Abstract
Purpose of Review
Vascularized bone free flaps are a fundamental tool in complex head and neck reconstruction. While the principles of bony reconstruction have largely remained unchanged, technological innovations have permeated reconstructive paradigms over the past four decades. The purpose of this review is to summarize new technology in bony reconstruction for head and neck defects.
Recent Findings
Numerous innovations have been described and offer significant improvements in functional outcomes, accuracy and reliability of bony reconstruction. These include optimization in surgical positioning facilitating improved exposure to the scapula donor site, virtual surgical planning for craniofacial defects, three-dimensional printers that have modernized how surgeons critically assess craniofacial anatomy and anticipate reconstructive challenges, and advances in material science including the use of absorbable plates.
Summary
This review describes fundamental innovations in bony reconstruction of complex head and neck defects that have vastly improved surgical approaches throughout all phases of reconstruction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Vascularized bone free flap (VBFF) reconstruction has evolved significantly since Hidalgo and others described novel free tissue donor sites for complex head and neck defects over four decades ago [1]. These flaps have enhanced our reconstructive armamentarium and permitted significant improvement in the functional-based approach to head and neck reconstruction. While core principles of bony free flap harvest and reconstruction have not changed, novel technological improvements have greatly expanded our understanding of and utility for them. This review will illustrate examples of recent innovations in bony free flap reconstruction, ranging from positioning to virtual planning and augmented reality.
Innovations in Bony Reconstruction
Surgical Positioning
Vascularized bone free flap harvest techniques have been modernized over the past decade to ease simplicity in operative planning and execution. Recent innovations have introduced novel approaches to positioning that vastly improve operative exposure and permit ease of access to previously difficult sites. An example of this is the scapula donor site.
The subscapular system permits chimeric flap design for both bone and soft-tissue defects, but has historically been a challenging donor site due to intraoperative positioning requirements. In his original description of the operative technique, dos Santos et al. described prone or lateral positioning [2]. Paek et al. [3] first described a dorsal decubitus position using a bean bag to rotate the thorax and pelvis thirty degrees, permitting simultaneous two-team surgical approach. These and other approaches, however, have traditionally relied on assistants to position and retract the arm and shoulder. A novel approach for arm and shoulder positioning was introduced by Stevens et al. in 2018 [4∙∙]. They described the use of the Spider Limb Positioner (Smith and Nephew, Andover, MA, USA) and bean bag, adopted from orthopedic surgeons, to facilitate precise and continuous fixation of the upper extremity without the need for an assistant or Mayo stand. Cited benefits include decongestion of the surgical field and the ability to perform concurrent two-team approach in all 78 cases studied. In this study there were no nerve compression injuries [4]. Furthermore, the ability to proceed either simultaneously or sequentially, without the need for repositioning allows for more efficient use of operating room time and reduction of re-prepping and draping (Fig. 1). Recent adaptations of the Spider Limb Positioner have also been applied for use in fibular free flap harvest. We have found that this allows a fixed and elevated positioning of the leg that allows a more accessible posterior dissection and minimizes the need of assistants for leg retraction (Fig. 2).
Indeed, novel surgical positioning equipment and mechanical retractors have permeated other facets of reconstructive surgery and will likely continue to be integrated into a broader swath of surgical procedures to not only optimize exposure but also enhance trainee education.
Virtual Surgical Planning
A major challenge in VBFF reconstruction is contouring longitudinal segments of bone to optimally restore facial symmetry and baseline function in an efficient and precise manner. Since the fibula free flap was first described by Hidalgo in 1989, traditional free-hand techniques for contouring and approximating bone segments continue to be used widely [1]. These often require advanced skillset and subjective assessment of complex defects. Operative efficiency is largely dependent upon intraoperative judgment, speed, and surgical experience. These surgeon-specific differences may contribute to imperfect and imprecise outcomes [5, 6].
Three-dimensional (3D) virtual surgical planning (VSP) for osseous head and neck defects was first introduced in 1993 and has evolved significantly over the past three decades to offer enhanced planning and execution of osseous reconstruction [7, 8]. Digital simulations of bony anatomy are derived from computed tomographic data that are digitized into computer aided design (CAD) software. VSP can be used to guide ablative planning, design stereolithographic models, facilitate design of pre-bent reconstructive plates and inform design and creation of complex intraoperative templates and cutting guides (Fig. 3) [9,10,11].
Since it was first introduced, VSP has been used selectively by surgeons; however, multi-institution and meta-analysis investigations suggest it may offer significant benefits to the surgeon and patient, including improved operative efficiency. Hanasono et al. [12∙] found that operative time for complex fibula reconstruction cases was significantly reduced from 10.5 to 8.8 h with VSP. A meta-analysis of 713 patients by Tang et al. [13] similarly found a significant decrease in operative time and ischemia time with no difference in complication rates. VSP allows the surgeon to perform pre-planned osteotomies, while the flap is still perfused, thereby further reducing ischemia time [14].
Importantly, there is data to support improved accuracy and precision in free fibula reconstruction with VSP. Hanasono et al. [12∙] demonstrated 2.4 mm accuracy of planned segment dimensions, and 3.5-degree accuracy for planned angles. Accuracy in fibula segment dimensions and anterior and posterior mandibular angles assessed based on pre- and postoperative imaging suggest that the technology is reliable and precise [15]. Survey studies suggest that surgeons perceive improved accuracy as a major benefit of VSP technology [16, 17]. Further supporting the benefits of the increased precisions seen with VSP, Chang et al. [18] confirmed that time was reduced in the VSP group, as well as less revisions and less bony non-unions. Additionally, VSP facilitates collaboration between ablative and reconstructive surgical teams. This may permit greater ablative accuracy afforded by better three-dimensional visualization of the tumor and willingness to plan more liberal resection margins [19]. Patient satisfaction-based surveys also suggest improved functional and esthetic outcomes in numerous studies [20, 21].
Indeed, while VSP allows the surgeon to overcome numerous challenges in precise and accurate osseous reconstruction, there are inherent limitations that may manifest as imperfections in pre-bent plates, cutting guide positioning, or malposition of fibula segments when compared to the intended design. Complex reconstructions with multiple segments and angles may be more prone to iterative errors if one or more of these imperfections become apparent intraoperatively, leading to frustration and further challenge. One of the other major challenges with VSP is intraoperative changes that need to be made either at resection of the primary site (i.e., larger resection) versus needing to change donor sites (i.e., using the opposite leg that was initially used for VSP). In many cases the surgeon must be facile to perform the reconstruction in the absence of VSP or be able to alter where the medial cuts are made on the bony flap. Modifications in cutting design or use of additional guiding devices to enhance segment registration and accuracy have been proposed and employed with success [22]. Widespread use of VSP may also be limited by costs associated with its use; however, proponents of it argue cost-savings derived from shorter operating room time supports its value in the current healthcare climate [23].
3D Printing
3D printing, also known as stereolithography, was first described in 1984 and later patented by Chuck Hull in 1986 as an additive manufacturing tool for industrial manufacturing [24]. Commercially available 3D printers were first released in 2009 and consumer-level 3D printers can now be purchased for less than $1000. The development of specialized 3D printers has permitted rapid prototype modeling (RPM). Realistic models of a patient’s craniofacial anatomy can facilitate beside surgical planning, for example the design and bending of reconstruction plates intraoperatively [25].
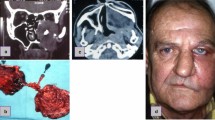
With the recent development and release of free virtual surgical planning software, hospital-driven planning software and printing of 3D cutting guides may be a cost-conscious alternative to third-party VSP entities. Zavattero et al. [26] demonstrated a low-cost virtual planning and 3D printing solution for mandibular reconstruction through an in-hospital 3D printing lab, offering a proposed pathway for widespread adoption of the technology for smaller institutions or in cases in which commercial options are not available. We have used 3D printed models to supplement complex reconstruction where VSP is not possible. Scapular reconstruction and VSP is limited by the bulky muscle left on the flap at the time of harvest, thus limited the ability to place cutting guides. We use 3D models to allow for sizing of the defect and scapular reconstruction (Fig. 4).
Augmented reality
Augmented reality (AR) has been introduced into multiple realms of medicine, most notably in medical education [27]. Recent studies suggest it may enhance VSP-aided reconstruction. Battaglia et al. described its use in visualizing and locating anatomy during fibula harvest and verifying position of cutting guides to optimize planning accuracy [28]. AR, which does not require fiducial tracking markers, has also been demonstrated as an aid in maxillary repositioning craniofacial surgery [29].
Absorbable Plates
Titanium plates and screws are the mainstay of rigid fixation for craniofacial trauma and reconstruction. Limitations of this technique include risk of implant exposure or extrusion, screw loosening, infection, radiographic artifact, potential need for secondary plate removal [30]. These limitations may be amplified in previously radiated patients. Bioabsorbable plates, made of poly(lactic-co-glycolic acids) or other co-polymers, were introduced as early as 1972 as an alternative to titanium implant systems for mandibular fractures [31]. As implied by their name, they are completely resorbable, do not cause radiographic artifact, and may provide comparable strength in the appropriate context. Whereas metallic fixation may lead to “stress shielding”, caused by deprivation of native bone from physiologic stress leading to thinner and weaker bone, bioabsorbable plates may minimize this risk and permit enhanced strength of grafted and native bone [32]. These devices allow for enhanced customization by way of simple molding, creation of customized holes while maintaining strength [32,33,34,35]. Their use for load-bearing mandibular defects, however, has not been described.
Bone implants for dental rehabilitation
Dental rehabilitation is an important consideration during mandibular rehabilitation and reconstruction. VSP has greatly improved accuracy and precision of mandibular reconstruction, and through CAD, surgeons can plan in advance for secondary dental rehabilitation by anticipating where dental posts may be placed and avoid screw placement in the same location. Primary placement of osseointegrated implants for fibula free flap reconstruction was first described by Urken et al. [36] in 1989 and preceded the advent of VSP; however, this has not been widely adopted. Dental rehabilitation procedures are often delayed until osseous integration occurs or until adjuvant treatment, such as radiation therapy, is completed.
In the era of VSP, however, there has been a recent trend toward earlier dental rehabilitation and placement of dental implants [37]. Single-stage mandibular ablation and reconstruction procedures, the so-called “Jaw in a Day”, were first described by Levine et al. in 2013 [38∙]. In these cases, implant-supported dental prostheses are placed at the time of fibula free flap harvest and inset. These cases rely on VSP to determine optimal placement of dental implants as well as dental prosthesis to optimize functional occlusion. Proponents of this single-stage procedure cite multiple benefits including elimination of partial or complete edentulism time period and improvement in patient recovery and psychological well being [39]. Long term outcomes data is currently lacking. The technique is notably dependent upon multidisciplinary collaboration between surgeon, prosthodontist, biomedical engineer and dental technicians which is not possible at many institutions. Additional studies are necessary to assess its success and safety from a functional and oncologic perspective.
Conclusion
Surgical innovation in bony free flap reconstruction has evolved significantly over the past few decades. Novel approaches to patient positioning using robotic devices, computer-assisted design software, and multidisciplinary ingenuity in dental rehabilitation underscore the future direction of advanced bony reconstruction in head and neck. These and other innovations will undoubtedly continue to evolve and allow surgeons to deliver cutting-edge surgical care to patients.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hidalgo DA. Fibula free flap: a new method of mandible reconstruction. Plast Reconstr Surg. 1989;84:71–9.
dos Santos LF. The vascular anatomy and dissection of the free scapular flap. Plast Reconstr Surg. 1984;73:599–604.
Paek LS, Boa O, Revol M, Servant JM, Harris PG, Danino AM. A new dorsal decubitus position for raising subscapular-based flaps. J Plast Reconstr Aesthet Surg. 2012;65:e60-63.
∙∙Stevens JR, Rosko AJ, Marchiano E, et al. The Spider Limb Positioner in subscapular system free flaps. Oral Oncol. 2018;85:24–8. Use of spider limb allows a more straightforward approach to the subscapular system to allow syncrhonous ablative and harvest procedures and removes the need for repositioning.
Leiggener CS, Krol Z, Gawelin P, Buitrago-Tellez CH, Zeilhofer HF, Hirsch JM. A computer-based comparative quantitative analysis of surgical outcome of mandibular reconstructions with free fibula microvascular flaps. J Plast Surg Hand Surg. 2015;49:95–101.
Brown JS, Shaw RJ. Reconstruction of the maxilla and midface: introducing a new classification. Lancet Oncol. 2010;11:1001–8.
Rose EH, Norris MS, Rosen JM. Application of high-tech three-dimensional imaging and computer-generated models in complex facial reconstructions with vascularized bone grafts. Plast Reconstr Surg. 1993;91:252–64.
Altobelli DE, Kikinis R, Mulliken JB, Cline H, Lorensen W, Jolesz F. Computer-assisted three-dimensional planning in craniofacial surgery. Plast Reconstr Surg. 1993;92:576–85.
Ciocca L, Mazzoni S, Fantini M, Persiani F, Marchetti C, Scotti R. CAD/CAM guided secondary mandibular reconstruction of a discontinuity defect after ablative cancer surgery. J Craniomaxillofac Surg. 2012;40:e511-515.
Derand P, Hirsch JM. Virtual bending of mandibular reconstruction plates using a computer-aided design. J Oral Maxillofac Surg. 2009;67:1640–3.
Sharaf B, Levine JP, Hirsch DL, Bastidas JA, Schiff BA, Garfein ES. Importance of computer-aided design and manufacturing technology in the multidisciplinary approach to head and neck reconstruction. J Craniofac Surg. 2010;21:1277–80.
∙Hanasono MM, Skoracki RJ. Computer-assisted design and rapid prototype modeling in microvascular mandible reconstruction. Laryngoscope. 2013;123:597–604. CAD-CAM technology demonstrates signigicantly reduced operative times relative to non-modeled/planned surgeries. CAD-CAM can be a critical adjunt for bony reconstruction when the original bony architechture has been altered.
Tang NSJ, Ahmadi I, Ramakrishnan A. Virtual surgical planning in fibula free flap head and neck reconstruction: a systematic review and meta-analysis. J Plast Reconstr Aesthet Surg. 2019;72:1465–77.
Seruya M, Fisher M, Rodriguez ED. Computer-assisted versus conventional free fibula flap technique for craniofacial reconstruction: an outcomes comparison. Plast Reconstr Surg. 2013;132:1219–28.
Metzler P, Geiger EJ, Alcon A, Ma X, Steinbacher DM. Three-dimensional virtual surgery accuracy for free fibula mandibular reconstruction: planned versus actual results. J Oral Maxillofac Surg. 2014;72:2601–12.
Patel A, Otterburn D, Saadeh P, Levine J, Hirsch DL. 3D volume assessment techniques and computer-aided design and manufacturing for preoperative fabrication of implants in head and neck reconstruction. Facial Plast Surg Clin North Am. 2011;19(683–709):ix.
Rodby KA, Turin S, Jacobs RJ, et al. Advances in oncologic head and neck reconstruction: systematic review and future considerations of virtual surgical planning and computer aided design/computer aided modeling. J Plast Reconstr Aesthet Surg. 2014;67:1171–85.
Chang EI, Jenkins MP, Patel SA, Topham NS. Long-term operative outcomes of preoperative computed tomography-guided virtual surgical planning for osteocutaneous free flap mandible reconstruction. Plast Reconstr Surg. 2016;137:619–23.
Ciocca L, Mazzoni S, Fantini M, et al. A CAD/CAM-prototyped anatomical condylar prosthesis connected to a custom-made bone plate to support a fibula free flap. Med Biol Eng Comput. 2012;50:743–9.
Modabber A, Legros C, Rana M, Gerressen M, Riediger D, Ghassemi A. Evaluation of computer-assisted jaw reconstruction with free vascularized fibular flap compared to conventional surgery: a clinical pilot study. Int J Med Robot. 2012;8:215–20.
Ueda K, Tajima S, Oba S, Omiya Y, Byun SI, Okada M. Mandibular contour reconstruction with three-dimensional computer-assisted models. Ann Plast Surg. 2001;46:387–93.
Zheng GS, Su YX, Liao GQ, et al. Mandible reconstruction assisted by preoperative simulation and transferring templates: cadaveric study of accuracy. J Oral Maxillofac Surg. 2012;70:1480–5.
Zweifel DF, Simon C, Hoarau R, Pasche P, Broome M. Are virtual planning and guided surgery for head and neck reconstruction economically viable? J Oral Maxillofac Surg. 2015;73:170–5.
Hall C. Apparatus for production of three-dimensional objects by stereolithography. In: Office USP, ed. United States of America: UVP, Inc., San Gabriel, California, 1986
Kernan BT, Wimsatt JA 3rd. Use of a stereolithography model for accurate, preoperative adaptation of a reconstruction plate. J Oral Maxillofac Surg. 2000;58:349–51.
Zavattero E, Fasolis M, Novaresio A, Gerbino G, Borbon C, Ramieri G. The shape of things to come: in-hospital three-dimensional printing for mandibular reconstruction using fibula free flap. Laryngoscope. 2020
Kamphuis C, Barsom E, Schijven M, Christoph N. Augmented reality in medical education? Perspect Med Educ. 2014;3:300–11.
Battaglia S, Badiali G, Cercenelli L, et al. Combination of CAD/CAM and augmented reality in free fibula bone harvest. Plast Reconstr Surg Glob Open. 2019;7:e2510.
Badiali G, Ferrari V, Cutolo F, et al. Augmented reality as an aid in maxillofacial surgery: validation of a wearable system allowing maxillary repositioning. J Craniomaxillofac Surg. 2014;42:1970–6.
Francel TJ, Birely BC, Ringelman PR, Manson PN. The fate of plates and screws after facial fracture reconstruction. Plast Reconstr Surg. 1992;90:568–73.
Getter L, Cutright DE, Bhaskar SN, Augsburg JK. A biodegradable intraosseous appliance in the treatment of mandibular fractures. J Oral Surg. 1972;30:344–8.
Ashammakhi N, Peltoniemi H, Waris E, et al. Developments in craniomaxillofacial surgery: use of self-reinforced bioabsorbable osteofixation devices. Plast Reconstr Surg. 2001;108:167–80.
Ashammakhi N, Suuronen R, Tiainen J, Tormala P, Waris T. Spotlight on naturally absorbable osteofixation devices. J Craniofac Surg. 2003;14:247–59.
Ashammakhi N, Serlo W. Reflections on complications to bioresorbable osteofixation devices. J Craniofac Surg. 2007;18:1242–3.
Ashammakhi N, Renier D, Arnaud E, et al. Successful use of biosorb osteofixation devices in 165 cranial and maxillofacial cases: a multicenter report. J Craniofac Surg. 2004;15:692–701.
Urken ML, Buchbinder D, Weinberg H, Vickery C, Sheiner A, Biller HF. Primary placement of osseointegrated implants in microvascular mandibular reconstruction. Otolaryngol Head Neck Surg. 1989;101:56–73.
Roser SM, Ramachandra S, Blair H, et al. The accuracy of virtual surgical planning in free fibula mandibular reconstruction: comparison of planned and final results. J Oral Maxillofac Surg. 2010;68:2824–32.
∙Levine JP, Bae JS, Soares M, et al. Jaw in a day: total maxillofacial reconstruction using digital technology. Plast Reconstr Surg. 2013;131:1386–91. Modeling technology integrated with bony dental implants offers a “jaw in a day” which can be critical for patients who need adjuvant radiation and may not be candidates for post-radiation dental implants.
Patel A, Harrison P, Cheng A, Bray B, Bell RB. Fibular reconstruction of the maxilla and mandible with immediate implant-supported prosthetic rehabilitation: jaw in a day. Oral Maxillofac Surg Clin North Am. 2019;31:369–86.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical collection on Plastic Surgery.
Rights and permissions
About this article
Cite this article
Sethi, R.K.V., Spector, M.E. & Chinn, S.B. New Technologies in Bony Reconstruction of Complex Head and Neck Defects. Curr Surg Rep 9, 13 (2021). https://doi.org/10.1007/s40137-021-00290-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s40137-021-00290-w