Abstract
Purpose of Review
Does management and outcomes of penetrating injuries to the left colon differ?
Recent Findings
Management pendulum has swung from non-operative management during the Civil War era, to mandatory exploration and fecal diversion by WWII. Continuing advancements in medical management, anesthesia, and surgical techniques have led to the transition from mandatory fecal diversion to primary repair. Civilian trauma experience further supported this paradigm shift with identification of risk factors better defining the role of primary repair. Patients with non-destructive injuries benefited from primary repair, while in those with destructive injuries, resection, and anastomosis is recommended. Injury location historically has been managed with the bias of left-sided colonic injuries mandating fecal diversion due to concerns for increased complications. Evolving literature contradicts such logic as colonic related outcomes appear similar.
Summary
The majority of penetrating colon injuries can be managed safely with primary repair despite anatomic injury location as outcomes are similar.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Similar to many advances in trauma care, the advancements in penetrating colonic injury management parallels that of military conflicts. Prior to World War I, the standard treatment of penetrating abdominal trauma was expectant management, an approach associated with mortality rates in excess of 90%. Exploratory laparotomy was rarely performed and wound management presented many challenges. World War I introduced high-velocity weaponry producing an increase incidence of destructive injuries, leading some surgeons to advocate for operative management of penetrating abdominal wounds. With advances in anesthesia, sterility and surgical techniques to include primary repair mortality rates were lowered to 50–75% [1, 2]. The World War II experience saw a continuing rise in incidence and severity of penetrating abdominal trauma. The combination of increased injury severity and inexperience young surgeons resulted in an unchanged high mortality rate. Surgical intervention, in the form of an exploratory laparotomy and fecal diversion, was mandated as the standard for management of penetrating colon injuries [3, 4]. With continued advancements in the areas of triage, resuscitation, and antibiotics, colon associated mortality fell to 22–35% while surgical management remained unchanged as all penetrating colon injuries were managed with exteriorization.
In 1951, Woodhall and Ochsner challenged the routine colostomy for penetrating colon injuries due to their civilian trauma experiences emphasizing the differences in injuries resulting from high-velocity versus low-velocity weaponry [5]. Their study reviewed 55 patients in which mortality for colonic wounds managed with primary repair was 9% compared to 40% for colonic wounds managed with a colostomy. Following World War II, surgeons returned to home with the engrained approach to penetrating colon injuries where fecal diversion was the rule. They soon discovered that civilian penetrating colon injuries differed as they were less destructive when compared to from those observed during military conflicts. Although mandatory diversion predominated for the next several decades, reports generating data supporting primary repair of penetrating colon injuries were published challenging this long established practice.
Evolution of Primary Repair
In 1979, the first randomized prospective trial comparing primary repair to diversion for management of penetrating colon injuries was published [6∙]. One hundred thirty-nine patients were randomized to primary repair (n = 67) or diversion (n = 72). The primary repair group demonstrated a lower incidence of wound infections, less intra-abdominal infections, and shorter hospital length of stay when compared to the diversion group. The findings demonstrated that primary repair was safe and associated with better outcomes. While the inclusion and exclusion criteria appear restrictive, the findings serve as the inflection point in the increasing role of primary repair in the management of penetrating colon injuries.
With increasing prospective and retrospective data favoring primary repair, the Eastern Association for the Surgery of Trauma put forth evidence-based guidelines for management of penetrating intraperitoneal injuries [7∙]. A level I recommendation supporting primary repair for non-destructive (< 50% of bowel wall involved) injuries and a Level II recommendation supporting resection and primary anastomosis for destructive injuries (> 50% bowel wall or devascularized segment) in the absence of shock, comorbidities, high injury severity, and peritonitis based upon review of pertinent literature (Table 1). In the presence of these risk factors, a fecal diversion procedure is recommended. A subsequent meta-analysis of 6 Level I studies comparing primary repair to fecal diversion in penetrating colon injuries was published in the Cochrane Database of Systemic Reviews [8]. The review, which included 705 patients, concluded that primary repair was the procedure of choice for penetrating colon injuries due to its association with significantly less morbidity, equitable mortality, and decreased procedure-related costs. A more recent meta-analysis reports congruent recommendations regardless of associated risk factors [9]. These compelling data lend supportive high level evidence to the paradigm shift in penetrating colonic injury management from a one size fits all management with fecal diversion to a more risk stratified approach of primary repair or resection and anastomosis.
Colon Injury Location
Management of penetrating colonic injuries based upon anatomic location (right side vs left side) continues to be debated. Concerns for increased complications of left-sided colonic injuries bias many practicing surgeons to perform fecal diversion procedures at a higher rate. More recent data reveal that this long held belief continues to dictate management of left-sided colonic injuries with diversion instead of evidence supported primary repair or resection and anastomosis. In 2004 a study evaluating penetrating colon injury management found that diversion was performed in 88% of left colonic injuries compared to only 31% for right colonic injuries [10]. Similar findings were reported from military data. Steele et al. reviewed the management of one hundred seventy-five colorectal injuries during Operation Iraqi Freedom and found that compared to right-sided colonic injuries, fecal diversion was performed at a higher rate for left-sided injuries (19% vs 36%) with no difference in rates of infectious complications or mortality [11]. Due to the retrospective nature of many of the studies looking at the effect of anatomic location and outcomes, the authors further concluded that the decision of the operating surgeon in terms of choice of repair introduces selection bias therefore definitive conclusions as to the effect of location on outcomes are not possible.
The first prospective study comparing outcomes of right-sided versus left-sided colonic injuries managed with primary repair demonstrated similar rates of fecal diversion, primary repair, morbidity, and mortality irrespective of anatomic location of the injury [12∙]. Sharpe et al. reported their outcomes based upon injury location (Cecum/right colon, Transverse colon, Splenic flexure, Descending colon, Sigmoid colon) [13]. Four hundred sixty-nine patients with penetrating injuries to the colon were retrospectively evaluated. Colonic injuries were managed based upon a previously established algorithm. Despite a higher rate of diversion procedures for sigmoid injuries, complications of suture line failure, intra-abdominal abscess and mortality, no statistical differences was found based on injury location. This led the authors to conclude that management of penetrating colon injuries based upon their algorithmic approach was safe irrespective of injury location. Stewart et al. reported similar results evaluating destructive colon injuries. They compared left-sided and right-sided penetrating colon injuries and found no difference in the development of anastomotic failure or intra-abdominal abscesses. Similar results were noted following multivariable logistic regression analysis [14].
Previous autopsy studies demonstrating a watershed circulation between the ascending branch of the left colic artery and the left branch of the middle colic artery have long been hypothesized to be a source for the difference in right verses left-sided colon injury management [15, 16]. Both reports describe the paucity or absence of the connection between the left branch of the middle colic artery and the ascending branch of the left colic artery. This has longed been thought to be a contributing factor to suture line failures when performing left-sided colocolostomies resulting in fecal diversion procedures being preferentially performed. Based upon the premise of colonic vasculature variation, Dente et al. sought to determine the effect of segmental variations on outcomes [17]. Two hundred seventeen patients with penetrating colonic injuries were divided into groups based upon injury location: ascending, transverse, descending and sigmoid colon. Seven suture line failures in seven patients, three in the distal transverse colon and four at the splenic flexure. The method of operative repair for the seven suture line failures were described as four occurred following primary repair and three occurred following resection and anastomosis. No suture line failure occurred in the ascending, descending, or sigmoid colon. Although the management of colonic wounds varied by segments, no significant outcome differences were noted. Three mortalities occurred in patients with high transfusion requirements, higher PATI, and advanced age. Hatch et al. performed a retrospective review using the National Trauma Data Bank evaluating outcomes of penetrating colonic injuries based on mechanism of injury, location and operative management. Of the 6817 patients included, 91% of patients suffering penetrating colonic injuries were managed by either primary repair or resection and anastomosis. No significant outcome differences could be appreciated based upon injury location [18].
Damage Control
The emergence of the damage control procedure has introduced another variable in the management of penetrating colonic trauma. Following control of hemorrhage and enteric contamination, the patient in extremis is admitted to the intensive care unit for resuscitation correcting associated acidosis, hypothermia, and coagulopathy. Upon correction of physiological derangements, the patient is returned to the operating theater usually within 24–48 h for a second-look procedure. It is usually at this time that the operating surgeon must decide whether to perform a delayed anastomosis verses a fecal diversion procedure. Questions such as what patients benefit from fecal diversion?, what is the optimal timing for performing a delayed anastomosis?, and is performing a delayed anastomosis safe? are often pondered. Miller et al. reported on 11 patients with destructive colon injuries managed with a damage control procedure. All patients received a delayed anastomosis with no reported anastomotic leaks [19]. Several subsequent series investigating resection and delayed anastomosis following a damage control laparotomy report varying colonic leak rates [20,21,22,23,24,25,26, 27∙, 28, 29] (Table 2).
As to the effect of injury location in this patient population, the data are sparse. Few studies published comment on location of the colonic injury. Ordonez et al. report 24 patients who were managed with resection and delayed anastomosis, where the anastomosis were equally distributed between both sides with 2 anastomotic leaks: one in the right colon and the other in the left colon. Georgoff et al. in their series described 6 anastomotic leaks with 4 of them colonic in location: 2 ileocolonic anastomosis, 2 transverse colocolostomies. The remaining two leaks were from primary repair of the duodenum and stomach in separate patients [26]. Another study examining colonic injury management in the setting of damage control described similar findings [28]. Out of 68 patients managed with a damage control laparotomy and delayed anastomosis, 9 (13%) leaks occurred. One leak occurred at an ileocolonic anastomosis while all others were localized to either the transverse or sigmoid colon. The Memphis group using an established management protocol for destructive colon injuries reviewed their experience with patients who received a damage control laparotomy to assess the safety of a delayed anastomosis in this setting [27]. One hundred forty-nine patients were identified, of which 42 underwent delayed anastomosis with 7 anastomotic failures occurring. However, when comparing patients who were not managed by the protocol versus those who were, a significant reduction in leak rate was noted (32% vs 4%). Four anastomotic leaks occurred in the ascending colon, 3 in the transverse colon, and 2 in the sigmoid colon. Due to both the paucity of studies as well as the limited reporting of location of anastomotic leaks the effect of location on outcomes in the damage control population remains unclear.
Conclusion
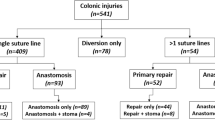
Penetrating colon injuries are common and often encountered by practicing acute care surgeons. Historically during military conflicts, these injuries were highly lethal with expectant management. Morbidity and the mortality secondary to colon injuries has dramatically declined due to advances in the management of penetrating colon injury that have resulted from both the military and civilian experiences. The increasing role of primary repair, resection, and anastomosis in properly selected patients has resulted in a marked improvement in anastomotic leaks, infectious complications, and mortality. Patients with previously identified risk factors, multiple comorbidities, and high transfusion requirements appear to be better served with fecal diversion. Despite mounting evidence supporting primary repair, there still persists concerns of colon injury location associated complications based upon evaluation of practice patterns. Anatomic location of penetrating colon injuries, more specifically left-sided verses right-sided injuries, appears to have similar outcomes. Injury location in the setting of damage control is less studied, therefore no evidence-based recommendations can be made currently. Further prospective studies that report clinical outcomes related to anatomic location of injury in the damage control setting is suggested. Such studies will provide important information to guide the acute care surgeon’s decision relative to the optimal timing of the most appropriate procedure that benefits this specific patient population. A penetrating colon injury management algorithm, based upon the current literature, for both damage control and non-damage control patients is provided (Figs. 1, 2).

Adapted from Trust et al. [30]
Defined management algorithm for penetrating colon injuries. PRBCs, packed red blood cells.

Adapted from Trust et al. [30]
Management of penetrating colon injuries in setting of damage control surgery.
References
Recently published papers of particular interest have been highlighted as: ∙ Of importance
Fraser J, Drummond H. A clinical and experimental study of three hundred perforating wounds of the abdomen. Br Med J. 1917;1:321–30.
Wallace C. A study of 1200 cases of gunshot wounds of the abdomen. Br J Surg. 1916;4:679–743.
Ogilvie WH. Abdominal wounds in the western desert. Bull US Army Med Dep. 1946;6:435–45.
Office of the Surgeon General of the United States. Circular letter 178, colon injuries. Washington, DC. 1943;173.
Woodhall JP, Ochsner A. The management of perforating injuries of the colon and rectum in civilian practice. Surgery. 1951;29:305–20.
∙ Stone HH, Fabian TC. Management of perforating colon trauma: randomization between primary closure and exteriorization. Ann Surg. 1979;190:430–6. Important study providing data supporting primary repair for management of penetrating colon injuries.
∙ Pasquale M, Fabian TC. Practice management guidelines for trauma from the Eastern Association for the Surgery of Trauma. J Trauma. 1998;44:941–56. Established guideline.
Nelson R, Singer M. Primary repair for penetrating colon injuries. Cochrane Database Syst Rev. 2003:CD002247.
DuBose J. Colonic trauma: indications for diversion vs repair. J Gastrointest Surg. 2009;13:403–4.
Adesanya AA, Ekanem EE. A ten year study of penetrating injuries of the colon. Dis Colon Rectum. 2004;47:169–77.
Steele SR, Wolcott KE, Mullenix PS, Martin MJ, Sebesta JA, Azarow KS, Beekley AC. Colon and rectal injuries during operation iraqi freedom: are there any changing trends in management or outcome? Dis Colon Rectum. 2007;50:970–7.
∙ Thompson JS, More EE, Moore JB. Comparison of penetrating injuries of the right and left colon. Ann Surg. 1981;193:414–8. Important study providing high level data as to similar outcomes based upon anatomic location of penetrating colon injuries.
Sharpe JP, Magnotti LJ, Weinberg JA, Zarzaur BL, Shahan CP, Parks NA, Fabian TC. Impact of location on outcome after penetrating colon injuries. J Trauma Acute Care Surg. 2012;73:1428–33.
Stewart RM, Fabian TC, Croce MA, Pritchard FE, Minard D, Kudsk KA. Is resection with primary anastomosis following destructive colon wounds always safe? Am J Surg. 1994;168:316–9.
Griffiths JD. Surgical Anatomy of the blood supply of the distal colon. Ann R Coll Surg Engl. 1956;19:241–56.
Meyers MA. Griffith’s point: critical anastomosis at the splenic flexure. Significance in ischemia of the colon. Am J Roentgenol. 1976;126:77–94.
Dente CJ, Feliciano DV, Rozycki GS, Wyrzykowski AD, Nicholas JM, Salomome JP, Ingram WL. Suture line failures in intra-abdominal colonic trauma: is there an effect of segmental variations in blood supply on outcome? J Trauma. 2005;59:359–68.
Hatch Q, Causey M, et al. Outcomes after colon trauma in the 21st century: an analysis of the U.S. National Trauma Data Bank. Surgery. 2013;154:397–403.
Miller PR, Chang MC, Hoth JJ, Holmes JH, Merideth JW. Colonic resection in the setting of damage control laparotomy: is delayed anastomosis safe? Am Surg. 2007;73:606–10.
Vertress A, Wakefield M, Pickett C, Greer L, Wilson A, Gillern S, Nelson J, Aydelotte J, Stojadinovic A, Shriver C. Outcomes of primary repair and primary anastomosis in war-related colon injuries. J Trauma. 2011;70:595–602.
Kashuk JL, Cothren CC, Moore EE, Johnson JL, Biffl WL, Barnett CC. Primary repair of civilian colon injuries is safe in the damage control scenario. Surgery. 2009;146:663–70.
Weinburg JA, Griffin RL, Vandromme MJ, Melton SM, George RL, Reiff DA, Kerby JD, Rue LW. Management of colon wounds in the setting of damage control laparotomy: a cautionary tale. J Trauma. 2009;67:929–35.
Ordonez CA, Pino LF, Badiel M, Sanchez AL, Loaiza J, Ballestas L, Puyana JC. Safety of performing a delayed anastomosis during damage control laparotomy in patients with destructive colon injuries. J Trauma. 2011;71:1512–8.
Ott MM, Norris PR, Diaz JJ, Collier BR, Jenkins JM, Gunter OL, Morris JA. Colon anastomosis after damage control laparotomy: recommendations from 174 trauma colectomies. J Trauma. 2011;70:596–602.
Burlew CC, Moore EE, Cuschieri J, Jurkovich GJ, Codner P, Crowell K, Nirula R, Hann J, Rowell SE, Kato CM. Sew it up! A western trauma Association multi-institutional study of enteric injury management in the post-injury open abdomen. J Trauma. 2011;70:273–7.
Georgoff P, Perales P, Laguna B, Holena D, Reilly P, Simms C. Colonic injuries and the damage control abdomen: does management strategy matter? J Surg Res. 2013;181:293–9.
∙ Sharpe JP, Magnotti LJ, Weinburg JA, Shahan CP, Cullinan DR, Marino KA, Fabian TC, Croce MA. Applicability of an established management algorithm for destructive colon injuries after abbreviated laparotomy: a 17 year experience. J Am Coll Surg. 2014;218:636–41. Excellent series regarding effect of algorithm based operative decision making in penetrating colon injuries.
Anjaria DJ, Ullman TM, Lavery R, Livingston DH. Management of colonic injuries in the setting of damage-control laparotomy: one shot to get it right. J Trauma Acute Care Surg. 2014;76:594–600.
Tatebe LC, Jennings A, Tatebe K, Handy A, Prajapati P, Smith M, Do T, Ogola G, Gandi RR, Duane TM, Luk S, Petrey LB. Traumatic colon injury in damage control laparotomy- A multicenter trial: is it safe to do a delayed anastomosis? J Trauma Acute Care Surg. 2017;82:742–9.
∙ Trust MD, Brown CV. Penetrating injuries to the colon and rectum. Curr Trauma Rep. 2015;1:113–8. Very good review with evidence based clinical management algorithm.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Nathaniel McQuay declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical collection on Trauma Surgery.
Rights and permissions
About this article
Cite this article
McQuay, N. Management of Penetrating Injury to the Left Colon. Curr Surg Rep 6, 19 (2018). https://doi.org/10.1007/s40137-018-0217-6
Published:
DOI: https://doi.org/10.1007/s40137-018-0217-6