Abstract
Purpose of Review
Summarizing the main steps that have led the endoscope to become one of the established tools in otological and neurotological surgery and evaluating the possible future applications of this device.
Recent Findings
Many are the features of the endoscope that are being improved. First the quality of the images, thanks to the introduction of 4K technology and the earliest 3D endoscopes, then the employment of robotic surgery with endoscope holders that ideally combine the endoscopic benefits with a two-handed technique.
Summary
Nowadays the endoscope is both used as the sole instrument and as an adjunct to the operative microscope for both ear and lateral skull base surgery. Thanks to courses and conventions this technique has spread worldwide, so many young surgeons have become proficient in both the operative microscope and endoscope and able to choose the appropriate treatment tool. However, further technological advancements are to be advocated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The history of endoscopic ear surgery (EES) is centred around the rediscovery of the external auditory canal as the main door to the tympanic cavity. This concept also represents one of the main advantages of this kind of approach. In cholesteatoma surgery, the transcanal endoscopic procedure enables the surgeon to tackle the pathology in the tympanic cavity and follow it in its extensions into hard-to-reach areas such as the sinus tympani and the facial recess. In fact, the endoscope bypasses the narrow portion of the ear canal, which constitutes an obstacle for the operative microscope, and allows for a look “around the corner” [1••].
Moreover, the transcanal approach provides direct access to the most upstream system of ventilation of the middle ear (the Eustachian tube and the tympanic isthmus) whose failure has been related to chronic otitis media [2, 3], whereas the traditional microscopic access through the mastoid is focused on the most downstream part of the ventilation system, the mastoid air cells.
Nowadays EES is performed in many ORs worldwide for tympanic neoplasm, otosclerosis, chronic otitis media and especially for cholesteatoma. It has turned out to be very effective in the treatment of the tympanic cavity and, in combination with the microscope, in case of mastoid extension of the lesion. Still a few drawbacks remain, in fact it is a one-handed technique with a steep learning curve, it provides a bidimensional vision and it is somewhat limited by a hard-to-manage intra-operative bleeding.
First Steps and Tools
In 1966, Harrold Hopkins developed the Hopkins rod endoscope with Karl Storz’s team and in 1984 Wullstein popularized the use of angled endoscopes. Otosurgeons therefore started using the endoscope to examine the tympanic membrane and to look through a tympanic perforation to observe the tympanic cavity, in particular to confirm perilymphatic fistulae [4] and to identify other middle ear pathological conditions [5]. Wullstein’s scope, a 2.7-mm optical system with 70° angle began to be employed for the inspection of the posterior recesses of the tympanic cavity. In 1988, the endoscope was first coupled with a micro-camera to obtain a video-monitored endoscopic experience.
The Endoscope as a Surgical Tool
While the diagnostic and documentation role of the endoscope initially played the most widely recognized part, later on this tool was employed as a companion device for the assistance in the removal of the disease. In 1990, Thomassin was the first author who described the endoscopic use in order to identify a residual cholesteatoma during microscopic surgery [6]. Later, McKennan described the technique of endoscopic second look, underlining the safety and reliability of the endoscope in detecting residual or recurrent disease, with a lower morbidity [7]. Similarly, Badr-el-Dine reported the value of endoscopy to assist cholesteatoma surgery and testified a reduced risk or recurrence thanks to its use [8], also confirmed by Ayache and colleagues [9].
Eventually the endoscope began to be used as the main working tool in ear surgery using a transcanal approach to access the tympanic cavity. The first report of endoscopic myringoplasty was published by El-Guindy in 1992 [10], but the main experience in cholesteatoma surgery dates back to 1997 thanks to the work of Tarabichi [11] who also reported his understanding of endoscopic tympanoplasty and stapes surgery in the following years [12]. As the main advantage of the tool, he underlined the possibility to evaluate the whole tympanic membrane and to treat a disease within the facial recess, hypotympanum, sinus tympani, attic and the anterior part of the tympanic cavity. In addition, the author saw the endoscopic potential of viewing structures from a multiplicity of angles, as opposed to the microscope’s single axis along the ear canal.
The current author (D.M.) and Presutti reported their first experience in endoscopic middle ear surgery in 2006 at the 93rd national congress of the Italian society of otolaryngology head and neck surgery. They stated that the use of angled endoscopes at the end of traditional microscopic procedures for cholesteatoma surgery greatly reduced the risk of leaving residues in classically hard to reach sites.
The International Working Group and Further Developments
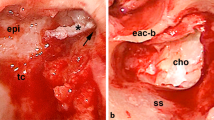
During the 2007 “8th International Conference on Cholesteatoma and Ear Surgery” in Antalya (Turkey), Dr. Stephane Ayache proposed to create an otosurgeons’ group from all over the world, who was employing the use of the endoscope for otologic procedures. This assembly, later to be named International Working Group on Endoscopic Ear Surgery (IWGEES), was initially formed by Dr. Mohamed Badr-El-Dine (Egypt), Muaaz Tarabichi (Dubai), Livio Presutti (Italy), Daniele Marchioni (Italy), Stephan Ayache (France), David Pothier (Canada) and Seiji Kakehata (Japan). They played a leading role in standardizing, teaching and spreading these techniques. In fact, many courses and congresses were organized worldwide, based on the new anatomical concepts regarding the tympanic cavity and the new physiopathological principles, developed thanks to the use of endoscopic cholesteatoma surgery (Fig. 1). New perspectives like the anatomical classification of the retrotympanic spaces and structures [13,14,15], the ventilation pathways of the middle ear [16, 17] and the selective attical dysventilation syndrome [3], which represents the rationale of the transcanal endoscopic approach to attical cholesteatoma, were perfected by the current author (D.M.) in cooperation with the Italian group of Modena. Another important contribution to the anatomical endoscopic knowledge of the middle ear was also provided by Patel et al. who focused on the protympanum [18].
After all, the advantages transcanal EES turned out to have are many, namely, the preservation of the mastoid cavity and its function, the conservation of the ossicular chain and the non-pathological mucosa, the magnification and possibility to work in the blind recesses of the middle ear avoiding any residual disease and the restoration of the ventilation pathways, thus preventing recurrence [19, 20]. In particular, the application of the endoscope in cholesteatoma surgery showed an advantage over microscopic exclusive surgery, especially regarding residual rate. Badr-El-Dine claimed that in primary surgery after a complete microscopic procedure, the overall incidence of intraoperative residuals, detected through the endoscope, for both canal wall up and canal wall down techniques, was a significant 22.8% [8]. In 2017, Panetti et al. compared the endoscopic-assisted surgical procedure to the microscopic one to treat cholesteatoma and they noticed a lower residual rate when the endoscope was employed (16.1% before the introduction of the endoscope and 5.6% in the period after that) [21].
From the Middle Ear to the Lateral Skull Base
A further advancement in the endoscopic transcanal technique was introduced by our Italian school which codified the endoscopic transcanal approach to the inner ear, specifically the transcanal transpromontorial route that enables the surgeon to remove intralabyrinthine and intracanalicular vestibular schwannomas in selected patients with a sensorineural hearing loss, the first case being successfully performed in 2013 [22]. This minimally invasive procedure avoids extended transtemporal approaches and the manipulation of the posterior and medial cranial fossa dura.
Relevant contributions to the spreading of the transcanal transpromontorial approach for vestibular schwannomas were given by Moon et al. [23•] and by the American working groups of Rivas and Isaacson [24], who adopted and further investigated this technique in their institutions.
In 2015, in addition to the previously mentioned transpromontorial route, also the transcanal suprageniculate and infracochlear corridors were codified by the present author, to effectively remove a pathological process involving the fundus of the internal auditory canal, the cochlea, the petrous apex and the geniculate ganglion region, with lower complication rates and less invasive procedures compared to traditional microscopic approaches [25].
Endoscopic-Assisted Cochlear Implantation
A further recent application of the endoscope in ear surgery is during cochlear implantation in association to a traditional microscopic retroauricular procedure [26]. An additional transcanal endoscopic approach to the tympanic cavity allows for a good exposure of the anatomical structures and the round window and it offers the possibility to perform an endoscopic cochleostomy through the round window membrane or, if the round window is not accessible, a promontorial cochleostomy. Possible indications for this kind of approach are an anomalous course of the facial nerve, malformations of the inner ear, an ossified cochlea [27], a high jugular bulb that prevents explorative tympanotomy and a sclerotic mastoid. In the opinion of the authors, endoscopic-assisted surgery allows for the extension of the indications for cochlear implantation and reduces the morbidity associated with this surgical procedure.
The Modern Equipment for EES
Nowadays the essential tools needed for this type of surgery include a rigid endoscope, a light source, an HD3-CCD camera and a video monitor [28]. The most widely used endoscopes are the 0°, the angled 30° and 45° ones, their diameter can be 2.7 or 3 or 4 mm and the most common working lengths can be 11 cm, 14 cm and 18 cm. According to the surgeon’s inclination, the light source can be halogen, LED or xenon based. A HD3-CCD camera allows for a sharp, 1080p and clear video picture with appropriate colour rendering; suitable professional video monitors should be employed to fully exploit the quality produced by the camera.
Alongside the technical advancement of the endoscope, new powered devices have been introduced as better means to work in restricted surgical spaces with a one-handed technique. For instance, ultrasonic devices like Piezosurgery (Mectron) and Sonopet (Stryker) allow for bone removal avoiding damage to the tympanomeatal flap and other soft tissues, as proven by Kakehata et al. in the transcanal endoscopic approach to the antrum for cholesteatoma surgery [29].
Future Technical Perspectives
Since one of the main benefits of EES is the better surgical view, thanks to a higher magnification and a wider angle, the advances in optical technology and image processing are the first advancements to be expected in this surgical field. 4K technology, that is gaining momentum in the ORs, increases the magnification, providing a more detailed view of both anatomical and pathological structures [30•].
In addition to 4K resolution, filters to highlight hypervascularity, like narrow band imaging (NBI) used in oncologic surgery [31] could be used in the otologic field to recognize the avascular nature of cholesteatoma and tympanosclerosis and to identify the hypervascular structures such as the granulation tissue, preventing a small residual disease from being left behind during surgery.
Despite these visual technical improvements, one of the most well-known drawbacks of EES is the 2-dimensional image it provides and the subsequent lack of depth. With the recent release of a 4-mm (0° or 30°) high-definition 3D endoscope, this disadvantage can be overcome, providing a benefit both for beginners and experienced surgeons [32]. However, no less than 4-mm diameter 3D endoscope is available, which makes the management of a narrow ear canal impossible, and the sole digital zoom capability somewhat limits the picture sharpness.
Another disadvantage underlined by EES opponents is the one-handed nature of the endoscopic procedures, which requires a long training time and limits the approach when bleeding is extensive. Endoscope holders have been designed with this problem in mind; they facilitate and allow two-handed surgery allowing for more delicate dissections and constant suctioning if needed for a blood-free field [33]. Nevertheless, some technical issues remain especially due to the three tools in the narrow ear canal and the time-consuming management of the endoscope in and out of the field when cleansing is necessary. Moreover, the heat generated by a static endoscope could damage the structures and an abrupt head movement of the patient might cause iatrogenic injury.
A new viable alternative to surgical microscopes and endoscopes for otologic and neurotologic surgery is the 3D-exoscope system which combines the features of both, while avoiding some of the limitations [34•]. This new system is outside the body surface like a microscope, but while the latter has a large frame and a fixed cumbersome design, which forces the surgeons to have static positions and limited visual angles, the exoscope provides better ergonomics and an excellent visualization at extreme angles because the surgeon no longer relies on an eyepiece but works using 3D-monitors. In comparison to the endoscope, which also allows for a comfortable working position and to operate looking at a monitor, the exoscope enables the surgeon to work with two hands and offers a stereoscopic visualization. The main drawbacks of exoscopic surgery are its low illumination in narrow surgical corridors and its still lower image quality if compared to the microscope [35•], in addition, adequate training in both endoscopic and microscopic surgery is recommended, since skills in both techniques are necessary. The current author (D.M.) described the largest case series of lateral skull base diseases treated using exclusively the exoscope, proving the feasibility of the technique and the value of the device [34•]. The possibility to use the exoscope as the sole viewing device was also analysed by Wanna et al. [36•] and by Lee et al. (35•), who significantly added to the body of evidence supporting this instrument in the treatment of lateral skull base lesions.
Conclusions
Over the course of 30 years, the endoscope has proved to be an efficient tool both for diagnostic purposes and for the treatment of otologic and neurotologic pathological processes, in combination with the microscope for the management of possible residual disease as well as the main workhorse of the otologic surgeon.
Among others, a valid contribution was given by the Italian school of Marchioni and Presutti who in particular provided the endoscopic description of the anatomy of the retrotympanum and the ventilation pathways of the middle ear with important consequences on the surgical procedures. Moreover, they extended their knowledge to the lateral skull base, with the illustration of totally endoscopic transcanal approaches and the use of the endoscope as an additional tool in many surgical procedures to the skull base.
Thanks to the IWGEES endoscope-based surgery has considerably spread, three World Congresses on Endoscopic Ear Surgery took place due to the contribution of the working groups of Dubai, Modena and Boston, with the routine adoption of this technique by more and more young surgeons.
Given that a few limitations to endoscopic surgery still remain, we hope for some technological advancements like the production of yet smaller and more versatile endoscopes, which could automatically change their viewing angle, coupled with cameras that provide an increasingly better image quality and a stereoscopic vision. Finally, the one-handed nature of the endoscopic approaches could be overcome with the introduction of less invasive and more flexible and manageable robotic holders.
We believe that the knowledge of both the operative microscope, the endoscope and any other incoming established surgical viewing tool, should be the basis of the surgical expertise of future otologists so that they will be able to choose the proper instrument according to the patient’s needs.
a Some of the founders and developers of the endoscopic ear surgery, above from left Mohamed Badr-El-Dine, Joao Flavio Nogueira, Seiji Kakehata, below from left Daniele Marchioni, Livio Presutti, Muaaz Tarabichi at the 2012 Nagasaki international cholesteatoma meeting, where Daniele Marchioni performed the first endoscopic dissection of the middle and inner ear. b Daniele Marchioni along with Livio Presutti during an endoscopic dissection
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Tarabichi M, Arsiwala Z. History of endoscopic ear surgery. Otolaryngol Clin North Am. 2021;54(1):1–9. This paper outlines the history of endoscopy from point of view of the first surgeon to employ the endoscope as the sole surgical tool for ear procedures.
Linstrom CJ, Silverman CA, Rosen A, Meiteles LZ. Eustachian tube endoscopy in patients with chronic ear disease: The Laryngoscope. 2000;110(11):1884–9.
Marchioni D, Alicandri-Ciufelli M, Molteni G, Artioli FL, Genovese E, Presutti L. Selective epitympanic dysventilation syndrome. The Laryngoscope. 2010;NA-NA.
Poe DS, Rebeiz EE, Pankratov MM. Evaluation of perilymphatic fistulas by middle ear endoscopy. Am J Otol. 1992;13(6):529–33.
Takahashi H, Honjo I, Fujita A, Kurata K. Transtympanic endoscopic findings in patients with otitis media with effusion. Arch Otolaryngol - Head Neck Surg. 1990;116(10):1186–9.
Thomassin JM, Inedjian JM, Rud C, Conciatori J, Vilcoq P. Otoendoscopy: application in the middle ear surgery. Rev Laryngol - Otol - Rhinol. 1990;111(5):475–7.
McKennan KX. Endoscopic ‘second look’ mastoidoscopy to rule out residual epitympanic/mastoid cholesteatoma: The Laryngoscope. 1993;103(7):810???814.
Badr-el-Dine M. Value of ear endoscopy in cholesteatoma surgery: Otol Neurotol. 2002;23(5):631–5.
Ayache S, Tramier B, Strunski V. Otoendoscopy in cholesteatoma surgery of the middle ear: what benefits can be expected? Otol Neurotol. 2008;29(8):1085–90.
El-Guindy A. Endoscopic transcanal myringoplasty. J Laryngol Otol. 1992;106(6):493–5.
Tarabichi M. Endoscopic management of acquired cholesteatoma. Am J Otol. 1997;18(5):544–9.
Tarabichi M. Endoscopic middle ear surgery. Ann Otol Rhinol Laryngol. 1999;108(1):39–46.
Marchioni D, Mattioli F, Alicandri-Ciufelli M, Presutti L. Transcanal endoscopic approach to the sinus tympani: a clinical report. Otol Neurotol. 2009;30(6):758–65.
Marchioni D, Alicandri-Ciufelli M, Grammatica A, Mattioli F, Presutti L. Pyramidal eminence and subpyramidal space: an endoscopic anatomical study: pyramidal eminence and subpyramidal space. Laryngoscope. 2010;120(3):557–64.
Marchioni D, Alicandri-Ciufelli M, Piccinini A, Genovese E, Presutti L. Inferior retrotympanum revisited: an endoscopic anatomic study: inferior retrotympanum revisited. Laryngoscope. 2010;120(9):1880–6.
Marchioni D, Mattioli F, Alicandri-Ciufelli M, Molteni G, Masoni F, Presutti L. Endoscopic evaluation of middle ear ventilation route blockage. Am J Otolaryngol. 2010;31(6):453–66.
Marchioni D, Mattioli F, Alicandri-Ciufelli M, Presutti L. Prevalence of ventilation blockages in patients affected by attic pathology: a case-control study: ventilation blockages in attic pathology. Laryngoscope. 2013;123(11):2845–53.
Jufas N, Marchioni D, Tarabichi M, Patel N. Endoscopic anatomy of the protympanum. Otolaryngol Clin North Am. 2016;49(5):1107–19.
Alicandri-Ciufelli M, Marchioni D, Kakehata S, Presutti L, Villari D. Endoscopic management of attic cholesteatoma. Otolaryngol Clin North Am. 2016;49(5):1265–70.
Presutti L, Anschuetz L, Rubini A, Ruberto M, Alicandri-Ciufelli M, Dematte M, et al. The impact of the transcanal endoscopic approach and mastoid preservation on recurrence of primary acquired attic cholesteatoma. Otol Neurotol. 2018;39(4):445–50.
Panetti G, Cavaliere M, Panetti M, Marino A, Iemma M. Endoscopic tympanoplasty in the treatment of chronic otitis media: our experience. Acta Otolaryngol (Stockh). 2017;137(3):225–8.
Presutti L, Alicandri-Ciufelli M, Cigarini E, Marchioni D. Cochlear schwannoma removed through the external auditory canal by a transcanal exclusive endoscopic technique: CS removed through the EAC by a transcanal approach. Laryngoscope. 2013;123(11):2862–7.
• Moon I, Cha D, Nam SI, Lee HJ, Choi J. The feasibility of a modified exclusive endoscopic transcanal transpromontorial approach for vestibular schwannomas. J Neurol Surg Part B Skull Base. 2019;80(01):082–7. This paper provides further and relevant insight on a minimally invasive transcanal exclusive endoscopic technique for lateral skull base surgery.
Wick CC, Arnaoutakis D, Barnett SL, Rivas A, Isaacson B. Endoscopic transcanal transpromontorial approach for vestibular schwannoma resection: a case series. Otol Neurotol. 2017;38(10):e490–4.
Marchioni D, Alicandri-Ciufelli M, Rubini A, Presutti L. Endoscopic transcanal corridors to the lateral skull base: initial experiences: transcanal corridors to lateral skull base. Laryngoscope. 2015;125:S1-13.
Marchioni D, Soloperto D, Guarnaccia MC, Genovese E, Alicandri-Ciufelli M, Presutti L. Endoscopic assisted cochlear implants in ear malformations. Eur Arch Otorhinolaryngol. 2015;272(10):2643–52.
Marchioni D, Soloperto D, Bianconi L, Guarnaccia MC, Genovese E, Presutti L. Endoscopic approach for cochlear implantation in advanced otosclerosis: a case report. Auris Nasus Larynx. 2016;43(5):584–90.
Kozin ED, Lee DJ. Basic principles of endoscopic ear surgery. Oper Tech Otolaryngol-Head Neck Surg. 2017;28(1):2–10.
Kakehata S, Watanabe T, Ito T, Kubota T, Furukawa T. Extension of indications for transcanal endoscopic ear surgery using an ultrasonic bone curette for cholesteatomas. Otol Neurotol. 2014;35(1):101–7.
• Nogueira JF, de Sousa Lobo Ferreira Querido R, Gonçalves da Silva Leite J, Cabral da Costa T. Future of endoscopic ear surgery. Otolaryngol Clin North Am. 2021 Feb;54(1):221–31. The experienced ear surgeon and his colleagues try to outline the state of the art and envisage the future technological advancements of endoscopic ear surgery.
Plaat BEC, Zwakenberg MA, van Zwol JG, Wedman J, van der Laan BFAM, Halmos GB, et al. Narrow-band imaging in transoral laser surgery for early glottic cancer in relation to clinical outcome. Head Neck. 2017;39(7):1343–8.
Bernardeschi D, Lahlou G, De Seta D, Russo FY, Mosnier I, Sterkers O. 3D endoscopic ear surgery: a clinical pilot study. Eur Arch Otorhinolaryngol. 2018;275(2):379–84.
Khan MM, Parab SR. Endoscopic cartilage tympanoplasty: a two-handed technique using an endoscope holder: two-handed endoscopic tympanoplasty. Laryngoscope. 2016;126(8):1893–8.
• Rubini A, Di Gioia S, Marchioni D. 3D exoscopic surgery of lateral skull base. Eur Arch Otorhinolaryngol. 2020;277(3):687–94. This paper reports one of the earliest and largest case series regarding the use of the exoscope for otological and neurotological procedures.
• Smith S, Kozin ED, Kanumuri VV, Barber SR, Backous D, Flávio Nogueira J, et al. Initial experience with 3-dimensional exoscope-assisted transmastoid and lateral skull base surgery. Otolaryngol Neck Surg. 2019;160(2):364–7. This paper reports one of the first experiences regarding the use of the exoscope for otological and lateral skull base procedures.
• Garneau JC, Laitman BM, Cosetti MK, Hadjipanayis C, Wanna G. The use of the exoscope in lateral skull base surgery: advantages and limitations. Otol Neurotol. 2019;40(2):236–40. This paper reports one of the first experiences regarding the use of the exoscope for lateral skull base procedures.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on OTOLOGY: Advances in Otology.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bonali, M., Marchioni, D. & Bisi, N. Endoscopic Ear Surgery: Past and Future. Curr Otorhinolaryngol Rep 10, 343–348 (2022). https://doi.org/10.1007/s40136-022-00424-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40136-022-00424-3