Abstract
Purpose of Review
This review was conducted to gain insight into the history, present and future of bariatric and/or metabolic surgery and endoscopic treatments of obesity. The challenges that have been overcome, the challenges we still face and our recommendations for the future are discussed.
Recent Findings
Over the last few decades, a number of treatment strategies have emerged for the treatment of obesity. Both endoscopic and surgical options are available and they lead to significant weight loss and comorbidity reduction. However, to remain a credible treatment alternative to the obesity pandemic, we need to perform these procedures in much larger numbers than we currently do. Even though significant gains have been made in reducing the morbidity and mortality of surgical interventions, there is further room for improvement, especially when it comes to long-term issues. Due to its impact on almost every single organ system in the human body, bariatric surgery has attracted the attention of academics from a variety of medical disciplines. This has led to a rapidly enlarging body of high-quality scientific literature, supporting its wider use and cost-effectiveness.
Conclusion
Despite the advances made in bariatric surgery, the criteria determining suitability of patients for bariatric surgery in most parts of the world are still based on a consensus agreed upon in the USA in 1991. There is a need to formulate some new consensus and guidelines that would allow for a significant expansion of the pool of patients that can be offered these procedures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is hard to define when bariatric or metabolic surgery was practiced for the very first time. In a way, it has been around for over 80 years, ever since the subtotal gastrectomy, vagotomy with or without antrectomy, or pylorotomies were performed to surgically treat peptic ulcer disease. These procedures were not intended to induce weight loss but were associated with weight loss and co-morbidity reduction [1].
Perhaps the intention to surgically treat a patient for obesity might best give an indication as to the true historical start of bariatric surgery. R.L. Varco, a surgeon at the University of Minnesota performed an end-to-end jejunoileostomy with a separate ileocecostomy for drainage of the bypassed segment in 1953. Their landmark article described the first hypoabsorptive procedure [2, 3]. In the following decades, many other procedures were developed but these procedures were not performed in large numbers, this was perhaps due to open surgery on patients suffering from severe obesity was not without its risks. It is also true that the global burden of disease was considerably less at the time and obesity had not caught the popular imagination as it has now. This may explain why bariatric surgery was slow to take off. It is probably due to a dramatic improvement in its safety and excellent outcomes in terms of weight loss and comorbidity that bariatric and metabolic surgery is now performed in very large numbers worldwide, with an estimated 700,000 surgeries being performed in 2016 alone [4].
When Pinchiera, Price and Mason published their article ‘Effect of bariatric surgery on erythromycin absorption’ in 1981 they might not have realised that it was probably the first with ‘bariatric surgery’ in its title [5]. Several years prior, in 1972, HW. Scott had already used the currently more common term ‘metabolic surgery’ to describe the effects of the ileal bypass on hypercholesterolaemia and arteriosclerosis [6]. This term was hardly used in the decades after it was published until it was picked up again in recent years. Slowly but steadily, in the same period, a number of different procedures developed that were initially categorised into three groups based on their supposed working mechanisms: restrictive, malabsorptive and combined malabsorptive-restrictive procedures. This categorisation of bariatric and metabolic procedure is however increasingly being challenged [7].
Stomach-Based Procedures
A number of bariatric procedures were developed with the original intention of creating a physical reduction of the gastric capacity but it later became apparent that the significant reduction in calorie intake seen with these procedures was probably mediated through as of yet, incompletely understood neuro-hormonal mechanisms, rather than the physical reduction of the available stomach size [8]. This is an important distinction to make, not just for the development of better surgical procedures in the future but eventually for durable non-surgical therapies for the treatment of obesity and its associated metabolic disorders.
Stomach-based procedures have the advantage of inducing weight loss without altering the normal passage of food through the intestinal tract. Mason and Printen were probably the first to publish a stomach-based technique called the horizontal gastroplasty in 1971 (Figs. 1 and 2). This technique divided the stomach into a small upper pouch and a lower larger pouch connected by a narrow passage along the greater curvature of the stomach. The weight loss, however, was unsatisfactory with this procedure, probably due to the dilatation of the pouch [2, 9]. Thereafter, Long et al. introduced the oblique gastroplasty using the thicker wall of the lesser curvature (Fig. 3) [2, 10]. Subsequently, Mason developed the vertical banded gastroplasty (VBG). In this procedure, a lesser curvature-based pouch is created in which the narrow passage is reinforced with a prosthetic (Marlex, Dacron) band (Fig. 4) [2, 11]. This procedure became quite popular and was performed for over 20 years. It then fell out of favour due to a large number of staple line disruptions and strictures which required surgical intervention [2, 12, 13].
Tretbar used a fundoplication technique in 1976 and sewed the fundus around the stomach to reduce its size [2, 14]. The introduction of a Marlex mesh and Dacron graft by Wilkinson and Molina in 1980 cleared the way for the use of the gastric bands (Fig. 5) [2, 15]. Kuzmak used the first adjustable gastric band (AGB) by inserting an inflatable silastic band connected to a subcutaneous port that was used to increase or decrease the diameter of the band in 1986 (Fig. 6) [16]. After the introduction of the laparoscopically placed AGB by Cantona in 1993, gastric bands were increasingly utilised for the treatment of morbid obesity especially after the FDA approval in the USA [4, 17]. Unfortunately, due to disappointing long-term results and high rates of removal, the number of patients who receive a gastric band rapidly decreased [4, 18, 19]. The most commonly performed bariatric procedure worldwide currently is the laparoscopic gastric sleeve (LSG), in which the majority of the stomach is resected leaving behind a narrow sleeve of the stomach. Its first variant was described by Marceau et al. in 1993 (Fig. 7), forming the restrictive part of a biliopancreatic diversion with a duodenal switch (BPD-DS) [20]. Nowadays, it is used as a standalone procedure with excellent medium-term results for weight loss and comorbidity reduction [21, 22].
Hind Gut-Based Procedures
An array of bariatric procedures has been developed over the years where a majority of the small bowel is bypassed. Even though they were previously labelled as malabsorptive (or hypoabsorptive) [23], it is not entirely clear if malabsorption is the main mechanism through which these procedures work while there also seems to be a role for certain gut hormones like PYY and GLP-1 [24, 25].
The first of such procedures was probably performed by Varco—a jejuno-ileal bypass (Fig. 8). This procedure and all its variations resulted in significant weight loss. However, it also led to an unacceptably high rate of malabsorptive complications [2]. The idea found support from Scopinaro many years later, who developed a biliopancreatic diversion in 1979 [2, 26, 27]. The idea was not to exclude any segment of the gut from the intestinal flow. A partial gastrectomy is performed in which the duodenal stump is closed. Then the jejunum is divided at 250 cm from the ileocecal valve. The distal part (Roux-limb) is anastomosed to the stomach and the proximal portion is connected to the ileum, 50 cm proximal to the ileocecal valve (Fig. 9) [26, 27]. The percentage of excess weight loss (%EWL) is a common measure of reporting weight loss after surgery. It is the percentage of overweight kilo’s lost using an ideal BMI of 25 kg/m2. This procedure results in a mean %EWL of 75% in the long term, but is also associated with complications such as diarrhoea, metabolic disorders and dumping syndrome, which often significantly impair the quality of life of the patient [28]. An adapted version of the original BPD procedure is still in use but accounts for a relatively miniscule proportion of the procedures worldwide [4].
The BPD-DS has been previously mentioned and it basically consists of a sleeve gastrectomy combined with a BPD-like distal bypass procedure of the small intestine. In 1986, Hess revised this procedure into its final form by preserving the pyloric sphincter, hereby reducing the incidence of stomal ulcers and dumping syndrome (Fig. 10) [2, 29]. As with the BPD, this procedure is not commonly used as a primary bariatric procedure [4].
More recently in 2010, Sanchez-Pernote and Torres published their experience with single anastomosis duodenal-ileal bypass with gastric sleeve (SADI-S) (Fig. 11) [30]. In this procedure, a sleeve gastrectomy is combined with an anastomosis of a loop of ileum, 250 cm proximal to the ileo-caecal junction to the first part of duodenum. Anastomosis of the small bowel with duodenum makes this procedure technically more challenging but it is emerging as one of the acceptable options after sleeve gastrectomy especially because it replicates the effect of the duodenal switch while simultaneously obviating the need for a second anastomosis [30, 31].
Stomach and Proximal Gut-Based Procedures
Another major category of bariatric procedures involves a significant reduction in available gastric capacity in conjunction with the bypass of a section of the proximal small intestine. They are loosely labelled as gastric bypass procedures. The first gastric bypass was first performed in 1966 by Mason and Ito. They divided the stomach horizontally to create a pouch on which a loop of the jejunum was placed [28, 29]. An important alteration was made to this procedure by Griffin et al. in 1977, who described the Roux-en-Y configuration instead of the loop. It reduced complications like bile reflux (Fig. 12) [32]. The procedure became very popular after the first laparoscopic Roux-en-Y gastric bypass (RYGB) was performed in 1994 by Wittgrove and Clarke [33].
The Roux-en-Y gastric bypass (RYGB) is now the second most common bariatric procedure in the world, having been replaced by the SG as the most common procedure in recent years [4]. Despite malabsorption being deemed to play a significant role behind this procedure in the past, it is now becoming clearer that malabsorption makes a very small contribution to the total calorie deficit after a RYGB in the short term and probably even less in the long term [34].
Rutledge published his first results in 2001 of a modified gastric bypass that he called the ‘mini-gastric bypass’ which involved the creation of a long and narrow gastric pouch that was anastomosed to a loop of proximal jejunum. Although the initial description of this procedure suggested a biliopancreatic limb of 200, more recently, the recommendation is to avoid using a biliopancreatic limb of longer than 150 for this procedure to reduce the rates of protein and calorie malnutrition requiring reoperation [35•, 36] (Fig. 13). The International Federation for Surgery of Obesity and Metabolic Diseases (IFSO) has now approved this procedure but recommended that the identified one anastomosis gastric bypass (OAGB) be used for it as the name ‘Mini’ may not reflect the true severity of this major bariatric procedure [37]. This procedure is rapidly becoming very popular and has now become the third most common primary bariatric procedure [4].
The Road to Improvement
Metabolic surgery has been challenged many times in the past by non-surgical treatments. Currently, none of these have proven to be superior or even equal to it in efficacy, especially in the long term. Some of these treatments have, however, shown promising results and have gained wide interest among healthcare providers and patients. One might argue, why look any further when a potent and cost-effective remedy like metabolic surgery to treat obesity and its related comorbidities is already available. Our quest for relatively less invasive options is likely to continue.
The benefits of bariatric surgery obviously come with risks. The surgery can be associated with significant morbidity and even mortality. Although the 30-day mortality with bariatric procedures has come down to 0.1–0.2% due to less complex procedures, operating techniques, patient care and advances in anaesthesia, surgery can still be associated with significant long-term morbidity and even mortality [38]. Some of the complications that patients can explain in the long term are gastro-oesophageal reflux disease, marginal ulcers, gall stones, dumping and nutritional issues.
Even though some procedures like RYGB or OAGB can technically be reversed, reversal can be challenging and certain others procedures like sleeve gastrectomy cannot be reversed. Gastric band is probably the only completely reversible bariatric procedure. Bariatric surgery should, therefore, be largely regarded as a permanent alteration to the gastrointestinal tract. Reversal, when possible, should be reserved for management of complications as it is inevitably associated with recurrence of obesity and its associated co-morbidities. Conversion to a different procedure is far more common and recommended whenever possible.
For any new treatment strategy to be successfully implemented for treatment of large numbers of patients suffering from obesity, it has to deliver sustained weight loss, be cost-efficient, have few complications, mortality no greater than non-operative treatment, be easily available, and accepted by both patients and healthcare professionals. There is no such alternative to bariatric surgery on the horizon.
Endoscopic Metabolic Procedures
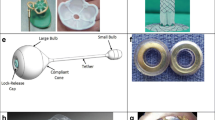
A number of endoscopic treatments have emerged over the last decades for the treatment of obesity and its associated co-morbidities. Perhaps, the best know endoscopic procedure is the gastric balloon (Fig. 14) which has the advantage of leading to a total body weight loss (TWL) up from 7 to 15% after 6 months and comes with a low morbidity and mortality risk. Introduced for the first time in 1985, we now have a number of balloon types, either filled with gas or liquid. This all probably lead to weight loss through both enhanced satiety and alteration of gut hormones [39,40,41]. Unfortunately, they have to be implanted and removed endoscopically and often do not result in long-term sustainable results. It remains to be seen if the recently introduced (non-endoscopic) swallowable gastric balloons that can be placed every 6 months will be more successful [42].
The technique that perhaps comes closest to metabolic surgery is endoscopic sleeve gastroplasty (Fig. 15), where the greater curvature is endoscopically (partially) inverted and functionally excluded. Using transgastric stitches, it decreases gastric capacity up to 70%. It also leads to better TWL compared to the gastric balloon with up to 19% TWL at 2 years and significantly reduced comorbidities. The downside is that is also comes with higher complication rates and long-term results are scarce [39, 43, 44].
Another promising endoscopic intervention is AspireAssist (Aspire Bariatrics, King of Prussia, PA, USA) (Fig. 16) [39, 45, 46]. Here, a catheter is placed into the stomach and after a meal, water is flushed through this catheter into the stomach and is aspirated afterwards, when the water has mixed with the gastric content. There is a lack of published data but with up to 12% of TWL [39], the technique can be regarded as promising. The disadvantages of this technique are its complications, the fact that the catheter remains in place and thus remains visible, and it requires time and effort to flush and aspirate.
Other endoscopic treatment options target the small intestine, especially the neuroendocrinologically important duodenum and proximal jejunum to treat obesity and type 2 diabetes mellitus (T2DM). A technique that showed promise is the duodenojejunal bypass liner or Endobarrier (GI dynamics, Lexington, MA, USA) (Fig. 17) [47•, 48, 49] which is placed post-pyloric and results in altered gut hormones and increased satiety. It showed good results with T2DM remission and %TWL of up to 10%. [39, 49] It unfortunately also showed high preliminary removals, and results did not seem durable [49, 50]. Targeting the neuroendocrine functions of the duodenum to treat T2DM, NAFLD and NASH can also be achieved by thermal ablation. Endoscopic duodenal mucosal resurfacing performed using the Revita system (Fractyl Laboratories, Cambridge, MA, USA) showed good HbA1C% reduction within the first week after treatment. But there is no medium and long-term data on weight loss [39].
Using magnets to form an anastomosis is not new, but was recently introduced for obesity treatment (Incisionless Anastomosis System (IAS) and the Incisionless Magnetic Anastomosis System (IMAS) (GI Windows, West Bridgewater, MA, USA), Magnamosis (Magnamosis Inc., San Francisco, California, USA) (Fig. 18). These magnets can be used to create a gastro-jejunostomy, or jejuno-ileostomy, bypassing nutrients and resulting in weight loss. Only small studies have been performed so far, but in our opinion, the gastro-jejunostomy in particular shows great promise as obesity and T2DM treatment while it is technically the least challenging option [39]. Theoretically, however, internal herniations might occur as we also see in gastric bypass surgery.
Table 1 shows a chronological overview of all procedures described in this article and whether they are still used nowadays.
Improving Outcomes of Bariatric Surgery
Metabolic surgery is not without risks, but in recent years, much has changed. Mortality rates have dropped significantly from up to 4% in 2002 to 0.6% in 2009 and 0.1% in 2017 in large American cohorts of patients [38]. In a report combining the outcomes of all Swedish and Dutch bariatric patients who were operated on in 2015 and 2016, mortality was even as low as 0.04% [51]. The possible risk factors for increased in-hospital mortality that has previously recorded in literature are amongst others: age, hypertension, T2DM, previous myocardial infarction, patients with increased embolism risk, BMI ≥ 50 kg/m2, male gender, operation type and open surgery [38, 51].
Health status can, however, be improved perioperatively. Perhaps the biggest contributor to improved care is the implementation of multidisciplinary teams in many bariatric clinics that not only look at things from a surgeon’s point of view but also clear the road for other specialists. Endocrine, cardiac and pulmonary evaluations might not be beneficiary for all patients, but for patients with such a specific history or complaints, it might lead to better perioperative care.
Anaesthesiologists also have a key role in preventing complications. With the current, improved understanding of the perioperative risks in obese patients with metabolic disease, anaesthesiologists are better equipped to filter out high-risk patients. The introduction of a selective relaxing binding agent (Sugammadex™) standardized neuromuscular blocks which lead to better operative views, a lowered use of opioids and less perioperative complications [52, 53]. Perhaps, the introduction of the enhanced recovery after bariatric surgery (ERABS) did not only improve efficiency but also reduced the amount of complications [54, 55]. For example, with better and faster mobilisation combined with preventive low molecular weight heparins, the risks for pulmonary embolisms reduce. Pulmonary instruction and intensified analgesia might lead to less postoperative pneumonia’s [56, 57].
The biggest revolution in the bariatric surgery itself is that it has transformed from an open to a laparoscopic procedure. With vastly improved views, operating times have declined significantly and with it, the perioperative risks.
There is however still room for improvement. Even though average complications and mortality rates are low, experienced high-volume centres have better outcomes. Increasing volumes might reduce these figures even further, but proper training is essential. It is widely known that the learning curves of surgeons and surgical residents trained by experienced bariatric teams are relatively short [58]. This kind of training should perhaps become mandatory for all surgeons performing bariatric surgery [59•].
The Future of Bariatric Surgery
Bariatric surgery is still a relatively new speciality, but since 2015, over a thousand articles per year are published on bariatric or metabolic surgery. To put this into perspective, in 2000, only 54 articles were published on the subject [60]. These articles are important to be able to evaluate treatments, develop new strategies and improve existing guidelines. It is this research that showed that bariatric surgery not only results in weight loss, but many related comorbidities are being resolved as well. To emphasize these effects and indirectly to increase acceptance of weight loss surgery, large scientific societies started to incorporate the word ‘metabolic’ into their names. An example is the American Society For Bariatric Surgery (ASBS) that changed their name to the American Society For Metabolic and Bariatric Surgery (ASMBS) in 2007. The IFSO did not change their abbreviation, but also added ‘and Metabolic’.
Randomized controlled trials (RCT) deliver some of the best evidence required to prove that new strategies or treatments give better outcomes compared to a gold standard or control group. However, one must realize that performing these trials in surgery patients is difficult and often proves impossible. All the challenges combined in surgery studies have led to the relatively small number of RCTs performed in bariatric surgery. This has resulted in the gross number of surgical trials that only describe the outcome of one type of procedure performed for the same indication. In 2018, Ozsoy and Demir showed for example, that the article ‘Outcomes after laparoscopic Roux-en-Y gastric bypass for morbid obesity’ by Schauer et al. was still the most cited article in bariatric surgery with over 750 citations [60]. Although these kinds of studies are valuable, they are often only offered for publication when the outcomes are positive. Because of the many differences in setups, length of follow up, measurements taken and patient populations, it becomes hard to compare the outcomes between studies. It must be said, however, that although RCTs are of great value, often in surgery, large prospective trials and databases are also of great value. These often better represent the actual clinical outcomes of surgical interventions compared to the outcomes of those in a well-organized and ideal setting found in RCTs.
Attempts have been made to change the most common guideline for bariatric surgery, but unfortunately, the gross majority of patients who consider metabolic surgery are still confronted with the NIH criteria published in 1991 [61]. These inclusion criteria are based on age (18–65 years of age), body mass index (BMI > 40) of BMI combined with comorbidity (BMI ≥35 kg/m2 and a related comorbidity) and patient readiness to change their lifestyle. Perhaps the latter is a soft criterium, but the first two are often too strict.
Conclusion
The change of the name bariatric surgery to metabolic surgery in recent years is not purely symbolic. It emphasises what is treated with our weight loss procedures: the comorbidities and not obesity per se. So, perhaps weight or BMI might still be used to select patients undergoing bariatric surgery, but new guidelines are eminent and should primarily focus on comorbidity reduction. In this context, the NIH criteria have to be reconsidered and we suggest organising a consensus conference to expand these criteria involving all stakeholders—for example surgeons, obesity experts, patients and funders, to improve care and reshape obesity treatment.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Buchwald H. Metabolic surgery: a brief history and perspective. Surg Obes Relat Dis. 2010;6:221–2.
Saber AA, Elgamal MH, McLeod MK. Bariatric surgery: the past, present and future. Obes Surg. 2008;18:121–8.
Martin LF. The evolution of surgery for morbid obesity. (2004). Obes Surg, 2004; 14:15–47.
Angrisani L, Santonicola A, Iovino P, Vitiello A, Higa K, Himpens J, et al. IFSO Worldwide Survey 2016: Primary, endoluminal, and revisional procedures. Obesity Sugery. 2018;28:3783–94.
Pinchiera JC, Prince RA, Mason EE. Effect of bariatric surgery on erythromycin absorption. Am J Hosp Pharm. 198(38):232.
Scott HW Jr. Metabolic surgery for hyperlipidemia and atherosclerosis. American Journal of Surg. 1972;123:3–12.
Mahawar K. Gastric bypass is not a “restrictive and malabsorptive” procedure. Obes Surg. 2016;26:2225–6.
Stefanidis A, Oldfield BJ. Neuroendocrine mechanisms underlying bariatric surgery: insights from human studies and animal models. J Neuroendocrinol. 2017;29(10).
Buchwald H, Rucker RD. The rise and fall of jejunoileal bypass. In: Nelson RL, Nyhus, editors. Surgery of the small intestine. Norwalk, CT: Appleton Century Crofts; 1987; 529–41.
Printen KJ, Mason EE. Gastric surgery for relief of morbid obesity. Arch Surg. 1973;106:428–31.
Long M, Collins JP. The technique and early results of high gastric reduction for obesity. Aust N Z J Surg. 1980;50:146–9.
Mason EE. Vertical banded gastroplasty for obesity. Arch Surg. 1982;11:701–6.
Mason EE, Cullen JJ. Management of complications in vertical banded gastroplasty. Curr Surg. 2003;60(1):33–7.
Salinas A, Santiago E, Yeguez J, et al. Silastic ring vertical gastric bypass: evolution of an open surgical technique, and review of 1,588 cases. Obes Surg 2005;15:1403–1407.
Tretbar LL, Taylor TL, Sifers EC. Weight reduction. Gastric plication for morbid obesity. J Kans Med Soc. 1976;77:488–90.
Kuzmak LI, Thelmo W, Abramson DL. Reversible adjustable gastric banding. Surgical technique. Eur J Surg. 1994;160:569–71.
Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2008. Obes Surg. 2009;19:1605–11.
Aarts EO, Dogan K, Koehestanie P, Aufenacker TJ, Janssen IMC, Berends FJ. Long term results after laparoscopic adjustable gastric banding: a mean fourteen year follow-up study. Surg Obes Relat Dis. 2014;24:1835–42.
Brown JJ, Boyle M, Mahawar K, Balupuri S, Small PK. Laparoscopic adjustable gastric band survival in a high-volume bariatric unit. Br J Surg. 2013;100:1614–8.
Marceau P, Biron S, Bourque RA, Potvin M, Hould FS, Simard S. Biliopancreatic diversion with a new type of gastrectomy. Obes Surg. 1993;3:29–35.
Langer FB, Bohdjalian A, Felberbauer FX, Fleischmann E, Reza Hoda M, Ludvik B, et al. Does gastric dilatation limit the success of sleeve gastrectomy as a sole operation for morbid obesity? Obes Surg. 2006;16:166–71.
Zhao H, Jiao L. Comparative analysis for the effect of Roux-en-Y gastric bypass vs sleeve gastrectomy in patients with morbid obesity: Evidence from 11 randomized clinical trials (meta-analysis). Int J Surg. 2019;72:216–23.
Gagner M. Hypoabsorption not malabsorption, hypoabsorptive surgery and not malabsorptive surgery. Obes Surg. 2016;26:2783–4.
Kral JG. Malabsorptive procedures in surgical treatment of morbid obesity. Gastroenterol Clin N Am. 1987;16:293–305.
Li W, Baraboi ED, Cluny NL, Roy MC, Samson P, Biertho L, et al. Malabsorption plays a major role in the effects of the biliopancreatic diversion with duodenal switch on energy metabolism in rats. Surg Obes Relat Dis. 2015;11:356–66.
Silecchia G, Boru C. Effectiveness of laparoscopic sleeve gastrectomy (first stage of biliopancreatic diversion with duodenal switch) on comorbidities in super-obese high-risk patients. Obes Surg. 2006;16:1138–44.
Scopinaro N, Gianetta E, Civalleri D, Bonalumi U, Bachi V Bilio-pancreatic bypass for obesity: II. Initial experience in man. Br J Surg 1979;66:618–620.
Scopinaro N, Gianetta E, Adami GF, Friedman D, Traverso E, Marinari GM, et al. Biliopancreatic diversion for obesity at eighteen years. Surgery. 1996;119:261–8.
Scopinaro N, Adami GF, Marinari GM, Gianetta E, Traverso E, Friedman D, et al. Biliopancreatic diversion. World J Surg. 1998;22:936–46.
Sánchez-Pernaute A, Herrera MA, Pérez-Aguirre ME, Talavera P, Cabrerizo L, Matía P, et al. Single anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S). One to three-year follow-up. Obes Surg. 2010;20:1720.
Martini F, Paolino L, Marzano E, D'Agostino J, Lazzati A, Schneck AS, et al. Single-anastomosis pylorus-preserving bariatric procedures: review of the literature. Obes Surg. 2016;26:2503–15.
Griffen WO Jr, Young VL, Stevenson CC. A prospective comparison of gastric and jejunoileal bypass procedures for morbid obesity. Ann Surg. 1977;186(4):500–9.
Wittgrove AC, Clark GW, Tremblay LJ. Laparoscopic gastric bypass, Roux-en-Y: preliminary report of five cases. Obes Surg. 1994;4:353–7.
Mahawar KK, Sharples AJ. Contribution of malabsorption to weight loss after Roux-en-Y gastric bypass: a systematic review. Obes Surg. 2017;8:2194–206.
• Mahawar KK, Parmar C, WRJ C, Jennings N, Schroeder N, Small PK. Impact of biliopancreatic limb length on severe protein-calorie malnutrition requiring revisional surgery after one anastomosis (mini) gastric bypass. J Minim Access Surg. 2018;14:37–43 This article clearly shows the downside of one of the hot topics of the moment; OAGB-MGB with a long biliopancreatic limb. Healthcare professionals should take care to prevent protein and micronutrient deficiencies with (too) long biliopancreatic limbs.
Boyle M, Mahawar K. One anastomosis gastric bypass performed with a 150-cm biliopancreatic limb delivers weight loss outcomes similar to those with a 200-cm biliopancreatic limb at 18–24 months. Obes Surg. 2019 [published online ahead of print].
De Luca M, Tie T, Ooi G, Higa K, Himpens J, Carbajo MA, et al. Mini gastric bypass-one anastomosis gastric bypass (MGB-OAGB)-IFSO position statement. Obes Surg. 2018;28:1188–206.
Foster MW, Gershuni VM, Tewksbury CM, Giri JS, Dumon KR, Rame JE, et al. Laparoscopic sleeve gastrectomy carries a lower perioperative mortality including sudden cardiac death over Roux-en-Y gastric bypass in patients with a prior cardiac history: an MBSAQIP analysis. Obes Surg. 2019 Dec;24 [Epub ahead of print].
Glass J, Chaudhry A, Zeeshan MS, Ramzan Z. New era: endoscopic treatment options in obesity–a paradigm shift. World J Gastroenterol. 2019;25:4567–79.
Ly HG, Dupont P, Van Laere K, Depoortere I, Tack J, Van Oudenhove L. Differential brain responses to gradual intragastric nutrient infusion and gastric balloon distension: a role for gut peptides? Neuroimage. 2017;144:101–12.
Bužga M, Evžen M, Pavel K, Tomáš K, Vladislava Z, Pavel Z, et al. Effects of the intragastric balloon MedSil on weight loss, fat tissue, lipid metabolism, and hormones involved in energy balance. Obes Surg. 2014;24:909–15.
Raftopoulos I, Giannakou A. The Elipse Balloon, a swallowable gastric balloon for weight loss not requiring sedation, anesthesia or endoscopy: a pilot study with 12-month outcomes. Surg Obes Relat Dis. 2017;13:1174–82.
Hedjoudje A, Abu Dayyeh BK, Cheskin LJ, Adam A, Neto MG, Badurdeen D, et al. Efficacy and safety of endoscopic sleeve gastroplasty: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2019;S1542-3565(19):30897–3.
Gys B, Plaeke P, Lamme B, Lafullarde T, Komen N, Beunis A, et al. Endoscopic gastric plication for morbid obesity: a systematic review and meta-analysis of published data over time. Obes Surg. 2019;29:3021–9.
Kumar N, Sullivan S, Thompson CC. The role of endoscopic therapy in obesity management: intragastric balloons and aspiration therapy. Diabetes Metab Syndr Obes. 2017;10:311–6.
Thompson CC, Abu Dayyeh BK, Kushner R, Sullivan S, Schorr AB, Amaro A, et al. Percutaneous gastrostomy device for the treatment of class II and class III obesity: results of a randomized controlled trial. Am J Gastroenterol. 2017;112:447–57.
• Betzel B, Cooiman MI, Aarts EO, Janssen IMC, Wahab PJ, Groenen MJM, et al. Clinical follow-up on weight loss, glycemic control, and safety aspects of 24 months of duodenal-jejunal bypass liner implantation. Surg Endosc. 2020;34:209–15 With many new techniques coming out to treat obesity, it is very important to look for the best risk-benefit ratios. Most often, the first results of new techniques are promising, very often there is hardly any follow-up published afterwards. This article is one of the few that shows disappointing medium term results of a device (Endobarrier) and reports on the downfalls and relapse of type two diabetes.
Betzel B, Homan J, Aarts EO, Janssen IMC, de Boer H, Wahab PJ, et al. Weight reduction and improvement in diabetes by the duodenal-jejunal bypass liner: a 198 patient cohort study. Surg Endosc. 2017;31:2881–91.
van Rijn S, Roebroek YGM, de Jonge C, Greve JWM, Bouvy ND. Effect of the EndoBarrier device: a 4-year follow-up of a multicenter randomized clinical trial. Obes Surg. 2019;29:1117–21.
Betzel B, Koehestanie P, Aarts EO, Dogan K, Homan J, Janssen IM, et al. Safety experience with the duodenal-jejunal bypass liner: an endoscopic treatment for diabetes and obesity. Gastrointest Endosc. 2015;82:845–52.
Poelemeijer YQM, Liem RL, Våge V, Mala T, Sundbom M, Ottosson J, et al. Perioperative outcomes of primary bariatric surgery in North-Western Europe: a pooled multinational registry analysis. Obes Surg. 2018;28:3916–22.
Mulier JP, Dillemans B. Anaesthetic factors affecting outcome after bariatric surgery, a retrospective levelled regression analysis. Obes Surg. 2019;29:1841–50.
Pouwels S, Buise MP, Twardowski P, Stepaniak PS, Proczko M. Obesity surgery and anesthesiology risks: a review of key concepts and related physiology. Obes Surg. 2019;29:2670–7.
Lemanu DP, Singh PP, Berridge K, et al. Randomized clinical trial of enhanced recovery versus standard care after laparoscopic sleeve gastrectomy. Br J Surg. 2013;100:482–9.
Dogan K, Kraaij L, Aarts EO, Hammink E, van Laarhoven CJ, Aufenacker TJ, et al. Fast-track bariatric surgery improves perioperative care and logistics compared to conventional care. Obes Surg. 2015 Jan;25:28–35.
Schijns W, Deenen MJ, Aarts EO, Homan J, Janssen IMC, Berends FJ, et al. The effect of obesity on anti-Xa concentrations in bariatric patients. Obes Surg. 2018;28:1997–2005.
Foster MW, Gershuni VM, Tewksbury CM, Giri JS, Dumon KR, Rame JE, et al. Laparoscopic sleeve gastrectomy carries a lower perioperative mortality including sudden cardiac death over Roux-en-Y gastric bypass in patients with a prior cardiac history: an MBSAQIP analysis. Obes Surg. 2019 Dec;24 [Epub ahead of print].
van Rijswijk AS, Moes DE, Geubbels N, Hutten BA, Acherman YIZ, van de Laar AW, et al. Can a laparoscopic Roux-en-Y gastric bypass be safely performed by surgical residents in a bariatric center-of-excellence? The learning curve of surgical residents in bariatric surgery. Surg Endosc. 2018;32:1012–20.
• Wehrtmann FS, de la Garza JR, Kowalewski KF, Schmidt MW, Müller K, Tapking C, et al. Learning curves of laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy in bariatric surgery: a systematic review and introduction of a standardization. Obes Surg. 2019; This article is of importance, while, although not the only one, it advocates something that will help comparing research in bariatric surgery in the future; standardization. The hardest thing nowadays is comparing between studies which makes it for example hard to actually compare outcomes of different surgeries performed. Although it will be hard to standardize everything, it would be a major step forward.
Ozsoy Z, Demir E. The evolution of bariatric surgery publications and global productivity: a bibliometric analysis. Obes Surg. 2018;28:1117–29.
Gastrointestinal surgery for severe obesity. Consens Statement. 1991: 9:1–20.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
Dr. Aarts has no conflicts of interest to disclose. Dr. Mahawar has been paid honoraria by Medtronic ®, Ethicon ®, Gore ®, Olympus ®, and various NHS Trusts in the United Kingdom for educational activities.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Disclaimer
Figures have all been drawn by Dr. E.O. Aarts and he holds current intellectual property.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on The Obesity Epidemic: Causes and Consequences
Rights and permissions
About this article
Cite this article
Aarts, E.O., Mahawar, K. From the Knife to the Endoscope—a History of Bariatric Surgery. Curr Obes Rep 9, 348–363 (2020). https://doi.org/10.1007/s13679-020-00382-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13679-020-00382-1