Abstract
Purpose of Review
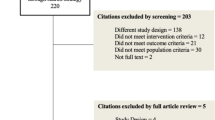
A growing body of research highlights the use of TNF inhibitors in the treatment of psoriasis and psoriatic arthritis. We aim to review the literature, compile psoriasis efficacy data for TNF inhibitors, and offer advice regarding the approach to treating this condition.
Recent Findings
The results of randomized placebo-controlled studies indicate that TNF inhibitors are efficacious and well tolerated in the treatment of psoriasis. There is a greater prevalence of anxiety, depression, cardiovascular disease, obesity, diabetes, hypertension, dyslipidemia, fatty liver disease, metabolic syndrome, and inflammatory bowel disease in psoriasis patients than in the general population. Severe psoriasis portends an increased risk of mortality.
Summary
Although patients with mild-to-moderate psoriasis do not have an increased mortality rate, the inherent inflammatory nature of psoriasis and its association with serious comorbid conditions may warrant the use of systemic medications, such as TNF inhibitors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Psoriasis is a chronic, inflammatory disease with both dermatologic and systemic manifestations. Biologics targeting TNF-alpha, interleukin (IL)-17, IL-12, and IL-23 have revolutionized our approach to treating psoriasis [1]. Though these immunomodulators pose some risk and require periodic monitoring, risk-benefit analysis often favors their use. A growing body of research highlights the use of TNF inhibitors including etanercept, infliximab, adalimumab, golimumab, and certolizumab pegol in the treatment of psoriasis and psoriatic arthritis. Etanercept, adalimumab, and infliximab are approved by the Food and Drug Administration (FDA) for use in psoriasis and psoriatic arthritis. Certolizumab pegol and golimumab are approved for use in psoriatic arthritis. We aim to review the literature to compile psoriasis efficacy data for these TNF inhibitors and offer advice regarding the approach to treating this condition.
Structure and Mechanism of Action
Etanercept is a dimeric fusion protein that consists of two domains of the human p75 TNF receptor combined with the Fc portion of IgG1. It inhibits TNF binding to cell surface receptors [2, 3]. Infliximab is a chimeric monoclonal antibody that binds to both soluble and transmembrane TNF-alpha with high affinity and specificity. It is composed of the constant regions of human IgG1ҡ that is coupled to the variable regions of a mouse anti-TNF-alpha monoclonal antibody. It prevents binding of TNF-alpha to the TNF receptor [3, 4]. Adalimumab is a human anti-TNF-alpha monoclonal antibody which binds with high affinity to soluble and transmembrane TNF-alpha and blocks its interaction with the p55 and p75 cell surface TNF receptors [3]. Golimumab is a human anti-TNF-alpha monoclonal antibody that targets and neutralizes soluble and membrane-bound TNF-alpha [3]. Certolizumab pegol is a TNF inhibitor composed of a humanized Fab fragment fused to a polyethylene glycol (PEG) moiety. The PEG component increases the products circulating half-life. The product recognizes and neutralizes the soluble and membrane-bound forms of human TNF [3, 5•]. Each of these TNF inhibitors prevents the TNF-alpha-induced pro-inflammatory activity, which is present in psoriasis and other immune-mediated inflammatory conditions (Fig. 1, Table 1).
The molecular structure of five TNF-α inhibitors. Adalimumab and golimumab both contain similar human IgG1 Fc and Fv portions. Infliximab contains the variable regions of a mouse anti-TNF-alpha monoclonal antibody alongside its constant human IgG1 Fc. Etanercept contains a constant human IgG1 Fc region as well as a TNFR2 region. Certolizumab pegol contains a PEGylated humanized Fab’ region. Fab fragment antigen binding, Fc fragment crystallizable, Fv fragment variable, PEG polyethylene glycol, TNF-α tumor necrosis factor alpha
Efficacy and Tolerability
Etanercept
Etanercept is effective in reducing the clinical manifestations of psoriatic arthritis and psoriasis. A 12-week, randomized, double-blinded, placebo-controlled study assessing the efficacy and safety of a twice-weekly subcutaneous injection of etanercept 25 mg noted improvement in psoriatic arthritis and psoriasis. Study endpoints included meeting Psoriatic Arthritis Response Criteria (PsARC) at 12 weeks, American College of Rheumatology 20% improvement criteria (ACR20) at 12 weeks, and 75% improvement from baseline in the Psoriasis Area and Severity Index score (PASI75) at 12 weeks. The PsARC endpoint was achieved in 87% of the subjects in the etanercept-treated group and 23% of the subjects in the placebo-treated group. The ACR20 endpoint was achieved in 73% of the subjects in the etanercept-treated group and 13% of the subjects in the placebo-treated group. The PASI75 endpoint was reached in 26% of the subjects in the etanercept-treated group, compared to none of the subjects in the placebo-treated group (p = 0.015). The median PASI improvement was 46% in the etanercept-treated group compared to 9% in the placebo-treated group. Etanercept was well tolerated in this cohort [6].
A randomized, double-blinded, placebo-controlled study assessing the safety and efficacy of etanercept in the treatment of plaque psoriasis noted reduction in disease severity over a 24-week time period. Subjects were randomized to receive placebo, low dose of etanercept (25 mg/week), medium dose of etanercept (25 mg twice weekly), or high dose of etanercept (50 mg twice weekly) during the first 12 weeks of the study. Subjects in the placebo group crossed over to receiving a medium dose of etanercept during the last 12 weeks of the study. The primary outcome measure was PASI75. Of the patients that received a low dose, medium dose, or high dose of etanercept, 14, 34, and 49% reached PASI75 at 12 weeks, respectively. In the placebo-treated group, just 4% of subjects reached PASI75 at 12 weeks (p < 0.001). Etanercept was generally well tolerated in this cohort [7].
A 24-week, randomized, double-blinded, placebo-controlled study assessing the efficacy, safety, and effect on radiographic progression of etanercept in patients with psoriatic arthritis noted reduction in the signs and symptoms of psoriatic arthritis and psoriasis. A total of 205 subjects were enrolled; 101 subjects received etanercept 25 mg twice weekly, and 104 subjects received placebo. Primary study endpoints assessing etanercept efficacy in psoriatic arthritis and psoriasis were ACR20 and PASI75. In the group that received etanercept, 59% achieved ACR20 at 12 weeks compared to 15% in the placebo group (p < 0.0001). Of the subjects who were eligible for psoriasis evaluation, 23% of the subjects in the etanercept group achieved PASI75, compared to 3% in the placebo-treated group (p = 0.001). Etanercept was well tolerated in this study cohort [8]. In a phase III, multicenter, randomized controlled trial assessing the safety and efficacy of etanercept, subjects were randomized to receive etanercept 25 mg twice weekly (BIW), etanercept 50 mg BIW, or placebo. PASI75 was achieved at week 12 in 49, 34, and 3% of subjects in the etanercept 50 mg, etanercept 25 mg, and placebo group, respectively [9]. In a pediatric study assessing the efficacy and safety of etanercept, subjects aged 4 to 17 with moderate-to-severe plaque psoriasis were randomized to receive etanercept 0.8 mg/kg weekly (QW) or placebo. PASI75 was achieved at 12 weeks in 57 and 11% of subjects in the etanercept group and placebo group, respectively [10] (Table 2).
Infliximab
Infliximab is an effective treatment for psoriasis and psoriatic arthritis. In a randomized, double-blind, placebo-controlled study of 33 subjects with moderate to severe plaque psoriasis, participants were randomized to receive intravenous placebo, intravenous infliximab 5 mg/kg, or intravenous infliximab 10 mg/kg at weeks 0, 2, and 6 and were clinically assessed at week 10. The primary endpoint was Physician’s Global Assessment (PGA) of “good,” “excellent,” or “clear.” Eighty-two percent of subjects treated with the 5 mg/kg infliximab dose, 91% of subjects treated with the 10 mg/kg infliximab dose, and 18% of subjects in the placebo group achieved a good, excellent, or clear rating on PGA over a 10-week period. There were no serious adverse events; infliximab was well tolerated in this cohort [11].
In an open-label, randomized, active-controlled trial comparing the efficacy of infliximab versus methotrexate in the treatment of moderate-to-severe plaque psoriasis, infliximab was superior in efficacy and was efficacious in subjects who initially failed methotrexate. Subjects were randomized to receive infliximab 5 mg/kg at weeks 0, 2, 6, 14, and 22 or methotrexate 15 mg weekly. Subjects in the methotrexate group were allowed to increase dose to 20 mg weekly after 6 weeks if PASI was less than 25% and switch to the infliximab group at week 16 if PASI was less than 50%. The primary efficacy endpoint was PASI75 response at week 16. This endpoint was achieved in 78% of infliximab-treated subjects and 42% of methotrexate-treated subjects (p < 0.001). The overall incidence of adverse events was similar between the methotrexate and infliximab groups; however, serious adverse event incidence was slightly higher in the infliximab group [12].
In a 46-week, phase III, randomized, double-blinded, placebo-controlled, multicenter trial, the efficacy of infliximab induction and maintenance regimens were assessed in subjects with moderate-to-severe plaque psoriasis. Subjects were randomized to receive either infliximab 5 mg/kg or placebo at weeks 0, 2, and 6 and every 8 weeks until 46 weeks. Subjects in the placebo group crossed over to infliximab treatment at week 24. The primary endpoint was 75% improvement from baseline PASI. Eighty percent of subjects treated with infliximab and 3% of subjects in the placebo group achieved PASI75 at week 10 (p < 0.0001). Eighty-two percent of subjects treated with infliximab and 4% of subjects in the placebo group achieved PASI75 at week 24 (p < 0.0001). Infliximab was well tolerated in the majority of patients [13] (Table 2).
Adalimumab
Adalimumab has utility in the treatment of both psoriasis and psoriatic arthritis. In a randomized, double-blinded, placebo-controlled trial assessing the efficacy and safety of adalimumab in the treatment of active psoriatic arthritis, subjects were randomized to receive subcutaneous injections of adalimumab 40 mg or placebo every other week for 24 weeks. Relevant endpoints were ACR20 and PASI75. Fifty-eight percent of subjects in the adalimumab group and 14% of subjects in the placebo group achieved ACR20 at week 12 (p < 0.001). Fifty-nine percent of subjects in the adalimumab group, who were eligible for evaluation with PASI, achieved PASI75 at week 24, compared to just 1% in the placebo group (p < 0.001). Adalimumab was generally well tolerated in study subjects [14]. In a randomized, placebo-controlled phase III trial assessing its efficacy and safety in patients with moderate-to-severe psoriasis, adalimumab was efficacious and well tolerated. Subjects were randomized to receive adalimumab 40 mg or placebo every other week for 15 weeks. Primary endpoint was PASI75. Seventy-one percent of the adalimumab group and 7% of the placebo group achieved PASI75 by week 16 [15]. In a 16-week, phase IIIb, open-label study evaluating the efficacy and safety of adalimumab in psoriasis patients with prior suboptimal response to etanercept, methotrexate, or narrowband (NB) ultraviolet (UV) B therapy, subjects who had a suboptimal response to these other treatment options had a 50% likelihood of achieving optimal response to adalimumab. Study participants had either discontinued suboptimal etanercept between 11 and 17 days or suboptimal methotrexate or UVB between 4 and 10 days prior to starting adalimumab 80 mg at week 0 and 40 mg per week thereafter for 16 weeks. The primary endpoint was achievement of a PGA rating of clear or “minimal.” Fifty-two percent of study subjects achieved this endpoint by 16 weeks [16] (Table 2).
Golimumab
The efficacy of golimumab in the treatment of psoriasis and psoriatic arthritis has been well documented in the literature. A randomized, placebo-controlled study assessing golimumab efficacy and safety in patients with active psoriatic arthritis established efficacy in the study cohort. Patients were randomized to receive subcutaneous injection of placebo, golimumab 50 mg, or golimumab 100 mg every 4 weeks for 20 weeks. Primary study endpoints included ACR20 and PASI. Forty-eight percent of subjects who received golimumab and 9% of subjects who received placebo reached ACR20 at week 14 (p < 0.001). Forty percent and 58% of subjects reached PASI75 by week 14 in the golimumab 50 mg and golimumab 100 mg groups, respectively. Only 3% of the placebo group reached this endpoint (p < 0.001) Golimumab was generally well tolerated in study subjects [17]. A 2-year long, randomized, placebo-controlled study assessed the clinical efficacy, radiographic findings, and safety findings of golimumab in patients with active psoriatic arthritis. Subjects were randomized to receive placebo, golimumab 50 mg, or golimumab 100 mg every 4 weeks for 20 weeks. After 24 weeks, all subjects would receive either golimumab 50 mg or golimumab 100 mg. Primary endpoints included ACR20 and PASI75. PASI75 was achieved at 104 weeks in 56–72% of golimumab recipients. ACR20 was achieved at 104 weeks in 63–70% of patients in the golimumab treatment group [18••] (Table 2).
Certolizumab Pegol
Certolizumab pegol is efficacious in the treatment of psoriasis and psoriatic arthritis. A randomized, double-blind, placebo-controlled study evaluating efficacy and safety of certolizumab pegol in the treatment of moderate-to-severe plaque psoriasis noted improved psoriasis in the certolizumab pegol treatment groups. Primary endpoint was PASI75 at week 12. Subjects were randomized to receive placebo or certolizumab pegol 400 mg at week 0 followed by placebo or certolizumab (200 or 400 mg) every other week for 10 weeks. Seventy-five percent, 83%, and 7% of subjects achieved PASI75 in the certolizumab pegol 200 mg, certolizumab pegol 400 mg, and placebo group at week 12, respectively (p < 0.001) [19].
In a randomized, placebo-controlled study assessing the efficacy and safety of certolizumab pegol in patients with psoriatic arthritis, subjects were randomized to receive certolizumab pegol 200 mg every 2 weeks (Q2W), 400 mg every 4 weeks (Q4W), or placebo. Primary endpoints included ACR20 at week 12 and modified total sharp score change from baseline (mTSS) at week 24. ACR20 response was 58.0, 51.9, and 24.3% in Q2W group, Q4W group, and placebo group, respectively (p < 0.001) [20••] (Table 2).
TNF inhibitors are generally safe and tolerable in adults with moderate-to-severe psoriasis. Though some patients did report adverse events during clinical trials, these events could not be directly attributed to the TNF inhibitor and may have been the result of an underlying comorbidity. Rarely reported adverse effects included opportunistic infection, latent tuberculosis reactivation, demyelinating disorder onset or exacerbation, psoriasis onset or exacerbation, lymphoma, drug-induced lupus, congestive heart failure, liver toxicity, hematologic abnormalities, and anaphylaxis. Common adverse effects included headaches, upper respiratory tract infections, cellulitis, urticaria, injection site reactions, subclinical elevated liver enzymes, and pruritus. Due to the potential causative relationship between TNF inhibitors and the aforementioned adverse events, procurement of a comprehensive patient history and patient education are crucial prior to prescribing these medications [21].
Conclusions
Psoriasis is a chronic inflammatory disorder with both cutaneous and systemic manifestations. Recent research has uncovered the association of psoriasis with several medical conditions. Metabolic syndrome, which includes features such as central obesity, insulin resistance, dyslipidemia, and hypertension, predisposes patients to developing cardiovascular disease [22•]. The greater the severity of psoriasis, the greater the association with metabolic syndrome [23]. There is a direct relationship between the risk of cardiovascular disease and the severity of psoriasis [24•]. There is a greater prevalence of anxiety, depression, cardiovascular disease, obesity, diabetes, hypertension, dyslipidemia, fatty liver disease, metabolic syndrome, and inflammatory bowel disease in psoriasis patients compared to the general public [25, 26•]. It is unclear whether this association is due to the systemic inflammatory mediators generated in psoriasis or shared risk factors. Modern pharmacotherapy research has dramatically improved the psoriasis armamentarium. Limited disease is typically managed with topical medications. In patients with more extensive involvement, topical medications may be used, but patients may opt for oral and injectable medications with systemic activity. We highlight the efficacy and tolerability of TNF inhibitors in the treatment of psoriasis. These medications allow practitioners to target the underlying inflammatory nature of psoriasis on a molecular level. Targeting TNF-alpha not only curbs cutaneous inflammation but also controls the systemic inflammation associated with psoriasis. Biologic medications have revolutionized how we approach the treatment of psoriasis. The morbidity associated with psoriasis is well documented and frequently discussed. Now, with research highlighting the potential cardiovascular and metabolic impact of psoriasis, a discussion on the mortality of psoriasis is appropriate. Severe psoriasis is associated with an increased risk of death; this finding persisted after adjustment for risk factors of mortality [27]. Although patients with mild-to-moderate psoriasis do not have an increased mortality rate, the inherent inflammatory nature of psoriasis and its association with serious comorbid conditions may warrant the use of systemic medications even in this patient group. Aggressive treatment of psoriasis is prudent; TNF inhibitors and other biologics present a highly efficacious treatment option with a relatively favorable side effect profile.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Weger W. Current status and new developments in the treatment of psoriasis and psoriatic arthritis with biological agents. Br J Pharmacol [Internet]. 2010;160(4):810–20. doi:10.1111/j.1476-5381.2010.00702.x.
Kirkham B. Tumor necrosis factor-alpha inhibitors: an overview of adverse effects [Internet]. [cited 2016 Dec 31]. Available from: http://www.uptodate.com/contents/tumor-necrosis-factor-alpha-inhibitors-an-overview-of-adverse-effects.
Wong M, Ziring D, Korin Y, Desai S, Kim S, Lin J, et al. TNFalpha blockade in human diseases: mechanisms and future directions. Clin Immunol [Internet]. 2008;126(2):121–36. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17916444.
Chen Y-F, Jobanputra P, Barton P, Jowett S, Bryan S, Clark W, et al. A systematic review of the effectiveness of adalimumab, etanercept and infliximab for the treatment of rheumatoid arthritis in adults and an economic evaluation of their cost-effectiveness. Health Technol Assess [Internet]. 2006;10(42):iii–v. xi–xiii, 1-229. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17049139.
• Felquer MLA, Soriano ER. New treatment paradigms in psoriatic arthritis. Curr Opin Rheumatol [Internet]. 2015;27(2):99–106. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00002281-201503000-00002. This is a review article that consolidates the treatment options for psoriatic arthritis, notably for certolizumab pegol.
Mease PJ, Goffe BS, Metz J, VanderStoep A, Finck B, Burge DJ. Etanercept in the treatment of psoriatic arthritis and psoriasis: a randomised trial. Lancet (London, England) [Internet]. 2000;356(9227):385–90. Available from: http://www.sciencedirect.com/science/article/pii/S0140673600025307.
Leonardi CL, Powers JL, Matheson RT, Goffe BS, Zitnik R, Wang A, et al. Etanercept as monotherapy in patients with psoriasis. N Engl J Med [Internet]. 2003;349(21):2014–22. Available from: http://www.ncbi.nlm.nih.gov/pubmed/14627786.
Mease PJ, Kivitz AJ, Burch FX, Siegel EL, Cohen SB, Ory P, et al. Etanercept treatment of psoriatic arthritis: safety, efficacy, and effect on disease progression. Arthritis Rheum. 2004;50(7):2264–72.
Papp KA, Tyring S, Lahfa M, Prinz J, Griffiths CEM, Nakanishi AM, et al. A global phase III randomized controlled trial of etanercept in psoriasis: safety, efficacy, and effect of dose reduction. Br J Dermatol [Internet]. 2005;152(6):1304–12. doi:10.1111/j.1365-2133.2005.06688.x.
Paller AS, Siegfried EC, Langley RG, Gottlieb AB, Pariser D, Landells I, et al. Etanercept treatment for children and adolescents with plaque psoriasis. N Engl J Med [Internet]. 2008;358(3):241–51. doi:10.1056/NEJMoa066886.
Chaudhari U, Romano P, Mulcahy LD, Dooley LT, Baker DG, Gottlieb AB. Efficacy and safety of infliximab monotherapy for plaque-type psoriasis: a randomised trial. Lancet (London, England) [Internet]. 2001;357(9271):1842–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11410193.
Barker J, Hoffmann M, Wozel G, Ortonne J-P, Zheng H, van Hoogstraten H, et al. Efficacy and safety of infliximab vs. methotrexate in patients with moderate-to-severe plaque psoriasis: results of an open-label, active-controlled, randomized trial (RESTORE1). Br J Dermatol [Internet]. 2011;165(5):1109–17. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21910713.
Reich K, Nestle FO, Papp K, Ortonne J-P, Evans R, Guzzo C, et al. Infliximab induction and maintenance therapy for moderate-to-severe psoriasis: a phase III, multicentre, double-blind trial. Lancet [Internet]. 2005;366(9494):1367–74. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16226614
Mease PJ, Gladman DD, Ritchlin CT, Ruderman EM, Steinfeld SD, Choy EHS, et al. Adalimumab for the treatment of patients with moderately to severely active psoriatic arthritis: results of a double-blind, randomized, placebo-controlled trial. Arthritis Rheum [Internet]. 2005;52(10):3279–89. doi:10.1002/art.21306.
Menter A, Tyring SK, Gordon K, Kimball AB, Leonardi CL, Langley RG, et al. Adalimumab therapy for moderate to severe psoriasis: a randomized, controlled phase III trial. J Am Acad Dermatol. 2008;58(1):106–15.
Strober BE, Poulin Y, Kerdel FA, Langley RG, Gu Y, Gupta SR, et al. Switching to adalimumab for psoriasis patients with a suboptimal response to etanercept, methotrexate, or phototherapy: efficacy and safety results from an open-label study. J Am Acad Dermatol. 2011;64(4):671–81.
Kavanaugh A, McInnes I, Mease P, Krueger GG, Gladman D, Gomez-Reino J, et al. Golimumab, a new human tumor necrosis factor α antibody, administered every four weeks as a subcutaneous injection in psoriatic arthritis: twenty-four-week efficacy and safety results of a randomized, placebo-controlled study. Arthritis Rheum [Internet]. 2009;60(4):976–86. doi:10.1002/art.24403.
•• Kavanaugh A, IB MI, Mease PJ, Krueger GG, Gladman DD, van der Heijde D, et al. Clinical efficacy, radiographic and safety findings through 2 years of golimumab treatment in patients with active psoriatic arthritis: results from a long-term extension of the randomised, placebo-controlled GO-REVEAL study. Ann Rheum Dis [Internet]. 2013;72(11):1777–85. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23161902. This randomized control trial illustrates the clinical efficacy and safety findings of golimumab in psoriatic arthritis.
Reich K, Ortonne J-P, Gottlieb AB, Terpstra IJ, Coteur G, Tasset C, et al. Successful treatment of moderate to severe plaque psoriasis with the PEGylated Fab′ certolizumab pegol: results of a phase II randomized, placebo-controlled trial with a re-treatment extension. Br J Dermatol [Internet]. 2012;167(1):180–90. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22413944.
•• Mease PJ, Fleischmann R, Deodhar AA, Wollenhaupt J, Khraishi M, Kielar D, et al. Effect of certolizumab pegol on signs and symptoms in patients with psoriatic arthritis: 24-week results of a phase 3 double-blind randomised placebo-controlled study (RAPID-PsA). Ann Rheum Dis [Internet]. 2014;73(1):48–55. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23942868. This randomised trial summarizes the clinical efficacy of certolizumab pegol (200mg vs 400mg) vs placebo.
Semble AL, Davis SA, Feldman SR. Safety and tolerability of tumor necrosis factor-α inhibitors in psoriasis: a narrative review. Am J Clin Dermatol [Internet]. 2014;15(1):37–43. Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/s40257-013-0053-5.
• Oliveira Mde FSP, Rocha Bde O, Duarte GV. Psoriasis: classical and emerging comorbidities. An Bras Dermatol. 2015;90(1):9. This review article summarizes the most recent comorbities associated with psoriasis.
Langan SM, Seminara NM, Shin DB, Troxel AB, Kimmel SE, Mehta NN, et al. Prevalence of metabolic syndrome in patients with psoriasis: a population-based study in the United Kingdom. J Invest Dermatol [Internet]. 2012;132(3):556–62. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0022202X15356712.
• Tablazon ILD, Al-Dabagh A, Davis SA, Feldman SR. Risk of cardiovascular disorders in psoriasis patients. Am J Clin Dermatol [Internet]. 2013;14(1):1–7. Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/s40257-012-0005-5. This review article summarizes the direct relationship between the risk of cardiovascular disease and the severity of psoriasis.
Ni C, Chiu MW. Psoriasis and comorbidities: links and risks. Clin Cosmet Investig Dermatol [Internet]. 2014;7:119–32. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24790463.
• Onumah N, Kircik LH. Psoriasis and its comorbidities. J Drugs Dermatol [Internet]. 2012;11(5 Suppl):s5–10. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22644770. This is a review article complementing reference #22 in summarizing the most recent comorbities associated with psoriasis.
Gelfand JM, Troxel AB, Lewis JD, Kurd SK, Shin DB, Wang X, et al. The risk of mortality in patients with psoriasis. Arch Dermatol [Internet]. 2007;143(12):1493–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18086997.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Steven Feldman declares research, speaking, and/or consulting support from a variety of companies including Galderma, GSK/Stiefel, Almirall, Leo Pharma, Baxter, Boeringer Ingelheim, Mylan, Celgene, Pfizer, Valeant, Taro, Abbvie, Cosmederm, Anacor, Astellas, Janssen, Lilly, Merck, Merz, Novartis, Regeneron, Novan, Parion, Qurient, National Biological Corporation, Caremark, Advance Medical, Sun Pharma, Suncare Research, Informa, UpToDate, and National Psoriasis Foundation. Dr. Feldman also consults for others through Guidepoint Global, Gerson Lehrman, and other consulting organizations. Dr. Feldman is founder and majority owner of www.DrScore.com. I am a founder and part owner of Causa Research, a company dedicated to enhancing patients’ adherence to treatment.
Leah A. Cardwell, Brandy Sullivan, Emilia Baran, and Elias Oussedik declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Funding
The Center for Dermatology Research is supported by an unrestricted educational grant from Galderma Laboratories, L.P.
Additional information
This article is part of the Topical Collection on Psoriasis
Rights and permissions
About this article
Cite this article
Cardwell, L.A., Sullivan, B., Baran, E. et al. TNF Inhibitors for Psoriasis and Psoriatic Arthritis. Curr Derm Rep 6, 113–120 (2017). https://doi.org/10.1007/s13671-017-0174-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13671-017-0174-9