Abstract
With an aging population worldwide, the incidence and prevalence of certain pulmonary conditions such as chronic obstructive pulmonary disease (COPD) and idiopathic pulmonary fibrosis (IPF) are increasing. Pulmonary function tests (PFTs) are helpful tools to confirm pulmonary disorders. However, in the elderly population, age-associated changes in PFTs increase the risk for over diagnosis of obstructive lung disease. Therefore, an individualized approach to diagnosis of pulmonary disorders is essential for optimal management. For patients with established pulmonary disorders, pulmonary rehabilitation is a valuable but underutilized therapeutic intervention which has been shown to improve patient’s quality of life, exercise tolerance, and overall prognosis. Recent evidence confirms that benefits of pulmonary rehabilitation are similar between the elderly and younger populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The elderly population is expanding around the world. The three leading causes of death in individuals ≥65 years include cardiovascular disease, cancer, and chronic lower respiratory tract diseases [1••]. Pulmonary disorders which are strongly associated with advanced age are chronic obstructive pulmonary disease (COPD) and idiopathic pulmonary fibrosis (IPF). This review will discuss the role of pulmonary function testing (PFT) in diagnosis of pulmonary diseases as it relates to the aging adults and the contribution of pulmonary rehabilitation (PR) in management of those conditions.
Epidemiology of common pulmonary diseases in the elderly population
On a global level, the elderly population (age ≥65 years) is projected to increase 104 % from 2005 to 2030, whereas the population <65 years of age will augment by only 21 % [2•]. The oldest-old (age ≥85 years) is the fastest growing population in many countries [2•].
As the population ages, the incidence and prevalence of pulmonary diseases which are most likely to occur and manifest later in life are projected to increase. According to the Centers for Disease Control (CDC) and Prevention in 2011, 6.5 % of US adults were estimated to have self-reported diagnosis of COPD. Prevalence of COPD increased almost fourfold from age 18–44 years to those age ≥65 years [3]. In a meta-analysis by Halbert et al., the reported pooled prevalence of COPD in individuals ≥65 years is 14.2 % (11–18 %) compared to 9.9 % (8.2–11.8 %) in those ≥40 years [4]. The reported heterogeneity in the study results is multifactorial, including disease definition, population studied as well as the methodologies used for data interpretation. Furthermore, the prevalence of COPD increases twofold for every 10-year increase in age after age 40 [5]. By 2020, the World Health Organization (WHO) predicts that COPD will become the third most common cause of morbidity and mortality worldwide [6]. In the USA, COPD is reported to be the primary and/or contributing factor for almost 20 % of all hospitalizations in the elderly population [7]. In addition to the disease burden, COPD carries a significant economic impact. In 2005, the annual total cost (related to morbidity and premature mortality) attributable to COPD was estimated at $38.8 billion [8]. Expenses increased significantly when compared to $23.9 billion spent in 1993 [7]. The annual direct cost attributable to COPD/patient averages $6300, while other respiratory-related costs averaged $4400 [9].
Asthma is another obstructive lung disease, which contrary to popular belief, is not uncommon in the elderly population. In 2004, the US prevalence of asthma in the elderly was 7 %, with more than 1 million patients reporting an asthma attack in the previous 12 months [10]. The elderly asthmatics have the highest death rate (51.3 per million people) compared to any other age group [11]. Asthma in the older population can be divided into the long-standing asthma (disease onset during childhood) and late-onset asthma (disease onset in the sixth decade of life or later) [12•]. Due to comorbid illnesses, as well as age-related changes in pulmonary and immune function, it is not uncommon for the late-onset asthmatic patients to be labeled as “COPD-ers” which leads to suboptimal treatment.
Idiopathic pulmonary fibrosis is a type of interstitial lung disease characterized by chronic, progressive interstitial fibrosis of unknown etiology. This extremely debilitating pulmonary condition tends to manifest in the sixth decade of life, and most patients die within 5 years from the diagnosis [13]. At any given time, there are up to 50,000 cases of IPF in the USA and 65 % of the IPF patients are greater than 65 years of age [14]. Fernandez-Perez and colleagues projected that the annual number of newly diagnosed cases of IPF in the US population may reach 21,000 by 2050 [15]. Individual course of disease varies between patients where some patients will have a rapid decline due to acute exacerbation of IPF while others may have a more protracted course of deterioration and disability.
General diagnostic and therapeutic considerations for pulmonary diseases in the elderly
Diagnostic dilemmas are frequently encountered in the elderly. The role of the clinician is to adequately assess patients’ risk factors, determine the need for additional evaluation, and provide an individualized treatment plan. Taking care of the aging population involves consideration of age-specific factors (functional and/or cognitive decline, limited transportation, delay in seeking care, etc.), coexisting comorbidities, and polypharmacy.
Respiratory symptoms of dyspnea, exertional limitation, wheezing, and cough are common in the aging population. Dyspnea associated with different activity levels has been reported by more than 50 % of individuals >70 years of age [14]. Symptoms are often multifactorial and could be related to a chronic respiratory condition (COPD, asthma, IPF), cardiac condition (congestive heart failure, arrhythmias), side effect of medications (ACE-I, beta-blockers), deconditioning, mental health disorder, etc. Physical exam and additional diagnostic investigations such as pulmonary function testing (PFTs) and radiographic imaging (chest x-ray, CT of the chest) are the basis for identifying an underlying pulmonary etiology.
The overall goals of treatment for patients with chronic pulmonary disorders include adequate symptom control, prevention of the complications and exacerbations, improvement in the activity level, and decrease in disease mortality. Those outcomes are achieved through a combination of pharmacotherapy, pulmonary rehabilitation [16••, 17••], and, when applicable, smoking cessation, oxygen supplementation, noninvasive positive pressure ventilation (NIPPV), surgical therapies such as lung volume reduction surgery, and lung transplantation [16••, 17••, 18, 19••].
Role of PFTs in diagnosis and management of pulmonary diseases in the elderly
PFT is a generic term which includes multiple diagnostic tests. Various combinations of these tests are useful to confirm pulmonary disease and its severity, assess response to therapeutic interventions, and monitor drug-related (e.g., amiodarone, methotrexate, nitrofurantoin) or occupation-related (e.g., asbestos, coal, silica) pulmonary toxicity. In addition, in patients undergoing surgery, risk assessment for peri-operative pulmonary complications is based on a combination of respiratory symptoms, exercise tolerance, smoking status, and PFTs [20].
There are no absolute contraindications to PFT evaluation. Relative contraindications include but are not limited to unstable angina, recent myocardial infarction (MI), recent eye or thoraco-abdominal surgery, hemoptysis, and pneumothorax [21, 22]. In addition, patients may not be able to conclude testing if unable to follow directions due to physical or cognitive impairment. Perceived difficulties seem to be reported more frequently in the elderly. However, age by itself is not a limiting factor in completing good-quality PFTs. In a retrospective review of patients undergoing testing, Haynes et al. demonstrated that a cohort of older adults (median age = 83) achieved similar spirometry and diffusion for carbon monoxide (DLCO) quality scores when compared to younger ones (median age = 46) [23••]. Therefore, approach to diagnostic evaluation of pulmonary disease in the elderly is no different when compared to younger individuals. Figure 1 outlines the general principles involved in integrating PFTs in clinical management. As highlighted, spirometry is almost always the initial PFT requested as it serves as a good screening tool for both obstructive and restrictive pulmonary conditions. Simple equipment and technical ease allow widespread use of spirometry in all settings (inpatient as well as outpatient). Additional PFT evaluation (e.g., lung volumes, DLCO) is performed based on the clinical context and would need referral to a PFT laboratory.
Decision tree for PFT interpretation. Single asterisk based on GOLD guidelines [17••]. Double asterisk based on ATS/ERS guidelines [24]. CHF congestive heart failure, DLCO diffusion lung capacity, FEV1 forced expiratory volume in 1 s, FVC forces vital capacity, ILD interstitial lung disease, LLN lower limit of normal, MIP/MEP maximum inspiratory/expiratory pressure, NMD neuromuscular disease, Post-BD post-bronchodilator, Pulm vasc dis pulmonary vascular disease
There is ongoing controversy regarding the optimal cutoff for forced expiratory volume in 1 s (FEV1)/forced vital capacity (FVC) ratio to diagnose obstructive lung disease. The American Thoracic Society/European Respiratory Society (ATS/ERS) guidelines for interpretative strategy for spirometry recommend using lower limit of normal (LLN) of FEV1/FVC ratio to classify obstructive disease. The LLN is characterized by a reduction below the 5th percentiles of the predicted value which is considered to be outside the expected “normal range” [24]. In the USA, the predicted values are derived from the National Health and Nutrition Examination Survey (NHANES) III reference equations which included individuals aged 8–80 years [25]. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines, including the most recent update published in December 2015, recommends use of fixed FEV1/FVC ratio of 0.7 to classify obstructive disease [17••]. The GOLD criterion creates risk for overdiagnosis of COPD in the elderly. In a study by Hardie et al. which included healthy, asymptomatic, never-smoker adults aged >70 years, 35 % had an FEV1/ FVC <0.7 and would be classified as having at least stage 1 COPD. Furthermore, in the subgroup ≥80 years of age, 50 % fulfilled the criteria for COPD diagnosis and approximately one third would have stage 2 COPD (FEV1 < 80 %) based on the GOLD guidelines [26]. One limitation of this study included use of the pre-bronchodilator spirometry value whereas the GOLD guidelines are based on the post-bronchodilator spirometry [17••].
Based on the existing literature, it is unclear whether these different approaches of interpretation affect patient outcomes. In the Cardiovascular Health Study, the severity of COPD was classified in a cohort of 4965 participants ≥65 years of age based on the two methods (fixed FEV1/FVC ratio vs. LLN). Participants with FEV1/FVC > LLN but <0.7 had higher mortality (hazard ratio 1.3, 95 % CI 1.1–1.5) and COPD-related hospitalizations (HR 2.6, 95 % CI 2.0–2.3) compared with asymptomatic individuals with FEV1/FVC >0.7 and >LLN. Mean follow-up was 11 years. Therefore, FEV1/FVC <0.7 appears to identify at risk patients regardless of age [27]. Currently, there are no guidelines regarding the clinical application of incidentally discovered abnormal lung function in asymptomatic elderly patients. For clinicians treating the elderly population, an optimal strategy to integrate PFT findings into disease management is to request PFT evaluation only in symptomatic patients. Abnormal results in such patients would result in a direct impact on their management.
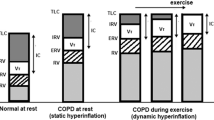
The role of PFTs and additional considerations in the elderly are summarized in Table 1. The age-related changes in pulmonary function testing are the result of multiple structural as well as functional alterations which include: (1) delayed alveolar emptying due to early closure of the airways at small volumes [31, 32]; (2) mechanical constraints resulting from stiffer chest wall, weaker respiratory muscles, and loss of static elastic recoil [33]; (3) gas exchange limitation due to decrease in the alveolar surface area and decreased capillaries per alveoli; and (4) some degree of decrease in the respiratory drive as well as central response to hypoxia and hypercapnia. The current understanding of the mechanism which results in those structural and functional changes remains very limited. Certain age-related changes in lung function (airflow limitation and loss of parenchymal tissue) are also markers of obstructive lung disease. An accelerated aging process represents a potential pathological mechanism for development of COPD. A recent investigation by Rutten et al described that one marker of aging mechanism (i.e., telemore length) is associated with lung function and could be an indicator of accelerated lung aging in patients with lung diseases [34•].
The role of pulmonary rehabilitation in the elderly
According to the most recent ATS/ERS official statement published in 2013, pulmonary rehabilitation is defined as a “comprehensive intervention based on a thorough patient assessment followed by tailored therapies that include, but are not limited to, exercise training, education and behavior change, designed to improve the physical and psychological condition of people with chronic respiratory disease and promote long-term adherence to health-enhancing behaviors” [16••]. The updated definition fully recognizes the systemic effects of COPD and other chronic pulmonary conditions. A patient-centric approach to disease management should integrate PR as a core component of treatment.
Exertional limitation and diminished quality of life in patients with lung disease is multifactorial. Pulmonary disease-specific factors such as increased dead space, mechanical restriction, delayed alveolar emptying, and gas exchange limitations contribute to poor exercise tolerance. Superimposed systemic and psychosocial issues such as peripheral muscle dysfunction, cardiac dysfunction, nutritional deficiency, depression, anxiety, social isolation, and suboptimal self-management strategies cause further impairment and disability [16••]. While pharmacotherapy primarily focuses on treatment of underlying lung disease, pulmonary rehabilitation provides a more holistic approach by also treating systemic contributors to symptoms [35–38]. The main goal of pulmonary rehabilitation is to restore the patient to the highest possible level of independent function. The general principles applied in a comprehensive pulmonary rehabilitation program are outlined in Table 2.
Initial research as well as clinical application of pulmonary rehabilitation primarily focused on patients with COPD due to high disease prevalence and its impact on the activity of daily living. In 2010, the US Burden of Disease Collaborators reported COPD to be the second leading cause of disability in the USA [39••]. According to the WHO global estimates, COPD will become the seventh leading cause of disability-adjusted life-years (DALYs) lost worldwide by 2030 [40]. The benefit of PR has been demonstrated in COPD patients with all degrees of disease severity and in inpatient as well as outpatient clinical settings. Benefit has now also been proved for other obstructive lung diseases (asthma, bronchiectasis, and cystic fibrosis), interstitial lung disease (idiopathic pulmonary fibrosis), neuromuscular diseases, pulmonary hypertension, and lung cancer [16••, 41•, 42, 43••, 44, 45•, 46•].
The overall beneficial effects of PR include reduction in respiratory symptoms such as dyspnea and fatigue, improvement in muscle strength and endurance, improvement in health-related quality of life, decreased healthcare utilization (hospitalizations and unscheduled healthcare visits), emotional function and self-efficacy, and possibly a reduction in mortality [47–49, 50••]. Anxiety and depression associated with severe lung disease could also be ameliorated by this intervention [16••].
A safe exercise program in the elderly population does require consideration of additional factors such as baseline physical activity level and coexisting comorbidities. The American College of Sports Medicine (ACSM) and American Heart Association (AHA) outlined specific recommendations for physical activity in older adults. The intensity of aerobic activity should be based on baseline aerobic fitness. Activities that maintain or increase flexibility are recommended, and additional balance exercises should be considered for older adults at risk of falls. The activity plan for achieving recommended physical activity level should integrate preventive and therapeutic recommendations for comorbidities [51].
Investigators have demonstrated that PR is as beneficial in the elderly as it is in younger patients in improving exercise capacity, symptoms, and self-reported quality of life [52, 53]. Baltaz et al. further demonstrated that even in patients ≥80 years, PR improves 6-min walk test distance (6MWT), the number of stairs completed in 2 min (2MST), Borg dyspnea scores after exertion, and objective functional scores similar to younger patients [54]. Furthermore, patients with both COPD and cardiac comorbidities are often enrolled in rehabilitation programs; 15 % of patients with COPD enrolled in PR have comorbid CHF [55] and 19 % of patients after CABG have COPD. Co-existent CAD and worsening dyspnea on exertion requires appropriate diagnostic work-up which need to be completed before considering increase in activity level.
In spite of the proven multifaceted benefit, PR continues to remain underutilized due to insufficient resources, lack of awareness (among patient, provider, and payer), and additional patient related barriers [50••, 56••]. A recent ATS/ERS international statement provided further policy recommendations to address all those limitations and encouraged research to support updated funding and reimbursement policy regarding PR [50••]. Furthermore, Gerald at el showed that only 25 % of individuals entering PR are reported to have advanced directives [57]. In the elderly, PR provides an opportunity to educate patients about advanced care directives, completion of the living will, and end of life care [58].
Conclusions
In patients with chronic lung disease, PFTs and PR are indispensable management tools that assist in optimizing care. The elderly are at risk for underutilization of these diagnostic and therapeutic tools despite the proven benefit in all age groups. When interpreting pulmonary diagnostic tests, it is important to consider that age-related changes in PFTs increase risk of over diagnosis of obstructive lung disease. The benefit of the PR extends beyond improvement in exercise tolerance; social isolation and mood disorders are common in the elderly and PR has been shown to be beneficial in addressing these psychosocial issues.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Centers for Disease Control and Prevention. http://www.cdc.gov/nchs/fastats/older-american-health.htm Accessed Feb 2016. 2014 Updated epidemiological data on health of older Americans.
United Nations Department of Economic and Social Affairs, Population Division. World Population Prospects. The 2004 Revision. New York: United Nations, 2004, publication date Sept 2011, updated January 2015. Accessed Feb 2016 http://esa.un.org/unpd/wpp/publications/Files/WPP2012_HIGHLIGHTS.pdf. Comprehensive review of worldwide demographic trends and future prospects.
Centers for Disease Control and Prevention. Chronic obstructive pulmonary disease among adults—United States, 2011. MMWR Morb Mortal Wkly Rep. 2012;61:938–43.
Halbert RJ, Natoli JL, Gano A, et al. Global burden of COPD: systematic review and meta-analysis. Eur Respir J. 2006;28(3):523–32.
Buist AS, McBurnie MA, Vollmer WM, et al. BOLD Collaborative Research Group. International variation in the prevalence of COPD (the BOLD study): a population-based prevalence study. Lancet. 2007;370(9589):741–50.
World Health Organization. Statistical dataset. Geneva, Switzerland; World Health Organization 2000. 3-1-2009. Available at: http://www.who.int/respiratory/copd/burden/en/index.html
Mannino DM. COPD: epidemiology, prevalence, morbidity and mortality, and disease heterogeneity. Chest. 2002;121(5, Suppl):121S–6.
Foster TS, Miller JD, Marton JP, et al. Assessment of the economic burden of COPD in the U.S.: a review and synthesis of the literature. COPD. 2006;3:211–8.
Menzin J, Boulanger L, Marton J, et al. The economic burden of chronic obstructive pulmonary disease (COPD) in a U.S. Medicare population. Respir Med. 2008;102:1248–56.
Hanania NA, King MJ, Braman SS, et al. Asthma in the elderly: current understanding and future research needs—a report of a National Institute on Aging (NIA) Workshop. J Allergy Clin Immunol. 2011;128(3):S4–24.
Moorman JE, Mannino DM. Increasing U.S. asthma mortality rates: who is really dying? J Asthma. 2001;38(1):65–71.
Al-Alawi M, Hassan T, Chortirmall SH. Advances in the diagnosis and management of asthma in older adults. Am J Med. 2014;127:370–8. Updated review on asthma diagnosis and management in elderly patients.
King Jr TE, Tooze JA, Schwarz MI, et al. Predicting survival in idiopathic pulmonary fibrosis: scoring system and survival model. Am J Respir Crit Care Med. 2001;164(7):1171–81.
Castriotta RJ, Eldadah BA, Foster M, et al. Workshop on idiopathic pulmonary fibrosis in older adults. Chest. 2010;138(3):693–703.
Fernandez-Perez ER, Daniels CE, Schroeder DR, et al. Incidence, prevalence, and clinical course of idiopathic pulmonary fibrosis. Chest. 2010;137:129–37.
Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13–64. New definition and key concepts on the science and applications of pulmonary rehabilitation.
Global strategy for diagnosis, management, and prevention of COPD-2016 http://www.goldcopd.org/guidelines-global-strategy-for-diagnosis-management.html. Updated GOLD guidelines on COPD management.
Geddes D, Davies M, Koyama H, et al. Effect of lung-volume–reduction surgery in patients with severe emphysema. N Engl J Med. 2000;343(4):239–45.
Weill D, Benden C, Corris PA, et al. A consensus document for the selection of lung transplant candidates: 2014–an update from the Pulmonary Transplantation Council of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant. 2015;34(1):1–15. Updated lung transplant recipient criteria.
Smetana GW. Preoperative pulmonary evaluation. N Engl J Med. 1999;340(12):937–44.
Cooper BG. An update on contraindications for lung function testing. Thorax. 2010. doi:10.1136/thx.2010.139881.
Contraindications to use of spirometry. AARC clinical practice guidelines. Spirometry 1996 Update. Respir Care 1996;417:629–36.
Haynes JM. Pulmonary function test quality in the elderly: the comparison with younger adults. Respir Care. 2014;59(1):16–21. Elderly patients can be expected to achieve spirometry and DLCO quality scores comparable to younger adult patients.
Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26(5):948–68.
Hankinson JL, Odencratz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med. 1999;159:179–87.
Hardie JA, Buist AS, Vollmer WM, et al. Risk of overdiagnosis of COPD in asymptomatic elderly never smokers. Eur Respir J. 2002;20(5):1117–22.
Mannino DM, Sonia Buist A. Vollmer WM Chronic obstructive pulmonary disease in the older adult: what defines abnormal lung function? Thorax. 2007;62(3):237–41.
Kradjan WA, Driesner NK, Abuan TH, et al. Effect of age on bronchodilator response. Chest. 1992;101(6):1545–51.
Crapo RO, Casaburi R, Coates AL, et al. Guidelines for methacholine and exercise challenge testing-1999. Am J Respir Crit Care Med. 2000;161(1):309–29.
Cuttitta G, Cibella F, Bellia V, et al. Changes in FVC during methacholine induced bronchoconstriction in elderly patients with asthma: bronchial hyperesponsiveness and aging. Chest. 2001;119(6):1685–90.
de Bisschop C, Marty ML, Tessier JF. Expiratory flow limitation and obstruction in the elderly. Eur Respir J. 2005;26(4):594–601.
Pride NB. Ageing and the lung mechanics. Eur Respir J. 2005;26(4):563–5.
Mahler DA, Rosiello RA, Loke J. The aging lung. Clin Geriatr Med. 1986;2(2):215–25.
Rutten EP, Gopal P, Wouters EF, et al. Various mechanistic pathways representing the aging process are altered in COPD. Chest. 2016;149(1):53–61. Evidence supporting role of accelerated aging as pathologic mechanism for COPD.
Sala E, Roca J, Marrades RM, et al. Effects of endurance training on skeletal muscle bioenergetics in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1999;159(6):1726–34.
Casaburi R, Porszasz J, Burns MR, et al. Physiologic benefits of exercise training and rehabilitation of patients with severe chronic obstructive pulmonary disease. Am J Respir Crit Care Medicine. 1997;155(5):1541–51.
Rabinovich RA, Ardite E, Troosters T, et al. Reduced muscle redox capacity after endurance training in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Medicine e. 2001;164:1114–8.
Rabinovich RA, Figueras M, Ardite E, et al. Increased tumor necrosis factor-IL5 plasma levels during moderate-intensity exercise in COPD patients. Eur Respir J. 2003;21:789–94.
US Burden of Disease Collaborators. The state of US Health, 1990–2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591–608. 1990-2010 US health report: morbidity and chronic disability account for nearly half of the US health burden.
Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11), e442.
Laurino RA, Barnabe V, Saraiva-Romanholo BM, et al. Respiratory rehabilitation: physiotherapy approach to the control of asthma symptoms and anxiety. Clinics (Sao Paulo). 2012;67(11):1291–7. Breathing retraining can improve disease control, anxiety and health-related quality of life in asthmatic patients.
Salhi B, Troosters T, Behaegel M, et al. Effects of pulmonary rehabilitation in patients with restrictive lung diseases. Chest. 2010;137(2):273–9.
Dowman L, Hill CJ, Holland AE. Pulmonary rehabilitation for interstitial lung disease. Cochrane Database Syst Rev. 2014;10:CD006322. Pulmonary rehabilitation is safe in patients with interstitial lung disease and can improve dyspnea, exercise capacity and quality of life.
Mereles D, Ehlken N, Kreuscher S, et al. Exercise and respiratory training improve exercise capacity and quality of life in patients with severe chronic pulmonary hypertension. Circulation. 2006;114(14):1482–9.
Edvardsen E, Skjønsberg OH, Holme I, et al. High-intensity training following lung cancer surgery: a randomised controlled trial. Thorax. 2015;70(3):244–50. High intensity endurance and strength training is well tolerated after lung cancer surgery and is associated with improved outcomes.
Morano MT, Araújo AS, Nascimento FB, et al. Preoperative pulmonary rehabilitation versus chest physical therapy in patients undergoing lung cancer resection: a pilot randomized controlled trial. Arch Phys Med Rehabil. 2013;94(1):53–8. 4 weeks of PR before lung cancer resection improves preoperative functional capacity and decreases the postoperative respiratory morbidity.
Güell R, Casan P, Belda J, et al. Long-term effects of outpatient rehabilitation of COPD: a randomized trial. Chest. 2000;117(4):976–83.
Griffiths TL, Burr ML, Campbell IA, et al. Results at one year of outpatient multidisciplinary pulmonary rehabilitation: a randomized controlled trial. Lancet. 2000;355(9201):362–8.
Puhan MA, Scharplatz M, Troosters T, et al. Respiratory rehabilitation after acute exacerbation of COPD may reduce risk for readmission and mortality—a systematic review. Respir Res. 2005;6:54.
Rochester CL, Vogiatzis I, Holland AE, et al. An Official American Thoracic Society/European Respiratory Society Policy Statement: enhancing implementation, use, and delivery of pulmonary rehabilitation. Am J Respir Crit Care Med. 2015;192(11):1373–86. ATS and ERS policy recommendations to improve access to and delivery of pulmonary rehabilitation services for suitable patients.
Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1094–105.
Couser Jr JI, Guthmann R, Hamadeh MA, et al. Pulmonary rehabilitation improves exercise capacity in older elderly patients with COPD. Chest. 1995;107(3):730–4.
Turner S, Eastwood P, Cook A, et al. Improvements in symptoms and quality of life following exercise training in older adults with moderate/severe persistent asthma. Respiration. 2011;81(4):302–10.
Baltzan MA, Kamel H, Alter A, et al. Pulmonary rehabilitation improves functional capacity in patients 80 years of age or older. Can Respir J. 2004;11(6):407–13.
Crisafulli E, Costi S, Luppi F, et al. Role of comorbidities in a cohort of patients with COPD undergoing pulmonary rehabilitation. Thorax. 2008;63(6):487–92.
McCarthy B, Casey D, Devane D, et al. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2015;2:CD003793. Review of the randomized control studies which support role of pulmonary rehabilitation as an important component of the management of COPD.
Gerald LB, Sanderson B, Fish L, et al. Advance directives in cardiac and pulmonary rehabilitation patients. J Cardpulm Rehabil. 2000;20(6):340–5.
Heffner E, Fahy B, Hilling L, et al. Outcomes of advance directive education of pulmonary rehabilitation patients. Am J Respir Crit Care Med. 1997;155(3):1055–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Andreea Anton and Kavita Ratarasarn declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Pulmonology and Respiratory Care
Rights and permissions
About this article
Cite this article
Anton, A., Ratarasarn, K. Pulmonary Function Testing and Role of Pulmonary Rehabilitation in the Elderly Population with Pulmonary Diseases. Curr Geri Rep 5, 117–123 (2016). https://doi.org/10.1007/s13670-016-0164-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13670-016-0164-y