Abstract
Amyotrophic lateral sclerosis (ALS) is a rapidly progressive disorder characterized primarily by selective neurodegeneration of the motor neurons. The basis of diagnosis is the presence of signs of both upper and lower motor neuron involvement in more than one body region. ALS was considered until a few years ago a disease of young adults but recently population-based studies have consistently shown that ALS is an age-related disease with age incidence curve similar to other age-dependent neurodegenerative diseases like Parkinson’s disease and Alzheimer’s disease. The peak of incidence is in the eighth decade and declines thereafter, first in men and then in women. In the majority of cases, ALS is sporadic while 5–10 % of the disease is familiar. After the identification of C9ORF72, it is now recognized that the definition of familial ALS can be enlarged to include family members with frontotemporal dementia considering the tight link between the two nosological entities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Amyotrophic lateral sclerosis (ALS) is a rapidly progressive disorder characterized primarily by selective neurodegeneration of motor neurons. Clinical features important for diagnosis and prognosis have been defined largely in tertiary centers [1]. ALS leads to death in 15 to 20 months after diagnosis in 50 % of patients [2••], generally due to respiratory failure. An older age and bulbar involvement at onset are the main negative prognostic factors. Ten percent survives more than 10 years. Younger age, predominant upper motor neuron involvement, and longer diagnostic delay (i.e., interval between first symptoms and diagnosis) favor a long survival. For 5 % of cases, there is a family history of ALS. Among those, 60 % can probably be explained by high-risk genes. Consequences of ALS are not only neurological, but also nutritional and respiratory. Apart from symptomatic treatments, to date there are no effective therapeutic agents that significantly modify the progression of ALS. The only approved drug is riluzole, which is associated with an increase in survival of a few months. The research is now strongly focused on early diagnosis and a better definition of progression through the use of imaging and molecular biomarkers. Most of the data presented in this review are based on epidemiological studies conducted in population-based settings [3••]. Previously, studies were based primarily on data from tertiary centers where the referral tend to include the younger individuals, of male sex, and with better prognosis [4]. This methodological approach has determined the recognition of a broader spectrum of the phenotypes and the definition of ALS as an age-related disease. Within this broader spectrum of clinical phenotypes, the use of biochemical, genetic, and imaging biomarkers is in progress to provide an early diagnosis, define prognosis, and assess therapeutic intervention [5].
Diagnosis, Staging, Prognosis
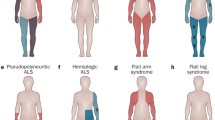
Clinical symptoms at onset are frequently non-specific: cramps, muscle weakness, fatigue, and lack of coordination. The diagnostic process can therefore be delayed. The mean diagnostic delay varies between 12 and 17 months [2••], it is probably longer in the USA, (e.g., 2.5 years) at least in Medicare data [6]. The shortest interval between first symptom and diagnosis is observed in patients with bulbar symptoms at onset like dysphagia and dysarthria. The delay is longer in subjects with clinical presentation mimicking other neurological diseases, especially more common in older subjects, such as cervical myelopathy. The most common exams used to determine the diagnosis includes magnetic resonance imaging (MRI) and computed tomography scans, electromyography, and sensory /motor nerve conduction tests [6]. ALS in older patients differs in terms of clinical presentation (i.e., more frequent bulbar onset) and prognosis (shorter survival), Table 1.
The diagnostic process improved considerably after the introduction of El Escorial Diagnostic Criteria (EEC) [7]. EEC are based only on clinical symptoms and signs and not on instrumental or laboratory data. The certainty of diagnosis (definite, probable, possible, suspected) depends on the classification of clinical signs related to the involvement of the upper and lower motor neurons and their localization in four body regions (head, trunk, superior, and inferior limbs). New criteria recommend the incorporation of electrophysiological and genetic results along with clinical data [8].
Staging systems of disease are designed to provide an objective measurement over time of the involvement of different part of the nervous system with increasing clinical severity. A proper and widely accepted staging is essential for prognosis, design of randomized clinical trials (RCT), and allocation of public resources. The critical points to be demonstrated are that most patients should progress through all or at least most of the consecutive stages and none should go back to earlier stages. There are two proposed ALS staging system:
-
1.
King’s College system is based on successive milestones in the clinical course: symptom onset, diagnosis, functional involvement of a second region and then of a third region, indication for gastrostomy and non-invasive ventilation [9].
-
2.
ALS Milano-Torino Staging is based on four functions: swallowing, walking/self-care, communicating and breathing. There are 5 stages that capture the observed progressive loss of independence and function and are based on the number of domains in which independence is lost [10]. Stage 0 corresponds to functional involvement but no loss of independence on any domain and stage 5 is death.
Both systems are still in the process of validation in different setting and populations.
The prognosis of ALS is very severe with death generally between 2 to 5 years: older age (e.g., ≥80 years) and bulbar involvement at onset are the main negative prognostic factors. Ten percent survives more than 10 years: younger age at onset (less than 45 years), predominant upper motor neuron involvement, longer interval onset diagnosis [11] determine a longer survival.
About 50 % of subjects with ALS have cognitive impairment at onset. Subjects with cognitive abnormalities have a poorer prognosis with worse disability, faster rates of motor decline, and higher mortality [12]. Normal cognition at baseline is associated with tendency to keep preserved cognitive functions until death. To date, no clear relationship has been identified between age and prevalence of ALS-associated frontotemporal dementia.
Nutrition and Respiratory Involvement in ALS
Consequences of ALS are not only neurological, but also nutritional and respiratory. Decreased food intake and higher energy expenditure may well promote the development of a state of malnutrition [13]. Decreased food intake is caused by swallowing and salivation disorders, frequent anorexia or constipation, modification of taste, problems due to possible respiratory insufficiency, and difficulties in activities of daily living such as shopping, cooking, or putting food into the mouth.
ALS patients progressively lose lean mass (LM) that should produce a decrease of resting energy expenditure (REE). However, 50 to 70 % of sporadic cases and all familial are characterized by an opposite phenomenon, hypermetabolism [14, 15], defined by a REE of 110 % or more of the theoretical value. Loss of weight and of body mass index (BMI) has been described at various times during the ALS course. Weight loss appears moderate (10 % of weight loss) to severe (20 %) in 25 to 30 % of patients [16] and estimates of the prevalence of malnutrition vary widely (between 10 and 30 %). The definitions of malnutrition are diverse and assessments have been made at different times in the course of the disease (Table 2). Relation between malnutrition and weight loss with sex and age has, to date, not been assessed. Other markers such as phase angle assessed by bioimpedance analysis appear dramatically reduced as compared to controls, reflecting severe cellular alterations. Disorders of lipid status are possible but inconsistent across studies and perhaps linked with cultural dietary habits [17, 18].
Malnutrition is associated with an eightfold increase in the risk of death [16]. Low BMI measured during follow-up [14], before gastrostomy placement [13], and weight loss at time of diagnosis are associated with a shorter survival [19••]. During the natural history of ALS, a higher level of fat as measured by fat mass using bioimpedance seems to be a positive factor for survival. Hypertriglyceridemia and hypercholesterolemia have been associated with better clinical evolution [20] and increased survival [17].
These data emphasize the prognostic value of nutritional assessment in the early stages after diagnosis and the therapeutic indication to increase the fat mass.
Likewise, respiratory involvement is present in almost all cases at some stage of the illness and is characterized by a rapid evolution with a strong impact on prognosis. Respiratory insufficiency is the commonest cause of death in ALS. The importance of a regular respiratory evaluation is related to the vital prognosis associated thereto. Respiratory function assessed at time of diagnosis is a major prognostic factor for survival of patients. This function is usually assessed using forced vital capacity (FVC) (expressed as % of predicted value) [21]. Respiratory symptoms appear only when FVC is lower than 50 % of the normal value. Decline of respiratory function, described as a linear phenomenon, was associated with survival in population-based [22], clinical series and RCT. Nevertheless, the sensitivity of FVC to identify alteration of inspiratory function is low, as studies have found significant alteration of inspiratory force in patients with normal vital capacity. Patients with bulbar muscle weakness might have difficulties performing spirometry because of facial muscular paresis, making FVC measurement challenging. Sniff nasal inspiratory pressure (SNIP) is another system better suited than FVC to evaluate respiratory failure [23, 24] and is a good indicator also of intra-thoracic pressures. SNIP is the best predictor of death or tracheostomy within 1-year of follow-up (adjusted HR of 10 for a SNIP <18 cmH20 as compared to >51 cmH20 [25••]. SNIP can be used in patients with bulbar dysfunction, as it does not require a seal around a mouthpiece. Other respiratory measures such as maximum expiratory and inspiratory pressure have been associated with survival [26].
The clinical importance of nutritional and respiratory status underlines the need for multidisciplinary care of the ALS patient as stated both in European and US guidelines [27, 28].
Epidemiology
Most of new evidence in the epidemiology of ALS is based on population-based registries, based mainly in Europe [3••]. ALS epidemiological studies are particularly difficult because of the heterogeneity of clinical phenotypes, especially at onset; absence of valid biomarkers; and uncertainties of the clinical diagnostic criteria (EEC and revised EEC). An additional issue compared with the other most common neurodegenerative diseases (Alzheimer’s disease, Parkinson’s disease) is that ALS is a rare disease with low incidence and prevalence. Recent work has shown that incidence of ALS can be as high as about 3/100,000, using the capture-recapture method to take into account different sources of patient referral to estimate the number of missed cases [36•].
Several studies have shown heterogeneity of the incidence rates across Europe, indicating a possible lower incidence in Mediterranean countries like Southern Italy, Sicily, and Catalonia [37–39]. Bulbar onset in the data from EURALS, the consortium of European population-based registries are more common in Ireland (more than 40 %) than in Italy (30 %) [3••].
Male/female ratio in most recent studies in Europe is around one but was 2:1 in the studies in the 1960s and in recent studies from countries in Africa and South America.
ALS was considered a disease of young adults but in population-based studies. ALS is an age-related disease with age incidence curve similar to other age-dependent neurodegenerative diseases like Parkinson’s disease. The peak of incidence is in the eighth decade and declines thereafter, first in men and then in women (Fig. 1). ALS patients older than age 80 are largely with bulbar onset and survive on average 6 months less than younger patients (Table 1) [40]. The likelihood that an elderly ALS patient is prescribed riluzole, PEG, or is referred to a neurologist is low.
The overall lifetime risk for ALS is around 1:400 for men and slightly lower for women. Familial ALS (fALS) cases are about 5–10 % in clinical setting, while it is close to 5 % in population-based studies [2••, 41].
The risk of ALS in families is much higher (twice) in first-degree males than females, and no increase in risk is present in distant relatives [42]. Incidence in Asian and African countries is lower. Mixed populations show lower incidence as measured by mortality compared to whites and black [2••,43].
The analyses of time trends in Europe and the USA show clearly that ALS incidence is rapidly increasing: in recent data from Denmark, of 2 % per year in the last 30 years. The increase is stronger over age 70 [44•]. The first explanation of this trend is the increased life-span. A possible role of reduced penetrance of some genes and a different distribution of environmental risk factors as shown by the change of sex ratio in the same period are hiyotheses that need further exploration.
Genetic Biomarkers
In the majority of cases, ALS is sporadic (sALS), while, part of familial aggregation (fALS) is probably due to a genetic effect. It is now recognized that the definition of fALS can be enlarged, including family members with frontotemporal dementia (FTD), considering the tight link between the two nosological entities [45]. It must be noted that fALS might be underrepresented in ALS patients, because of inadequate recording of family history, early death due to other causes, misdiagnosis, small family sizes and illegitimacy, or because of low penetrance of the Mendelian causative genes. An oligogenic hypothesis has recently been proposed for fALS with Mendelian inheritance [46]. Based on this model, mutations in two or more genes are required for an individual for disease manifestation. This hypothesis is supported by reports of patients with mutations in more than one ALS-associated gene [47, 48].
Genetically, fALS are associated with a large number of pleiotropic genes whose mutations impair different biochemical pathways, resulting in overlapping clinical and pathological phenotypes. Mutations in large-effect genes associated with fALS may be detected in cases with sALS. Overall, phenotypic characteristics are often indistinguishable between mutation carriers and non-carriers. Table 3 shows the most common high penetrance genes involved in the pathogenesis of ALS, along with the corresponding cellular pathways impaired and the age of onset (range). The molecular genetics of ALS started in 1993 when Rosen and colleagues identified mutations in the superoxide dismutase-1 (SOD1) gene as causative of fALS [49]. For more than one decade, SOD1 was thought to be the primary genetic cause of fALS and sALS, although it accounts for only 12 % of fALS and 1 % of sALS [50]. In 2008 and 2009, two other causative genes were discovered: TAR DNA-binding protein (TARDBP) on chromosome 1 [51] and fused in sarcoma/translated in liposarcoma (FUS/TLS) on chromosome 16 [52] that increased the understanding of the pathogenesis of ALS, but did not change considerably the known heritability of ALS. The turning point was in 2011 when two groups simultaneously reported the finding of a noncoding GGGGCC hexanucleotide repeat expansion in C9ORF72, which co-segregated with ALS, spell out FTD, and ALS-FTD [53••,54••]. The mutations seem to be geographically clustered in Europe and North America where the mutation is present in about a third of fALS cases. Mutations in C9ORF72 seem associated with a specific phenotype of ALS, with earlier age of onset, more malignant course of disease, a bulbar onset, and a frequent occurrence of psychotic symptoms. However, characteristics of age at onset of C9ORF72 as well as other genotypes are discordant.
Results from genome-wide association studies (GWAS) are often conflicting. They have been useful to identify genetic susceptibility loci but most of them failed to be replicated in different populations. In addition to searching for susceptibility loci, there have been GWA efforts to identify genetic variants influencing ALS phenotype. For example, genetic variation in the KIFAP3 and EPHA4 loci has been reported to significantly influence survival among ALS patients [55, 56], and a large meta-analysis of ALS GWAS recently reported that age of onset is modulated by a locus on the short arm of chromosome 1 [57].
It has been proposed that with the discovery of C9ORF72, about 60 % of the heritability of fALS and 10 % of the heritability of sALS can now be explained [53••]. Nevertheless, twin studies have estimated the genetic component of sALS at 0.61 (range 0.38–0.78) [58], underlining that a large part of the heritability of ALS is still unknown. Furthermore, the majority of ALS genetic research has been largely focused on European populations, and other ethnicities have been only recently studied, showing that genetic architecture of ALS is probably different in populations of different ancestral origin.
Biochemical Biomarkers
Both early diagnosis and prognostication remain elusive in ALS despite the availability of diagnostic criteria and functional rating scales which capture the extension, severity, and phenotypic expression of the disease, based on clinical and neurophysiological evaluations [8, 59]. To improve this largely ineffective approach, the identification and validation of disease-specific biological signals to be used for disease recognition and monitoring is critical. The added value of novel disease biomarkers in ALS is also in the pharmacodynamic potential they offer and in the opportunity they provide to design more cost-effective RCT. Only recently, neurochemical biomarkers have started shaping new ways to monitor disease progression and to predict survival in ALS but they have not gone far enough to provide any means for early disease recognition and had so far no real impact on diagnostic latency [60]. The main stumbling block in this research has been the significant clinical heterogeneity in ALS, whereby rate of progression can vary significantly with a protean clinical presentation dominated by either bulbar or spinal features from disease onset [61]. Arguably, a neurochemical marker’s adoption in clinic requires also complex procedures of analytical and pre-clinical validation. In addition, while cerebrospinal fluid (CSF) is the natural biorepository of any product of neuroaxonal disintegration and the ideal biofluid for biomarkers discovery, lumbar punctures become impractical in advanced ALS patients when serial sampling for treatment monitoring is needed. The limitation imposed by CSF collection has also emerged in recent studies where cross-sectional analysis of biomarkers to define their ALS-specificity against healthy control or other ALS-mimicking syndromes has been extended to incorporate the study of the same markers throughout the disease trajectory in longitudinal studies [62, 63]. The latter approach seems relevant when looking at the natural history of any biological signal of disease, when the endpoint is, for example, the change of the same biomarker after the administration of neurorestorative treatments.
In the case of neurofilaments (Nf), blood measurements have started only recently to be a feasible alternative to CSF analyses, despite a number of technical challenges that any measurement in this complex matrix implies [63–69]. Nf are among the most stable neuroaxonal component released in biological fluids upon neuronal disintegration and have emerged as leading blood and CSF “universal” markers of axonal loss in ALS and in other neurodegenerative conditions [62, 63, 65, 66]. Studies have gone some way towards the goal of providing both cross-sectional and longitudinal data matched against the rate of progression [63–67, 70, 71]. The choice of a more accessible albeit complex matrix like blood poses analytical challenges including Nf aggregation causing epitope masking and reducing detection by antibody-based techniques andautoimmunity to Nf with an increase of antibodies against Nf in advanced stages of the disease which have a possible Nf-clearing effect from circulation [66, 67, 72].
Tentative neurochemical biomarkers with prognostic values in ALS have encompassed a wide range of moieties, either directly linked to neuroaxonal disintegration (e.g., Nf) or related to the immune response to the process of neurodegeneration as well as to metabolic alterations believed to be intrinsic to the disease process [20, 73, 74]. It has become clear that the immune response to neurodegeneration in ALS could provide clues to the stage and progression of ALS [73]. The expression of immune mediators like cytokines and acute phase reactants change with the disease progression while the immunological profile of the disease may be dominated by a change in immunotolerance with a raising adaptive immune response after the initial innate reaction to the pathology [72, 73, 75]. Another important step towards establishing a biomarker of ALS by immunomonitoring is the discovery of a profound T regulatory cell (treg) downregulation in individuals with ALS, particularly in those who present a faster disease progression [74]. The identification of markers of inflammation has gone in parallel with the characterization of other signatures of disease progression, which relate to metabolism. Hypermetabolism has been found to correlate with the disease process in association with lipid dysmetabolism, and these findings taken together may provide an additional prognostic biomarker [20].
The relative absence of published data on the role of disease biomarkers to monitor treatment response in ALS is mitigated by a few published pilot studies. CSF analysis to evaluate pioglitazone HCl and tretinoin treatment in ALS by measurement of the levels of CSF tau and phosphorilated neurofilament heavy chain (pNFH) were undertaken [76]. Over 6 months of therapy, CSF tau levels decreased in subjects randomized to active treatment and increased in subjects on placebo, while the rate of disease progression was strongly correlated with levels of pNFH in the CSF at baseline. In an animal model of the disease, treatment with arimoclomol with a confirmed motor cell-sparing effect was associated with a steady reduction of the area under the curve of plasma NfH and increased survival in these animals [67].
As in other neurodegenerative conditions, the future of biomarkers in ALS lies in a proper multi-modal approach, whereby a panel of neurochemical markers of disease progression is combined with imaging improving diagnostic potency. This composite biomarker has not as yet been produced in ALS and each domain of investigation has so far progressed rather independently providing a fragmented picture of the pathogenesis and limited information on survival and prognosis [60, 77].
Imaging
Conventional MRI is not informative in the most ALS patients and is essentially useful in excluding disorders that have symptoms mimicking ALS. Neuroimaging studies using advanced quantitative MR techniques and PET much increased in the last years, in the attempt to provide pathophysiological information, diagnostic tools, and biomarkers of progression [78]. Many studies focused on gray matter pathology, mostly using voxel-based [79••,80, 81] or surface-based morphometry [82, 83], revealing cortical atrophy of the primary motor cortex, but also of extra-motor regions, as at the level of the frontotemporal and parietal cortex, correlated with the presence of cognitive dysfunctions. Notably, longitudinal analysis revealed progressive and widespread changes in the gray matter, including the basal ganglia, in contrast with a limited white matter pathology progression [79••], with implications for the development of effective imaging biomarkers. Neuronal loss in the motor cortex was also detected using 1H-magnetic resonance spectroscopy (1H-MRS), showing reduced N-acetylaspartate (NAA) concentrations or NAA/creatine ratio, with high sensitivity (86 %) but low specificity (37 %) to detect upper motor neuron signs [84]. 1H-MRS findings also suggested an imbalance between excitatory (raised glutamate-glutamine) and inhibitory (reduced GABA) signaling [85].
Pathological abnormalities at the level of white matter fibers, mainly the corticospinal tracts and middle-posterior parts of the corpus callosum, were reported by a great number of diffusion tensor (DTI) studies, in terms of decreased fractional anisotropy and increased mean diffusivity, and correlated to clinical severity and rate of disease progression [78] [79••,86]. An individual patient data meta-analysis, reviewing all DTI studies, compared mean cerebral corticospinal tract fractional anisotropy values between ALS subjects and controls, and calculated diagnostic accuracy with pooled sensitivity of 65 % and pooled specificity of 67 % [87•]. As for gray matter pathology, also white matter pathology extended beyond motor pathways. Indeed, DTI abnormalities, other than corticospinal tracts and corpus callosum, involved long association white matter tracts bilaterally, as cingulum, inferior longitudinal, inferior fronto-occipital, and uncinate fasciculi, and were associated with changes in cognitive functions [88].
Degeneration of the corticospinal tracts leads to damage of the cervical cord, which was reported by studies using spinal cord MRI, in terms of atrophy [89], DTI abnormalities [90], and reduced NAA to creatine ratio [91]. DTI abnormalities were greater changed at more distal cervical segments, supporting the dying back hypothesis of neurodegeneration in ALS [92].
An increasing number of neuroimaging studies investigated functional and structural connectivity in ALS patients by using resting state fMRI and DT-tractography analyses, reporting decreased functional connectivity within the sensorimotor network and in brain networks related to cognition and behavior [78], which paralleled the structural connectivity changes in the same networks [93]. An increased functional connectivity of sensorimotor networks was also reported, specifically in those ALS patients with less severe corticospinal tract DTI changes, suggesting an initial attempt to compensate for the structural damage. Such higher functional connectivity might be also related to pathogenic loss of local inhibitory circuitry, as supported by the decreased uptake of the PET marker of benzodiazepine receptor 11C-flumazenil seen in the primary motor cortex and frontal cortex of ALS patients [94].
Finally, 18 F-FDG-PET seems to be a promising biomarker for diagnosis. It was able to detect motor and extra-motor hypometabolism and brainstem and medial temporal cortex hypermetabolism, providing a very high accuracy in discriminating patients with ALS from controls [95].
Therapy
To date there are no effective therapeutic agents that significantly contrast the progression of ALS. The only approved drug is riluzole that showed a substantial improvement in survival at 1 year in a randomized clinical trial (RCT) conducted in 1993–1994 on 155 outpatients with ALS [96], and in subsequent RCT [97–99]. As a consequence, the search for new and better treatment strategies for ALS is a top priority. The aim is to find additional treatments that have cumulative effects to riluzole and that can stop the disease process in an early stage. Numerous distinct therapeutic interventions have been examined but currently ALS does not have a cure or an efficacious treatment. This is probably due to the extreme heterogeneity of the disease in terms of phenotype, genetic predisposition, pathogenesis, and involved pathophysiological pathways. This could also be due in some extent to the inclusion in RCT of selected subset of patients, with better prognosis factors (including younger age), as a consequence of restrictive inclusion criteria and recruitment founded on referral centers. Those patients who are not representative of the entire ALS population could be less prone to benefit from experimental drugs. Also, available transgenic mouse models for ALS do not represent the entire spectrum of the disease. Consequently, all the drugs that had showed promising results in animal models failed to replicate efficacy in phase II and phase III RCT in humans. The most recent example is dexpramipexole, a free-radical scavenger, with an effect on mitochondrial dysfunction, which prolonged the life-span of ALS-SOD1 transgenic mice [100], was well tolerated and showed a moderate affect in phase II RCT [101], but failed to produce beneficial results in the recent phase III RCT [102]. Small phase II RCT are more likely to involve small homogeneous subgroups more responsive to the trial drug. Specific post hoc analyses that take into account factors of heterogeneity, simultaneous testing of different drugs with different therapeutic targets, and use of biomarkers of therapeutic response can be some examples of methods to improve RCT design in ALS.
Research conducted in the last decade has provided insights in the biological mechanisms of the disease, and novel therapeutic targets have been identified. Stem cells, in particular induced pluripotent stem cells (iPSC), represented one of the major tools in the fight against ALS. Patient-derived iPSC can be used to generate individual-specific disease models to find novel therapies [103], and can provide an autologous transplant source that can produce motor neurons [104]. Gene therapy, using antisense oligonucleotides or small interfering RNAs, seems to be promising. In other neurodegenerative diseases (Huntington’s disease and two types of spinocerebellar ataxia (SCA), it has been demonstrated that the expression of the mutant protein can be silenced and this could halt and even reverse the disease phenotype [105, 106]. Furthermore, mutant proteins can be cleared by specifically designed antibodies. Passive and active immunization against misfolded SOD1 shows therapeutic potential in mouse models [107].
Developing a causal therapy that targets a specific disease-causing gene can have a huge effect by preventing the pathological events responsible for the disease. However, only a limited number of patients affected by ALS might benefit from this type of therapy. Another approach can be targeting each pathogenic process that is involved in ALS such as non-neuronal cell alterations, mitochondrial dysfunction, deregulated autophagy, and/or axonal transport dysfunction. Most likely, the effect of such a modifying treatment will be smaller compared to that of a causal treatment, but the target population will be larger as all ALS patients could benefit from this treatment. In order to achieve a more prominent effect, future approaches will combine different modifying therapies to have an additive and hopefully even a synergistic effect.
Conclusions
The phenotype definition and understanding of the pathogenesis of ALS has considerably improved in the last few years. However, the improved survivorship due to the only licensed drug, riluzole, in the real world is really disappointing, only 2–3 months. The future is largely based on the development of new molecular and imaging biomarkers to effect early detection and improve follow-up. The appropriate definition of risk due to the genes associated with sporadic forms and the possible role of environmental risk factors are areas for research. The ALS trials have tested more than 100 compounds in animal and human experiments with an impressive series of failures [108]. ALS trials have been shown to select patients with better prognosis [109]. Future trials will benefit from the inclusion of samples representative of the entire phenotype spectrum.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Logroscino G, Traynor BJ, Hardiman O, Chio A, Couratier P, Mitchell JD, et al. Descriptive epidemiology of amyotrophic lateral sclerosis: new evidence and unsolved issues. J Neurol Neurosurg Psychiatry. 2008;79(1):6–11.
Marin B, Boumediene F, Logroscino G, Labrunie A, Babron MC, Leutenneger AL. Population ancestral origin in Amyotrophic Lateral Sclerosis incidence, phenotype, and outcome. J Neurol Neurosurg Psychiatry. 2015. This meta-analysis reports main aspects of ALS incidence and phenotype produced to date by worldwide population-based studies (fALS, age at onset and diagnosis, sex ratio, bulbar onset, comorbidities, survival time) and considers variations by sub-continents.
Logroscino G, Traynor BJ, Hardiman O, Chio A, Mitchell D, Swingler RJ, et al. Incidence of amyotrophic lateral sclerosis in Europe. J Neurol Neurosurg Psychiatry. 2010;81(4):385–90. This is the first collaborative collection of incident cases of population- based studies in Europe.
Lee JR, Annegers JF, Appel SH. Prognosis of amyotrophic lateral sclerosis and the effect of referral selection. J Neurol Sci. 1995;132(2):207–15.
Otto M, Bowser R, Turner M, Berry J, Brettschneider J, Connor J, et al. Roadmap and standard operating procedures for biobanking and discovery of neurochemical markers in ALS. Amyotroph Lateral Scler. 2012;13(1):1–10.
Williams JR, Fitzhenry D, Grant L, Martyn D, Kerr DA. Diagnosis pathway for patients with amyotrophic lateral sclerosis: retrospective analysis of the US Medicare longitudinal claims database. BMC Neurol. 2013;13:160.
Brooks BR. El Escorial World Federation of Neurology Criteria for the Diagnosis of Amyotrophic Lateral Sclerosis. Subcommittee on Motor Neuron Diseases/Amyotrophic Lateral Sclerosis of the World Federation of Neurology Research Group on Neuromuscular Diseases and the El Escorial "Clinical Limits of Amyotrophic Lateral Sclerosis" Workshop Contributors. J Neurol Sci. 1994;124:Suppl:96–107.
Costa J, Swash M, de Carvalho M. Awaji criteria for the diagnosis of amyotrophic lateral sclerosis: a systematic review. Arch Neurol. 2012;69(11):1410–6.
Roche JC, Rojas-Garcia R, Scott KM, Scotton W, Ellis CE, Burman R, et al. A proposed staging system for amyotrophic lateral sclerosis. Brain. 2012;135(Pt 3):847–52.
Chio A, Hammond ER, Mora G, Bonito V, Filippini G. Development and evaluation of a clinical staging system for amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry. 2015;86(1):38–44.
Zoccolella S, Beghi E, Palagano G, Fraddosio A, Guerra V, Samarelli V, et al. Predictors of long survival in amyotrophic lateral sclerosis: a population-based study. J Neurol Sci. 2008;268(1–2):28–32.
Phukan J, Elamin M, Bede P, Jordan N, Gallagher L, Byrne S, et al. The syndrome of cognitive impairment in amyotrophic lateral sclerosis: a population-based study. J Neurol Neurosurg Psychiatry. 2012;83(1):102–8.
Desport JC, Preux PM, Truong CT, Courat L, Vallat JM, Couratier P. Nutritional assessment and survival in ALS patients. Amyotroph Lateral Scler Other Motor Neuron Disord. 2000;1(2):91–6.
Desport JC, Torny F, Lacoste M, Preux PM, Couratier P. Hypermetabolism in ALS: correlations with clinical and paraclinical parameters. Neurodegener Dis. 2005;2(3–4):202–7.
Funalot B, Desport JC, Sturtz F, Camu W, Couratier P. High metabolic level in patients with familial amyotrophic lateral sclerosis. Amyotroph Lateral Scler. 2009;10(2):113–7.
Desport JC, Preux PM, Truong TC, Vallat JM, Sautereau D, Couratier P. Nutritional status is a prognostic factor for survival in ALS patients. Neurology. 1999;53(5):1059–63.
Dupuis L, Corcia P, Fergani A, Gonzalez De Aguilar JL, Bonnefont-Rousselot D, Bittar R, et al. Dyslipidemia is a protective factor in amyotrophic lateral sclerosis. Neurology. 2008;70(13):1004–9.
Chio A, Calvo A, Ilardi A, Cavallo E, Moglia C, Mutani R, et al. Lower serum lipid levels are related to respiratory impairment in patients with ALS. Neurology. 2009;73(20):1681–5.
Marin B, Desport JC, Kajeu P, Jesus P, Nicolaud B, Nicol M, et al. Alteration of nutritional status at diagnosis is a prognostic factor for survival of amyotrophic lateral sclerosis patients. J Neurol Neurosurg Psychiatry. 2011;82(6):628–34. This work investigated for the first time the relation between weight loss at time of diagnosis and survival, highlighting the importance to consider nutritional aspects as soon as possible.
Ikeda K, Hirayama T, Takazawa T, Kawabe K, Iwasaki Y. Relationships between disease progression and serum levels of lipid, urate, creatinine and ferritin in Japanese patients with amyotrophic lateral sclerosis: a cross-sectional study. Intern Med. 2012;51(12):1501–8.
Stambler N, Charatan M, Cedarbaum JM. Prognostic indicators of survival in ALS ALS CNTF Treatment Study Group. Neurology. 1998;50(1):66–72.
Chio A, Mora G, Leone M, Mazzini L, Cocito D, Giordana MT, et al. Early symptom progression rate is related to ALS outcome: a prospective population-based study. Neurology. 2002;59(1):99–103.
Chio A, Logroscino G, Hardiman O, Swingler R, Mitchell D, Beghi E, et al. Prognostic factors in ALS: a critical review. Amyotroph Lateral Scler. 2009;10(5–6):310–23.
Morgan RK, McNally S, Alexander M, Conroy R, Hardiman O, Costello RW. Use of sniff nasal-inspiratory force to predict survival in amyotrophic lateral sclerosis. Am J Respir Crit Care Med. 2005;171(3):269–74.
Capozzo R, Quaranta VN, Pellegrini F, Fontana A, Copetti M, Carratu P, et al. Sniff nasal inspiratory pressure as a prognostic factor of tracheostomy or death in amyotrophic lateral sclerosis. J Neurol. 2014. This work investigated various methods of investigation respiratory function. It identified Sniff test as the best predictor of death or tracheostomy within 1 year of follow-up.
Schmidt EP, Drachman DB, Wiener CM, Clawson L, Kimball R, Lechtzin N. Pulmonary predictors of survival in amyotrophic lateral sclerosis: use in clinical trial design. Muscle Nerve. 2006;33(1):127–32.
Andersen PM, Abrahams S, Borasio GD, de Carvalho M, Chio A, Van Damme P, et al. EFNS guidelines on the clinical management of amyotrophic lateral sclerosis (MALS)—revised report of an EFNS task force. Eur J Neurol. 2012;19(3):360–75.
Miller RG, Jackson CE, Kasarskis EJ, England JD, Forshew D, Johnston W, et al. Practice parameter update: the care of the patient with amyotrophic lateral sclerosis: drug, nutritional, and respiratory therapies (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2009;73(15):1218–26.
Mazzini L, Corrà T, Zaccala M, Mora G, Del Piano M, Galante M. Percutaneous endoscopic gastrostomy and enteral nutrition in amyotrophic lateral sclerosis. J Neurol. 1995;242(10):695–8.
Jesus P, Massoulard A, Marin B, Nicol M, Laplagne O, Baptiste A, Gindre-Poulvelarie L, Couratier P, Fraysse JL, Desport JC. First assessment at home of amyotrophic lateral sclerosis (ALS) patients by a nutrition network in the French region of Limousin. Amyotroph Lateral Scler. 2012;13(6):538–43.
Bouteloup C, Desport JC, Clavelou P, Guy N, Derumeaux-Burel H, Ferrier A, Couratier P. Hypermetabolism in ALS patients: an early and persistent phenomenon. J Neurol. 2009;256(8):1236–42.
Worwood AM, Leigh PN. Indicators and prevalence of malnutrition in motor neurone disease. Eur Neurol. 1998;40(3):159–63.
Limousin N, Blasco H, Corcia P, Gordon PH, De Toffol B, Andres C, Praline J. Malnutrition at the time of diagnosis is associated with a shorter disease duration in ALS. J Neurol Sci. 2010;297(1–2):36–9.
Slowie LA, Paige MS, Antel JP. Nutritional considerations in the management of patients with amyotrophic lateral sclerosis (ALS). J Am Diet Assoc. 1983;83(1):44–7.
Meininger V, Bensimon G, Lacomblez L, Salachas F. Natural history of amyotrophic lateral sclerosis. A discussion. Adv Neurol 1995;68:199–207.
Marin B, Hamidou B, Couratier P, Nicol M, Delzor A, Raymondeau M, et al. Population-based epidemiology of amyotrophic lateral sclerosis (ALS) in an ageing Europe—the French register of ALS in Limousin (FRALim register). Eur J Neurol. 2014;21(10):1292–300. This work performed in a region of France characterized by an old population (30% of subjects older than 60 years) identified a crude ALS incidence as high as 3.2/100,000 person-year of follow-up.
Pradas J, Puig T, Rojas-Garcia R, Viguera ML, Gich I, Logroscino G. Amyotrophic lateral sclerosis in Catalonia: a population based study. Amyotroph Lateral Scler Frontotemporal Degener. 2013;14(4):278–83.
Ragonese P, Cellura E, Aridon P, D’Amelio M, Spataro R, Taiello AC, et al. Incidence of amyotrophic lateral sclerosis in Sicily: a population based study. Amyotroph Lateral Scler. 2012;13(3):284–7.
Logroscino G, Beghi E, Zoccolella S, Palagano R, Fraddosio A, Simone IL, et al. Incidence of amyotrophic lateral sclerosis in southern Italy: a population based study. J Neurol Neurosurg Psychiatry. 2005;76(8):1094–8.
Forbes RB, Colville S, Swingler RJ. The epidemiology of amyotrophic lateral sclerosis (ALS/MND) in people aged 80 or over. Age Ageing. 2004;33(2):131–4.
Byrne S, Walsh C, Lynch C, Bede P, Elamin M, Kenna K, et al. Rate of familial amyotrophic lateral sclerosis: a systematic review and meta-analysis. J Neurol Neurosurg Psychiatry. 2011;82(6):623–7.
Gibson SB, Figueroa KP, Bromberg MB, Pulst SM, Cannon-Albright L. Familial clustering of ALS in a population-based resource. Neurology. 2014;82(1):17–22.
Zaldivar T, Gutierrez J, Lara G, Carbonara M, Logroscino G, Hardiman O. Reduced frequency of ALS in an ethnically mixed population: a population-based mortality study. Neurology. 2009;72(19):1640–5.
Seals RM, Hansen J, Gredal O, Weisskopf MG. Age-period-cohort analysis of trends in amyotrophic lateral sclerosis in Denmark, 1970-2009. Am J Epidemiol. 2013;178(8):1265–71. This age-period-cohort analysis identified a 2% annual increment in the adjusted incidence of ALS in Denmark. Consistent results were obtained for mortality rates.
Byrne S, Bede P, Elamin M, Kenna K, Lynch C, McLaughlin R, et al. Proposed criteria for familial amyotrophic lateral sclerosis. Amyotroph Lateral Scler. 2011;12(3):157–9.
van Blitterswijk M, van Es MA, Hennekam EA, Dooijes D, van Rheenen W, Medic J, et al. Evidence for an oligogenic basis of amyotrophic lateral sclerosis. Hum Mol Genet. 2012;21(17):3776–84.
Daoud H, Valdmanis PN, Gros-Louis F, Belzil V, Spiegelman D, Henrion E, et al. Resequencing of 29 candidate genes in patients with familial and sporadic amyotrophic lateral sclerosis. Arch Neurol. 2011;68(5):587–93.
Luigetti M, Lattante S, Zollino M, Conte A, Marangi G, Del Grande A, et al. SOD1 G93D sporadic amyotrophic lateral sclerosis (SALS) patient with rapid progression and concomitant novel ANG variant. Neurobiol Aging. 2011;32(10):1924.
Rosen DR, Siddique T, Patterson D, Figlewicz DA, Sapp P, Hentati A, et al. Mutations in Cu/Zn superoxide dismutase gene are associated with familial amyotrophic lateral sclerosis. Nature. 1993;362(6415):59–62.
Chio A, Traynor BJ, Lombardo F, Fimognari M, Calvo A, Ghiglione P, et al. Prevalence of SOD1 mutations in the Italian ALS population. Neurology. 2008;70(7):533–7.
Sreedharan J, Blair IP, Tripathi VB, Hu X, Vance C, Rogelj B, et al. TDP-43 mutations in familial and sporadic amyotrophic lateral sclerosis. Science. 2008;319(5870):1668–72.
Vance C, Rogelj B, Hortobagyi T, De Vos KJ, Nishimura AL, Sreedharan J, et al. Mutations in FUS, an RNA processing protein, cause familial amyotrophic lateral sclerosis type 6. Science. 2009;323(5918):1208–11.
Renton AE, Majounie E, Waite A, Simon-Sanchez J, Rollinson S, Gibbs JR, et al. A hexanucleotide repeat expansion in C9ORF72 is the cause of chromosome 9p21-linked ALS-FTD. Neuron. 2011;72(2):257–68. This paper represents a real turning point in the genetics of ALS.
DeJesus-Hernandez M, Mackenzie IR, Boeve BF, Boxer AL, Baker M, Rutherford NJ, et al. Expanded GGGGCC hexanucleotide repeat in noncoding region of C9ORF72 causes chromosome 9p-linked FTD and ALS. Neuron. 2011;72(2):245–56. This paper represents a real turning point in the genetics of ALS.
Landers JE, Melki J, Meininger V, Glass JD, van den Berg LH, van Es MA, et al. Reduced expression of the kinesin-associated protein 3 (KIFAP3) gene increases survival in sporadic amyotrophic lateral sclerosis. Proc Natl Acad Sci U S A. 2009;106(22):9004–9.
Van Hoecke A, Schoonaert L, Lemmens R, Timmers M, Staats KA, Laird AS, et al. EPHA4 is a disease modifier of amyotrophic lateral sclerosis in animal models and in humans. Nat Med. 2012;18(9):1418–22.
Ahmeti KB, Ajroud-Driss S, Al-Chalabi A, Andersen PM, Armstrong J, Birve A, et al. Age of onset of amyotrophic lateral sclerosis is modulated by a locus on 1p34.1. Neurobiol Aging. 2013;34(1):357. e7-19.
Al-Chalabi A, Fang F, Hanby MF, Leigh PN, Shaw CE, Ye W, et al. An estimate of amyotrophic lateral sclerosis heritability using twin data. J Neurol Neurosurg Psychiatry. 2010;81(12):1324–6.
Brooks BR, Miller RG, Swash M, Munsat TL. El Escorial revisited: revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotroph Lateral Scler Other Motor Neuron Disord. 2000;1(5):293–9.
Bowser R, Turner MR, Shefner J. Biomarkers in amyotrophic lateral sclerosis: opportunities and limitations. Nat Rev Neurol. 2011;7(11):631–8.
Kiernan MC, Vucic S, Cheah BC, Turner MR, Eisen A, Hardiman O, et al. Amyotrophic lateral sclerosis. Lancet. 2011;377(9769):942–55.
Gaiottino J, Norgren N, Dobson R, Topping J, Nissim A, Malaspina A, et al. Increased neurofilament light chain blood levels in neurodegenerative neurological diseases. PLoS One. 2013;8(9):e75091.
Boylan KB, Glass JD, Crook JE, Yang C, Thomas CS, Desaro P, et al. Phosphorylated neurofilament heavy subunit (pNF-H) in peripheral blood and CSF as a potential prognostic biomarker in amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry. 2013;84(4):467–72.
Tortelli R, Ruggieri M, Cortese R, D’Errico E, Capozzo R, Leo A, et al. Elevated cerebrospinal fluid neurofilament light levels in patients with amyotrophic lateral sclerosis: a possible marker of disease severity and progression. Eur J Neurol. 2012;19(12):1561–7.
Tortelli R, Copetti M, Ruggieri M, Cortese R, Capozzo R, Leo A, et al. Cerebrospinal fluid neurofilament light chain levels: marker of progression to generalized amyotrophic lateral sclerosis. Eur J Neurol. 2014;22:215–8.
Lu CH, Petzold A, Topping J, Allen K, Macdonald-Wallis C, Clarke J, et al. Plasma neurofilament heavy chain levels and disease progression in amyotrophic lateral sclerosis: insights from a longitudinal study. J Neurol Neurosurg Psychiatry. 2014.
Lu CH, Petzold A, Kalmar B, Dick J, Malaspina A, Greensmith L. Plasma neurofilament heavy chain levels correlate to markers of late stage disease progression and treatment response in SOD1(G93A) mice that model ALS. PLoS One. 2012;7(7):e40998.
Ganesalingam J, Bowser R. The application of biomarkers in clinical trials for motor neuron disease. Biomark Med. 2010;4(2):281–97.
Zetterberg H, Jacobsson J, Rosengren L, Blennow K, Andersen PM. Cerebrospinal fluid neurofilament light levels in amyotrophic lateral sclerosis: impact of SOD1 genotype. Eur J Neurol. 2007;14(12):1329–33.
Boylan K, Yang C, Crook J, Overstreet K, Heckman M, Wang Y, et al. Immunoreactivity of the phosphorylated axonal neurofilament H subunit (pNF-H) in blood of ALS model rodents and ALS patients: evaluation of blood pNF-H as a potential ALS biomarker. J Neurochem. 2009;111(5):1182–91.
Lu CH, Kalmar B, Malaspina A, Greensmith L, Petzold A. A method to solubilise protein aggregates for immunoassay quantification which overcomes the neurofilament “hook” effect. J Neurosci Methods. 2011;195(2):143–50.
Puentes F, Topping J, Kuhle J, van der Star BJ, Douiri A, Giovannoni G, et al. Immune reactivity to neurofilament proteins in the clinical staging of amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry. 2014;85(3):274–8.
Malaspina A, Puentes F, Amor S. Disease origin and progression in amyotrophic lateral sclerosis: an immunology perspective. Int Immunol. 2014.
Henkel JS, Beers DR, Wen S, Rivera AL, Toennis KM, Appel JE, et al. Regulatory T-lymphocytes mediate amyotrophic lateral sclerosis progression and survival. EMBO Mol Med. 2013;5(1):64–79.
Qureshi M, Brown Jr RH, Rogers JT, Cudkowicz ME. Serum ferritin and metal levels as risk factors for amyotrophic lateral sclerosis. Open Neurol J. 2008;2:51–4.
Levine TD, Bowser R, Hank NC, Gately S, Stephan D, Saperstein DS, et al. A pilot trial of pioglitazone HCl and tretinoin in ALS: cerebrospinal fluid biomarkers to monitor drug efficacy and predict rate of disease progression. Neurol Res Int. 2012;2012:582075.
Turner MR, Agosta F, Bede P, Govind V, Lule D, Verstraete E. Neuroimaging in amyotrophic lateral sclerosis. Biomark Med. 2012;6(3):319–37.
Chio A, Pagani M, Agosta F, Calvo A, Cistaro A, Filippi M. Neuroimaging in amyotrophic lateral sclerosis: insights into structural and functional changes. Lancet Neurol. 2014;13(12):1228–40.
Menke RA, Korner S, Filippini N, Douaud G, Knight S, Talbot K, et al. Widespread grey matter pathology dominates the longitudinal cerebral MRI and clinical landscape of amyotrophic lateral sclerosis. Brain. 2014;137(Pt 9):2546–55. This longitudinal analysis revealed progressive and widespread changes in the grey matter in contrast with a limited white matter pathology progression, with implications for the development of effective imaging biomarkers.
Mioshi E, Lillo P, Yew B, Hsieh S, Savage S, Hodges JR, et al. Cortical atrophy in ALS is critically associated with neuropsychiatric and cognitive changes. Neurology. 2013;80(12):1117–23.
Chen Z, Ma L. Grey matter volume changes over the whole brain in amyotrophic lateral sclerosis: a voxel-wise meta-analysis of voxel based morphometry studies. Amyotroph Lateral Scler. 2010;11(6):549–54.
Mezzapesa DM, D’Errico E, Tortelli R, Distaso E, Cortese R, Tursi M, et al. Cortical thinning and clinical heterogeneity in amyotrophic lateral sclerosis. PLoS One. 2013;8(11):e80748.
Schuster C, Kasper E, Dyrba M, Machts J, Bittner D, Kaufmann J, et al. Cortical thinning and its relation to cognition in amyotrophic lateral sclerosis. Neurobiol Aging. 2014;35(1):240–6.
Kaufmann P, Pullman SL, Shungu DC, Chan S, Hays AP, Del Bene ML, et al. Objective tests for upper motor neuron involvement in amyotrophic lateral sclerosis (ALS). Neurology. 2004;62(10):1753–7.
Foerster BR, Pomper MG, Callaghan BC, Petrou M, Edden RA, Mohamed MA, et al. An imbalance between excitatory and inhibitory neurotransmitters in amyotrophic lateral sclerosis revealed by use of 3-T proton magnetic resonance spectroscopy. JAMA Neurol. 2013;70(8):1009–16.
Li J, Pan P, Song W, Huang R, Chen K, Shang H. A meta-analysis of diffusion tensor imaging studies in amyotrophic lateral sclerosis. Neurobiol Aging. 2012;33(8):1833–8.
Foerster BR, Dwamena BA, Petrou M, Carlos RC, Callaghan BC, Churchill CL, et al. Diagnostic accuracy of diffusion tensor imaging in amyotrophic lateral sclerosis: a systematic review and individual patient data meta-analysis. Acad Radiol. 2013;20(9):1099–106. This individual patient data meta-analysis, reviewing all DTI studies, reported diagnostic accuracy of cerebral corticospinal tract fractional anisotropy in ALS subjects.
Sarro L, Agosta F, Canu E, Riva N, Prelle A, Copetti M, et al. Cognitive functions and white matter tract damage in amyotrophic lateral sclerosis: a diffusion tensor tractography study. AJNR Am J Neuroradiol. 2011;32(10):1866–72.
Branco LM, De Albuquerque M, De Andrade HM, Bergo FP, Nucci A, Franca Jr MC. Spinal cord atrophy correlates with disease duration and severity in amyotrophic lateral sclerosis. Amyotroph Lateral Scler Frontotemporal Degener. 2014;15(1–2):93–7.
Valsasina P, Agosta F, Benedetti B, Caputo D, Perini M, Salvi F, et al. Diffusion anisotropy of the cervical cord is strictly associated with disability in amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry. 2007;78(5):480–4.
Carew JD, Nair G, Pineda-Alonso N, Usher S, Hu X, Benatar M. Magnetic resonance spectroscopy of the cervical cord in amyotrophic lateral sclerosis. Amyotroph Lateral Scler. 2011;12(3):185–91.
Nair G, Carew JD, Usher S, Lu D, Hu XP, Benatar M. Diffusion tensor imaging reveals regional differences in the cervical spinal cord in amyotrophic lateral sclerosis. Neuroimage. 2010;53(2):576–83.
Schmidt R, Verstraete E, de Reus MA, Veldink JH, van den Berg LH, van den Heuvel MP. Correlation between structural and functional connectivity impairment in amyotrophic lateral sclerosis. Hum Brain Mapp. 2014;35(9):4386–95.
Lloyd CM, Richardson MP, Brooks DJ, Al-Chalabi A, Leigh PN. Extramotor involvement in ALS: PET studies with the GABA(A) ligand [(11)C]flumazenil. Brain. 2000;123(Pt 11):2289–96.
Pagani M, Chio A, Valentini MC, Oberg J, Nobili F, Calvo A, et al. Functional pattern of brain FDG-PET in amyotrophic lateral sclerosis. Neurology. 2014;83(12):1067–74.
Bensimon G, Lacomblez L, Meininger V. A controlled trial of riluzole in amyotrophic lateral sclerosis ALS/Riluzole Study Group. N Engl J Med. 1994;330(9):585–91.
Lacomblez L, Bensimon G, Leigh PN, Guillet P, Meininger V. Dose-ranging study of riluzole in amyotrophic lateral sclerosis Amyotrophic Lateral Sclerosis/Riluzole Study Group II. Lancet. 1996;347(9013):1425–31.
Yanagisawa N, Shindo M. Neuroprotective therapy for amyotrophic lateral sclerosis (ALS). Rinsho Shinkeigaku. 1996;36(12):1329–30.
Bensimon G, Lacomblez L, Delumeau JC, Bejuit R, Truffinet P, Meininger V. A study of riluzole in the treatment of advanced stage or elderly patients with amyotrophic lateral sclerosis. J Neurol. 2002;249(5):609–15.
Danzeisen R, Schwalenstoecker B, Gillardon F, Buerger E, Krzykalla V, Klinder K, et al. Targeted antioxidative and neuroprotective properties of the dopamine agonist pramipexole and its nondopaminergic enantiomer SND919CL2x [(+)2-amino-4,5,6,7-tetrahydro-6-Lpropylamino-benzathiazole dihydrochloride]. J Pharmacol Exp Ther. 2006;316(1):189–99.
Cudkowicz M, Bozik ME, Ingersoll EW, Miller R, Mitsumoto H, Shefner J, et al. The effects of dexpramipexole (KNS-760704) in individuals with amyotrophic lateral sclerosis. Nat Med. 2011;17(12):1652–6.
Cudkowicz ME, van den Berg LH, Shefner JM, Mitsumoto H, Mora JS, Ludolph A, et al. Dexpramipexole versus placebo for patients with amyotrophic lateral sclerosis (EMPOWER): a randomised, double-blind, phase 3 trial. Lancet Neurol. 2013;12(11):1059–67.
Yang YM, Gupta SK, Kim KJ, Powers BE, Cerqueira A, Wainger BJ, et al. A small molecule screen in stem-cell-derived motor neurons identifies a kinase inhibitor as a candidate therapeutic for ALS. Cell Stem Cell. 2013;12(6):713–26.
Emborg ME, Liu Y, Xi J, Zhang X, Yin Y, Lu J, et al. Induced pluripotent stem cell-derived neural cells survive and mature in the nonhuman primate brain. Cell Rep. 2013;3(3):646–50.
Yamamoto A, Lucas JJ, Hen R. Reversal of neuropathology and motor dysfunction in a conditional model of Huntington’s disease. Cell. 2000;101(1):57–66.
Furrer SA, Waldherr SM, Mohanachandran MS, Baughn TD, Nguyen KT, Sopher BL, et al. Reduction of mutant ataxin-7 expression restores motor function and prevents cerebellar synaptic reorganization in a conditional mouse model of SCA7. Hum Mol Genet. 2013;22(5):890–903.
Liu HN, Tjostheim S, Dasilva K, Taylor D, Zhao B, Rakhit R, et al. Targeting of monomer/misfolded SOD1 as a therapeutic strategy for amyotrophic lateral sclerosis. J Neurosci. 2012;32(26):8791–9.
Traynor BJ, Bruijn L, Conwit R, Beal F, O’Neill G, Fagan SC, et al. Neuroprotective agents for clinical trials in ALS: a systematic assessment. Neurology. 2006;67(1):20–7.
Chio A, Canosa A, Gallo S, Cammarosano S, Moglia C, Fuda G, et al. ALS clinical trials: do enrolled patients accurately represent the ALS population? Neurology. 2011;77(15):1432–7.
Acknowledgements
We thank P Couratier and JC Desport for their suggestions on the nutrition and respiratory sections of the paper.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Giancarlo Logroscino, Rosanna Tortelli, Giovanni Rizzo, Benoît Marin, Pierre Marie Preux, and Andrea Malaspina declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Neurology of Aging
Rights and permissions
About this article
Cite this article
Logroscino, G., Tortelli, R., Rizzo, G. et al. Amyotrophic Lateral Sclerosis: An Aging-Related Disease. Curr Geri Rep 4, 142–153 (2015). https://doi.org/10.1007/s13670-015-0127-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13670-015-0127-8
Keywords
- Amyotrophic lateral sclerosis
- Motor neuron disease
- Aging
- Neurodegenerative disorder
- Diagnosis
- Staging
- Prognosis
- Biomarkers
- Nutrition
- Respiratory insufficiency
- Epidemiology
- Incidence
- Sex ratio
- Population-based studies
- Genetics
- Superoxide dismutase 1
- Frontotemporal dementia
- Phenotype
- Ethnicity
- Therapy
- Randomized controlled trial