Abstract
Purpose of Review
To critically evaluate the most recent evidence on obstetric outcomes in women with adenomyosis.
Recent Findings
There is growing evidence suggesting an increased risk of obstetrical complications in women with adenomyosis.
Summary
An electronic search was conducted among the databases of PubMed, Google Scholar, and Cochrane review from January 2016 to March 2021. Nine observational studies fulfilled the inclusion criteria. Limitations of eligible studies include the presence of a majority of pregnancies achieved by ART, despite ART pregnancies being reported to be associated per se with a higher risk of adverse obstetric outcome; lack of information regarding the presence or absence of endometriosis; nonhomogeneous diagnostic criteria for adenomyosis; lack of the description of the severity of adenomyosis; and different timing of the diagnosis either before or during pregnancy. All studies reported that adenomyosis is associated with preterm delivery. Moreover, available data suggest that adenomyosis is associated with lower pregnancy rates after assisted reproductive techniques (ART) and higher rates of small-for-gestational-age (SGA)/low–birth weight (LBW) infants, cesarean delivery, and hypertensive disorder of pregnancy (HDP). Further studies on naturally conceived pregnancies, accurately designed in order to consider potential confounding factors, are needed in order to estimate the actual role of adenomyosis on fertility and obstetric and neonatal outcomes. Until more accurate data are available, it seems wise to foresee, when managing pregnant women with adenomyosis, the possible need for additional obstetric and intra-partum care.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In the last decade, several studies have evaluated the potential role of endometriosis in determining an adverse obstetric outcome. However, previous studies evaluating obstetric outcome in women with adenomyosis have reported conflicting results. On the one hand, a relatively recent review, published in 2016, concluded that adenomyosis does not affect obstetrical outcome [1]. On the other hand, 5 years later, in 2021, a systematic review and meta-analysis reported impaired fertility outcomes after assisted reproductive techniques (ART), such as a reduced clinical pregnancy rate and a higher miscarriage rate, as well as a significant association between adenomyosis and an increased risk of preeclampsia, preterm delivery, cesarean delivery, fetal malpresentation, small-for-gestational-age (SGA) infants, and postpartum hemorrhage (PPH) [2••].
Published studies on this subject are potentially biased, because they do not always take into account potential confounding factors such as age, parity, mode of conception, concomitant endometriosis, diagnostic criteria, and severity of adenomyosis and previous medical or surgical treatment of adenomyosis [2••]. In the last years, however, the importance of overcoming such methodological biases has been repeatedly pointed out and standard and reproducible ultrasonographic and MRI diagnostic criteria for adenomyosis have been established [3, 4].
In order to ascertain whether the increased focus on the adenomyotic disease in recent years contributed to the availability of more solid evidence, we sought to pursue this narrative mini-review investigating the evidence published in the last 5 years regarding the association of adenomyosis with reproductive, obstetric, and neonatal outcomes of women who conceived either naturally or by ART.
Materials and Methods
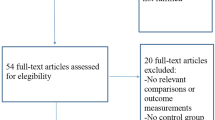
A search of PubMed publisher-supplied records for studies published between January 2016 and March 2021 was performed. We searched “adenomyosis and obstetrical outcome” and found 6318 articles. Two reviewers independently reviewed titles, abstracts, and full article’s text to identify eligible studies. Discrepancies were resolved by discussion. Studies were excluded for the following reasons: 4873 were deemed clearly unrelated to the topic, 395 were not comparative, 178 were not in English, 439 lacked to consider obstetric and neonatal outcomes or to describe how adenomyosis was diagnosed or whether infertility was present, 26 used animal models (Fig. 1). One reviewer abstracted data into standard evidence tables, and the second reviewer checked them for accuracy. Some outcomes were calculated from raw data reported in study publications to facilitate comparability across trials and thus may differ from the findings highlighted in the main results of the original publications.
Nine observational studies were eventually considered eligible for the present mini-review. Five studies were retrospective [5•, 6–9], and 4 were prospective [10–13]. In four studies, pregnancies achieved by ART only were evaluated [7, 11–13]. In the remaining five studies, both naturally conceived (NC) and ART pregnancies were evaluated [5•, 6, 8–10]. In these studies, results were presented altogether without differentiating NC and ART pregnancies, with the exception of one study presenting, in addition to the overall results, also the results separately for NC and ART pregnancies [8].
All studies included one or more control group/s of women without adenomyosis. In one study, all women in both adenomyosis and control group had endometriosis [6]. In another study, women with adenomyosis only and women with adenomyosis and endometriosis were separately evaluated, and controls included women with endometriosis without adenomyosis as well as women with tubal infertility [7]. In two studies, focal adenomyosis, located in only one part of the myometrium, and diffuse adenomyosis, defined as the presence of ill-defined lesion dispersed within the entire myometrium [6, 9], were separately evaluated. In one study, the outcomes of ART in women with adenomyosis receiving a long vs. ultra-long GnRH agonist were compared [13]. In one study, clinical pregnancy rates were evaluated according to a sonographic score that classifies adenomyosis in different grades of severity [12].
Adenomyosis was diagnosed by transvaginal ultrasonography (TVUS) alone in six studies: 2D TVUS was used in four of them [6–8, 13], and 3D TVUS in the remaining two studies [11, 12]. In two studies, adenomyosis was diagnosed by TVUS and/or MRI [5•, 9], and in one study, data were collected with a self-reported questionnaire [10].
Adenomyosis was diagnosed before conception in five studies [6, 7, 11–13], before pregnancy, or in early pregnancy in two studies [5•, 9] and in the first trimester of pregnancy in one study [8].
Clinical pregnancy was defined as the detection by TVUS of an intrauterine gestational sac [11] or as the presence of an embryo with a heartbeat assessed by TVUS either at 4 weeks [7], 6 weeks [12], or 8 weeks [13] after embryo transfer. Miscarriage was defined as clinical pregnancy loss before 20 weeks [7, 11], between 13 and 22 weeks [5•], before 28 weeks [13], or regardless of gestational age [12]. Live birth was defined as the delivery of an alive fetus after 26 completed weeks of gestation [7]. SGA were neonates with a birthweight below the 10th percentile [5•, 6, 9], or below −1.5 standard deviations for gestational age [10]. Low birth weight (LBW) was less than 2500 g [8, 10] and very low birth weight was less than 1500 g [10] regardless of gestational age. Preeclampsia was defined as gestational hypertension and proteinuria > 300 mg/24 h [5•, 6, 7]. Hypertensive disorder of pregnancy (HDP) was defined as blood pressure persistently higher than 140/90 mmHg after 20 weeks of gestation in a previously normotensive woman [5•, 9]. Post-partum hemorrhage (PPH) was defined as a blood loss > 1000 ml after cesarean delivery or > 500 ml after vaginal delivery.
Results
The findings of studies that included only women who conceived by ART, both in the adenomyosis group and in the control group, are reported in Table 1. A total of 837 women with adenomyosis and 5331 without adenomyosis were included.
Clinical Pregnancy Rate
Clinical pregnancy rate was significantly lower in women with adenomyosis in three out of four studies. In the study by Sharma et al., a higher pregnancy rate was observed in tubal factor control group as compared to both groups endometriosis plus adenomyosis (34.5% vs. 22.7%; OR: 1.79, 95% CI: 1.05–3.06; p = 0.03) and adenomyosis only (34.5% vs. 23.4%; OR: 1.72, 95% CI: 0.93–3.17; p = 0.07); similarly, a higher pregnancy rate was observed in endometriosis control group as compared to both groups endometriosis plus adenomyosis (36.6% vs. 22.7%; OR: 1.96, 95% CI: 1.14–3.38; p = 0.01) and adenomyosis only (36.6% vs. 23.4%; OR: 1.89, 95% CI: 1.02–3.50; p = 0.04) [7]. Hou and colleagues observed that the clinical pregnancy rate was significantly lower in women with adenomyosis receiving a long GnRH agonist treatment as compared to both controls (50.5% vs. 68.4%; p < 0.001) and to women with adenomyosis receiving an ultra-long GnRH agonist treatment (50.5% vs. 63.8%; p = 0.017) [13]. In the study by Mavrelos et al., the clinical pregnancy rate was significantly lower in women with adenomyosis as compared to controls (29.2% vs. 42.6%, RR 0.68; p = 0.044) [12]. Neal et al. did not find any significant difference in clinical pregnancy rate between adenomyosis group and controls (80% vs. 75%, p = 0.29) [11].
Miscarriage
Miscarriage rate was significantly higher in women with adenomyosis in two out of four studies. In the study by Sharma et al., a lower miscarriage rate was observed in tubal factor control group as compared to both groups endometriosis plus adenomyosis (13.04% vs. 35%; OR: 0.27, 95% CI: 0.09–0.77; p = 0.01) and adenomyosis only (13.04% vs. 40%; OR: 0.22, 95% CI: 0.07–0.69; p = 0.009); similarly, a lower miscarriage rate was observed in endometriosis control group as compared to both groups endometriosis plus adenomyosis (14.6% vs. 35%; OR: 0.32, 95% CI: 0.11–0.90; p = 0.03) and adenomyosis only (14.6% vs. 40%; OR: 0.26, 95% CI: 0.08–0.80; p = 0.02) [7]. Hou et al. observed the miscarriage rate to be significantly higher, as compared to controls, in women with adenomyosis that were either treated with long GnRH agonist (10.4% vs. 25.5%; p < 0.05) or with ultra-long GnRH agonist (10.4% vs. 17.4%; p < 0.05) [13]. A comparable rate of miscarriage between adenomyosis and control groups was reported in the studies by Neal et al. (10.5% vs. 7.7%, p = 0.36) [11] and by Mavrelos et al. (4.8% vs. 16.3%, RR 0.29; p = NS) [12].
Live Birth Rate
Live birth rate was significantly lower in women with adenomyosis in two out of three studies. In the study by Sharma et al., a higher live birth rate was observed in tubal factor control group as compared to both groups endometriosis plus adenomyosis (27.5% vs. 11.3%; OR: 2.95, 95% CI: 1.48–5.88; p = 0.002) and adenomyosis only (27.5% vs. 12.5%; OR: 2.65, 95% CI: 1.22–5.71; p = 0.01); similarly, a higher live birth rate was observed in endometriosis control group as compared to both groups endometriosis plus adenomyosis (26.5% vs. 11.3%; OR: 2.81, 95% CI: 1.40–5.65; p < 0.04) and adenomyosis only (26.5% vs. 12.5%; OR: 2.52, 95% CI: 1.16–5.49; p = 0.02) [7]. Hou et al. found that live birth rate was significantly lower in women with adenomyosis receiving a long GnRH agonist treatment as compared to both controls (37.6% vs. 58.5%; p < 0.001) and to women with adenomyosis receiving a ultra-long GnRH agonist treatment (37.6% vs. 52.4%; p = 0.01) [13]. Neal et al. did not find any significant difference in the live birth rate between adenomyosis group and controls (69.5% vs. 66.5%, p = 0.57) [11].
Other Outcomes
Shin et al. reported a higher rate in the adenomyosis group of preterm delivery before 37 weeks (28.0% vs. 6.4%; p = 0.003) and of low birth weight < 2500 g (28.0% vs. 4.8%; p = 0.003) [8]. Sharma et al. reported an increased rate of SGA infants in women with adenomyosis (with and without endometriosis) as compared to tubal factor controls (22.7% vs. 5%, OR: 0.17, 95%, CI: 0.05–0.62; p = 0.007) [7]. In this study, no significant differences were observed for the following outcomes: preeclampsia, PPH for both cesarean and vaginal delivery, antepartum hemorrhage, severe preterm delivery, intrauterine demise (p = NS) [7]. Hou et al. found that implantation rate was significantly lower in women with adenomyosis receiving a long GnRH agonist treatment as compared to both controls (36.9% vs. 49.5%; p = 0.001) and to women with adenomyosis receiving an ultra-long GnRH agonist treatment (36.9% vs. 43.5%; p = 0.047) [13].
The outcomes of the studies that included both NC and ART pregnancies are reported in Table 2 and Table 3. A total of 551 women with adenomyosis and 101,904 without adenomyosis are included. The prevalence of ART pregnancies among cases and controls was comparable in three studies, ranging between 17.2 and 46.9% in women with adenomyosis and between 12.8 and 46.9% in controls [5•, 6, 9]. In the remaining two studies, the proportion of women who conceived by ART was significantly higher in the adenomyosis group than in the control group: 34.7% vs. 2.3% and 19.3% vs. 3%, respectively [8, 10].
In the subgroup of NC pregnancies only, reported in one study only, the rate of preterm delivery (4.3% vs. 4.0%) and the rate of LBW neonates (6.4% vs. 3.1%; p = 0.175) were comparable between women with adenomyosis and controls [8].
Preterm Delivery
All the four NC/ART studies evaluating this issue found a significantly higher risk of preterm delivery before 37 weeks. Shin et al. found preterm delivery to be significantly higher in the adenomyosis group as compared to controls both before 37 weeks (12.5% vs. 4.1%, OR: 3.36, 95% CI: 1.66–6.82; p < 0.001) and before 32 weeks (6.9% vs. 0.3%, OR: 24.53, 95% CI: 9.12–66.02; p < 0.001) [8]. In the study of Yamaguchi et al., preterm delivery was significantly more frequent in the adenomyosis group than in the control group, both before 37 weeks (15.8% vs. 5.2%; p < 0.001) and before 34 weeks (3.5% vs. 1.2%; p < 0.001) [10]. Preterm delivery before 37 weeks was found to be significantly more frequent in the adenomyosis group than in the control group in the studies by Hashimoto et al. (24.4% vs. 9.3%, OR: 3.1, 95% CI: 1.2–7.2; p = 0.003) [5•] and Shinohara et al. (21.3% vs. 9.4%, OR: 2.6, 95% CI: 1.23–5.5; p = 0.01) [9]. In the study by Shinohara et al., women with diffuse adenomyosis, as compared to women with focal adenomyosis, showed a higher rate of preterm delivery before 37 weeks (29.3% vs. 7.3%, OR 5.24, 95% CI 2.15–12.8, p < 0.001) as well as a smaller median gestational age at delivery (35.8 ± 4.3 vs. 38.7 ± 1.4, p = 0.004) [9].
Small-for-Gestational-Age and Low Birth Weight
A significantly higher rate of SGA neonates was observed in three out of four NC/ART studies and a significantly higher rate of LBW neonates in two out of three NC/ART studies evaluating these issues. Scala et al. reported that the rate of SGA babies, as compared to control women with endometriosis and without adenomyosis, was significantly increased in women with endometriosis and diffuse adenomyosis (40% vs. 10.8%; p < 0.005), but was not significantly increased in women with endometriosis and focal adenomyosis (21.1% vs. 10.8%, p = 0.093) [6]. Shin et al. reported that women with adenomyosis, as compared to women without adenomyosis, had a significantly higher risk of LBW neonates (13.9% vs. 3.1%, OR: 5.05, 95% CI: 2.56–9.97; p < 0.001) as well as of VLBW neonates (4.2% vs. 0.3%, OR: 15.54; 95% CI: 4.56–52.97; p < 0.001) [8]. Hashimoto et al. found a significant difference in the risk of delivering a SGA neonate in the adenomyosis group vs. the control group (20.9% vs. 7.0%, OR: 3.5, 95% CI: 1.2–9.0; p = 0.004) [5•]. In the study by Yamaguchi et al., women with adenomyosis, as compared to controls, had a significantly increased rate of SGA neonates (8.7% vs. 5.2%, p = 0.006), LBW neonates (18.3% vs. 8.8%; p < 0.001), and VLBW neonates (2.9% vs. 0.7%; p < 0.001) [10]. Shinohara et al. did not find any significant difference in the rate of SGA neonates when comparing women with diffuse adenomyosis and controls (14.6% vs. 8.5%) or women with focal adenomyosis and controls (10% vs. 7.5%) [9].
Postpartum Hemorrhage
Postpartum hemorrhage was significantly higher in women with adenomyosis in one out of two studies that evaluated this outcome. In the study by Shinohara et al., a significant increase of PPH in the adenomyosis group vs. control group was observed for the total amount of women in the study (57.3% vs. 36.8%, OR: 2.30, 95% IC 1.30–4.07; p = 0.004) and for women undergoing cesarean delivery (82.6% vs. 35.7%, OR: 8.55, IC 2.45–29.8; p < 0.001), but not for women who delivered vaginally (40.7% vs. 37.7%, OR: 1.13, IC 0.49–2.61; p = 0.76). In the cesarean delivery group, the rate of PPH was significantly more frequent as compared to controls in women with diffuse adenomyosis (89.5% vs. 34.6%, OR: 16.1, 95% IC: 3.01–85.6; p < 0.001), whereas it was comparable to controls in women with focal adenomyosis (50% vs. 44.4%, p = NS). In the vaginal delivery group, the incidence of PPH, as compared to controls, was not significantly different for women with diffuse adenomyosis (58.3% vs. 45.9%, OR: 1.64, 95% CI: 0.49–5.50; p = 0.54) and for women with focal adenomyosis (50.3% vs. 45.9%, p = NS) [9]. Hashimoto et al. did not find any significant difference in blood loss in the adenomyosis group compared to controls after cesarean delivery (32% vs. 12.5%) or vaginal delivery (53.3% vs. 41.6%) [5•].
Cesarean Delivery
Cesarean delivery rate was significantly higher in women with adenomyosis in three out of four studies that evaluated this outcome. A significant increase of cesarean delivery rate was reported by Hashimoto et al. (65.1% vs. 31.4%, OR: 4.0, 95% CI: 1.9–8.6; p < 0.001), Yamaguchi et al. (36.7% vs. 19.5%; p < 0.001), and Shinohara et al. (46.0% vs. 20.9%, OR: 3.22 95% IC: 1.68–6.19; p < 0.001) [5•, 9, 10]. Shin et al. did not find a significant difference between women with adenomyosis and controls in cesarean delivery rate, 43.8% vs. 36.4%, p = NS [8].
Hypertensive Disorder of Pregnancy and Preeclampsia
Hypertensive disorder of pregnancy and preeclampsia were significantly higher in women with adenomyosis in two out of two studies and in one out of two studies that evaluated these outcomes, respectively. Hashimoto et al. reported an increase risk in the adenomyosis group as compared to the control of both HDP (30.6% vs. 6.1%, OR: 6.7, 95% CI: 2.7–18.2; p < 0.001) and preeclampsia (18.3% vs. 1.2%, OR: 21.0, 95% CI: 4.8–124.5; p < 0.001) [5•]. In this study, preeclampsia was significantly more common in nulliparous than in multiparous women with adenomyosis and it was not related to increased maternal age [5•]. Shinohara et al. found that the incidence of HDP was significantly higher in the adenomyosis group as compared to the control group (13.1% vs. 5.3%, OR: 2.68, 95% CI: 1.06–6.8; p = 0.045). Severe HDP (blood pressure > 160/100) was more frequent in the adenomyosis group, but the difference was not significant (9.8% vs. 3.6%, p = NS) [9]. Scala and colleagues, comparing the diffuse adenomyosis group to controls (20.0 vs. 8.1%, p = NS) and the focal adenomyosis group to controls (15.8% vs. 8.1%, p = NS), did not find any significant difference in the prevalence of preeclampsia [6].
Miscarriage
Miscarriage was evaluated by one study only. Hashimoto et al. reported a significantly higher rate of spontaneous second trimester miscarriage in the adenomyosis group than in the control group (12.2% vs. 1.2%, OR: 11.2, 95% CI: 2.2–71.2; p < 0.001) [5•].
Placental Malposition
Placental malposition was significantly higher in women with adenomyosis in one out of two studies that evaluated this outcome. Hashimoto et al. reported a significant increase of incidence of placental malposition, including placenta previa, in the adenomyosis group than in the control group (14.2% vs. 3.2%, OR: 4.9, 95% CI: 1.4–16.3; p < 0.001) [5•]. Shinohara et al. found a not significant increase in the adenomyosis group as compared to the control group (8.2% vs. 3.3%, OR: 2.63, 95% IC 0.83–8–36; p = 0.14) [9].
Fetal Malpresentation
Fetal malpresentation was not significantly increased in women with adenomyosis vs. controls in both the studies that evaluated this outcome (16.3% vs. 8.9% and 8.2% vs. 3.3%, respectively; p = NS) [5•, 9].
Other Outcomes
Neonatal Apgar score after 5 minutes: none out of two studies found any significant difference between the adenomyosis group and controls (p = NS) [5•, 6]. The frequency of gestational diabetes was not significantly increased in women with adenomyosis vs. controls in the studies of Shinohara et al. (14.8% vs. 8.6%, OR: 1.83, 95% IC: 0.80–4.25, p = NS) and Hashimoto et al. (2% vs. 17.1%, OR: NA; p = NS) [5•, 9]. Shinohara et al. reported pPROM to be significantly increased in the diffuse adenomyosis group as compared to the control group (12.2% vs. 2.4%, OR: 5.56, 95% IC 1.42-–21.7; p = 0.02) [9].
Discussion
The most recent studies published in the last 5 years on the role of adenomyosis on pregnancy outcome still reveal methodological flaws. The most evident confounding factor is that the majority of pregnancies were achieved by ART, despite ART pregnancies being reported to be associated per se with a higher risk of adverse obstetric outcomes, such as preeclampsia, preterm delivery, and low birth weight [14, 15]. In this regard, it has to be noted that the only study comparing obstetric outcomes in women with adenomyosis by mode of conception reported significantly higher rates of preterm delivery and low birth weight neonates only after conception by ART and not after natural conception [8]. Another limitation, affecting five out of nine studies included in this mini-review, is the lack of information regarding the presence or absence of endometriosis in both case and control groups [5•, 8, 9, 11, 12 ]. In fact, adenomyosis and endometriosis have the tendency to coexist and they may share some of the biological mechanisms that are supposed to impair pregnancy outcome such as activation of local and systemic inflammatory pathways; change in the immunologic milieu of the endometrium with higher levels of pro-inflammatory mediators such as prostaglandins; and altered uterine contractility [16–18]. Finally, we found that among studies included in the present review, the diagnosis of adenomyosis was not uniform. In the largest study, the diagnosis was based on a self-reported questionnaire collected during pregnancy, without an imaging assessment by the authors [10], whereas in the remaining studies, although there was general agreement on the ultrasonographic diagnostic criteria for adenomyosis, potential confounding factors were represented by lack of the description of the severity of adenomyosis in most study and by the different timing of the diagnosis, either before or during pregnancy. Due to these intrinsic limitations of previous studies and the heterogeneity of data, we abstained from performing a proper meta-analysis and decided to simply report the most recent findings on the relationship between adenomyosis and obstetric outcome in a narrative review.
Available results from the latest evidence do not seem to allow definitive conclusions on the effect of adenomyosis on obstetrical outcome. Among studies evaluating ART pregnancies only, previous findings reporting a lower clinical pregnancy rate and a lower live birth rate in women with adenomyosis [19, 20] are supported by three out of four studies [7, 12, 13]. Confounding factors for these outcomes are the potential older age of women with adenomyosis as compared to controls [11] as well as the inclusion of almost 50% of parous women, thus possibly selecting a population at better “a priori” fertility prognosis, in the study that did not report any detrimental effect of adenomyosis [11]. Even more uncertain was the evidence on the risk of miscarriage, significantly correlated to adenomyosis in two studies [7, 13], but unrelated to adenomyosis in two other studies [11, 12], as well as on the risks of preterm delivery, LBW, and SGA neonates that were evaluated and found increased for women with adenomyosis in a single study only [8].
Among studies mixing NC and ART pregnancies, the most solid evidence, in agreement with previous findings evaluating this issue [16, 21, 22], concerns the risk of preterm delivery that was evaluated in four studies and found significantly increased in women with adenomyosis in all of them [5•, 8–10].
As for other obstetrical outcomes, although the quality of evidence is lower due to conflicting results between studies and/or to the small number of women recruited, the present mini-review suggests, in agreement with previous findings [2••, 23], an increased prevalence among women with adenomyosis of SGA and/or LBW neonates (observed in four out of five studies) [5•, 6, 8, 10], cesarean delivery (three out of four studies) [5•, 9, 10], HDP (two out of two studies) [5•, 9], and miscarriage (one study) [5•]. These findings suggest that pregnant women with adenomyosis face an increased risk of obstetric complications and are in need of receiving additional and specific obstetric care.
The evidence from the studies included in this mini-review are inconsistent on whether adenomyosis might be associated with an increased risk of preeclampsia, placental malposition, and hemorrhage after cesarean delivery. Further studies are needed to draw definitive conclusions on these relevant obstetric complications. In our opinion, a particular consideration should be paid by future studies on pregnant women with adenomyosis, to the evaluation of the possibly increased risks associated with delivery. In fact, it is imperative to know whether women with adenomyosis, or what kind of women with adenomyosis, are to be equated, as for the risk of peripartum complications, to women with placenta previa and/or severe deep endometriosis [23]. Such evidence is needed in order to allow women at increased risk for life-threatening complications such as massive hemorrhage and visceral lesions and the need for obstetric hysterectomy to be referred for delivery in tertiary care institutions with the availability of expert surgeons and a blood bank [24, 25].
Conclusion
In conclusion, the most recent studies, published over the last 5 years, demonstrate that adenomyosis is associated with preterm delivery. Also, available data suggest that adenomyosis is associated with lower pregnancy rates after ART and higher rates of SGA/LBW infants, cesarean delivery, and HDP. Further studies on naturally conceived pregnancies, accurately designed in order to consider potential confounding factors, are needed in order to estimate the actual role of adenomyosis on fertility and obstetric and neonatal outcomes.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Harada T, Khine YM, Kaponis A, Nikellis T, Decavalas G, Taniguchi F. The Impact of Adenomyosis on Women’s Fertility. Obstet Gynecol Surv. 2016;71:557–68. https://doi.org/10.1097/OGX.0000000000000346.
•• Nirgianakis K, Kalaitzopoulos DR, Schwartz ASK, Spaanderman M, Kramer BW, Mueller MD, et al. Pregnancy and neonatal outcomes of patients with adenomyosis: a systematic review and meta-analysis. Reprod Biomed Online. 2021;42:185–206. https://doi.org/10.1016/j.rbmo.2020.09.023. Epub 2020 Oct 4. Findings from this study suggest that adenomyosis is associated with a significantly lower clinical pregnancy rate and higher miscarriage rate after ART, especially when a short GnRH agonist or antagonist protocol is administered for ovarian stimulation.
Van den Bosch T, Dueholm M, Leone FP, Valentin L, Rasmussen CK, Votino A, et al. Terms, definitions and measurements to describe sonographic features of myometrium and uterine masses: a consensus opinion from the Morphological Uterus Sonographic Assessment (MUSA) group. Ultrasound Obstet Gynecol. 2015;46:284–98. https://doi.org/10.1002/uog.14806. Epub 2015 Aug 10.
Bazot M, Daraï E. Role of transvaginal sonography and magnetic resonance imaging in the diagnosis of uterine adenomyosis. Fertil Steril. 2018;109:389–97. https://doi.org/10.1016/j.fertnstert.2018.01.024.
• Hashimoto A, Iriyama T, Sayama S, Nakayama T, Komatsu A, Miyauchi A, et al. Adenomyosis and adverse perinatal outcomes: increased risk of second trimester miscarriage, preeclampsia, and placental malposition. J Matern Fetal Neonatal Med. 2018;31:364–9. https://doi.org/10.1080/14767058.2017.1285895. Epub 2017 Feb 9. In this matched, case-control study, they found that patients who had adenomyosis were more likely associated with spontaneous second trimester miscarriage, preeclampsia, placental malposition, and preterm delivery, and to delivery of a SGA infant.
Scala C, Leone Roberti Maggiore U, Racca A, Barra F, Vellone VG, Venturini PL, et al. Influence of adenomyosis on pregnancy and perinatal outcomes in women with endometriosis. Ultrasound Obstet Gynecol. 2018;52:666–671. https://doi.org/10.1002/uog.18989.
Sharma S, Bathwal S, Agarwal N, Chattopadhyay R, Saha I, Chakravarty B. Does presence of adenomyosis affect reproductive outcome in IVF cycles? A retrospective analysis of 973 patients. Reprod Biomed Online. 2019;38:13–21. https://doi.org/10.1016/j.rbmo.2018.09.014. Epub 2018 Oct 26.
Shin YJ, Kwak DW, Chung JH, Kim MY, Lee SW, Han YJ. The risk of preterm births among pregnant women with adenomyosis. J Ultrasound Med. 2018;37:1937–43. https://doi.org/10.1002/jum.14540. Epub 2018 Jan 24.
Shinohara S, Okuda Y, Hirata S, Suzuki K. Adenomyosis as a potential risk factor for adverse pregnancy outcomes: a multicenter case-control study. Tohoku J Exp Med. 2020;251:231–9. https://doi.org/10.1620/tjem.251.231.
Yamaguchi A, Kyozuka H, Fujimori K, Hosoya M, Yasumura S, Yokoyama T, et al. Japan Environment and Children’s Study Group. Risk of preterm birth, low birthweight and small-for-gestational-age infants in pregnancies with adenomyosis: a cohort study of the Japan Environment and Children’s Study. Acta Obstet Gynecol Scand. 2019 Mar;98:359–364. https://doi.org/10.1111/aogs.13498. Epub 2018 Dec 2.
Neal S, Morin S, Werner M, Gueye NA, Pirtea P, Patounakis G, et al. Three-dimensional ultrasound diagnosis of adenomyosis is not associated with adverse pregnancy outcome following single thawed euploid blastocyst transfer: prospective cohort study. Ultrasound Obstet Gynecol. 2020;56:611–7. https://doi.org/10.1002/uog.22065.
Mavrelos D, Holland TK, O’Donovan O, Khalil M, Ploumpidis G, Jurkovic D, et al. The impact of adenomyosis on the outcome of IVF-embryo transfer. Reprod Biomed Online. 2017;35:549–54. https://doi.org/10.1016/j.rbmo.2017.06.026. Epub 2017 Jul 29.
Hou X, Xing J, Shan H, Mei J, Sun Y, Yan G, et al. The effect of adenomyosis on IVF after long or ultra-long GnRH agonist treatment. Reprod Biomed Online. 2020;41:845–53. https://doi.org/10.1016/j.rbmo.2020.07.027 (Epub 2020 Aug 1).
Pandey S, Shetty A, Hamilton M, Bhattacharya S, Maheshwari A. Obstetric and perinatal outcomes in singleton pregnancies resulting from IVF/ICSI: a systematic review and meta-analysis. Hum Reprod Update. 2012 Sep-Oct;18:485–503. doi: https://doi.org/10.1093/humupd/dms018. Epub 2012 May 19.
Qin JB, Sheng XQ, Wu D, Gao SY, You YP, Yang TB, et al. Worldwide prevalence of adverse pregnancy outcomes among singleton pregnancies after in vitro fertilization/intracytoplasmic sperm injection: a systematic review and meta-analysis. Arch Gynecol Obstet. 2017;295:285–301. https://doi.org/10.1007/s00404-016-4250-3 (Epub 2016 Nov 28).
Juang CM, Chou P, Yen MS, Twu NF, Horng HC, Hsu WL. Adenomyosis and risk of preterm delivery. BJOG. 2007;114:165–9. https://doi.org/10.1111/j.1471-0528.2006.01186.x. Epub 2006 Dec 4.
Brosens I, Pijnenborg R, Benagiano G. Defective myometrial spiral artery remodeling as a cause of major obstetrical syndromes in endometriosis and adenomyosis. Placenta. 2013;34:100–5.
Vannuccini S, Clifton VL, Fraser IS, Taylor HS, Critchley H, Giudice LC, et al. Infertility and reproductive disorders: impact of hormonal and inflammatory mechanisms on pregnancy outcome. Hum Reprod Update. 2016 Jan-Feb;22:104–15. doi: https://doi.org/10.1093/humupd/dmv044. Epub 2015 Sep 22.
Younes G, Tulandi T. Effects of adenomyosis on in vitro fertilization treatment outcomes: a meta-analysis. Fertil Steril. 2017;108:483-490.e3. https://doi.org/10.1016/j.fertnstert.2017.06.025.
Vercellini P, Consonni D, Dridi D, Bracco B, Frattaruolo MP, Somigliana E. Uterine adenomyosis and in vitro fertilization outcome: a systematic review and meta-analysis. Hum Reprod. 2014;29:964–77. https://doi.org/10.1093/humrep/deu041. Epub 2014 Mar 12.
Mochimaru A, Aoki S, Oba MS, Kurasawa K, Takahashi T, Hirahara F. Adverse pregnancy outcomes associated with adenomyosis with uterine enlargement. J Obstet Gynaecol Res. 2015;41:529–33. https://doi.org/10.1111/jog.12604. Epub 2014 Nov 3.
•• Horton J, Sterrenburg M, Lane S, Maheshwari A, Li TC, Cheong Y. Reproductive, obstetric, and perinatal outcomes of women with adenomyosis and endometriosis: a systematic review and meta-analysis. Hum Reprod Update. 2019;11(25):592–632. https://doi.org/10.1093/humupd/dmz012. Findings from this study suggest that adenomyosis and endometriosis have a negative impact on oocyte yield and number of mature oocytes and they increase the risk of miscarriage, preterm birth, cesarean section delivery, and neonatal unit admission following delivery.
Vercellini P, Parazzini F, Pietropaolo G, Cipriani S, Frattaruolo MP, Fedele L. Pregnancy outcome in women with peritoneal, ovarian and rectovaginal endometriosis: a retrospective cohort study. BJOG. 2012;119:1538–43. https://doi.org/10.1111/j.1471-0528.2012.03466.x. Epub 2012 Aug 20.
Exacoustos C, Lauriola I, Lazzeri L, De Felice G, Zupi E. Complications during pregnancy and delivery in women with untreated rectovaginal deep infiltrating endometriosis. Fertil Steril. 2016;106:1129-1135.e1.
Vercellini P, Frattaruolo MP, Barbara G, Buggio L, Somigliana E. The ominous association between severe endometriosis, in vitro fertilisation, and placenta previa: raising awareness, limiting risks, informing women. BJOG. 2018;125:12–5. https://doi.org/10.1111/1471-0528.14789. Epub 2017 Jul 26.
Author information
Authors and Affiliations
Contributions
NB and PV were responsible for conception and design of the study and for critical revision of the article for intellectual content. Acquisition of data was performed by AD, FF, and ML. Analysis and interpretation of data was accomplished by NB and PV. All the authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Nicola Berlanda, Agnese Donati, Francesco Fedele, Massimo Lepri, and Paolo Vercellini declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Uterine Fibroids and Endometrial Lesions
Rights and permissions
About this article
Cite this article
Berlanda, N., Donati, A., Fedele, F. et al. Adenomyosis and Obstetrical Outcome: a Narrative Mini-Review of the Latest Evidence. Curr Obstet Gynecol Rep (2022). https://doi.org/10.1007/s13669-021-00316-1
Accepted:
Published:
DOI: https://doi.org/10.1007/s13669-021-00316-1