Abstract
Purpose of Review
The approval of nintedanib and pirfenidone has changed the treatment landscape of idiopathic pulmonary fibrosis (IPF); however, both drugs only slow disease progression and are burdened by tolerability issues. We summarize the most advanced developmental drugs in IPF, but also mention selected compounds in earlier phases.
Recent Findings
Several compounds are currently being tested in IPF; the number of trials has increased exponentially in the last 3 years. Four compounds have reached phase 3: BI101550, an oral PDE4B preferential inhibitor; Pamrevlumab, an anticonnective tissue growth factor intravenous monoclonal antibody; Pentraxin-2, a recombinant human form of serum amyloid protein; Treprostinil, a synthetic prostanoid, with an inhaled formulation, currently used for pulmonary hypertension.
Summary
New drugs are likely to reach the clinic in the near future. This will provide more opportunities for treatment of IPF but will also pose unprecedented challenges regarding drug selection and administration(i.e., sequential vs. combination).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
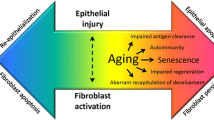
Idiopathic pulmonary fibrosis (IPF), the most common of the idiopathic interstitial pneumonias, is a chronic, progressive, and ultimately fatal disease characterized radiologically and histologically by the usual interstitial pneumonia (UIP) pattern of fibrosis [1,2,3]. Although disease pathogenesis remains incompletely understood, IPF is believed to result from and exuberant and dysregulated reparative response following recurrent alveolar epithelial cell (AEC) injury [4]. Aberrantly activated AECs secrete a multitude of cytokines and chemokines, which induce fibroblast recruitment, activation, proliferation, and differentiation to myofibroblasts [5]. Several factors have been associated with the development and progression of IPF, including, among others, smoking, chronic microaspiration of gastric content, occupational/environmental exposure, pollution, and subclinical viral infection [6,7,8,9]. These triggers are likely to interact with host genetic factors, including, among others, rare variants within telomerase-related genes [10] or MUC5B rs35705950 promoter polymorphism [11], to determine the disease. Innate and acquired immunity [12], epigenetic changes [13], telomere attrition [14], mitochondrial dysfunction [15], and cellular senescence [16] are additional likely contributors to disease pathogenesis.
Historically, IPF has been treated with a combination of corticosteroids and immunosuppressants (with or without N-acetylcysteine), the rationale being that chronic inflammation was considered a prerequisite for the disease to develop [17]. However, this treatment strategy has been proven not only inefficacious but also harmful [18]. Therefore, a multitude of potential treatments has been tested in randomized controlled trials (RCTs) in an effort to find a real cure for IPF; yet, most of these trials have yielded negative results (Table 1). Currently, two drugs are approved worldwide for the treatment of IPF: pirfenidone and nintedanib [19]. Pirfenidone acts by downregulating transforming growth factor (TGF)-β, one of the most potent profibrotic cytokines, and tumor necrosis factor (TNF)-α, both in vitro and in vivo [20,21,22], although its mechanism of action is known only partially. Nintedanib is an intracellular tyrosine kinase inhibitor, which, by acting on fibroblast growth factor (FGF), platelet-derived growth factor (PDGF), and vascular endothelial growth factor (VEGF), interferes with the signaling needed for the proliferation and migration of fibroblasts and their differentiation to myofibroblasts [23,24,25]. Apart from the respective pivotal studies [26, 27], the efficacy of both nintedanib and pirfenidone in reducing functional decline, as assessed by annual change in forced vital capacity (FVC) and disease progression, has been confirmed by real word and registry data [28,29,30,31,32,33,34]. However, both drugs have tolerability issues, mainly skin rash and gastrointestinal discomfort with pirfenidone and diarrhea with nintedanib [25, 35], which lead to drug discontinuation in a significant minority of patients [36,37,38]. Thus, the unmet IPF need remains high, and more efficacious and better tolerated drugs are urgently needed. In this review, we summarize and critically discuss the most advanced developmental drugs in IPF, with the aim to provide the reader with a glimpse of what the landscape of IPF treatment looks like. However, selected compounds in earlier phases of development are also mentioned (Table 2).
BI1015550
BI1015550 is an oral phosphodiesterase (PDE) 4B preferential inhibitor [39•]. PDEs are a superfamily of enzymes composed of more than 100 isoforms. They act by hydrolyzing cyclic nucleotides, in particular cyclic adenosine monophosphate (cAMP) and cyclic guanine monophosphate (cGMP), thus regulating their intracellular concentration [40]. The PDE4 A-D family displays high specificity for cAMP but no activity on cGMP [41]. Therefore, PDE4 exerts proinflammatory activities by blocking the cAMP pathways mediated by both protein kinase A (PKA) and exchange factors activated by cAMP (Epac1/2) [42]. PKA reduces the production of proinflammatory cytokines via phosphorylation of cAMP-responsive element-binding protein (CREB), through the modulation of the transcriptional activity of nuclear factor kappa-light-chain-enhancer of activated B cells (NFkB) and by interfering with B cell lymphoma 6 protein (Bcl-6) [43,44,45,46]. Epac1/2, on the other hand, shows anti-inflammatory activities through epigenetic modulation of NFkB targets [47]. Owing to their well-established anti-inflammatory properties, PDE4 inhibitors are approved for the treatment of inflammatory airway disease, psoriatic arthritis, and atopic dermatitis [41].
PDE4 inhibition has also antifibrotic effects. In bleomycin-treated mice and rats, roflumilast reduced the transcription and bronchoalveolar lavage (BAL) levels of several profibrotic genes, including TNFα and TGF-β, and improved fibrotic changes in the lung [48]. The antifibrotic effect of PDE4 inhibitors has also been shown in other animal models of fibrosis, such as type II AEC injury [49] and graft-vs-host disease [50], and with other compounds, such as cilomilast [51]. In vitro, human lung fibroblasts exposed to PDE4 inhibitors show lower expression of profibrotic proteins (or their mRNA), such as connective tissue growth factor (CTGF), collagen-α1, fibronectin, or α-smooth muscle actin, which are markers of fibrosis, fibroblast proliferation, or fibroblast-to-myofibroblast differentiation [52,53,54,55].
Preclinical studies have confirmed the anti-inflammatory properties of BI1015550 through reduction of TNF-α and interleukin 2 (IL-2) production by mononuclear blood cells and inhibition of monocyte and neutrophil influx in the lung. The compound was also efficacious in two different animal models of fibrosis, with improvement of FVC values in the bleomycin model and reduced BALF inflammation in the silica model in mice. Furthermore, BI1015550 reduced TGF-β-induced collagen production in human fibroblasts, alone or synergistically with nintedanib [39•].
The safety and efficacy of BI1015550 have been evaluated in a phase 2 trial in IPF; 147 patients were randomized to either BI1015550 or placebo with a 2:1 ratio and stratified based on background treatment (nintedanib or pirfenidone) [56••]. Inclusion criteria included a high-resolution CT pattern of definite or probable UIP, as assessed centrally, FVC ≥ 45%, and DLco between 25 and 80% of the predicted value. BI1015550 was administered orally at a dose of 18 mg twice a day for 12 weeks. Notably, the authors used a Bayesian approach to reduce the number of patients randomized to placebo, including historical data from patients included in the placebo arms of previous nintedanib trials [57]. The study met its primary endpoint irrespective of background antifibrotic therapy. Indeed, the median change in FVC was 5.7 ml in the BI1015550 group and − 81.7 ml in the placebo group among patients without background antifibrotic therapy and 2.7 ml in the BI1015550 group and − 59.2 ml in the placebo group among patients with background antifibrotic use. No differences in the secondary endpoints of change in diffusing capacity of the lung for carbon monoxide (DLco) or change in quality of life were found. The most frequently reported adverse events were gastrointestinal, in particular diarrhea, but the proportion of patients with serious or severe adverse events was similar in the two trial groups.
A phase 3 RCT (NCT05321069), FIBRONEER-IPF, is ongoing. This study will enroll 963 patients with IPF. Inclusion criteria include an FVC ≥ 45% and DLco between 25 and 90% of the predicted value. Patients will be randomized to two doses of BI1015550 or placebo for 52 weeks. Estimated study completion date is November 2024. The primary endpoint is the change in absolute FVC; secondary endpoints include time to functional worsening (decline in FVC ≥ 10% or DLco ≥ 15%), time to the first occurrence of the composite outcome comprehending hospitalization for respiratory cause, death or acute exacerbation, time to acute exacerbation, time to hospitalization for respiratory cause or death, absolute change in FVC% and DLco% predicted, and change in Living with Pulmonary Fibrosis Questionnaire score.
Pamrevlumab
Pamrevlumab, formerly known by its developmental name FG-3019, is a fully human recombinant antibody that binds to CTGF, inhibiting it from binding to its receptors [58•].
CTGF is a secreted glycoprotein that interacts with a plethora of cytokines involved in connective tissue regeneration and wound healing [59, 60]. CTGF has a key role in fibroblast proliferation and differentiation to myofibroblasts. Treatment of fibroblasts with recombinant CTGF and TGF-β increases profibrotic markers in fibroblasts, thus suggesting a synergistic effect of CTGF and TGF-β in inducing pulmonary fibrosis [61]. A similar positive feedback loop has been observed between CTGF and other fibrogenic molecules such as VEGF and integrins [62]. Moreover, CTGF appears to act as TGF-β cofactor: in fact, in CTGF knockout mice, TGF-β cannot exert its profibrotic activity [63, 64]. In IPF lung, CTGF is increased both transcriptionally and translationally in AECs and fibroblasts [65, 66].
In vivo, Pamrevlumab reduces collagen deposition and fibrosis in different animal models, including bleomycin- and radiotherapy-induced lung fibrosis [64, 67]. Pamrevlumab is able to induce fibroblast apoptosis in a model of mesothelioma [68], and a similar effect is also plausible on IPF myofibroblasts [69].
Pamrevlumab has been evaluated in two phase 2 studies in IPF. The first was an open-label study that assessed the safety and efficacy of two different doses of the drug (15 or 30 mg/kg) [70]. Patients received Pamrevlumab intravenously every 3 weeks for 45 weeks. FG-3019 displayed a good safety and tolerability profile. Notably, changes in fibrosis correlated with changes in pulmonary function, and FG-3019 was associated with an increase in FVC and reduction in the extent of fibrosis in about one-third of patients. The PRAISE trial randomized 103 IPF patients to Pamrevlumab 30 mg/kg or placebo over 48 weeks [71••]. Inclusion criteria included a definite UIP pattern on chest CT or a probable UIP and lung biopsy, an FVC ≥ 55%, and a DLco ≥ 30%; background antifibrotic treatment was not allowed. The study met its primary endpoint. Indeed, Pamrevlumab reduced the decline in FVC% predicted by 60% at week 48 (mean change from baseline − 2.9% with Pamrevlumab vs − 7.2% with placebo; p = 0.033). The secondary endpoints of absolute decline in FVC, number of patients with an FVC decline ≥ 10%, and extent of lung fibrosis on HRCT were also met. Conversely, no differences in quality of life as assessed by the Saint George Respiratory Questionnaire were observed. The safety and tolerability profile of Pamrevlumab were similar to those of placebo.
The phase 3 Zephyrus I and II trials (NCT03955146-NCT04419558) are currently ongoing. Each study will enroll 340 IPF patients. Inclusion criteria include age between 40 and 80 years, FVC percentage of predict between 45 and 90%, DLco between 25 and 90%, and fibrotic changes at HRCT between 10 and 50%. Background antifibrotic therapy is not allowed. Patients will be randomized to Pamrevlumab 30 mg/kg or placebo administered intravenously every 3 weeks for 48 weeks. Estimated completion date is June 2024 for Zephyrus I and May 2023 for Zephyrus II. For both studies, the primary endpoint is the change in FVC from baseline; secondary endpoints include time to disease progression (decline in FVC ≥ 10% or death), time to respiratory hospitalization, death and acute exacerbation, as single occurrence or as composite outcome, and changes in the quantitative lung fibrosis score.
Pentraxin-2
Pentraxin-2, also known as serum amyloid protein (SAP), is a pleiotropic pentameric protein secreted by the liver. SAP is a highly conserved protein, and neither genetic deficiencies nor polymorphisms have been reported to date [72]. It exerts antifibrotic activities through different mechanisms. Specifically, SAP inhibits monocyte-to-fibroblast differentiation and activation of profibrotic macrophages by inducing IL-10 production. SAP also interferes with numerous profibrotic signals such as thrombin, tryptase, IL-4, and IL-13 [73]. Conversely, inhibition of SAP induces persistent inflammation and fibrosis following bleomycin challenge in mice [74]. Reduced serum levels of SAP, or increased levels with reduced activity through desialylation, have been found in patients with IPF and other fibrotic diseases [75,76,77,78]. This effect is likely to be secondary to the accumulation of SAP in fibrotic and injury sites [79].
In a mouse model of kidney fibrosis, SAP reduced inflammation as well as fibroblast and myofibroblast activation [79]. In a mouse model of bleomycin-induced lung fibrosis, the administration of human SAP reduced inflammation and fibrosis through inhibition of TGF-β-induced macrophage activity [76, 80, 81].
Owing to its antifibrotic properties, a recombinant form of human Pentraxin-2, also known as PRM-151, has been evaluated in IPF [82]. In a phase 2 study (PRM-151–202), 116 IPF patients were randomized in a 2:1 ratio to Pentraxin-2 or placebo over 24 weeks [83]. The drug was administered intravenously at a dose of 10 mg/kg every 4 weeks with a loading regimen of three doses at the start of treatment (day 1, 3, and 5). Inclusion criteria were a definite/probable UIP pattern on chest CT, an FVC between 50 and 90%, and DLco between 25 and 90% of the predicted values; concurrent therapy with pirfenidone or nintedanib was permitted if the dosage was stable for at least 3 months. The study met its primary endpoint of mean change in FVC% predicted from baseline to week 28, which was − 2.5% in patients treated with recombinant human Pentraxin-2 and − 4.8% in those in the placebo group. In addition, the change in 6-min walk distance was − 0.5 m for patients treated with Pentraxin-2 vs. − 31.8 m for those in the placebo group (p < 0.001). Conversely, no difference was found in quantitative parenchymal features on HRCT or changes in DLco. The drug was safe and well tolerated with the most common adverse events in the Pentraxin-2 vs. placebo group being cough (18% vs. 5%, respectively) and fatigue (17% vs. 10%, respectively).
Patients who completed the 28-week double-blind period of the PRM-151–202 trial were eligible to participate in the open-label extension study (at 76 and 128 weeks) [84, 85]. Specifically, patients previously enrolled in the Pentraxin-2 arm continued this treatment while those previously randomized to placebo crossed over to Pentraxin-2. Both analyses confirmed that long-term treatment with Pentraxin-2 was well tolerated and that the positive effects on FVC and 6-min walking distance were persistent on continuation and positive in patients who crossed over from placebo.
A phase 3 trial (NCT04594707), STARSCAPE, was conducted to confirm the efficacy and safety of recombinant human Pentraxin-2 in patients with IPF. The study has recently been terminated for futility with the results yet to be released. This study enrolled 665 patients. Inclusion criteria were an FVC ≥ 45% and DLco between 30 and 90% of the predicted values. The primary endpoint was the change in absolute FVC while secondary endpoints included changes in 6MWT, FVC% and DLco, time to respiratory-related hospitalization, acute exacerbation, or all-cause mortality over 48 weeks. Quality of life, as assessed by SGRQ and University of California, San Diego-Shortness of Breath Questionnaire, was also evaluated.
Treprostinil
Treprostinil is a chemically stable prostacyclin analog, developed and approved for the treatment of pulmonary hypertension (PH) [86]. This compound acts through a complex network of prostanoid receptors on different cellular types [87]. In particular, prostaglandin I2 receptor (IP), prostaglandin D2 receptor 1 (DP1), and prostaglandin E2 receptor 2 (EP2), all Gs protein-coupled receptors, increase cellular concentrations of cAMP [88]. In turn, the increase in cAMP inhibits the extracellular regulated kinase (Erk1/2) signaling, thus blocking several profibrotic pathways [89]. Potential antifibrotic effects of Treprostinil include reduction of TGF-β- and PDGF-induced collagen deposition [90], inhibition of fibroblast proliferation through nuclear accumulation of cAMP [91], and modulation of inflammatory cell accumulation via inhibition of NFkB, as shown in bleomycin-induced pulmonary fibrosis in mice [92]. Another signaling pathway inhibited by increased cAMP levels is the Yes-associated protein (YAP)/transcriptional coactivator with PDZ-binding motif (TAZ). These nuclear factors have a role in the transcription of TGF-β-activated genes [93]. Additional antifibrotic activities may be due to the immunomodulatory effects of prostanoid receptors [94,95,96].
Treprostinil was initially evaluated as a continuous subcutaneous infusion to treat group 1 PH [97]. To avoid infusion-related side effects, an inhaled formulation has been developed, and this has led to the approval of Treprostinil for the treatment of PH in USA, Israel, and Argentina [98]. Further studies have suggested the efficacy of inhaled Treprostinil in group 3 PH, including PH secondary to IPF [99, 100]. The INCREASE trial, a phase 3 RCT, assessed the safety and efficacy of inhaled Treprostinil in patients with PH secondary to ILD [101]. In this trial, patients had PH confirmed by right heart catheter and ILD confirmed by centrally reviewed CT scans and were allowed to remain on a stable dose of antifibrotic therapy. The drug was administered by an ultrasonic, pulsed-delivery nebulizer at a dose of 6 μg per breath, starting with 3 breaths 4 times a day, with the dose increased by 1 breath every 3 days until reaching the target dose of 9 breaths per session, up to a maximum of 12 per session. The study met its primary endpoint of change in peak 6-MWD from baseline through week 16. Change in NTproBNP levels and time to clinical worsening were also significantly different favoring Treprostinil. The study drug was well tolerated, and the most frequently reported adverse events were cough, headache, dyspnea, dizziness, nausea, fatigue, and diarrhea. Notably, 22% of patients in the Treprostinil arm and 39% of patients in the placebo arm experienced exacerbation of their underlying disease, a percentage substantially higher than in other clinical trials of IPF/fibrotic ILD [27, 102•]. A post hoc analysis of this study looked at patients with IPF and found that Treprostinil treatment was associated with preserved lung function, as assessed by FVC, and reduced risk of acute exacerbation [102•].
Based on these results, two parallel RCTs (TETON) will evaluate the efficacy of inhaled Treprostinil, either alone or on background antifibrotic therapy, in patients with IPF (NCT05255991; NCT04708782) [103••]. Each study will enroll 396 patients. Inclusion criteria include an FVC ≥ 45% predicted. Pirfenidone and nintedanib are allowed provided patients are on a stable and optimized dose for ≥ 30 days prior to baseline. Treprostinil will be administered as in the INCREASE study [101], and the study is expected to be concluded in June 2025. The primary endpoint is the change in absolute FVC from baseline to week 52; secondary endpoints include time to clinical worsening and acute exacerbation, overall survival, FVC% decline, and change in King’s Brief Interstitial Lung Disease Questionnaire score.
Future Perspectives
One decade after the approval of pirfenidone and nintedanib, the unmet need in IPF remains high. A large number of trials have been conducted, particularly in the last 3 years (Fig. 1; Table 2). Intravenous or endobronchial delivery of mesenchymal stem cells has proven safe and potentially efficacious, but the available data does not allow drawing firm conclusions; a number of phase 1 and phase 2 studies are ongoing [104••]. TRK-250 is an inhaled small interfering RNA with the potential to suppress TGF-β expression. A phase 1 study has recently been completed, but the results have not been released yet [105]. C21, an oral angiotensin II type 2 receptor agonist, has been associated with improvement of FVC in an interim analysis of an ongoing Phase 2 trial in IPF [106]. Dasatinib + quercetin are oral senolytics that act through inhibition of antiapoptotic pathways. In a recently completed phase 1 study, these drugs were safe and well tolerated [107].
Finally, two studies [108, 109] have shown that the combination of nintedanib and pirfenidone is safe and well tolerated; a phase 4 study is currently evaluating the safety and efficacy of the combination pirfenidone and nintedanib compared to a “switch monotherapy” (i.e., switching from the current to the other of the two drugs prescribed as monotherapy) in patients with IPF experiencing progression despite antifibrotic therapy (NCT03939520).
Conclusions
The approval of nintedanib and pirfenidone has changed the landscape of IPF treatment, and more drugs are likely to reach the clinic in the next few years. This represents an unprecedented opportunity; yet, it also poses new challenges regarding the choice of the drug and the possibility to combine them or to use them sequentially. However, the development of truly efficacious drugs able to halt or even reverse fibrosis requires a better understanding of the mechanisms involved in disease pathogenesis with the final aim to provide the right patient with the right drug at the right time.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Raghu G, Remy-Jardin M, Richeldi L, Thomson CC, Antoniou KM, Bissell BD, et al. Idiopathic pulmonary fibrosis (an update) and progressive pulmonary fibrosis in adults: an official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med. 2022;205:E18-47. https://doi.org/10.1164/rccm.202202-0399ST.
Raghu G, Remy-Jardin M, Myers JL, Richeldi L, Ryerson CJ, Lederer DJ, et al. Diagnosis of idiopathic pulmonary fibrosis an official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med. 2018;198:e44-68. https://doi.org/10.1164/rccm.201807-1255ST.
Lynch DA, Sverzellati N, Travis WD, Brown KK, Colby TV, Galvin JR, et al. Diagnostic criteria for idiopathic pulmonary fibrosis: a Fleischner Society White Paper. Lancet Respir Med. 2018;6:138–53. https://doi.org/10.1016/S2213-2600(17)30433-2.
Strunz M, Simon LM, Ansari M, Kathiriya JJ, Angelidis I, Mayr CH, et al. Alveolar regeneration through a Krt8+ transitional stem cell state that persists in human lung fibrosis. Nat Commun. 2020;11:3559. https://doi.org/10.1038/s41467-020-17358-3.
Selman M, Pardo A. The leading role of epithelial cells in the pathogenesis of idiopathic pulmonary fibrosis. Cell Signal. 2020;66:109482. https://doi.org/10.1016/j.cellsig.2019.109482.
Sheng G, Chen P, Wei Y, Yue H, Chu J, Zhao J, et al. Viral infection increases the risk of idiopathic pulmonary fibrosis: a meta-analysis. Chest. 2020;157:1175–87. https://doi.org/10.1016/j.chest.2019.10.032.
Pardo A, Selman M. The interplay of the genetic architecture, aging, and environmental factors in the pathogenesis of idiopathic pulmonary fibrosis. Am J Respir Cell Mol Biol. 2021;64:163–72. https://doi.org/10.1165/rcmb.2020-0373PS.
Bédard Méthot D, Leblanc É, Lacasse Y. Meta-analysis of gastroesophageal reflux disease and idiopathic pulmonary fibrosis. Chest. 2019;155:33–43. https://doi.org/10.1016/j.chest.2018.07.038.
Baumgartner KB, Samet JM, Stidley CA, Colby TV, Waldron JA. Cigarette smoking: a risk factor for idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 1997;155:242–8. https://doi.org/10.1164/ajrccm.155.1.9001319.
Stock CJW, Renzoni EA. Telomeres in interstitial lung disease. J Clin Med. 2021;7:1384. https://doi.org/10.3390/jcm10071384.
Wu X, Li W, Luo Z, Chen Y. The minor T allele of the MUC5B promoter rs35705950 associated with susceptibility to idiopathic pulmonary fibrosis: a meta-analysis. Sci Rep. 2021;11:1–18. https://doi.org/10.1038/s41598-021-03533-z.
Spagnolo P, Tonelli R, Samarelli AV, Castelli G, Cocconcelli E, Petrarulo S, et al. The role of immune response in the pathogenesis of idiopathic pulmonary fibrosis: far beyond the Th1/Th2 imbalance. Expert Opin Ther Targets. 2022;26:617–31. https://doi.org/10.1080/14728222.2022.2114897.
Tirelli C, Pesenti C, Miozzo M, Mondoni M, Fontana L, Centanni S. The genetic and epigenetic footprint in idiopathic pulmonary fibrosis and familial pulmonary fibrosis: a state-of-the-art review. Diagnostics. 2022;12:3107. https://doi.org/10.3390/diagnostics12123107.
Cronkhite JT, Xing C, Raghu G, Chin KM, Torres F, Rosenblatt RL, et al. Telomere shortening in familial and sporadic pulmonary fibrosis. Am J Respir Crit Care Med. 2008;178:729–37. https://doi.org/10.1164/rccm.200804-550OC.
Spagnolo P, Semenzato U. Revealing the pathogenic and ageing-related mechanisms of the enigmatic idiopathic pulmonary fibrosis (and chronic obstructive pulmonary disease). Curr Opin Pulm Med. 2022;28:296–302. https://doi.org/10.1097/MCP.0000000000000876.
Minagawa S, Araya J, Numata T, Nojiri S, Hara H, Yumino Y, et al. Accelerated epithelial cell senescence in IPF and the inhibitory role of SIRT6 in TGF-β-induced senescence of human bronchial epithelial cells. Am J Physiol - Lung Cell Mol Physiol. 2011;300:391–401. https://doi.org/10.1152/ajplung.00097.2010.
ATS Board Of Directors, ERS Executive Committee. Idiopathic pulmonary fibrosis: diagnosis and treatment international consensus statement. Am J Respir Crit Care Med. 2000;161:646–64. https://doi.org/10.1164/ajrccm.161.2.ats3-00.
Idiopathic Pulmonary Fibrosis Clinical Research Network, Raghu G, Anstrom KJ, King TE, Lasky JA, Martinez FJ. Prednisone, azathioprine, and N-acetylcysteine for pulmonary fibrosis. N Engl J Med. 2012;366:1968–77. https://doi.org/10.1056/NEJMoa1113354.
Raghu G, Rochwerg B, Zhang Y, Garcia CAC, Azuma A, Behr J, et al. An official ATS/ERS/JRS/ALAT clinical practice guideline: treatment of idiopathic pulmonary fibrosis: an update of the 2011 clinical practice guideline. Am J Respir Crit Care Med. 2015;192:e3-19. https://doi.org/10.1164/rccm.201506-1063ST.
Oku H, Nakazato H, Horikawa T, Tsuruta Y, Suzuki R. Pirfenidone suppresses tumor necrosis factor-α, enhances interleukin-10 and protects mice from endotoxic shock. Eur J Pharmacol. 2002;446:167–76. https://doi.org/10.1016/s0014-2999(02)01757-0.
Nakazato H, Oku H, Yamane S, Tsuruta Y, Suzuki R. A novel anti-fibrotic agent pirfenidone suppresses tumor necrosis factor-α at the translational level. Eur J Pharmacol. 2002;446:177–85. https://doi.org/10.1016/s0014-2999(02)01758-2.
Iyer SN, Margolin SB, Hyde DM, Giri SN. Lung fibrosis is ameliorated by pirfenidone fed in diet after the second dose in a three-dose bleomycin-hamster model. Exp Lung Res. 1998;24:119–33. https://doi.org/10.3109/01902149809046058.
Wollin L, Maillet I, Quesniaux V, Holweg A, Ryffel B. Antifibrotic and anti-inflammatory activity of the tyrosine kinase inhibitor nintedanib in experimental models of lung fibrosis. J Pharmacol Exp Ther. 2014;349:209–20. https://doi.org/10.1124/jpet.113.208223.
Hostettler KE, Zhong J, Papakonstantinou E, Karakiulakis G, Tamm M, Seidel P, et al. Anti-fibrotic effects of nintedanib in lung fibroblasts derived from patients with idiopathic pulmonary fibrosis. Respir Res. 2014;15:157. https://doi.org/10.7326/0003-4819-134-2-200101160-00015.
Roth GJ, Binder R, Colbatzky F, Dallinger C, Schlenker-Herceg R, Hilberg F, et al. Nintedanib: from discovery to the clinic. J Med Chem. 2015;58:1053–63. https://doi.org/10.1021/jm501562a.
King TE, Bradford WZ, Castro-Bernardini S, Fagan EA, Glaspole I, Glassberg MK, et al. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N Engl J Med. 2014;370:2083–92. https://doi.org/10.1056/NEJMoa1402582.
Richeldi L, du Bois RM, Raghu G, Azuma A, Brown KK, Costabel U, et al. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl J Med. 2014;370:2071–82. https://doi.org/10.1056/NEJMoa1402584.
Cameli P, Alonzi V, d’Alessandro M, Bergantini L, Pordon E, Guerrieri M, et al. The effectiveness of nintedanib in patients with idiopathic pulmonary fibrosis, familial pulmonary fibrosis and progressive fibrosing interstitial lung diseases: a real-world study. Biomedicines. 2022;8:1973. https://doi.org/10.3390/biomedicines10081973.
Antoniou K, Markopoulou K, Tzouvelekis A, Trachalaki A, Vasarmidi E, Organtzis J, et al. Efficacy and safety of nintedanib in a greek multicentre idiopathic pulmonary fibrosis registry: a retrospective, observational, cohort study. ERJ Open Res. 2020;27;6(1):00172–2019. https://doi.org/10.1183/23120541.00172-2019.
Vietri L, Cameli P, Perruzza M, Cekorja B, Bergantini L, d’Alessandro M, et al. Pirfenidone in idiopathic pulmonary fibrosis: real-life experience in the referral centre of Siena. Ther Adv Respir Dis. 2020;14:1–8. https://doi.org/10.1177/1753466620906326.
Lancaster L, Crestani B, Hernandez P, Inoue Y, Wachtlin D, Loaiza L, et al. Safety and survival data in patients with idiopathic pulmonary fibrosis treated with nintedanib: pooled data from six clinical trials. BMJ Open Respir Res. 2019;6:1–7. https://doi.org/10.1136/bmjresp-2018-000397.
Nathan SD, Albera C, Bradford WZ, Costabel U, Glaspole I, Glassberg MK, et al. Effect of pirfenidone on mortality: pooled analyses and meta-analyses of clinical trials in idiopathic pulmonary fibrosis. Lancet Respir Med. 2017;5(1):33–41. https://doi.org/10.1016/S2213-2600(16)30326-5.
Zurkova M, Kriegova E, Kolek V, Lostakova V, Sterclova M, Bartos V, et al. Effect of pirfenidone on lung function decline and survival: 5-yr experience from a real-life IPF cohort from the Czech EMPIRE registry. Respir Res. 2019;20:1–11.
Margaritopoulos GA, Trachalaki A, Wells AU, Vasarmidi E, Bibaki E, Papastratigakis G, et al. Pirfenidone improves survival in IPF: results from a real-life study. BMC Pulm Med. 2018;18:1–7. https://doi.org/10.1186/s12890-018-0736-z.
Lancaster LH, de Andrade JA, Zibrak JD, Padilla ML, Albera C, Nathan SD, et al. Pirfenidone safety and adverse event management in idiopathic pulmonary fibrosis. Eur Respir Rev 2017;146:170057. https://doi.org/10.1183/16000617.0057-2017.
Tzouvelekis A, Karampitsakos T, Kontou M, Granitsas A, Malliou I, Anagnostopoulos A, et al. Safety and efficacy of nintedanib in idiopathic pulmonary fibrosis: a real-life observational study in Greece. Pulm Pharmacol Ther. 2018;49:61–6. https://doi.org/10.1016/j.pupt.2018.01.006.
Dobashi M, Tanaka H, Taima K, Itoga M, Ishioka Y, Shiratori T, et al. The efficacy of nintedanib in 158 patients with idiopathic pulmonary fibrosis in real-world settings: a multicenter retrospective study. SAGE Open Med. 2021;9:205031212110233. https://doi.org/10.1177/20503121211023357.
Bando M, Yamauchi H, Ogura T, Taniguchi H, Watanabe K, Azuma A, et al. Clinical experience of the long-term use of pirfenidone for idiopathic pulmonary fibrosis. Intern Med. 2016;55:443–8. https://doi.org/10.2169/internalmedicine.55.5272.
• Herrmann FE, Hesslinger C, Wollin L, Nickolaus P. BI 1015550 is a PDE4B inhibitor and a clinical drug candidate for the oral treatment of idiopathic pulmonary fibrosis. Front Pharmacol. 2022;13:1–17. https://doi.org/10.3389/fphar.2022.838449. In this paper, the preclinical effects of BI1015550 in vitro and in vivo are presented; they provide the rationale for its use as antifibrotic agent in IPF patients.
Azevedo MF, Faucz FR, Bimpaki E, Horvath A, Levy I, De Alexandre RB, et al. Clinical and molecular genetics of the phosphodiesterases (pdes). Endocr Rev. 2014;35:195–233. https://doi.org/10.1210/er.2013-1053.
Li H, Zuo J, Tang W. Phosphodiesterase-4 inhibitors for the treatment of inflammatory diseases. Front Pharmacol. 2018;9:1–21. https://doi.org/10.3389/fphar.2018.01048.
Kolb M, Crestani B, Maher TM. Phosphodiesterase 4B inhibition: a potential novel strategy for treating pulmonary fibrosis. Eur Respir Rev. 2023;167:220206. https://doi.org/10.1183/16000617.0206-2022.
Takahashi N, Tetsuka T, Uranishi H, Okamoto T. Inhibition of the NF-κB transcriptional activity by protein kinase A. Eur J Biochem. 2002;269:4559–65. https://doi.org/10.1046/j.1432-1033.2002.03157.x.
Schafer P. Apremilast mechanism of action and application to psoriasis and psoriatic arthritis. Biochem Pharmacol. 2012;83:1583–90. https://doi.org/10.1016/j.bcp.2012.01.001.
MacKenzie SJ, Houslay MD. Action of rolipram on specific PDE4 cAMP phosphodiesterase isoforms and on the phosphorylation of cAMP-response-element-binding protein (CREB) and p38 mitogen-activated protein (MAP) kinase in U937 monocytic cells. Biochem J. 2000;347:571–8. https://doi.org/10.1042/0264-6021:3470571.
Hernández-Flórez D, Valor L. Selective phosphodiesterase inhibitors: a new therapeutic option in inflammation and autoimmunity. Reumatol Clínica. English Ed. 2016;12:303–6. https://doi.org/10.1016/j.reuma.2016.07.011.
Lehrke M, Kahles F, Makowska A, Tilstam PV, Diebold S, Marx J, et al. PDE4 inhibition reduces neointima formation and inhibits VCAM-1 expression and histone methylation in an Epac-dependent manner. J Mol Cell Cardiol. 2015;81:23–33. https://doi.org/10.1016/j.yjmcc.2015.01.015.
Cortijo J, Iranzo A, Milara X, Mata M, Cerdá-Nicolás M, Ruiz-Saurí A, et al. Roflumilast, a phosphodiesterase 4 inhibitor, alleviates bleomycin-induced lung injury. Br J Pharmacol. 2009;156:534–44. https://doi.org/10.1111/j.1476-5381.2008.00041.x.
Sisson TH, Christensen PJ, Muraki Y, Dils AJ, Chibucos L, Subbotina N, et al. Phosphodiesterase 4 inhibition reduces lung fibrosis following targeted type II alveolar epithelial cell injury. Physiol Rep. 2018;6:1–15. https://doi.org/10.14814/phy2.13753.
Kim SW, Lim JY, Rhee CK, Kim JH, Park CK, Kim TJ, et al. Effect of roflumilast, novel phosphodiesterase-4 inhibitor, on lung chronic graft-versus-host disease in mice. Exp Hematol. 2016;44:332-341.e4. https://doi.org/10.1016/j.exphem.2016.02.002.
Udalov S, Dumitrascu R, Pullamsetti SS, Al-Tamari HM, Weissmann N, Ghofrani HA, et al. Correction to: Effects of phosphodiesterase 4 inhibition on bleomycin-induced pulmonary fibrosis in mice. BMC Pulm Med. 2022;22:113. https://doi.org/10.1186/s12890-022-01876-5.
Dunkern TR, Feurstein D, Rossi GA, Sabatini F, Hatzelmann A. Inhibition of TGF-β induced lung fibroblast to myofibroblast conversion by phosphodiesterase inhibiting drugs and activators of soluble guanylyl cyclase. Eur J Pharmacol. 2007;572:12–22. https://doi.org/10.1016/j.ejphar.2007.06.036.
Selige J, Hatzelmann A, Dunkern T. The differential impact of PDE4 subtypes in human lung fibroblasts on cytokine-induced proliferation and myofibroblast conversion. J Cell Physiol. 2011;226:1970–80. https://doi.org/10.1002/jcp.22529.
Tannheimer SL, Wright CD, Salmon M. Combination of roflumilast with a beta-2 adrenergic receptor agonist inhibits proinflammatory and profibrotic mediator release from human lung fibroblasts. Respir Res. 2012;13:1–11. https://doi.org/10.1186/1465-9921-13-28.
Vecchio D, Acquaviva A, Arezzini B, Tenor H, Martorana PA, Gardi C. Downregulation of NOX4 expression by roflumilast N-oxide reduces markers of fibrosis in lung fibroblasts. Mediators Inflamm. 2013;2013. https://doi.org/10.1155/2013/745984.
•• Richeldi L, Azuma A, Cottin V, Hesslinger C, Stowasser S, Valenzuela C, et al. Trial of a preferential phosphodiesterase 4B inhibitor for idiopathic pulmonary fibrosis. N Engl J Med. 2022;386:2178–87. https://doi.org/10.1056/NEJMoa2201737. This phase 2 study shows that BI1015550 is able to reduce FVC decline irrespective of background antifibrotic therapy.
Schmidli H, Gsteiger S, Roychoudhury S, O’Hagan A, Spiegelhalter D, Neuenschwander B. Robust meta-analytic-predictive priors in clinical trials with historical control information. Biometrics. 2014;70:1023–32. https://doi.org/10.1111/biom.12242.
• Sgalla G, Franciosa C, Simonetti J, Richeldi L. Pamrevlumab for the treatment of idiopathic pulmonary fibrosis. Expert Opin Investig Drugs. 2020;29:771–7. https://doi.org/10.1080/13543784.2020.1773790. This paper describes the preclinical and clinical evidence on Pamrevlumab.
Chen Z, Zhang N, Chu HY, Yu Y, Zhang ZK, Zhang G, et al. Connective tissue growth factor: from molecular understandings to drug discovery. Front Cell Dev Biol. 2020;8:1–17. https://doi.org/10.3389/fcell.2020.593269.
Bradham DM, Igarashi A, Potter RL, Grotendorst GR. Connective tissue growth factor: a cysteine-rich mitogen secreted by human vascular endothelial cells is related to the SRC-induced immediate early gene product CEF-10. J Cell Biol. 1991;114:1285–94. https://doi.org/10.1083/jcb.114.6.1285.
Yanagihara T, Tsubouchi K, Gholiof M, Chong SG, Lipson KE, Zhou Q, et al. Connective-tissue growth factor contributes to TGF-b1-induced lung fibrosis. Am J Respir Cell Mol Biol. 2022;66:260–70. https://doi.org/10.1165/rcmb.2020-0504OC.
Yang H, Huang Y, Chen X, Liu J, Lu Y, Bu L, et al. The role of CTGF in the diabetic rat retina and its relationship with VEGF and TGF-β2, elucidated by treatment with CTGFsiRNA. Acta Ophthalmol. 2010;88:652–9. https://doi.org/10.1111/j.1755-3768.2009.01641.x.
Lipson KE, Wong C, Teng Y, Spong S. CTGF is a central mediator of tissue remodeling and fibrosis and its inhibition can reverse the process of fibrosis. Fibrogenesis Tissue Repair. 2012;5:2–9. https://doi.org/10.1186/1755-1536-5-S1-S24.
Wang Q, Usinger W, Nichols B, Gray J, Xu L, Seeley TW, et al. Cooperative interaction of CTGF and TGF-β in animal models of fibrotic disease. Fibrogenes Tissue Repair. 2011;4:1–11. https://doi.org/10.1186/1755-1536-4-4.
Shi-Wen X, Leask A, Abraham D. Regulation and function of connective tissue growth factor/CCN2 in tissue repair, scarring and fibrosis. Cytokine Growth Factor Rev. 2008;19:133–44. https://doi.org/10.1016/j.cytogfr.2008.01.002.
Pan LH, Yamauchi K, Uzuki M, Nakanishi T, Takigawa M, Inoue H, et al. Type II alveolar epithelial cells and interstitial fibroblasts express connective tissue growth factor in IPF. Eur Respir J. 2001;17:1220–7. https://doi.org/10.1183/09031936.01.00074101.
Sternlicht MD, Wirkner U, Bickelhaupt S, Lopez Perez R, Tietz A, Lipson KE, et al. Radiation-induced pulmonary gene expression changes are attenuated by the CTGF antibody Pamrevlumab. Respir Res. 2018;19:1–16. https://doi.org/10.1186/s12931-018-0720-4.
Ohara Y, Chew SH, Misawa N, Wang S, Somiya D, Nakamura K, et al. Connective tissue growth factor-specific monoclonal antibody inhibits growth of malignant mesothelioma in an orthotopic mouse model. Oncotarget. 2018;9:18494–509. https://doi.org/10.18632/oncotarget.24892.
Thannickal VJ, Horowitz JC. Evolving concepts of apoptosis in idiopathic pulmonary fibrosis. Proc Am Thorac Soc. 2006;3:350–6. https://doi.org/10.1513/pats.200601-001TK.
Raghu G, Scholand MB, De Andrade J, Lancaster L, Mageto Y, Goldin J, et al. FG-3019 anti-connective tissue growth factor monoclonal antibody: results of an open-label clinical trial in idiopathic pulmonary fibrosis. Eur Respir J. 2016;47:1481–91. https://doi.org/10.1183/13993003.01030-2015.
•• Richeldi L, Fernández Pérez ER, Costabel U, Albera C, Lederer DJ, Flaherty KR, et al. Pamrevlumab, an anti-connective tissue growth factor therapy, for idiopathic pulmonary fibrosis (PRAISE): a phase 2, randomised, double-blind, placebo-controlled trial. Lancet Respir Med. 2020;8:25–33. https://doi.org/10.1016/S2213-2600(19)30262-0. This phase 2 trial suggests that pamrevlumab is safe and well tolerated and efficiacious in reducing FVC decline in patients with IPF.
Pepys MB. The pentraxins 1975–2018: Serendipity, diagnostics and drugs. Front Immunol. 2018;9:1–18. https://doi.org/10.3389/fimmu.2018.02382.
Pilling D, Gomer RH. The development of serum amyloid p as a possible therapeutic. Front Immunol. 2018;9:1–10. https://doi.org/10.3389/fimmu.2018.02328.
Pilling D, Gomer RH. Persistent lung inflammation and fibrosis in serum amyloid P component (Apcs-/-) knockout mice. PLoS ONE. 2014;9:29–33. https://doi.org/10.1371/journal.pone.0093730.
Basturk T, Ojalvo D, Mazi EE, Hasbal NB, Ozagari AA, Ahbap E, et al. Pentraxin-2 is associated with renal fibrosis in patients undergoing renal biopsy. Clinics. 2020;75:1–5. https://doi.org/10.6061/clinics/2020/e1809.
Murray LA, Chen Q, Kramer MS, Hesson DP, Argentieri RL, Peng X, et al. TGF-beta driven lung fibrosis is macrophage dependent and blocked by serum amyloid P. Int J Biochem Cell Biol. 2011;43:154–62. https://doi.org/10.1016/j.biocel.2010.10.013.
Verna EC, Patel J, Bettencourt R, Nguyen P, Hernandez C, Valasek MA, et al. Novel association between serum pentraxin-2 levels and advanced fibrosis in well-characterised patients with non-alcoholic fatty liver disease. Aliment Pharmacol Ther. 2015;42:582–90. https://doi.org/10.1111/apt.13292.
Chen W, Karhadkar TR, Ryu C, Herzog EL, Gomer RH. Reduced sialylation and bioactivity of the antifibrotic protein serum amyloid p in the sera of patients with idiopathic pulmonary fibrosis. ImmunoHorizons. 2020;4:352–62. https://doi.org/10.4049/immunohorizons.2000043.
Castaño AP, Lin SL, Surowy T, Nowlin BT, Turlapati SA, Patel T, et al. Serum amyloid P inhibits fibrosis through FcγR-dependent monocyte-macrophage regulation in vivo. Sci Transl Med. 2009;5:5ra13. https://doi.org/10.1126/scitranslmed.3000111.
Pilling D, Roife D, Wang M, Ronkainen SD, Crawford JR, Travis EL, et al. Reduction of bleomycin-induced pulmonary fibrosis by serum amyloid P. J Immunol. 2007;179:4035–44. https://doi.org/10.4049/jimmunol.179.6.4035.
Murray LA, Rosada R, Moreira AP, Joshi A, Kramer MS, Hesson DP, et al. Serum amyloid P therapeutically attenuates murine bleomycin-induced pulmonary fibrosis via its effects on macrophages. PLoS ONE. 2010;5:1–9. https://doi.org/10.1371/journal.pone.0009683.
Tzouvelekis A, Tzilas V, Antoniou KM, Bouros D. Human pentraxin 2 protein treatment for IPF. Lancet Respir Med. 2019;7:640–1. https://doi.org/10.1016/S2213-2600(19)30173-0.
Raghu G, van den Blink B, Hamblin MJ, Brown AW, Golden JA, Ho LA, et al. Effect of recombinant human pentraxin 2 vs placebo on change in forced vital capacity in patients with idiopathic pulmonary fibrosis. JAMA. 2018;319:2299. https://doi.org/10.1001/jama.2018.6129.
Raghu G, Hamblin MJ, Brown AW, Golden JA, Ho LA, Wijsenbeek MS, et al. Long-term evaluation of the safety and efficacy of recombinant human pentraxin-2 (rhPTX-2) in patients with idiopathic pulmonary fibrosis (IPF): an open-label extension study. Respir Res. 2022;23:1–12. https://doi.org/10.1186/s12931-022-02047-0.
Raghu G, van den Blink B, Hamblin MJ, Brown AW, Golden JA, Ho LA, et al. Long-term treatment with recombinant human pentraxin 2 protein in patients with idiopathic pulmonary fibrosis: an open-label extension study. Lancet Respir Med. 2019;7:657–64. https://doi.org/10.1016/S2213-2600(19)30172-9.
Olschewski H, Rose F, Schermuly R, Ghofrani HA, Enke B, Olschewski A, et al. Prostacyclin and its analogues in the treatment of pulmonary hypertension. Pharmacol Ther. 2004;102:139–53. https://doi.org/10.1016/j.pharmthera.2004.01.003.
Woodward DF, Jones RL, Narumiya S. International union of basic and clinical pharmacology. LXXXIII: classification of prostanoid receptors, updating 15 years of progress. Pharmacol Rev. 2011;63:471–538. https://doi.org/10.1124/pr.110.003517.
Whittle BJ, Silverstein AM, Mottola DM, Clapp LH. Binding and activity of the prostacyclin receptor (IP) agonists, treprostinil and iloprost, at human prostanoid receptors: treprostinil is a potent DP 1 and EP 2 agonist. Biochem Pharmacol. 2012;84:68–75. https://doi.org/10.1016/j.bcp.2012.03.012.
Nikam VS, Wecker G, Schermuly R, Rapp U, Szelepusa K, Seeger W, et al. Treprostinil inhibits the adhesion and differentiation of fibrocytes via the cyclic adenosine monophosphate-dependent and ras-proximate protein-dependent inactivation of extracellular regulated kinase. Am J Respir Cell Mol Biol. 2011;45:692–703. https://doi.org/10.1165/rcmb.2010-0240OC.
Lambers C, Roth M, Jaksch P, Muraközy G, Tamm M, Klepetko W, et al. Treprostinil inhibits proliferation and extracellular matrix deposition by fibroblasts through cAMP activation. Sci Rep. 2018;8:1–10. https://doi.org/10.1038/s41598-018-19294-1.
Roberts MJ, May LT, Keen AC, Liu B, Lam T, Charlton SJ, et al. Inhibition of the proliferation of human lung fibroblasts by prostacyclin receptor agonists is linked to a sustained camp signal in the nucleus. Front Pharmacol. 2021;12:1–14. https://doi.org/10.3389/fphar.2021.669227.
Nikitopoulou I, Manitsopoulos N, Kotanidou A, Tian X, Petrovic A, Magkou C, et al. Orotracheal treprostinil administration attenuates bleomycin-induced lung injury, vascular remodeling, and fibrosis in mice. Pulm Circ. 2019;9. https://doi.org/10.1177/2045894019881954.
Zmajkovicova K, Menyhart K, Bauer Y, Studer R, Renault B, Schnoebelen M, et al. The antifibrotic activity of prostacyclin receptor agonism is mediated through inhibition of YAP/TAZ. Am J Respir Cell Mol Biol. 2019;60:578–91. https://doi.org/10.1165/rcmb.2018-0142OC.
Boniface K, Bak-Jensen KS, Li Y, Blumenschein WM, McGeachy MJ, McClanahan TK, et al. Prostaglandin E2 regulates Th17 cell differentiation and function through cyclic AMP and EP2/EP4 receptor signaling. J Exp Med. 2009;206:535–48. https://doi.org/10.1084/jem.20082293.
Napolitani G, Acosta-Rodriguez EV, Lanzavecchia A, Sallusto F. Prostaglandin E2 enhances Th17 responses via modulation of IL-17 and IFN-γ production by memory CD4+ T cells. Eur J Immunol. 2009;39:1301–12. https://doi.org/10.1002/eji.200838969.
Yao C, Sakata D, Esaki Y, Li Y, Matsuoka T, Kuroiwa K, et al. Prostaglandin E2-EP4 signaling promotes immune inflammation through TH1 cell differentiation and TH17 cell expansion. Nat Med. 2009;15:633–40. https://doi.org/10.1038/nm.1968.
Simonneau G, Barst RJ, Galie N, Naeije R, Rich S, Bourge RC, et al. Continuous subcutaneous infusion of treprostinil, a prostacyclin analogue, in patients with pulmonary arterial hypertension: a double-blind, randomized, placebo-controlled trial. Am J Respir Crit Care Med. 2002;165:800–4. https://doi.org/10.1164/ajrccm.165.6.2106079.
McLaughlin VV, Benza RL, Rubin LJ, Channick RN, Voswinckel R, Tapson VF, et al. Addition of inhaled treprostinil to oral therapy for pulmonary arterial hypertension: a randomized controlled clinical trial. J Am Coll Cardiol. 2010;55:1915–22. https://doi.org/10.1016/j.jacc.2010.01.027.
Faria-Urbina M, Oliveira RKF, Agarwal M, Waxman AB. Inhaled treprostinil in pulmonary hypertension associated with lung disease. Lung. 2018;196:139–46. https://doi.org/10.1007/s00408-017-0081-7.
Bajwa AA, Shujaat A, Patel M, Thomas C, Rahaghi F, Burger CD. The safety and tolerability of inhaled treprostinil in patients with pulmonary hypertension and chronic obstructive pulmonary disease. Pulm Circ. 2017;7:82–8. https://doi.org/10.1086/689291.
Waxman A, Restrepo-Jaramillo R, Thenappan T, Ravichandran A, Engel P, Bajwa A, et al. Inhaled treprostinil in pulmonary hypertension due to interstitial lung disease. N Engl J Med. 2021;384:325–34. https://doi.org/10.1056/NEJMoa2008470.
• Nathan SD, Waxman A, Rajagopal S, Case A, Johri S, DuBrock H, et al. Inhaled treprostinil and forced vital capacity in patients with interstitial lung disease and associated pulmonary hypertension: a post-hoc analysis of the INCREASE study. Lancet Respir Med. 2021;9:1266–74. https://doi.org/10.1016/S2213-2600(21)00165-X. This post hoc analysis shows that inhaled treprostinil reduces the decline in FVC in patients with IPF.
•• Nathan SD, Behr J, Cottin V, Lancaster L, Smith P, Deng CQ, et al. Study design and rationale for the TETON phase 3, randomised, controlled clinical trials of inhaled treprostinil in the treatment of idiopathic pulmonary fibrosis. BMJ open Respir Res. 2022;9:198–207. https://doi.org/10.1136/bmjresp-2022-001310. This paper describes the design of TETON, a study that evaluates inhaled Treprostinil as antifibrotic treatment in IPF.
•• Spagnolo P, Kropski JA, Jones MG, Lee JS, Rossi G, Karampitsakos T, et al. Idiopathic pulmonary fibrosis: disease mechanisms and drug development. Pharmacol Ther [Internet]. Elsevier Inc.; 2021;222:107798 https://doi.org/10.1016/j.pharmthera.2020.107798. This review discusses drug development and potential therapeutic targets in IPF.
Shibata A, Matsumoto T, Uchida M, Yamada M, Miyamoto Y, Inada H, et al. A Novel siRNA-based oligonucleotide, TRK-250, and its efficacy for treatment of idiopathic pulmonary fibrosis (IPF). C64 Pulm Fibros Model Mech INSIGHTS. Am Thorac Soc. 2019;A5391–A5391. https://doi.org/10.1164/ajrccm-conference.2019.199.1_MeetingAbstracts.A5391.
Maher T, Ganslandt C, Batta R, Tornling G, Bengtsson T, Pophale H, et al. Interim results from AIR, an open-label, single arm, 36-week ph 2 trial of C21 in subjects with idiopathic pulmonary fibrosis. 1201 - idiopathic interstitial pneumonias. Eur Respir Soc. 2022;4402. https://doi.org/10.1183/13993003.congress-2022.4402.
Nambiar A, Kellogg D, Justice J, Goros M, Gelfond J, Pascual R, et al. Senolytics dasatinib and quercetin in idiopathic pulmonary fibrosis: results of a phase I, single-blind, single-center, randomized, placebo-controlled pilot trial on feasibility and tolerability. eBioMedicine. 2023;90:104481. https://doi.org/10.1016/j.ebiom.2023.104481.
Vancheri C, Kreuter M, Richeldi L, Ryerson CJ, Valeyre D, Grutters JC, et al. Nintedanib with add-on pirfenidone in idiopathic pulmonary fibrosis: results of the INJOURNEY trial. Am J Respir Crit Care Med. 2018;197:356–63. https://doi.org/10.1164/rccm.201706-1301OC.
Flaherty KR, Fell CD, Huggins JT, Nunes H, Sussman R, Valenzuela C, et al. Safety of nintedanib added to pirfenidone treatment for idiopathic pulmonary fibrosis. Eur Respir J. 2018;52:1–10. https://doi.org/10.1183/13993003.00230-2018.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
PS reports institutional grants, personal fees, and non-financial support from PPM Services and Boehringer Ingelheim; institutional grants from Roche; personal fees from Chiesi, Novartis, Galapagos, Lupin, Pieris, Behring, AstraZeneca, Glycocore Pharma, and Menarini outside the submitted work; wife employee of AstraZeneca. EB reports personal fees from Boehringer Ingelheim and Roche outside the submitted work. EC reports personal fees from Boehringer Ingelheim outside the submitted work. GC and NB do not have any conflicts of interest to declare.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Castelli, G., Cocconcelli, E., Bernardinello, N. et al. Idiopathic Pulmonary Fibrosis: 8 Years On After Nintedanib and Pirfenidone Approval—What Is on the Horizon?. Curr Pulmonol Rep 12, 113–124 (2023). https://doi.org/10.1007/s13665-023-00315-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13665-023-00315-y