Abstract
Purpose of Review
Treatment of idiopathic pulmonary fibrosis (IPF) shifted significantly in the past few years, in the light of advances in understanding pathological pathways. The promising results coming from recent trials led to a growing number of studies dealing with IPF. The purpose of this article is to review scientific evidences supporting approved therapies and to provide an overview of experimental treatments that are currently under investigation.
Recent Findings
Approved anti-fibrotic treatments are based on large randomized trials showing the efficacy of pirfenidone and nintedanib in slowing IPF progression with an acceptable tolerability. However, we are still far from a definite cure and research efforts are focused on exploring new therapeutic targets and alternative treatment strategies.
Summary
Although pirfenidone and nintedanib remain the mainstay of IPF treatment, novel therapies are under investigation in clinical trials. Combination therapy will probably be a successful key for the future, targeting multiple pathways simultaneously.
Clinical Registration
NCT01619085
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic pulmonary fibrosis (IPF) is a chronic and progressive fibrosing interstitial pneumonia associated with an overall poor prognosis. The etiology and pathogenesis remain unclear and the clinical course is heterogeneous and unpredictable [1•]. Recently, scientific advances have led to a deeper knowledge of the molecular pathways and, consequently, the management of IPF dramatically changed, marking the end of the triple-therapy regimen [2] and welcoming the era of anti-fibrotic medications. Two drugs, pirfenidone and nintedanib, have been approved for the treatment of IPF on the basis of their efficacy in slowing disease progression, as reported in the updated 2015 American Thoracic Society (ATS)/European Respiratory Society (ERS)/Japanese Respiratory Society (JRS)/Latin American Thoracic Society (ALAT) guidelines [3•]. It represents an important milestone but we are still far from a definite cure. Great efforts are necessary to define new therapeutic targets and novel strategies. Currently, a number of clinical trials are in progress for the treatment of IPF, including investigations on combination therapies and on experimental drugs targeting alternative pathogenic pathways.
This manuscript aims at reviewing current approved therapies for IPF and at providing an overview on emerging experimental therapies. Ongoing clinical trials investigating combination therapies will be briefly described.
Approved Therapies for Idiopathic Pulmonary Fibrosis
The approval of pirfenidone and nintedanib for the treatment of IPF opened the era of the anti-fibrotic therapy and offered new hope to patients due to their efficacy in slowing functional decline and disease progression. Currently, direct comparisons are not available, and consequently, there are no evidences or recommendations to choose either of these agents over the other. The therapeutic decision usually follows a detailed evaluation and discussion with patients about potential side effects, drug interactions, and co-morbidities. A combination of these two drugs, such as combinations of either pirfenidone or nintedanib with other agents, is under investigation.
Pirfenidone
Pirfenidone was the first licensed drug for the treatment of patients with mild to moderate IPF in Europe in 2011. The US Food and Drug Administration (FDA) approval arrived in 2014, after an additional study. According to the results of clinical trials showing its positive benefit-risk profile, pirfenidone received a conditional recommendation in favor of its use in the 2015 update of ATS/ERS/JRS/ALAT guidelines [3•].
Pirfenidone is an orally bioavailable pyridone compound whose mechanism of action is still unclear. Anti-fibrotic, anti-inflammatory, and antioxidant properties were demonstrated by the results coming from in vitro studies and animal models of pulmonary fibrosis [4,5,6]. Anti-fibrotic activity is thought to rely on two predominant pathogenic mechanisms: suppression of transforming growth factor-beta (TGF-β) and other pro-fibrotic growth factors (thus preventing fibroblast differentiation into myofibroblasts) and inhibition of fibroblast proliferation.
The recommended dosage of pirfenidone is 2403 mg/day (divided three times per day) and it is usually achieved after a 2-week stepwise escalation of the dose. Capsules should be taken with a full meal to minimize gastrointestinal side effects [7]. Pirfenidone is mainly metabolized in the liver by the cytochrome P450 1A2; consequently, potential drug interactions should be carefully evaluated and avoided because of a concomitant use of other agents inhibiting or inducing these enzymes. Severe hepatic and renal impairment and contemporaneous treatment with fluvoxamine are contraindications for the use of pirfenidone [8, 9]. The most common adverse drug reactions (ADRs) are gastrointestinal (nausea, anorexia, diarrhea, vomiting, and dyspepsia) and skin-related (rash and photosensitivity) events [10]. No higher risk of drug intolerability was found in the real world in patients with significant co-morbidities and with a greater respiratory impairment [11]. Dose adjustment and education are two helpful strategies to ameliorate tolerability [12].
The therapeutic efficacy of pirfenidone is supported by four double-blind, placebo-controlled, randomized phase III trials. The first one, conducted in Japan, lasted 52 weeks and demonstrated a significant decrease in the vital capacity (VC) decline and an increase in the progression-free survival (PFS) time compared to the placebo group, with a favorable tolerability profile [13]. The CAPACITY program was designed in order to confirm the efficacy and the safety of pirfenidone. It included two trials (study 004 and 006); no serious adverse event occurred and the drug was generally well tolerated. In study 004, at week 72, differently from study 006, significant treatment effects were found in favor of pirfenidone and consisted in a reduction in the rate of forced vital capacity (FVC) decline and in a prolonged PFS [14•]. An additional trial was therefore requested by the FDA; results coming from the ASCEND (Assessment of Pirfenidone to Confirm Efficacy and Safety in Idiopathic Pulmonary Disease) study confirmed the favorable benefit-risk profile and the acceptable side-effect profile of the drug. After 52 weeks, beneficial treatment effects on disease progression were reported and measured by a reduced decline in FVC and 6-min walk distance and an improved PFS [15•]. These results led to the approval of pirfenidone by the FDA. Analysis of pooled data from clinical trials supported the safety and the beneficial effect of pirfenidone on disease progression and mortality and demonstrated that continued treatment reduced the risk of subsequent functional decline or death in patients who progressed during therapy [16,17,18,19]. Furthermore, post hoc analysis of data from the CAPACITY and ASCEND studies showed comparable beneficial effects of pirfenidone between patients with more preserved (FVC ≥ 80%) versus less preserved (FVC < 80%) lung function, supporting an early treatment [20]. Similarly, a post hoc analysis by Costabel and co-workers suggested the efficacy of pirfenidone in patients with more severe lung function impairment (FVC < 50% and/or DLCO < 35%) [21].
Long-term safety of pirfenidone was investigated in the RECAP study by enrolling patients who had completed one of the three previous phase III studies (ASCEND or CAPACITY 004 and 006). The cumulative total exposure was 2482 patient exposure years (PEY), with a median treatment duration of 88 weeks. No significant differences were found in the rate of discontinuation and in the risk of ADRs, supporting the safety profile of the drug even after a prolonged treatment [22]. Real-world data, coming from an interim analysis in the PASSPORT study, confirmed the tolerability and safety of pirfenidone [23].
Recently, results from the INJOURNEY trial were published and showed an acceptable safety and tolerability profile of nintedanib with add-on pirfenidone, opening the way to further research into combination strategies for the treatment of IPF. Another two phase IV studies have been completed exploring the pharmacokinetics (NCT 02606877) and the safety (NCT02598193) of combinations of nintedanib and pirfenidone. Results are not yet available.
the combination of pirfenidone with other drugs is under investigation. Currently, a phase IIb study is recruiting patients to evaluate the benefit/risk profile of a combination of pirfenidone and sildenafil (NCT02951429) in patients with advanced IPF and at risk of group 3 pulmonary hypertension. Trials exploring the combination of pirfenidone with vismodegib (phase Ib NCT02648048) and of pirfenidone with lebrikizumab (phase II; NCT01872689) have been completed.
Nintedanib
Nintedanib (formerly known as BIBF 1120) is an orally bioavailable 6-methoxycarbonyl-substituted indolinone with multi-target tyrosine kinase inhibition (TKI) effect against the fibroblast growth factor receptor (FGFR), the platelet-derived growth factor receptor (PDGF-R), and the vascular endothelial growth factor receptor (VEGFR) [24, 25], and other pleiotropic effects on non-receptorial tyrosine kinases as well [26,27,28]. It was originally conceived as an anti-neoplastic drug; in fact, nintedanib acts on multiple cellular pathways that have been linked to several malignant and non-malignant disorders: cell differentiation, mitosis, cell proliferation, migration, and apoptosis [29]. Nintedanib has been approved for IPF treatment in 2014 in the USA and in 2015 in Europe. As with pirfenidone, nintedanib received a conditional recommendation in favor of its use in the 2015 evidence-based international guidelines [3•].
The recommended daily dosage is 150 mg twice-a-day, but a dose reduction to 100 mg twice-a-day may be considered to achieve better tolerance and to manage adverse events, even though the highest efficacy is guaranteed by the full dose [30, 31]. The drug showed a favorable pharmacokinetic profile, with both rapid absorption and biotransformation, a high volume of distribution, a half-life of 7–19 h and a complete clearance 24 h after the administration [25, 32]. The biotransformation of nintedanib after adsorption is mainly played by methyl ester cleavage, whereas the cytochrome P450 (CYP450) pathway is less important. The product of the metabolism of the drug is the carboxylate free acid BIBF 1202; then, this first molecule is conjugated to glucuronic acid, forming a long half-life metabolite (1-O-acylglucoronide) [33].
The Safety and efficacy of nintedanib in the treatment of IPF have been shown in three randomized, double-blind, placebo-controlled clinical trials: the phase II TOMORROW trial [34•] and the phase III INPULSIS-1 and INPULSIS-2 trials [35]. The TOMORROW (To Improve Pulmonary Fibrosis With BIBF 1120) trial was designed as a dose-finding study; four doses (50 mg once-a-day; 50 mg, 100 mg, and 150 mg twice-a-day) or placebo were tested for 52 weeks. At the end of the study, the adjusted annual decline in FVC (primary end point of the trial) was significantly lower in the 150-mg twice-a-day group than in the placebo group (60 ml/year vs. 190 ml/year); a reduction in incidence of acute exacerbations and a better quality of life were also observed [34•]. The INPULSIS trials were designed as two 52-week identical placebo-controlled and multicenter studies; the efficacy and safety of nintedanib 150 mg twice-a-day were tested in 1066 patients with IPF. The primary end point was again the annual rate of change in FVC. In both trials, the rate of decline was significantly lower in the nintedanib group (114.7 ml/year vs. 239.8 ml/year, P < 0.001 in INPULSIS-1; 113.6 ml/year vs. 207 ml/year, P < 0.001 in INPULSIS-2). The two studies differed in secondary end points such as prevention of acute exacerbations and quality of life that were significantly better only in INPULSIS-2 [35]. The efficacy of nintedanib in homogeneous groups of patients has also been verified by subgroup analyses of pooled data from the INPULSIS trials, showing no significant difference in functional decline by sex, age, race, pulmonary function at baseline, presence/absence of emphysema, and use of other medications (namely systemic corticosteroids and anti-acid medications). Data about race have been confirmed also in the Japanese patients enrolled in the two INPULSIS trials [36,37,38]. The reduction in both frequency and mortality of acute exacerbations has also been observed in pooled data from the TOMORROW and INPULSIS trials. Furthermore, patients with a preserved lung function (FVC > 90%) had a similar rate of FVC decline when compared to patients with a reduced one (FVC ≤ 90%) in a subgroup analysis of the two INPULSIS trials [39]. An interim analysis of the open-label extension trial INPULSIS-ON showed both efficacy and safety of long-term nintedanib 150 mg twice-a-day, similarly to INPULSIS trials (clinicaltrials.gov identifier number NCT01619085). In addition, the absolute average rate of decline is comparable between patients with more severe impairment of FVC and patients with a relatively preserved function (FVC ≤ 50% vs. FVC > 50%) [40, 41].
Treatment with nintedanib is safe in most patients, with a usually manageable adverse-event profile. The most common ADRs are gastrointestinal: diarrhea, nausea, elevated liver enzymes. The diarrhea is quite common, but led to permanent drug discontinuation in less than 5% of patients in both INPULSIS trials. Overall, about 20% of patients in TOMORROW and INPULSIS trials permanently discontinued the drug for gastrointestinal adverse events. An increased risk of bleeding, mainly non-serious events such as epistaxis, has been reported. Dose adjustments allow a better management of ADRs [31, 42, 43].
Nintedanib is currently investigated in combination therapy with other molecules. The INSTAGE, a 24-week, double-blind, randomized, parallel-group study (NCT02802345), evaluated the efficacy and safety of nintedanib co-administered with oral sildenafil compared to nintedanib alone in patients with advanced lung function impairment [44]. The study has been completed and we are waiting for the publication of the results.
Experimental Therapies for Idiopathic Pulmonary Fibrosis
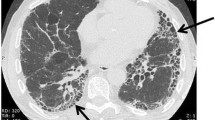
Pirfenidone and nintedanib were shown to slow but not to reverse disease progression. The pathogenesis of IPF is not completely understood; several molecular pathways are involved in the inception and progression of this disabling and lethal disease. Currently, numerous ongoing clinical trials are investigating new drugs for the treatment of IPF, targeting many potential underlying pathogenic mechanisms (Fig. 1).
Experimental Therapies Targeting Pro-fibrotic Signaling Pathways
Pentraxin-2 Analogues
Pentraxin-2 (PTX-2) is an endogenous blood plasma protein, also known as serum amyloid P, that regulates the wound healing process and scar resolution [45]. PTX-2 inhibits the differentiation of circulating monocytes into fibrocytes and M2 macrophages, a phenotype of macrophage that produces pro-fibrotic mediators. In IPF patients, circulating levels of PTX-2 are reduced and M2 macrophages are predominant. Regulating macrophage phenotype is a promising therapeutic approach for lung fibrosis. In mice models, the administration of PTX-2 intravenously has been associated with decreased fibrosis extent [46]. PRM-151, a recombinant form of human PTX-2 [47], has been administered as single ascending intravenous doses to healthy subjects in a first-in-human trial [48]. The results showed a good safety and tolerability profile. In addition, PRM-151 has been associated with a reduction in circulating fibrocytes in IPF patients [48]. A phase I randomized, double-blind, placebo-controlled trial (NCT01254409) has demonstrated that PRM-151 is safe and well tolerated. Furthermore, trends toward improvement, although not statistically significant, have been observed for FVC and 6-min walk test [49]. The results of a phase II study (NCT02550873) on efficacy and safety of PRM-151 administered through 28 weeks to IPF subjects were recently published. A slower decline in lung function was observed in IPF patients treated with recombinant human pentraxin 2 in comparison to the placebo group [50].
Anti-connective Tissue Growth Factor Antibodies
Connective tissue growth factor (CTGF) is a matricellular protein involved in the wound healing process. CTGF links extracellular matrix (ECM) and cell surface and mediates cell adhesion, migration, proliferation, and angiogenesis [51]. In preclinical mice models, CTGF induces a pro-fibrotic response both alone [52] or in combination with TGF-β [53]. IPF subjects present higher levels of CTGF in BAL fluid compared with healthy controls [54]. Due to its role in pro-fibrotic pathways, CTGF is an interesting target for IPF treatment. Anti-CTGF antibodies demonstrated to inhibit collagen deposition and to reduce histological signs of fibrosis [53]. An open-label phase II study has evaluated the safety and efficacy of two doses of pamrevlumab (FG-3019), a human monoclonal anti-CTGF antibody [55], administered by intravenous infusion for 45 weeks in IPF patients. FG-3019 presented a good safety profile and yielded promising results with regard to changes in pulmonary function and extent of pulmonary fibrosis by imaging [55]. To confirm these findings, a randomized, placebo-controlled, double-blind phase II trial (NCT01890265) has been completed. This study aimed to evaluate the safety and tolerability of FG-3019, and the efficacy of this antibody in slowing FVC decline and lung fibrosis (assessed by quantitative HRCT) in subjects with IPF [56]. Results were presented at the ERS 2017 Conference: patients treated with pamrevlumab showed a statistically significant reduction in the rate of lung fibrosis progression in comparison to placebo [57].
Another antibody, PBI-4050, demonstrated to reduce CTGF activity and collagen I mRNA expression in preclinical studies. A phase II open-label single-arm trial exploring the safety and tolerability of oral administration of 800 mg per day of PBI-4050 in 40 adult IPF patients (NCT02538536) is now completed. Preliminary results found that PBI-4050 has a strong safety and tolerability profile. In addition, this antibody seems to be clinically effective in reducing lung function decline and disease progression, either alone or in combination with nintedanib [58].
Anti-integrin Antibodies
Integrins are glycoproteins that bind cells to each other or to the basement membrane. Integrins also activate TGF-β by displacing its ligand, latency activated peptide (LAP). The most pro-fibrotic pathway is the one mediated by TGF-β1 under the regulation of integrin ανβ6. The TGF-β1 pathway recruits fibroblasts and stimulates myofibroblast differentiation and persistence [59]. In murine models, partial inhibition of αvβ6 integrin prevents bleomycin-induced pulmonary fibrosis [60]. A phase II study (NCT01371305, completed) tested safety and tolerability of the humanized monoclonal antibody against αvβ6 integrin in IPF patients. Study results are still unpublished. A first-in-human phase I study has been conducted on a single daily nebulized drug dose of GSK3008348, a novel integrin αvβ6 antagonist (NCT02612051). GSK3008348 resulted well tolerated at single doses up to 3000 mcg in healthy participants [61].
Autotaxin-LPA Pathway Inhibitors
The autotaxin-lysophosphatidic acid (LPA) pathway determines fibroblast recruitment and persistence, epithelial apoptosis, and endothelial damage. The enzyme autotaxin and its product LPA are elevated in BAL fluid of IPF patients compared with healthy subjects [62]. The inhibition of autotaxin activity aims to reduce LPA. A randomized, double-blind, parallel-group, placebo-controlled, exploratory phase IIa trial (NCT02738801, completed), compared to 600 mg orally administered GLPG1690 (autotaxin inhibitor) [63] versus placebo for 12 weeks. Study results show a stabilization of FVC in the treatment group. Focusing on the same pathogenic pathway, the effect of an oral LPA 1 receptor antagonist (BMS-986020) on FVC decline has been investigated in IPF patients in a randomized placebo-controlled phase II trial (NCT01766817).
Anti-lysyl Oxidase Antibodies
The lysyl oxidase (LOX) family is composed of enzymes that confer stiffness to the ECM by catalyzing collagen type I cross-linking. One of these enzymes, LOX-like 2 (LOXL2) was found to be increased in lung biopsies of IPF patients; therefore, its pathogenic role has been hypothesized. Thus, some researchers tried to reduce ECM deposition by inhibiting this enzyme. A phase II randomized, double-blind, placebo-controlled trial tested a human antibody GS6624 (simtuzumab). Simtuzumab did not improve progression-free survival in a well-defined population of IPF patients and the results do not support its use for patients with IPF [64].
Experimental Therapies Targeting Immunity
Over the years, an abnormal activation of the immune system has been postulated as a potential pathogenetic mechanism involved in IPF and was the rationale for the administration of immunomodulatory agents. Currently, it is well known that no effective modulation of the immune system is associated with evidence of improving mortality or modifying the clinical course of IPF [2]. However, a certain involvement of immunity in IPF pathobiology was observed, although its significance is still under debate. Therefore, several therapeutic strategies targeting immunity and autoimmunity have been proposed over time and new drugs are currently under investigation.
Tralokinumab, Lebrikizumab, QAX576, SAR156597
A certain grade of Th2 activation was observed in IPF. The Th2 cytokines IL-4, IL-5, and IL-13 are upregulated in cellular cultures from IPF patients if compared to controls [65]. IL-13 receptors are more abundant in lung biopsies from UIP patients and fibroblastic foci strongly stain for IL-4 and IL-13 receptors [66]. These findings formed the basis for exploring the effects of potential therapeutic strategies targeting IL4, IL13, and their receptors.
Two phase II studies were designed to explore the safety and efficacy of multiple doses of tralokinumab, a human recombinant monoclonal antibody blocking IL13 (NCT02036580, NCT01629667). One of them was prematurely stopped due to the lack of efficacy in the primary end point (annual change of FVC) after a predefined interim analysis, despite an acceptable safety and tolerability profile [67]. The subgroup analysis on periostin levels, a putative marker of IL13 axis activation, could not be performed and concerns regarding the low retention rate were raised, leading to non-definitive conclusions [68].
Lebrikizumab is another humanized anti-IL13 monoclonal antibody. A phase II study comparing the safety profile and the effects of lebrikizumab alone or in combination with pirfenidone, compared to placebo or to pirfenidone, was recently completed (NCT01872689). The results have been reported for the first time at the ATS 2018 International Conference. No statistically significant beneficial effects on lung function or mortality was observed in favor of lebrikizumab both as a monotherapy [69] and in combination with pirfenidone [70] over 52 weeks of treatment in IPF patients. A safety profile was reported. Combination therapy showed a favorable trend on mortality and acute exacerbations.
An open-label multicenter study investigating the effects of a single intravenous dose of QAX576, a fully human anti-IL13 monoclonal antibody, was closed early because of the slow enrollment rate (NCT00532233). A phase II study addressed to assess the safety, tolerability, efficacy, pharmacodynamics, and pharmacokinetics of QAX576 in rapidly progressive IPF over 1 year of treatment was terminated; reasons were not reported (NCT01266135).
SAR156597 is a dual anti-IL4 and IL13 monoclonal antibody tested in IPF. After the conclusion of a phase I study on safety and tolerability of different dosages (NCT01529853), a phase II study on efficacy of this drug has been recently completed (NCT02345070). SAR156597 was not associated with a favorable treatment effect on lung function decline and on disease progression both as monotherapy and in combination with the current standard of care (either pirfenidone or nintedanib). These results were presented at the ATS 2018 International Conference [71].
Rituximab
Some IPF patients display autoantibodies targeting structural components of the matrix with potential prognostic role for some of them [72,73,74,75,76]. Although the effects of B lymphocyte-depleting treatment have been explored in non IPF-ILDs with promising results [77], in IPF the evidence is scarce and debated. A phase II trial was designed to evaluate the efficacy of rituximab in reducing the circulating levels of autoantibody potentially involved in lung damage in IPF. It was completed in 2017. The primary end point was the titer of anti-HEp-2 autoantibodies over 9 months, and among secondary end points, there are changes in FVC and the rate of exacerbation. No results have been yet published (NCT01969409).
Tipelukast
The 5-lipoxigenase(5-LO)/leukotriene pathway emerged as another potential immune pathogenic mechanism involved in lung fibrosis. Arachidonic acid-derived metabolites, produced by various immune cell types via 5-LO pathway, are involved in the host defense system against infection and invasion by foreign bodies. They participate in the pathogenesis of IPF but their role in IPF pathobiology is still unclear [78]. IPF patients show elevated concentration of leukotriene B4 (LTB4), one of the most potent chemoattractants and activators of leukocytes, both in bronchoalveolar lavage fluid and lung tissues [79,80,81]. In animal models, the administration of a non-selective leukotriene B4 receptor antagonist attenuated the bleomicin-induced lung fibrosis and hydroxyproline content, through the inhibition of inflammation, neutrophil chemotaxis, and the modulation of several cytokines [82, 83]. Currently a phase II trial evaluating the efficacy, safety, and tolerability of tipelukast in IPF is recruiting participants (NCT02503657). This novel, orally bioavailable molecule exerts multiple effects including leukotriene receptor antagonism and inhibition of phosphodiesterases and 5-LO.
IW001
It is possible to adopt specific immune-mediated strategies aimed at obtaining tolerance toward structural components over-expressed in IPF lung interstitium that often trigger autoantibody production. This is the case of oral immunotherapy for type V collagen (Col(V)). Results from a phase I clinical trial (NCT01199887) showed the safety and tolerability of an oral solution of purified bovine Col(V) in IPF patients with positive Col(V) autoantibodies and demonstrated an intriguing trend toward FVC stabilization [84].
Experimental Therapies Targeting Tyrosine Kinases
Tyrosine kinases are implicated in the pathogenesis of IPF as they control several signaling pathways that are crucial for cellular homeostasis. They represent important potential therapeutic targets and many agents inhibiting tyrosine kinases are now under investigation.
Src is a non-receptor protein-tyrosine kinase codified by a proto-oncogene that is involved in various cellular signaling and transduction pathways. In fibroblasts, this molecule has been found in endosomes, perinuclear membranes, secretory vesicles, and cytoplasmic face of the plasma membrane. Src interacts with several tyrosine kinase receptors at the plasma membrane, including fibroblast growth factor receptor (FGFR), platelet-derived growth factor receptors (PDGF-R), epidermal growth factor receptor (EGFR), and insulin-like growth factor (IGFR) providing a bi-directional flow of information. Moreover, it can interact with integrin, G protein-coupled receptors and other intracellular kinases as focal adhesion kinase (FAK) and mitogen-activated protein kinases (MAPKs) [85].
Dasatinib is an inhibitor of BCR-ABL and Src family kinases (Src, Lck, Yes, Fyn). It is approved for the treatment of chronic myeloid leukemia and it showed positive promising effect in animal models of bleomycin-induced lung fibrosis and in other lung interstitial diseases [86, 87]. A phase I, open-label, interventional, single-group assignment human study in IPF is currently recruiting participants. The purpose of the study is to evaluate the effects of the association of dasatinib and quercetin, an antioxidant agent, on the expression of pro-inflammatory cells obtained by skin biopsy of IPF patients. The estimated primary completion date is December 2018 (NCT02874989).
Stem Cells
Regenerative medicine and the use of stem cells represent an intriguing strategy explored in the last decade with potential therapeutic efficacy in patients suffering from chronic lung diseases including IPF.
In 2014, in a single-center, non-randomized, dose-escalation phase Ib trial, patients with moderately severe IPF received either 1 × 106 or 2 × 106 unrelated-donor, placenta-derived mesenchymal stem cells (MSC)/kg via a peripheral vein. The researchers showed that intravenous MSC administration was feasible with a good short-term safety profile [88].
A phase Ib, non-randomized, clinical trial assessed the safety and tolerability of multiple endobronchial infusions of autologous adipose-derived stromal cells (ADSCs)-stromal vascular fraction (SVF) (0.5 million cells per kg of body weight per infusion) in patients with IPF. While short-term infusion transient desaturation, fever, and heartburn were reported, no long-term adverse events or ectopic tissue formation were observed [89].
In 2016, the first clinical phase I pilot study evaluating safety and tolerability of intravenous allotransplant of three different dosages of exogenous human bone narrow–derived MSC in IPF patients was published (NCT02013700). It did not report any significant treatment-related serious adverse events and showed a 3.0% mean decline in percentage predicted FVC and a 5.4% mean decline in percentage predicted diffusing capacity for carbon monoxide (DLco) 60 weeks after infusion [90].
In May 2018, a clinical trial phase I, open, multicentric, non-randomized, study aiming to evaluate the safety and feasibility of the endobronchial administration of mesenchymal autologous stem cells derived from bone marrow (BM-MSC) in patients with mild-to-moderate IPF was completed (NCT01919827). Furthermore, an interesting ongoing phase 1–2, open-label study is going to evaluate the safety and efficacy of endobronchial administration of autologous lung stem cells isolated from IPF patient’s distal airways and expanded in vitro (NCT02745184). Estimated study completion date is December 2018.
Antibiotics and Antiviral Drugs
The role of viruses and bacteria in the pathogenesis, progression, and acute exacerbation of IPF is still unclear: it represents an interesting field of research and the comprehension of viral and bacterial involvement in IPF could help the development of novel therapeutic approaches [91].
It has been proposed that viruses could play a key role as cofactors in the initiation and progression of IPF. Therefore, antiviral therapy could represent an important tool to modify the course of disease. Egan and co-workers conducted a small but significant study of open-label ganciclovir in 14 patients with severe IPF and positive EBV-IgG serology: it has been interesting to observe that following a period of 2 weeks of ganciclovir, 9 of the 14 patients showed an improvement in 8 weeks in at least three of the four outcomes, such as reduction in steroid therapy, improvement in FVC, and an improvement in DTPA (diethylenetriaminepentaacetic acid) clearance [92].
The role of bacteria in the pathogenesis and progression of IPF is less clear: recent data suggest an association between IPF and bacteria/lung microbiome [91, 93].
Trials on antibiotic therapy may help to clarify if this altered respiratory microbiome plays a key role in causing/modifying IPF or not. In a double-blind, multicenter study, 181 IPF patients have been randomized to receive co-trimoxazole 960 mg twice-daily or placebo for 12 months in addition to “standard” anti-fibrotic therapy. Results show that co-trimoxazole has no effect on lung function, but improves quality of life, reduces the rate of patients that need to increase oxygen therapy, and, most of all, reduces all-cause mortality. These findings could be due to its antimicrobial activity as there is a remarkable decrease in the number of infections in those adhering to treatment [94].
An ongoing randomized, un-blinded, phase III, multi-center clinical trial is investigating the effect of standard care, versus standard of care plus antimicrobial therapy (co-trimoxazole or doxycycline), on clinical outcomes in patients diagnosed with IPF (NCT02759120). Subjects are randomized 1:1 to either receive 160 mg trimethoprim/800 mg sulfamethoxazole (double strength co-trimoxazole) twice-daily plus folic acid 5 mg daily OR doxycycline 100 mg once-daily if weight < 50 kg or 100 mg twice-daily if weight > 50 kg. Patients randomized to receive antimicrobial therapy will take co-trimoxazole. In case of allergy or contraindication to co-trimoxazole, renal insufficiency, hyperkalemia, or concomitant therapy with an angiotensin-converting enzyme inhibitor, angiotensin receptor blocker, or potassium-sparing diuretic, they will receive doxycycline. Estimated primary completion date is July 2019.
A single-center, prospective, randomized, double-blind, 2-treatment, 2-period crossover study with two 12-week treatment periods with azithromycin (AZT) separated by a 4-week drug-free washout period and a 4-week follow-up period is ongoing. The investigators hypothesize that immunomodulatory treatment of IPF patients with AZT might reduce cough frequency and might improve lung function (NCT02173145). Estimated primary completion date is December 2018.
Conclusions
Recent insights into pathobiology and the approval of two anti-fibrotic drugs marked a new era for the treatment of IPF, encouraging investigations and becoming a hot research topic. Despite these latest advances, further strides need to be made with the aim of increasing knowledge about this life-threatening disease and improving survival. Precision medicine could be a key tool for the next future, helping patients to receive tailored treatments. Combination therapies currently are gaining great interest among the scientific community. Combining two or more agents, targeting different pathways or treating concomitant conditions, could reveal as a successful strategy and it could become a cornerstone of IPF treatment. In this period of extraordinary efforts in IPF research, scientific developments are expected to happen and to provide additional evidences and stronger recommendations in order to optimize care and, hopefully, to finally change the destiny of IPF patients.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
• Raghu G, Remy-Jardin M, Myers JL, Richeldi L, Ryerson CJ, Lederer DJ, et al. Diagnosis of idiopathic pulmonary fibrosis. An official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med. 2018;198:e44–68 This international, evidence-based guideline provides an update on the diagnosis of IPF.
Idiopathic Pulmonary Fibrosis Clinical Research Network, Raghu G, Anstrom KJ, King TE, Lasky JA, Martinez FJ. Prednisone, azathioprine, and N-acetylcysteine for pulmonary fibrosis. N Engl J Med. 2012;366:1968–77.
• Raghu G, Rochwerg B, Zhang Y, Garcia CAC, Azuma A, Behr J, et al. An official ATS/ERS/JRS/ALAT clinical practice guideline: treatment of idiopathic pulmonary fibrosis: an update of the 2011 clinical practice guideline. Am J Respir Crit Care Med. 2015;192:e3–e19 This guideline provides recommendations for or against specific agents based on literature evidences; nintedanid and pirfenidone received for the first time a conditional recommandation for the treatment in IPF patients.
Conte E, Gili E, Fagone E, Fruciano M, Iemmolo M, Vancheri C. Effect of pirfenidone on proliferation, TGF-B-induced myofibroblast differentiation and fibrogenic activity of primary human lung fibroblasts. Eur J Pharm Sci. 2014;58:13–9.
Iyer SN, Gurujeyalakshmi G, Giri SN. Effects of pirfenidone on transforming growth factor-beta gene expression at the transcriptional level in bleomycin hamster model of lung fibrosis. J Pharmacol Exp Ther. 1999;291:367–73.
Nakayama S, Mukae H, Sakamoto N, Kakugawa T, Yoshioka S, Soda H, et al. Pirfenidone inhibits the expression of HSP47 in TGF-β1-stimulated human lung fibroblasts. Life Sci. 2008;82:210–7.
Meyer KC, Decker CA. Role of pirfenidone in the management of pulmonary fibrosis. Ther Clin Risk Manag. 2017;13:427–37.
Kim ES, Keating GM. Pirfenidone: a review of its use in idiopathic pulmonary fibrosis. Drugs 2015.
Spagnolo P, Maher TM, Richeldi L. Idiopathic pulmonary fibrosis: recent advances on pharmacological therapy. Pharmacol. Ther. [Internet] Elsevier Inc. 2015;152:18–27. https://doi.org/10.1016/j.pharmthera.2015.04.005.
Lancaster LH, de Andrade JA, Zibrak JD, Padilla ML, Albera C, Nathan SD, Wijsenbeek MS, Stauffer JL, Kirchgaessler KU, Costabel U. Pirfenidone safety and adverse event management in idiopathic pulmonary fibrosis. Eur Respir Rev. [Internet] 2017; 26Available from: https://doi.org/10.1183/16000617.0057-2017.
Galli JA, Pandya A, Vega-Olivo M, Dass C, Zhao H, Criner GJ. Pirfenidone and nintedanib for pulmonary fibrosis in clinical practice: tolerability and adverse drug reactions. Respirology. 2017;22:1171–8.
Margaritopoulos GA, Vasarmidi E, Antoniou KM. Pirfenidone in the treatment of idiopathic pulmonary fibrosis: an evidence-based review of its place in therapy. Core Evid. [Internet]. 2016;11:11–22 Available from: http://www.ncbi.nlm.nih.gov/pubmed/27445644%5Cn http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC4936814.
Taniguchi H, Ebina M, Kondoh Y, Ogura T, Azuma A, Suga M, et al. Pirfenidone Clinical Study Group in Japan. Pirfenidone in idiopathic pulmonary fibrosis. Eur Respir J. 2010;35:821–9.
• Noble PW, Albera C, Bradford WZ, Costabel U, Glassberg MK, Kardatzke D, et al. Pirfenidone in patients with idiopathic pulmonary fibrosis (CAPACITY): two randomised trials. Lancet. 2011;377(9779):1760–9 This study supported the use of pirfenidone in the treatment of IPF.
• King TE, Bradford WZ, Castro-Bernardini S, Fagan EA, Glaspole I, Glassberg MK, et al. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N Engl J Med BioMed Central. 2014;370:2083–92 This study confirmed the efficacy of pirfenidone in reducing disease progression in IPF, leading to its approval by the FDA.
Lancaster L, Albera C, Bradford WZ, Costabel U, Du Bois RM, Fagan EA, et al. Safety of pirfenidone in patients with idiopathic pulmonary fibrosis: integrated analysis of cumulative data from 5 clinical trials. BMJ Open Resp Res [Internet]. 2016;3. https://doi.org/10.1136/bmjresp-2015-000105.
Noble PW, Albera C, Bradford WZ, Costabel U, Du Bois RM, Fagan EA, et al. Pirfenidone for idiopathic pulmonary fibrosis: analysis of pooled data from three multinational phase 3 trials. Eur Respir J [Internet]. 2016, 47:243–53. https://doi.org/10.1183/13993003.00026-2015.
Nathan SD, Albera C, Bradford WZ, Costabel U, du Bois RM, Fagan EA, et al. Effect of continued treatment with pirfenidone following clinically meaningful declines in forced vital capacity: analysis of data from three phase 3 trials in patients with idiopathic pulmonary fibrosis. Thorax [Internet]. 2016;71:429–35. https://doi.org/10.1136/thoraxjnl-2015-207011.
Nathan SD, Albera C, Bradford WZ, Costabel U, Glaspole I, Glassberg MK, et al. Effect of pirfenidone on mortality: pooled analyses and meta-analyses of clinical trials in idiopathic pulmonary fibrosis. Lancet Respir Med. 2017;5:33–41.
Albera C, Costabel U, Fagan EA, Glassberg MK, Gorina E, Lancaster L, et al. Efficacy of pirfenidone in patients with idiopathic pulmonary fibrosis with more preserved lung function. Eur Respir J. 2016.
Robalo-Cordeiro C, Campos P, Carvalho L, Borba A, Clemente S, Freitas S, Furtado S, Jesus JM, Leal C, Marques A, Melo N, Souto-Moura C, Neves S, Sousa V, Santos A, Morais A. Idiopathic pulmonary fibrosis in the era of antifibrotic therapy: Searching for new opportunities grounded in evidence. Rev Port Pneumol (English Ed. 2017; 23: 287–293.
Costabel U, Albera C, Lancaster LH, Lin C-Y, Hormel P, Hulter HN, et al. An open-label study of the long-term safety of pirfenidone in patients with idiopathic pulmonary fibrosis (RECAP). Respiration [Internet]. 2017:408–15. https://doi.org/10.1159/000479976.
Koschel D, Cottin V, Skold M, Tomassetti S, Azuma A, Giot C, et al. Pirfenidone post-authorization safety registry (PASSPORT) – interim analysis of IPF treatment. Eur Respir J. 2014;44.
Mazzei ME, Richeldi L, Collard HR. Nintedanib in the treatment of idiopathic pulmonary fibrosis. Ther Adv Respir Dis. 2015;9:121–9.
Roth GJ, Binder R, Colbatzky F, Dallinger C, Schlenker-Herceg R, Hilberg F, et al. Nintedanib: from discovery to the clinic. J Med Chem [Internet]. 2015;58:1053–63 Available from: http://www.ncbi.nlm.nih.gov/pubmed/25474320.
Sun L, Tran N, Tang F, App H, Hirth P, McMahon G, et al. Synthesis and biological evaluations of 3-substituted indolin-2-ones: a novel class of tyrosine kinase inhibitors that exhibit selectivity toward particular receptor tyrosine kinases. J Med Chem. 1998;41:2588–603.
Hilberg F, Roth GJ, Krssak M, Kautschitsch S, Sommergruber W, Tontsch-Grunt U, et al. BIBF 1120: triple angiokinase inhibitor with sustained receptor blockade and good antitumor efficacy. Cancer Res. 2008;68:4774–82.
Roth GJ, Heckel A, Colbatzky F, Handschuh S, Kley J, Lehmann-Lintz T, et al. Design, synthesis, and evaluation of indolinones as triple angiokinase inhibitors and the discovery of a highly specific 6-methoxycarbonyl-substituted indolinone (BIBF 1120). J Med Chem. 2009;52:4466–80.
Grimminger F, Schermuly RT, Ghofrani HA. Targeting non-malignant disorders with tyrosine kinase inhibitors. Nat Rev Drug Discov Nat Publ Group. 2010;9:956–70.
Fukihara J, Kondoh Y. Nintedanib (OFEV) in the treatment of idiopathic pulmonary fibrosis. Expert Rev Respir Med [Internet]. 2016;10:1247–54 Available from: http://www.ncbi.nlm.nih.gov/pubmed/27744713.
Varone F, Sgalla G, Iovene B, Bruni T, Richeldi L. Nintedanib for the treatment of idiopathic pulmonary fibrosis. Expert Opin Pharmacother [Internet]. 2018;19:167–75 Available from: http://www.tandfonline.com/action/journalInformation?journalCode=ieop20.
Dallinger C, Trommeshauser D, Marzin K, Liesener A, Kaiser R, Stopfer P. Pharmacokinetic properties of nintedanib in healthy volunteers and patients with advanced cancer. J Clin Pharmacol [Internet]. 2016;56:1387–94 Available from: http://www.ncbi.nlm.nih.gov/pubmed/27093880.
Stopfer P, Rathgen K, Bischoff D, Lüdtke S, Marzin K, Kaiser R, et al. Pharmacokinetics and metabolism of BIBF 1120 after oral dosing to healthy male volunteers. Xenobiotica. [Internet]. 2011;41:297–311 Available from: http://www.ncbi.nlm.nih.gov/pubmed/21204634.
• Richeldi L, Costabel U, Selman M, Kim DS, Hansell DM, Nicholson AG, et al. Efficacy of a tyrosine kinase inhibitor in idiopathic pulmonary fibrosis. N Engl J Med [Internet]. 2011;365:1079–87 Available from: http://www.ncbi.nlm.nih.gov/pubmed/21992121. This study supported the efficacy and safety of nintedanib in the treatment of IPF.
Richeldi L, du Bois RM, Raghu G, Azuma A, Brown KK, Costabel U, et al. INPULSIS Trial InvestigatorsEfficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl J Med [Internet]. 2014;370:2071–82 Available from: http://www.ncbi.nlm.nih.gov/pubmed/24836310.
Costabel U, Inoue Y, Richeldi L, Collard HR, Tschoepe I, Stowasser S, et al. Efficacy of nintedanib in idiopathic pulmonary fibrosis across prespecified subgroups in INPULSIS. Am J Respir Crit Care Med [Internet]. 2016;193:178–85 Available from: http://www.ncbi.nlm.nih.gov/pubmed/26393389.
Kolb M, Richeldi L, Behr J, Maher TM, Tang W, Stowasser S, Hallmann C, du Bois RM. Nintedanib in patients with idiopathic pulmonary fibrosis and preserved lung volume. Thorax [Internet] McMaster University, Hamilton, Ontario, Canada. National Institute for Health Research Southampton Respiratory Biomedical Research Unit and Clinical and Experimental Sciences, University of Southampton, Southampton, UK. Medizinische Klinik und Poliklinik; 2017; 72: 340–346Available from: http://www.ncbi.nlm.nih.gov/pubmed/27672117.
Azuma A, Taniguchi H, Inoue Y, Kondoh Y, Ogura T, Homma S, Fujimoto T, Sakamoto W, Sugiyama Y, Nukiwa T. Nintedanib in Japanese patients with idiopathic pulmonary fibrosis: a subgroup analysis of the INPULSIS® randomized trials. Respirology [Internet] John Wiley & Sons, Ltd; 2017; 22: 750–757Available from: https://doi.org/10.1111/resp.12960.
Richeldi L, Cottin V, du Bois RM, Selman M, Kimura T, Bailes Z, et al. Nintedanib in patients with idiopathic pulmonary fibrosis: combined evidence from the TOMORROW and INPULSIS(®) trials. Respir Med [Internet]. 2016;113:74–9 Available from: http://www.ncbi.nlm.nih.gov/pubmed/26915984.
Crestani B, Quaresma M, Kaye M, Stansen W, Stowasser S, Kreuter M. Long-term treatment with nintedanib in patients with IPF: an update from INPULSIS®-ON. 1.5 Diffus. Parenchymal Lung Dis. [Internet] European Respiratory Society; 2016. p. OA4960Available from: https://doi.org/10.1183/13993003.congress-2016.OA4960.
Wuyts WA, Kolb M, Stowasser S, Stansen W, Huggins JT, Raghu G. First data on efficacy and safety of nintedanib in patients with idiopathic pulmonary fibrosis and forced vital capacity of ≤50% of predicted value. Lung [Internet] Springer; 2016; 194: 739–743 Available from: http://www.ncbi.nlm.nih.gov/pubmed/27377558.
Mazzei ME, Richeldi L, Collard HR. Nintedanib in the treatment of idiopathic pulmonary fibrosis. Ther Adv Respir Dis [Internet]. 2015;9:121–9 Available from: http://www.ncbi.nlm.nih.gov/pubmed/25862013.
Cottin V. The safety and tolerability of nintedanib in the treatment of idiopathic pulmonary fibrosis. Expert Opin Drug Saf [Internet]. 2017 [cited 2017 Jun 15];16:857–65. https://doi.org/10.1080/14740338.2017.1338268.
Inchingolo R, Condoluci C, Smargiassi A, Mastrobattista A, Boccabella C, Comes A, Golfi N, Richeldi L. Are newly launched pharmacotherapies efficacious in treating idiopathic pulmonary fibrosis? Or is there still more work to be done? Expert Opin. Pharmacother. [Internet] Taylor & Francis; 2017; 00: 1–12 Available from: https://doi.org/10.1080/14656566.2017.1383382.
Pilling D, Roife D, Wang M, Ronkainen SD, Crawford JR, Travis EL, et al. Reduction of bleomycin-induced pulmonary fibrosis by serum amyloid P. J Immunol [Internet]. 2007 [cited 2018 May 20];179:4035–44 Available from: http://www.ncbi.nlm.nih.gov/pubmed/17785842.
Murray LA, Chen Q, Kramer MS, Hesson DP, Argentieri RL, Peng X, et al. TGF-beta driven lung fibrosis is macrophage dependent and blocked by Serum amyloid P. Int J Biochem Cell Biol [Internet]. 2011 [cited 2018 May 20];43:154–62 Available from: http://www.ncbi.nlm.nih.gov/pubmed/21044893.
Murray LA, Rosada R, Moreira AP, Joshi A, Kramer MS, Hesson DP, Argentieri RL, Mathai S, Gulati M, Herzog EL, Hogaboam CM, Serum Amyloid P Therapeutically attenuates murine bleomycin-induced pulmonary fibrosis via its effects on macrophages. Feghali-Bostwick C, editor. PLoS One [Internet] 2010 [cited 2018 May 20]; 5: e9683Available from: http://www.ncbi.nlm.nih.gov/pubmed/20300636.
Dillingh MR, van den Blink B, Moerland M, van Dongen MGJ, Levi M, Kleinjan A, et al. Recombinant human serum amyloid P in healthy volunteers and patients with pulmonary fibrosis. Pulm Pharmacol Ther [Internet]. 2013 [cited 2018 May 20];26:672–6 Available from: http://www.ncbi.nlm.nih.gov/pubmed/23380438.
van den Blink B, Dillingh MR, Ginns LC, Morrison LD, Moerland M, Wijsenbeek M, et al. Recombinant human pentraxin-2 therapy in patients with idiopathic pulmonary fibrosis: safety, pharmacokinetics and exploratory efficacy. Eur Respir J [Internet] European Respiratory Society. 2016 [cited 2018 May 20];47:889–97 Available from: http://www.ncbi.nlm.nih.gov/pubmed/26869678.
Raghu G, van den Blink B, Hamblin MJ, Brown AW, Golden JA, Ho LA, et al. Effect of recombinant human pentraxin 2 vs placebo on change in forced vital capacity in patients with idiopathic pulmonary fibrosis: a randomized clinical trial. JAMA [Internet] American Medical Association. 2018 [cited 2018 Aug 21];319:2299–307 Available from: https://jamanetwork.com/journals/jama/article-abstract/2681945.
Leask A, Parapuram SK, Shi-wen X, Abraham DJ. Connective tissue growth factor (CTGF, CCN2) gene regulation: a potent clinical bio-marker of fibroproliferative disease? J Cell Commun Signal [Internet]. 2009 [cited 2018 May 20];3:89–94 Available from: http://www.ncbi.nlm.nih.gov/pubmed/19156539.
Bonniaud P, Martin G, Margetts PJ, Ask K, Robertson J, Gauldie J, et al. Connective tissue growth factor is crucial to inducing a profibrotic environment in “fibrosis-resistant” Balb/c mouse lungs. Am J Respir Cell Mol Biol [Internet] American Thoracic Society. 2004 [cited 2018 May 20], 31:510–6. https://doi.org/10.1165/rcmb.2004-0158OC.
Wang X, Wu G, Gou L, Liu Z, Wang X, Fan X, et al. A novel single-chain-Fv antibody against connective tissue growth factor attenuates bleomycin-induced pulmonary fibrosis in mice. Respirology [Internet] Wiley/Blackwell (10.1111). 2011 [cited 2018 May 20];16:500–7. https://doi.org/10.1111/j.1440-1843.2011.01938.x.
Allen JT, Knight RA, Bloor CA, Spiteri MA. Enhanced insulin-like growth factor binding protein–related protein 2 (connective tissue growth factor) expression in patients with idiopathic pulmonary fibrosis and pulmonary sarcoidosis. Am J Respir Cell Mol Biol [Internet] American Thoracic SocietyNew York, NY. 1999 [cited 2018 May 20];21:693–700. https://doi.org/10.1165/ajrcmb.21.6.3719.
Raghu G, Scholand MB, de Andrade J, Lancaster L, Mageto Y, Goldin J, et al. FG-3019 anti-connective tissue growth factor monoclonal antibody: results of an open-label clinical trial in idiopathic pulmonary fibrosis. Eur Respir J [Internet] European Respiratory Society. 2016 [cited 2018 May 20];47:1481–91 Available from: http://www.ncbi.nlm.nih.gov/pubmed/26965296.
Gorina E, Richeldi L, Raghu G, Fernandez Perez E, Costabel U, Albera C, Lederer D, Flaherty K, Ettinger N, Bercz P, Singh B, Perez R, Goldin J, Kouchakji E, Porter S. PRAISE, a randomized, placebo-controlled, double-blind Phase 2 clinical trial of pamrevlumab (FG-3019) in IPF patients. Diffus Parenchymal Lung Dis. [Internet] European Respiratory Society; 2017 [cited 2018 May 20]. p. OA3400 Available from: https://doi.org/10.1183/1393003.congress-2017.OA3400.
Gorina E, Goldin J, Hyun KG, Zhong M, Sekayan T, Yu P , Kouchakji E. Lung fibrosis measured by quantitative high resolution computed tomography (qHRCT) in idiopathic pulmonary fibrosis (IPF) patients treated with pamrevlumab (FG-3019). 2018; Available from: https://www.atsjournals.org/doi/abs/10.1164/ajrccm-conference.2018.197.1_MeetingAbstracts.A7688.
Parker J, Sawtell R, Gagnon L, Hagerimania A, Laurin P, Kolb M, et al. PBI-4050 is safe and well tolerated and shows evidence of benefit in idiopathic pulmonary fibrosis. Am J Crit Care Med. 2017;195:A7606.
Saini G, Porte J, Weinreb PH, Violette SM, Wallace WA, McKeever TM, et al. αvβ6 integrin may be a potential prognostic biomarker in interstitial lung disease. Eur Respir J [Internet] European Respiratory Society. 2015 [cited 2018 May 22];46:486–94 Available from: http://www.ncbi.nlm.nih.gov/pubmed/25745053.
Horan GS, Wood S, Ona V, Li DJ, Lukashev ME, Weinreb PH, et al. Partial inhibition of integrin αvβ6 prevents pulmonary fibrosis without exacerbating inflammation. Am J Respir Crit Care Med [Internet] American Thoracic Society. 2008 [cited 2018 May 22];177:56–65. https://doi.org/10.1164/rccm.200706-805OC.
Maden CH, Fairman D, Chalker M, Costa MJ, Fahy WA, Garman N, et al. Safety, tolerability and pharmacokinetics of GSK3008348, a novel integrin αvβ6 inhibitor, in healthy participants. Eur J Clin Pharmacol [Internet] Springer. 2018 [cited 2018 May 22];74:701–9 Available from: http://www.ncbi.nlm.nih.gov/pubmed/29532104.
Black KE, Berdyshev E, Bain G, Castelino F V, Shea BS, Probst CK, Fontaine BA, Bronova I, Goulet L, Lagares D, Ahluwalia N, Knipe RS, Natarajan V, Tager AM. Autotaxin activity increases locally following lung injury, but is not required for pulmonary lysophosphatidic acid production or fibrosis. FASEB J. [Internet] The Federation of American Societies for Experimental Biology; 2016 [cited 2018 May 22]; 30: 2435–2450 Available from: http://www.ncbi.nlm.nih.gov/pubmed/27006447.
Desroy N, Housseman C, Bock X, Joncour A, Bienvenu N, Cherel L, Labeguere V, Rondet E, Peixoto C, Grassot J-M, Picolet O, Annoot D, Triballeau N, Monjardet A, Wakselman E, Roncoroni V, Le Tallec S, Blanque R, Cottereaux C, Vandervoort N, Christophe T, Mollat P, Lamers M, Auberval M, Hrvacic B, Ralic J, Oste L, van der Aar E, Brys R, Heckmann B. Discovery of 2-[[2-Ethyl-6-[4-[2-(3-hydroxyazetidin-1-yl)-2-oxoethyl]piperazin-1-yl]-8-methylimidazo[1,2- a ]pyridin-3-yl]methylamino]-4-(4-fluorophenyl)thiazole-5-carbonitrile (GLPG1690), a first-in-class autotaxin inhibitor undergoing clinical evaluation for the treatment of idiopathic pulmonary fibrosis. J Med Chem. [Internet] 2017 [cited 2018 May 22]; 60: 3580–3590Available from: http://www.ncbi.nlm.nih.gov/pubmed/28414242.
Raghu G, Brown KK, Collard HR, Cottin V, Gibson KF, Kaner RJ, et al. Efficacy of simtuzumab versus placebo in patients with idiopathic pulmonary fibrosis: a randomised, double-blind, controlled, phase 2 trial. Lancet Respir Med. [Internet] 2017 [cited 2018 May 21]. 5:22–32 Available from: http://www.ncbi.nlm.nih.gov/pubmed/27939076.
Furuie H, Yamasaki H, Suga M, Ando M. Altered accessory cell function of alveolar macrophages: a possible mechanism for induction of Th2 secretory profile in idiopathic pulmonary fibrosis. Eur Respir J. 1997;10:787–94.
Jakubzick C, Choi ES, Kunkel SL, Evanoff H, Martinez FJ, Puri RK, et al. Augmented pulmonary IL-4 and IL-13 receptor subunit expression in idiopathic interstitial pneumonia. J Clin Pathol. 2004;57:477–86.
Parker JM, Glaspole IN, Lancaster LH, Haddad TJ, She D, Roseti SL, Fiening JP, Grant EP, Kell CM, Flaherty KR. A Phase 2 randomized controlled study of tralokinumab in subjects with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. [Internet] 2017; : 201704–201784 Available from: https://doi.org/10.1164/rccm.201704-0784OC%0A http://www.ncbi.nlm.nih.gov/pubmed/28787186.
Jones MG, Sgalla G, Richeldi L. Do randomized clinical trials always provide certain results? The case of tralokinumab in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med [Internet] 2018; 197: 9–10 Available from: https://doi.org/10.1164/rccm.201708-1666ED.
Swigris JJ, Ogura T, Scholand M, Glaspole I, Maher TM, Kardatzke D, Kaminski J. The RIFF Study ( Cohort A ): A phase II , randomized , double-blind , placebo-controlled Trial of lebrikizumab as monotherapy in patients with idiopathic pulmonary fibrosis. 2018; Available from:https://doi.org/10.1164/ajrccm conference.2018.197.1_MeetingAbstracts.A6167.
Maher TM, Kondoh Y, Corte TJ, Glassberg MK, Costabel U, Lancaster LH. The RIFF Study ( Cohort B ): A phase II , randomized , double-blind , placebo-controlled trial of lebrikizumab in combination with pirfenidone in patients with idiopathic pulmonary fibrosis. 2018; Available from: https://doi.org/10.1164/ajrccm conference.2018.197.1_MeetingAbstracts.A6168.
Raghu G, Richeldi L, Crestani B, Wung P, Bejuit R, Esperet C, Soubrane C. Safety and efficacy of SAR156597 in idiopathic pulmonary fibrosis ( IPF ): a phase 2 , randomized, double-blind , placebo-controlled study. 2018; Available from: https://doi.org/10.1164/ajrccm conference.2018.197.1_MeetingAbstracts.A2441.
Todd NW, Scheraga RG, Galvin JR, Iacono AT, James Britt E, Luzina IG, et al. Lymphocyte aggregates persist and accumulate in the lungs of patients with idiopathic pulmonary fibrosis. J Inflamm Res. 2013;6:63–70.
Lee JS, Kim EJ, Lynch KL, Elicker B, Ryerson CJ, Katsumoto TR, et al. Prevalence and clinical significance of circulating autoantibodies in idiopathic pulmonary fibrosis. Respir Med. 2013;107:249–55.
Shum AK, Alimohammadi M, Tan CL, Cheng MH, Metzger TC, Law CS, et al. BPIFB1 is a lung-specific autoantigen associated with interstitial lung disease. Sci Transl Med. 2013;5:206ra139.
Li FJ, Surolia R, Li H, Wang Z, Kulkarni T, Liu G, et al. Autoimmunity to vimentin is associated with outcomes of patients with idiopathic pulmonary fibrosis. J Immunol [Internet]. 2017;199:1596–605. https://doi.org/10.4049/jimmunol.1700473.
Kahloon RA, Xue J, Bhargava A, Csizmadia E, Otterbein L, Kass DJ, et al. Patients with idiopathic pulmonary fibrosis with antibodies to heat shock protein 70 have poor prognoses. Am J Respir Crit Care Med. 2013;187:768–75.
Keir GJ, Maher TM, Ming D, Abdullah R, De Lauretis A, Wickremasinghe M, et al. Rituximab in severe, treatment-refractory interstitial lung disease. Respirology. 2014;19:353–9.
Peters-Golden M, Henderson WR. Leukotrienes. N Engl J Med [Internet]. 2007;357:1841–54 Available from: http://www.ncbi.nlm.nih.gov/pubmed/17978293.
Yokomizo T, Izumi T, Shimizu T. Leukotriene B4: metabolism and signal transduction. Arch. Biochem. Biophys. 2001. p. 231–241.
Wardlaw AJ, Hay H, Cromwell O, Collins JV, Kay AB. Leukotrienes, LTC4 and LTB4, in bronchoalveolar lavage in bronchial asthma and other respiratory diseases. J Allergy Clin Immunol. 1989;84:19–26.
Wilborn J, Bailie M, Coffey M, Burdick M, Strieter R, Peters-Golden M. Constitutive activation of 5-lipoxygenase in the lungs of patients with idiopathic pulmonary fibrosis. J Clin Invest [Internet]. 1996;97:1827–36 Available from: http://www.ncbi.nlm.nih.gov/pubmed/8621765%5Cn http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC507250.
Izumo T, Kondo M, Nagai A. Cysteinyl-leukotriene 1 receptor antagonist attenuates bleomycin-induced pulmonary fibrosis in mice. Life Sci. 2007;80:1882–6.
Shimbori C, Shiota N, Okunishi H. Effects of montelukast, a cysteinyl-leukotriene type 1 receptor antagonist, on the pathogenesis of bleomycin-induced pulmonary fibrosis in mice. Eur J Pharmacol. 2011;650:424–30.
Wilkes DS, Chew T, Flaherty KR, Frye S, Gibson KF, Kaminski N, et al. Oral immunotherapy with type V collagen in idiopathic pulmonary fibrosis. Eur Respir J. 2015;45:1393–402.
Roskoski R. Src protein-tyrosine kinase structure, mechanism, and small molecule inhibitors. Pharmacol Res. 2015;94:9–25.
Yilmaz O, Oztay F, Kayalar O. Dasatinib attenuated bleomycin-induced pulmonary fibrosis in mice. Growth Factors. 2015;33:366–75.
Cruz FF, Horta LFB, De Albuquerque ML, Lopes-Pacheco M, Da Silva AB, Morales MM, et al. Dasatinib reduces lung inflammation and fibrosis in acute experimental silicosis. PLoS One. 2016;11:1–17.
Chambers DC, Enever D, Ilic N, Sparks L, Whitelaw K, Ayres J, Yerkovich ST, Khalil D, Atkinson KM, Hopkins PMA. A phase 1b study of placenta-derived mesenchymal stromal cells in patients with idiopathic pulmonary fibrosis. Respirology 2014; .
Tzouvelekis A, Paspaliaris V, Koliakos G, Ntolios P, Bouros E, Oikonomou A, et al. Prospective , non-randomized , no placebo-controlled , phase Ib clinical trial to study the safety of the adipose derived stromal cells-stromal vascular fraction in idiopathic pulmonary fibrosis. J Transl Med. 2013;11:1.
Glassberg MK, Minkiewicz J, Toonkel RL, Simonet ES, Rubio GA, Difede D, Shafazand S, Khan A, Pujol M V., LaRussa VF, Lancaster LH, Rosen GD, Fishman J, Mageto YN, Mendizabal A, Hare JM. Allogeneic human mesenchymal stem cells in patients with idiopathic pulmonary fibrosis via intravenous delivery (AETHER): a phase I, safety, clinical trial. Chest 2016; .
Molyneaux PL, Maher TM. The role of infection in the pathogenesis of idiopathic pulmonary fibrosis. Eur Respir Rev. 2013;22:376–81.
Egan JJ, Adamali HI, Lok SS, Stewart JP, Woodcock AA. Ganciclovir antiviral therapy in advanced idiopathic pulmonary fibrosis: an open pilot study. Pulm Med. 2011;2011:240805.
Molyneaux PL, Cox MJ, Willis-Owen SAG, Mallia P, Russell KE, Russell AM, et al. The role of bacteria in the pathogenesis and progression of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2014;190:906–13.
Shulgina L, Cahn AP, Chilvers ER, Parfrey H, Clark AB, Wilson ECF, et al. Treating idiopathic pulmonary fibrosis with the addition of co-trimoxazole: a randomised controlled trial. Thorax. 2013;68:884–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Giuliana Pasciuto, Riccardo Inchingolo, Carola Condoluci, Daniele Magnini, Bruno Iovene, and Luca Richeldi declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Interstitial Lung Disease
Rights and permissions
About this article
Cite this article
Pasciuto, G., Inchingolo, R., Condoluci, C. et al. Approved and Experimental Therapies for Idiopathic Pulmonary Fibrosis. Curr Pulmonol Rep 7, 107–117 (2018). https://doi.org/10.1007/s13665-018-0209-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13665-018-0209-0