Abstract
Purpose
We sought to understand the beliefs and practices of Canadian intensivists regarding their use of ketamine as a sedative in critically ill patients and to gauge their interest in a randomized controlled trial (RCT) examining its use in the intensive care unit (ICU).
Methods
We designed and validated an electronic self-administered survey examining the use of ketamine as a sedative infusion for ICU patients. We surveyed 400 physician members of the Canadian Critical Care Society (CCCS) via email between February and April 2022 and sent three reminders at two-week intervals. The survey was redistributed in January 2023 to improve the response rate.
Results
We received 87/400 (22%) completed questionnaires. Most respondents reported they rarely use ketamine as a continuous infusion for sedation or analgesia in the ICU (52/87, 58%). Physicians reported the following conditions would make them more likely to use ketamine: asthma exacerbation (73/87, 82%), tolerance to opioids (68/87, 77%), status epilepticus (44/87, 50%), and severe acute respiratory distress syndrome (33/87, 38%). Concern for side-effects that limited respondents’ use of ketamine include adverse psychotropic effects (61/87, 69%) and delirium (47/87, 53%). The majority of respondents agreed there is need for an RCT to evaluate ketamine as a sedative infusion in the ICU (62/87, 71%).
Conclusion
This survey of Canadian intensivists illustrates that use of ketamine as a continuous infusion for sedation is limited, and is at least partly driven by concerns of adverse psychotropic effects. Canadian physicians endorse the need for a trial investigating the safety and efficacy of ketamine as a sedative for critically ill patients.
Résumé
Objectif
Nous avons cherché à comprendre les croyances et les pratiques des intensivistes pratiquant au Canada concernant leur utilisation de la kétamine comme sédatif chez la patientèle gravement malade et à évaluer leur intérêt pour une étude randomisée contrôlée (ERC) examinant son utilisation à l’unité de soins intensifs (USI).
Méthode
Nous avons mis au point et validé un sondage électronique auto-administré examinant l’utilisation de la kétamine comme perfusion sédative pour les patient·es aux soins intensifs. Nous avons envoyé le sondage à 400 médecins membres de la Société canadienne de soins intensifs (SCCC) par courriel entre février et avril 2022 et envoyé trois rappels à intervalles de deux semaines. Le sondage a été redistribué en janvier 2023 afin d’améliorer le taux de réponse.
Résultats
Nous avons reçu 87 questionnaires remplis sur 400 (22 %). La plupart des personnes répondantes ont déclaré qu’elles utilisaient rarement la kétamine en perfusion continue pour la sédation ou l’analgésie à l’USI (52/87, 58 %). Les médecins ont déclaré que les conditions suivantes les rendraient plus susceptibles d’utiliser de la kétamine : une exacerbation de l’asthme (73/87, 82 %), une tolérance aux opioïdes (68/87, 77 %), un état de mal épileptique (44/87, 50 %) et un syndrome de détresse respiratoire aigu (33/87, 38 %). Les inquiétudes quant aux effets secondaires qui ont limité l’utilisation de la kétamine par les répondant·es comprennent les effets psychotropes indésirables (61/87, 69 %) et le delirium (47/87, 53 %). La majorité des personnes répondantes étaient d’accord qu’une ERC est nécessaire pour évaluer la kétamine en tant que perfusion sédative à l’USI (62/87, 71 %).
Conclusion
Cette enquête menée auprès d’intensivistes au Canada montre que l’utilisation de la kétamine comme perfusion continue pour la sédation est limitée, au moins en partie en raison d’inquiétudes liées aux effets psychotropes indésirables. Les médecins pratiquant au Canada reconnaissent la nécessité d’une étude sur l’innocuité et l’efficacité de la kétamine comme sédatif pour la patientèle gravement malade.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Sedation is administered to critically ill patients in the intensive care unit (ICU) to treat discomfort, anxiety, and agitation, and to help facilitate care (e.g., optimize mechanical ventilation). The recognition and management of pain, oversedation, and delirium are crucial as they are associated with increased morbidity and mortality in ICU patients.1 Pain, in particular, is essential to identify and manage as it is prevalent in the majority of ICU patients at various points during their clinical course.2 Consequences of untreated pain include delirium, agitation with higher energy expenditure, posttraumatic stress disorder, anxiety, and depression.1 Furthermore, pain is the most common memory patients have of their ICU stay.2
The most commonly used drugs for sedation in the ICU include propofol, midazolam, and dexmedetomidine; however, most of these drugs lack analgesic effects.3 Ketamine is a general anesthetic with sedative and analgesic properties and is frequently used for procedural sedation by anesthesiologists and emergency physicians, but has not been well studied in the ICU. In addition to its analgo-sedative properties, ketamine has favourable physiologic properties as it preserves cardiac output, maintains airway reflexes, and causes bronchodilation; this makes it an attractive substitute to opioids.4 Alternatives to opioid-based analgesia have become increasingly relevant as the COVID-19 pandemic resulted in significant drug shortages worldwide.5 Furthermore, opioid use has been associated with delirium in a dose-dependent fashion.6 Prolonged use of opioids may precipitate tolerance, dependence, hyperalgesia, and iatrogenic opioid withdrawal.7 In a study of opioid-naïve patients, 20% of invasively mechanically ventilated patients received a prescription for opioids after hospital discharge and 2.6% met criteria for persistent use.8 This is particularly problematic with an aging population being hospitalized more frequently,9 and being at a higher risk of developing opioid-related side-effects.10 Adjunctive ketamine may decrease opioid use in the ICU.5
At present, it is unclear how often ketamine is used in Canadian ICUs, and the perspectives of Canadian intensivists regarding the role of ketamine for critically ill patients are not known. It is important to explore ketamine use in Canadian ICUs to better understand barriers and facilitators to expanded clinical use, and acceptability of clinical trials.
The objective of this survey was to understand the beliefs and practices of Canadian intensivists regarding their use of sedatives in the ICU and to gauge their support for a randomized controlled trial (RCT) examining the use of ketamine in this setting. The results of this survey will inform a research program examining the role of ketamine in mechanically ventilated ICU patients.
Methods
Ethics
The Hamilton Integrated Research Ethics Board approved the study (Hamilton, ON, Canada; project number 13586). We deidentified survey responses using LimeSurvey (LimeSurvey GmbH, Hamburg, Germany).11
Instrument development
We designed a survey instrument adhering to formal development and testing methods.12 We generated an exhaustive list of items based on an informal literature review and email correspondence among coinvestigators representing Canadian intensivists and pharmacists. We performed item reduction to ensure parsimonious, functional, and internally consistent items were included.13 This was conducted by assessing for duplication and prioritizing questions based on relevance with coinvestigators. The self-administered instrument (Electronic Supplemental Material eAppendix) consisted of 15 items that focused on four domains: respondent and ICU characteristics, current personal sedation practices, views about the risk of current sedatives used in the ICU, and interest in participating in a future trial. Responses were yes/no, “select all that apply,” Likert scales, and optional free-text entry.
Instrument testing
We conducted a sensibility assessment and pilot testing of the survey. We invited seven colleagues (five intensivists and two pharmacists, including four methodologists) with clinical and methodologic expertise to evaluate the comprehensiveness, clarity, and text of the instrument. This feedback helped refine the questions and assess content validity. Furthermore, six members of the Canadian Critical Care Trials Group (CCCTG) pilot tested the instrument to ensure functionality and ease of completion.
Instrument administration
Following approval from the Canadian Critical Care Society (CCCS), we sent the survey to all critical care physician members of the CCCS (n = 400). On February 2022, we sent an e-mail with a link to the web-based survey on LimeSurvey, which included instructions for completing the survey. We raffled three gift cards as incentives for survey completion. We distributed three standardized reminders every two weeks. The link to the survey was closed two weeks after the final reminder email in April 2022 (a total response window of ten weeks). We distributed the survey once more for a two-week period on 10 January 2023 because the response rate to the initial distribution was low.
Statistical analysis
We used descriptive statistics for reporting. Data are presented as mean (standard deviation [SD]). Absolute counts and proportions are presented as appropriate. The American Association for Public Opinion Research defined a completed questionnaire as at least 80% of complete responses;14 however, for the purposes of this survey manuscript, a “complete questionnaire,” is one with 100% complete responses. At the request of reviewers, we analyzed the frequency of the use of ketamine as an infusion by medical specialty.
Results
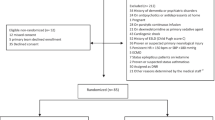
Of the 400 potential respondents, we received 101 responses from 63 centres across Canada. Of those, 14 partially completed the survey and these partially completed surveys were excluded from the analysis, leaving 87 (22% completed questionnaires) in the final analysis. Upon initial distribution of the survey, we had a completed questionnaire rate of 16%. The answers to the survey questions in 2023 were remarkably similar compared with those of the initial distribution in 2022, suggesting there was no big temporal impact on ketamine use or views and preferences related to ketamine during this short interval between distributions. Close to half of the respondents were in practice for more than ten years (47%) (Table 1). The highest proportion of respondents had a background in internal medicine (43/87, 49%), followed by anesthesia (16/87, 18%), emergency medicine (9//87, 10%), and general surgery (6/87, 7%) (Table 1). Three-quarters of the survey respondents work at an academic centre (63/87, 72%), and a smaller proportion work at an academic community centre (17/87, 20%) or a nonacademic community centre (7/87, 8%).
Survey respondents reported propofol as the most common first-line sedative infusion agent in the ICU (82/87, 91%), followed by midazolam (5/87, 6%), dexmedetomidine (2/87, 2%), and ketamine (1/87, 1%) (Fig. 1). With respect to the second sedative infusion agent of choice if the first was not available, survey respondents reported using midazolam (52/87, 58%), followed by dexmedetomidine (18/87, 20%), opioids only (5/87, 6%), propofol (8/87, 9%), and ketamine (6/87, 7%) (Fig. 1). When asked about adjunctive sedative medications when the first-choice infusion was not adequate to attain the goal sedation depth, respondents reported using midazolam (32/87, 36%), ketamine (22/87, 24%), dexmedetomidine (21/87, 23%), and opioids (9/87, 10%). Importantly, the aforementioned questions focused only on sedative agents and outlined that appropriate analgesia had already been achieved.
In terms of patient populations, most survey respondents reported that they rarely use ketamine as a continuous infusion for sedation/analgesia in the ICU for general medical mechanically ventilated patients (52/87, 58%) (Fig. 2) while a smaller proportion said they sometimes use ketamine in this circumstance (26/87, 29%). When comparing ketamine use among different medical specialties, we did not find any meaningful differences between the specialties of anesthesia, emergency medicine, general surgery, or internal medicine (Fig. 3). Survey respondents reported that the following clinical circumstances would make them more likely to use ketamine as an adjunctive infusion: 1) pain refractory to opioids (78/87, 87%), 2) asthma exacerbation (73/87, 82%), 3) known tolerance to opioids (68/87, 77%), 4) to minimize the side-effects of other sedatives (54/87, 61%), 5) status epilepticus (44/87, 50%), 6) deep sedation for acute respiratory distress syndrome (33/87, 38%), and 7) noninvasive positive-pressure ventilation (22/87, 25%) (Fig. 4).
With respect to side effects that would limit their wider use of ketamine, respondents reported the following: 1) possible psychotropic effects (61/87, 69%), 2) delirium (47/87, 53%); 3) tachycardia (20/87, 23%); 4) increased secretions (15/87, 17%); 5) arrhythmias (13/87, 15%), and 6) hypertension (10/87, 11%) (Table 2).
Most survey respondents reported it was more important to study the use of ketamine as an adjunctive sedative infusion (64/87, 74%) rather than a primary sedative infusion (12/87, 14%). Overall, 71% of respondents responded that they would be willing to enrol their patients in a RCT to examine the efficacy and safety of ketamine as an adjunctive sedative in the ICU.
Discussion
In this national survey, 1% of Canadian intensivists reported using ketamine as a primary sedative infusion, and 24% as an adjunctive sedative infusion when the first-choice sedative was insufficient to maintain the goal depth of sedation. Importantly, 71% of respondents expressed their interest in participating in a trial examining the efficacy and safety of ketamine as a sedative in the ICU.
Ketamine has been the most commonly used agent for painful emergency department (ED) procedures in children for over 20 years.15 Studies done in adult EDs have also shown the safety and efficacy of ketamine for dissociative transient sedation to facilitate care for procedures such as cardioversion, and reduction of fractures.16,17,18,19 A 2018 survey of 10,737 paramedics in the USA found that two-thirds of them had administered ketamine for acute sedation or pain and 94% were comfortable with its use.20 This comfort with ketamine use among emergency providers is also reflected in Canadian prehospital practice, as well as in medical directives for its use by paramedics, which exist in several provinces.21 Despite this, our survey findings indicate that ketamine use as an infusion in the ICU is fairly consistent among different medical specialties.
This survey showed clear interest among respondents in participating in a RCT to further investigate the role of ketamine in critically ill patients. This may, in part, be due to the potential benefits of ketamine in other settings. In the ED, procedural sedation with ketamine has rare associated adverse events while preserving pharyngeal reflexes and stimulating cardiovascular tone thereby avoiding hemodynamic sequalae.19 Furthermore, for perioperative analgesia, ketamine has been found to significantly reduce opioid consumption.22 In mechanically ventilated patients, use of adjunctive ketamine infusions has been associated with decreased vasopressor requirements compared with propofol and fentanyl.23 In addition to a more optimal side effect profile, another reason for the interest in ketamine in the ICU may be the increased comfort of physicians given it has been used more often since the COVID-19 pandemic because of drug shortages and standardization of intubation protocols.24,25 With reports of drug shortages worldwide due to manufacturing issues and supply being outstripped by demand, it is incredibly important to establish the efficacy and safety of multiple sedative options, including, but not limited to, ketamine.26
Despite its potential benefits, more than half of our survey respondents were concerned about possible psychotropic effects and delirium as a side effect of ketamine. Given that the duration of ICU delirium may be associated with mortality up to one year after ICU admission,27 it is important to determine the safety profile of ketamine as it is being used with increasing frequency in ICUs since the COVID-19 pandemic.28,29 From a physiologic perspective, ketamine is a rapid-acting antidepressant drug.30 Nevertheless, ketamine is also a psychoactive drug with known hallucinogenic properties31 that could theoretically contribute to agitation and delirium, especially in vulnerable patients (i.e., alcohol use disorder, substance use disorders).32 At present, the evidence evaluating the association of delirium with ketamine is conflicting and inconclusive.
Ketamine is associated with adverse emergence phenomena, including recovery agitation and delirium, in 10–20% of patients in the ED undergoing procedural sedation.19 In the perioperative setting, physicians sometimes use benzodiazepines to attenuate the emergence phenomenon associated with ketamine.33 Whether ketamine infusions in the ICU would result in patients requiring benzodiazepines to curb emergence phenomena is unclear. In a multicentre retrospective study, ketamine use in the ICU was not associated with an increased risk for delirium.34 Furthermore, in an RCT of 162 patients, an adjunctive ketamine infusion (0.20 mg−1·kg−1·hr−1) was associated with a decreased duration of delirium compared with placebo.35 Whether related to side effects or other considerations, the findings of this survey are consistent with other data reporting that intensivists express a lack of comfort with ketamine use and rarely use it.25 All sedatives used in the ICU have been associated with potential adverse effects. Propofol can cause bradycardia, hypotension, propofol infusion syndrome, hypertriglyceridemia, and pancreatitis;1 midazolam is associated with a higher risk of delirium and prolonged sedation;1 and dexmedetomidine can cause hypotension, bradycardia, and nausea.1 Although ketamine also has side-effects, the reported data associates it with fewer complications.19
This reported discomfort with ketamine use in the ICU setting is relatively pervasive. Guidelines for managing mechanically ventilated patients continually acknowledge the lack of high-quality evidence on which to base recommendations for use of this drug to facilitate sedation and analgesia.36,37 In fact, there are no specific recommendations for ketamine use as an infusion in the ICU apart from a conditional recommendation for its use in postsurgical patients to help reduce opioid consumption.37 Commonly employed justification for this lack of guidance includes the heterogeneity of the eligibility criteria of published studies and the fact that published studies have not focused on patient important outcomes.
Strengths of this study include the novel question, rigorous survey development with interprofessional input, and the diverse medical specialty background and broad geographic representation of respondents. To our knowledge, this is the first survey evaluating ketamine practice and beliefs among Canadian intensivists. Furthermore, we employed a comprehensive approach to the development of this survey using rigorous methods, exhaustive item generation, item reduction, and piloting. The limitations of this study include the low response rate, limited number of pediatric practitioners, and possible response bias, including the overrepresentation of academic intensivists. Of note, although 72% of respondents practiced in an academic ICU, this is only slightly higher than a 2019 Canadian Medical Association poll, which reported that 59% of all intensivists in Canada work at an academic teaching hospital.38 Another limitation of this study was the redistribution of the survey to garner more responses eight months after the initial invitation. Of note, the responses acquired after the initial survey distribution were similar to the original responses indicating that practice and perceptions around sedatives did not change over that eight-month span. Reasons for the low survey response rate are likely multifactorial and likely, in part, due to increased burnout among intensivists (64% in a survey).39 Furthermore, there is emerging evidence on survey fatigue during the COVID-19 pandemic with postpandemic survey response rates significantly reduced compared with prepandemic levels.40 In the future, we could perhaps increase our survey response rate by using means other than email to disseminate the survey.
Conclusion
This survey of Canadian intensivists illustrates that current use of ketamine as a continuous infusion is limited and is likely driven by concerns of adverse psychotropic effects or delirium. Canadian physicians agree with the need for a trial investigating the safety and efficacy of ketamine as a sedative in the ICU.
References
Reade MC, Finfer S. Sedation and delirium in the intensive care unit. N Engl J Med 2014; 370: 444–54. https://doi.org/10.1056/nejmra1208705
Stein-Parbury J, McKinley S. Patients' experiences of being in an intensive care unit: a select literature review. Am J Crit Care 2000; 9: 20–7.
Hughes CG, McGrane S, Pandharipande PP. Sedation in the intensive care setting. Clin Pharmacol 2012; 4: 53–63. https://doi.org/10.2147/cpaa.s26582
Ragule CA, Wade KL, Rubino S. Update on the physiologic effects of ketamine in general anesthesia and spinal blockade: a review of the literature. AANA J 2019; 87: 489–94.
Siow WT, Tang SH, Agrawal RV, Tan AY, See KC. Essential ICU drug shortages for COVID-19: what can frontline clinicians do? Crit Care 2020; 24: 260. https://doi.org/10.1186/s13054-020-02971-x
Duprey MS, Dijkstra-Kersten SM, Zaal IJ, et al. Opioid use increases the risk of delirium in critically ill adults independently of pain. Am J Respir Crit Care Med 2021; 204: 566–72. https://doi.org/10.1164/rccm.202010-3794oc
Murray BP, Newsome AS. Opioids for sedation: has the pendulum swung too far? Am J Respir Crit Care Med 2021; 204: 611. https://doi.org/10.1164/rccm.202104-1012le
Wunsch H, Hill AD, Fu L, et al. New opioid use after invasive mechanical ventilation and hospital discharge. Am J Respir Crit Care Med 2020; 202: 568–75. https://doi.org/10.1164/rccm.201912-2503oc
Haas LE, Karakus A, Holman R, Cihangir S, Reidinga AC, de Keizer NF. Trends in hospital and intensive care admissions in the Netherlands attributable to the very elderly in an ageing population. Crit Care 2015; 19: 353. https://doi.org/10.1186/s13054-015-1061-z
Kim JY, Kim JH, Yee J, Song SJ, Gwak HS. Risk factors of opioid-induced adverse reactions in elderly male outpatients of Korea Veterans Hospital. BMC Geriatr 2018; 18: 293. https://doi.org/10.1186/s12877-018-0990-1
LimeSurvey GmbH. Welcome to LimeSurvey. The LifeSurvey. Available from URL: https://www.limesurvey.org (accessed June 2023).
Burns KE, Duffett M, Kho ME, et al. A guide for the design and conduct of self-administered surveys of clinicians. CMAJ 2008; 179: 245–52. https://doi.org/10.1503/cmaj.080372
Boateng GO, Neilands TB, Frongillo EA, Melgar-Quiñonez HR, Young SL. Best practices for developing and validating scales for health, social, and behavioral research: a primer. Front Public Health 2018; 6: 149. https://doi.org/10.3389/fpubh.2018.00149
American Association of Public Opinion Research. Standard definitions: final dispositions of case codes and outcome rates for surveys. 2016. Available from URL: https://aapor.org/wp-content/uploads/2022/11/Standard-Definitions20169theditionfinal.pdf (accessed July 2023).
Green SM, Roback MG, Krauss B, et al. Predictors of airway and respiratory adverse events with ketamine sedation in the emergency department: an individual-patient data meta-analysis of 8,282 children. Ann Emerg Med 2009; 54: 158–68. https://doi.org/10.1016/j.annemergmed.2008.12.011
Newton A, Fitton L. Intravenous ketamine for adult procedural sedation in the emergency department: a prospective cohort study. Emerg Med J 2008; 25: 498–501. https://doi.org/10.1136/emj.2007.053421
Vardy JM, Dignon N, Mukherjee N, Sami DM, Balachandran G, Taylor S. Audit of the safety and effectiveness of ketamine for procedural sedation in the emergency department. Emerg Med J 2008; 25: 579–82. https://doi.org/10.1136/emj.2007.056200
Sener S, Eken C, Schultz CH, Serinken M, Ozsarac M. Ketamine with and without midazolam for emergency department sedation in adults: a randomized controlled trial. Ann Emerg Med 2011; 57: 109–14. https://doi.org/10.1016/j.annemergmed.2010.09.010
Strayer RJ, Nelson LS. Adverse events associated with ketamine for procedural sedation in adults. Am J Emerg Med 2008; 26: 985–1028. https://doi.org/10.1016/j.ajem.2007.12.005
Buckland DM, Crowe RP, Cash RE, et al. Ketamine in the prehospital environment: a national survey of paramedics in the United States. Prehosp Disaster Med 2018; 33: 23–8. https://doi.org/10.1017/s1049023x17007142
Yuhalogarasan A, Barclay C, Verbeek PR. Low-dose ketamine in the prehospital setting. CMAJ 2022; 194: E171. https://doi.org/10.1503/cmaj.80599
Kurdi MS, Theerth KA, Deva RS. Ketamine: current applications in anesthesia, pain, and critical care. Anesth Essays Res 2014; 8: 283–90. https://doi.org/10.4103/0259-1162.143110
Hui C, Monteiro JP, Trivedi D, Vasant D, Carino G. Effect of ketamine on vasopressor needs in mechanically ventilated patients: a retrospective study. Brown K Hosp Med 2022; 1: 1–9. https://doi.org/10.56305/001c.36988
Shrestha GS, Shrestha N, Lamsal R, et al. Emergency intubation in Covid-19. N Engl J Med 2021; 384: e20. https://doi.org/10.1056/nejmvcm2007198
Ilg A BC, Shih J, Yankama T, Hayes Mm, Moskowitz A. Ketamine in critical care: exploring before and during COVID-19 attitudes and practices. Am J Respir Crit Care Med 2022; 205: A3556. Available from URL: https://www.atsjournals.org/https://doi.org/10.1164/ajrccm-conference.2022.205.1_MeetingAbstracts.A3556 (accessed June 2023).
Patel R, Samiee-Zafarghandy S, Ziesenitz V, et al. US drug shortages compared to the World Health Organization's model list of essential medicines for children: a cross-sectional study. Am J Health Syst Pharm 2022; 79: 2012–7. https://doi.org/10.1093/ajhp/zxac210
Pisani MA, Kong SY, Kasl SV, Murphy TE, Araujo KL, Van Ness PH. Days of delirium are associated with 1-year mortality in an older intensive care unit population. Am J Respir Crit Care Med 2009; 180: 1092–7. https://doi.org/10.1164/rccm.200904-0537oc
Luz M, Barreto BB, de Castro RE, et al. Practices in sedation, analgesia, mobilization, delirium, and sleep deprivation in adult intensive care units (SAMDS-ICU): an international survey before and during the COVID-19 pandemic. Ann Intensive Care 2022; 12: 9. https://doi.org/10.1186/s13613-022-00985-y
Gershengorn HB, Wunsch H. Temporal trends and variability in ketamine use for mechanically ventilated adults in the United States. Ann Am Thorac Soc 2022; 19: 1534–42. https://doi.org/10.1513/annalsats.202112-1376oc
Kishimoto T, Chawla JM, Hagi K, et al. Single-dose infusion ketamine and non-ketamine N-methyl-d-aspartate receptor antagonists for unipolar and bipolar depression: a meta-analysis of efficacy, safety and time trajectories. Psychol Med 2016; 46: 1459–72. https://doi.org/10.1017/s0033291716000064
Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists' Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain 2016; 17: 131–57. https://doi.org/10.1016/j.jpain.2015.12.008
Kraus C, Rabl U, Vanicek T, et al. Administration of ketamine for unipolar and bipolar depression. Int J Psychiatry Clin Pract 2017; 21: 2–12. https://doi.org/10.1080/13651501.2016.1254802
Perumal DK, Adhimoolam M, Selvaraj N, Lazarus SP, Mohammed MA. Midazolam premedication for Ketamine-induced emergence phenomenon: a prospective observational study. J Res Pharm Pract 2015; 4: 89–93. https://doi.org/10.4103/2279-042x.155758
Groth CM, Droege CA, Connor KA, et al. Multicenter retrospective review of ketamine use in the ICU. Crit Care Explor 2022; 4: e0633. https://doi.org/10.1097/cce.0000000000000633
Perbet S, Verdonk F, Godet T, et al. Low doses of ketamine reduce delirium but not opiate consumption in mechanically ventilated and sedated ICU patients: a randomised double-blind control trial. Anaesth Crit Care Pain Med 2018; 37: 589–95. https://doi.org/10.1016/j.accpm.2018.09.006
Baron R, Binder A, Biniek R, et al. Evidence and consensus based guideline for the management of delirium, analgesia, and sedation in intensive care medicine. Revision 2015 (DAS-Guideline 2015)—short version. Ger Med Sci 2015; 13: Doc19. https://doi.org/10.3205/000223
Devlin JW, Skrobik Y, Gélinas C, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med 2018; 46: e825–73. https://doi.org/10.1097/ccm.0000000000003299
Canadian Medical Association. Critical care medicine profile. 2019. Available from URL: https://www.cma.ca/sites/default/files/2020-10/critical-care-e.pdf (accessed July 2023).
Burns KEA, Moss M, Lorens E, et al. Wellness and coping of physicians who worked in ICUs during the pandemic: a multicenter cross-sectional North American survey. Crit Care Med 2022; 50: 1689–700.
de Koning R, Egiz A, Kotecha J, et al. Survey fatigue Dduring the COVID-19 pandemic: an analysis of neurosurgery survey response rates. Front Surg 2021; 8: 690680. https://doi.org/10.3389/fsurg.2021.690680
Author contributions
Bram Rochwerg and Sameer Sharif designed the study, analyzed the results, and drafted the initial manuscript. Laveena Munshi, Lisa Burry, Sara Gray, Dipayan Chaudhuri, Sangeeta Mehta, Mark Duffett, and Reed A. Siemieniuk all equally contributed in editing the contents of the manuscript.
Acknowledgement
We would like to thank the CCCS members for their help with disseminating the survey. We would also like to thank all the CCCS members who responded to the survey.
Disclosures
None.
Funding statement
Dr. Sameer Sharif holds a McMaster University Department of Medicine Internal Career Research Award.
Editorial responsibility
This submission was handled by Dr. Alexis F. Turgeon, Associate Editor, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sharif, S., Munshi, L., Burry, L. et al. Ketamine sedation in the intensive care unit: a survey of Canadian intensivists. Can J Anesth/J Can Anesth 71, 118–126 (2024). https://doi.org/10.1007/s12630-023-02608-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-023-02608-x