Abstract
Purpose
The COVID-19 pandemic has caused intensive care units (ICUs) to reach capacities requiring triage. A tool to predict mortality risk in ventilated patients with COVID-19 could inform decision-making and resource allocation, and allow population-level comparisons across institutions.
Methods
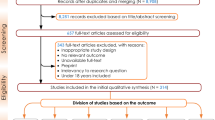
This retrospective cohort study included all mechanically ventilated adults with COVID-19 admitted to three tertiary care ICUs in Toronto, Ontario, between 1 March 2020 and 15 December 2020. Generalized estimating equations were used to identify variables predictive of mortality. The primary outcome was the probability of death at three-day intervals from the time of ICU admission (day 0), with risk re-calculation every three days to day 15; the final risk calculation estimated the probability of death at day 15 and beyond. A numerical algorithm was developed from the final model coefficients.
Results
One hundred twenty-seven patients were eligible for inclusion. Median ICU length of stay was 26.9 (interquartile range, 15.4–52.0) days. Overall mortality was 42%. From day 0 to 15, the variables age, temperature, lactate level, ventilation tidal volume, and vasopressor use significantly predicted mortality. Our final clinical risk score had an area under the receiver-operating characteristics curve of 0.9 (95% confidence interval [CI], 0.8 to 0.9). For every ten-point increase in risk score, the relative increase in the odds of death was approximately 4, with an odds ratio of 4.1 (95% CI, 2.9 to 5.9).
Conclusion
Our dynamic prediction tool for mortality in ventilated patients with COVID-19 has excellent diagnostic properties. Notwithstanding, external validation is required before widespread implementation.
Résumé
Objectif
En raison de la pandémie de COVID-19, les unités de soins intensifs (USI) ont atteint des taux d’occupation nécessitant un triage. Un outil pour prédire le risque de mortalité chez les patients sous ventilation atteints de COVID-19 pourrait éclairer la prise de décision et l’attribution des ressources tout en permettant des comparaisons populationnelles entre les établissements.
Méthode
Cette étude de cohorte rétrospective a inclus tous les adultes atteints de COVID-19 sous ventilation mécanique admis dans trois USI de centres de soins tertiaires à Toronto, en Ontario, entre le 1er mars 2020 et le 15 décembre 2020. Des équations d’estimation généralisées ont été utilisées pour identifier les variables prédictives de mortalité. Le critère d’évaluation principal était la probabilité de décès à des intervalles de trois jours à partir du moment de l’admission à l’USI (jour 0), avec un nouveau calcul du risque tous les trois jours jusqu’au jour 15; le calcul final du risque a estimé la probabilité de décès au jour 15 et au-delà. Un algorithme numérique a été mis au point à partir des coefficients du modèle final.
Résultats
Cent vingt-sept patients étaient éligibles à l’inclusion. La durée médiane de séjour à l’USI était de 26,9 jours (écart interquartile, 15,4 à 52,0). La mortalité globale était de 42 %. Du jour 0 au jour 15, les variables que sont l’âge, la température, les taux de lactate, le volume courant de ventilation et l’utilisation de vasopresseurs ont constitué des prédicteurs significatifs de mortalité. Notre score de risque clinique final avait une aire sous la courbe ROC de 0,9 (intervalle de confiance [IC] à 95 %, 0,8 à 0,9). Pour chaque augmentation de dix points du score de risque, l’augmentation relative des risques de décès était d’environ 4, avec un rapport de cotes de 4,1 (IC 95 %, 2,9 à 5,9).
Conclusion
Notre outil de prédiction dynamique de la mortalité pour les patients ventilés atteints de COVID-19 possède d’excellentes propriétés diagnostiques. Néanmoins, une validation externe est nécessaire avant sa mise en œuvre généralisée.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
COVID-19 caused by SARS-CoV2, continues to cause significant worldwide morbidity and mortality. Since the beginning of the pandemic, over 133 million cases have been documented worldwide, with more than 1 million cases in Canada.1 In Canada alone, over 23,000 individuals have died of COVID-19.2 Data from the province of Ontario indicate that 13% of identified cases have been hospitalized and 3% have been admitted to the intensive care unit (ICU),3 although identified cases likely represent a small fraction of total infections. At the time of writing 1,397 patients with COVID-19 have been hospitalized in Ontario, of which 504 (35%) were admitted to an ICU and 320 (23%) received ventilation.4 Historically, Ontario’s ICU capacity has been limited to 1,122 beds capable of accommodating patients requiring mechanical ventilation.5 Currently, emerging variants of concern are placing increasing strains on health resources,1,3 underscoring the need for evidence-informed tools to guide decision-making. Such tools can be used to understand differences in population risk and help with local resource planning, guide data-driven discussions with patients and families regarding prognosis, allow comparisons of patient illness severity and outcomes across different critical care units, and also be used to compare baseline risk between treatment groups in clinical studies.
Existing COVID-19 risk prediction algorithms, including novel deep learning models, have proven useful for forecasting progression to critical illness at the time of hospital admission or during earlier phases of illness.6,7,8,9,10 Nevertheless, models predicting mortality have largely focused on all hospitalized patients rather than the subset of patients who are critically ill.10,11,12,13,14,15,16,17 While prognostic scoring systems such as the Sequential Organ Failure Assessment (SOFA) score have been widely applied in ICU patients, recent work has suggested lower than anticipated accuracy for the prediction of mortality in COVID-19 patients requiring ventilation.18 Additionally, the utility of this score in patients transferred from other ICUs is unclear. Importantly, to our knowledge there are no tools that allow for estimation of mortality in ventilated patients with COVID-19 dynamically (i.e., using clinical data from after the time of admission), which is essential to account for changes in a patient’s clinical condition. The objective of this study was to create a dynamic risk prediction model for mortality in ventilated COVID-19 patients, applied every three days over the initial 15 days of ICU admission. The advantage of this approach would be the ability to continually reassess risk as new patient information is obtained during the course of treatment.
Methods
Data sources and collection
This study was approved by the University Health Network and Sinai Health System research ethics boards (20-5378.1 and 20-0115-C) and follows the Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD) guidelines.19 Written informed consent was waived given the retrospective design and the use of de-identified data. The records of patients admitted to intensive care units (ICUs) at Sinai Health System, Toronto Western Hospital and Toronto General Hospital were reviewed from 1 March 2020 to 15 December 2020. Adult patients (≥ 18 yr) with polymerase chain reaction-confirmed SARS-CoV2 infection (Seegene Allplex™ 2019 n-CoV assay; Seegene Inc., Seoul, South Korea) receiving invasive mechanical ventilation at any point during their ICU stay were eligible for inclusion. Patients prescribed high-flow nasal cannula or non-invasive ventilation (e.g., continuous positive airway pressure or bilevel positive airway pressure) were not eligible. A team of experienced clinical data abstractors assessed electronic and paper charts. Data were collected and stored on a centralized electronic database.
Selection of potential predictive variables
Candidate predictors (i.e., laboratory, demographic, and clinical parameters) were selected from existing models and published literature 6,7,9,11,12,20,21 and included age, sex, Acute Physiology and Chronic Health Evaluation II (APACHE II) score at the time of ICU admission,22 respiratory rate, oxygen requirements and saturation, temperature at admission, white blood cell count and lymphopenia, end-organ dysfunction (including acute kidney injury and evidence of hepatic injury through elevations of hepatic enzymes), and preadmission patient comorbidities (e.g., hypertension, diabetes, coronary artery disease, current smoker, pulmonary disease). Data on biomarkers such as albumin, procalcitonin, ferritin, d-dimer, C-reactive protein (CRP), lactate dehydrogenase, and erythrocyte sedimentation rate were collected where available.23All data were collected at the time of ICU admission (day 0) and in three-day intervals thereafter (day 3, 6, 9, 12, 15) until the patient was discharged from ICU.
Outcomes
The primary outcome was the risk of mortality from the day 0 until day 15 and beyond, assessed dynamically every three days. Secondary outcomes included the median duration of survival, ICU stay, and mechanical ventilation from day 0 and the median duration of hospital stay from the time of intubation. All outcomes were collected up to 30 days, except for overall mortality, which was collected up until study termination on 15 December 2020.
Statistical analysis
Sixty-one variables were used in the initial univariable screening process (Electronic Supplementary Material [ESM] eTable 1), specifying a preset alpha of 0.25.24,25 Two variables, smoking status and alcohol use, were not reliably documented and were excluded from further analysis. Biomarkers not routinely collected as part of patient care (lactate dehydrogenase, ferritin, CRP, and d-dimer) were excluded from the final model because of high rates of missing data. Otherwise, missing data were not common (≤ 10% for any variable) and were addressed using multiple imputation approaches and sensitivity analyses to test the robustness of the study results.
Generalized estimating equations (GEE), which adjust for clustering on the patient, were used to determine the final set of risk factors for inclusion into the model analyzed as repeated measures over time.26,27 The likelihood ratio test was used in a backwards elimination process (P < 0.05 to retain) to select risk factors for retention into the model. As this was an event-driven model, we utilized the recommended ratio of 10:1 for the number of events per included variable.28 The goodness of fit of the final model was assessed with the Hosmer-Lemeshow test. We evaluated model calibration by estimating a smooth calibration line between the observed and predicted outcomes.29 Nonparametric bootstrapping was applied to test the internal validity of the final prediction model.29,30 Resampled data (1,000 iterations) were used to generate bootstrap estimates of the regression coefficients. The confidence intervals of the regression coefficient estimates from the bootstrap sampling were compared with the values calculated by the GEE regression analysis for each time point.
Our intent was to develop a mortality risk algorithm that could be applied to ventilated patients every three days. From the GEE regression outputs, the contribution of the individual risk factor to the risk of mortality was weighted with the final model coefficients. The coefficients were transformed by multiplying each by a constant and then rounding to the nearest unit value. A summary mortality risk score was assigned to each patient by adding the transformed coefficient values (points) for each risk factor they possessed.
The predictive accuracy of the final risk scoring algorithm was assessed by the specificity, sensitivity, and area under the receiver operating characteristic (ROC) curve.31,32 A cut point maximizing sensitivity and specificity was identified. Patients with risk scores above this threshold were classified as “high risk” for mortality over the next three-day period.
Time-to-event outcomes consisting of duration of overall survival, mechanical ventilation, ICU stay, and hospitalization were evaluated by the method of Kaplan-Meier. Time-to-event outcomes were reported as medians, with their interquartile range [IQR]. All statistical analyses were performed using Stata, V16.0 (Stata Corp., College Station, TX, USA).
Results
Demographic and clinical characteristics of the derivation cohort
Four hundred twenty-seven ICU patients were screened for inclusion between 1 March 2020 and 15 December 2020, with 127 meeting eligibility criteria and comprising the final analysis set. The mean (standard deviation [SD]) patient age was 58 (14) yr, and 90 (71%) were male. Most were transferred from other institutions (65%), while the remainder (35%) were internal transfers from wards or the emergency department. At day 0, 83 (65%) patients were intubated, with 28 (22%) intubated on day 1 and 16 (13%) intubated on day 2. The median [IQR] APACHE II score at day 0 was 22 [10–34]. Patients were generally ventilated in accordance with ARDSNet,33 with tidal volumes of 6–8 mL·kg-1 of predicted body weight and permissive hypercapnia (ESM eTables 2 and 3). Until discharge from ICU or death, 39 (31%) patients received extracorporeal membrane oxygenation (ECMO). Demographic and clinical characteristics are shown in ESM eTable 1.
Clinical outcomes in ventilated COVID-19 patients
Overall mortality was 42% (53 patients), with 29% (37 patients) dying within the first 30 days of ICU admission (ESM eTable 2). In the 39 patients who received ECMO, overall mortality was 59% compared with 34% in the 88 patients who did not receive ECMO (P = 0.01). The median [IQR] duration of hospital stay from the day of intubation was 36.9 [19.1–58.5] days, with a median [IQR] duration of intubation of 26.6 [5.6–not reached] days and a median [IQR] duration of ICU stay of 26.9 [15.4–52] days. Median [IQR] overall survival from ICU admission was 43 [22–not reached] days (Table 1).
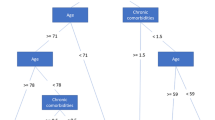
Predictor selection and development of a repeated-measures model
Sixty-one predictors were identified for potential inclusion in the model (ESM eTable 1). After the initial univariable selection procedures, 12 predictors remained for inclusion in the multivariable model. Inclusion of these 12 variables in the multivariable GEE regression model resulted in five variables that remained significantly associated with mortality during the first 15 days of the ICU stay and beyond. The final five variables retained as significant predictors of total mortality on day 0 and at subsequent three-day intervals to day 15 were: age, 24-hr peak temperature, 24-hr peak lactate level, tidal volume at the time of lowest arterial partial pressure of oxygen/fraction of inspired oxygen (PaO2/FiO2) or highest peak pressure (whichever was lowest), and need for vasopressors (Table 2). Corticosteroid administration or elevated CRP was not associated with mortality (ESM eTable 1). A U-shaped mortality curve was observed between the mortality risk and days spent in the ICU. The reference time interval was days 0–2 of ICU admission. The risk of death increased on days 3–6 after ICU admission, declined again between days 9–12, and dramatically increased after day 15 (Table 2). Overall, the lowest risk of death was in the initial 0–2 days of admission. The confidence intervals of the regression coefficients from the bootstrap samples were similar to the values of the coefficients obtained from the GEE multivariable regression analysis, supporting the internal validity of the model.
Development of a scoring tool for the prediction all-cause mortality in ventilated COVID-19 patients
A clinical risk scoring system was derived from the regression coefficients and intercepts generated from the multivariable GEE model. The model was developed to be scored at day 0 and at subsequent three-day intervals following admission (ICU day 3, 6, 9, 12, and 15). The final product was a scoring system between 0 and 100 where higher scores were associated with an increased risk of mortality over each three-day interval from the day 0 (Table 3, Figure). The clinical risk scores were then used to create six risk stratification categories ranging from scores of ≤ 30 to > 70, with higher scores corresponding to a higher risk of mortality. Observed mortality rates are shown by category in Table 4. A risk score > 60 was identified as a threshold for identifying patients at high risk of mortality over the next three-day period. Detailed results are presented in Tables 4 and 5 as the selection of a risk threshold is not a static process and can change based on a clinician’s risk tolerance. The model was further characterized utilizing ROC curve analysis, including an area under the ROC curve (AUC). The AUC was high, at 0.9 (95% confidence interval [CI], 0.8 to 0.9). For each ten-point increase in the risk score, the relative increase in the risk of death was greater than four times, with an odds ratio of 4.1 (95% CI, 2.9 to 5.9).
Relationship between patient risk score and probability of death in intubated COVID-19 patients. Area under the ROC curve = 0.9 (95% CI, 0.8 to 0.9). For every ten-point increase in the risk score, the relative increase in the risk of death is approximately four times (OR = 4.1; 95% CI, 2.9 to 5.9). CI = confidence interval; OR = odds ratio; ROC = receiver operating characteristic
Discussion
The preservation of health system capacity has been a foremost priority during the COVID-19 pandemic, particularly the availability of scarce critical care beds with capacity for invasive mechanical ventilation.34 This paper describes the derivation and internal validation of an accurate, pragmatic, and dynamic clinical risk score for the prediction of all-cause mortality in ventilated COVID-19 patients over three-day intervals during the first 15 days of ICU stay, allowing for risk reassessment related to changes in disease course. The U-shaped curve we observed between mortality risk and days spent in the ICU confirms the importance of reassessing risk after admission.
Our risk score was derived from patients who either presented or were transferred to academic ICUs within one of the largest networks of teaching hospitals in Canada and thus represent a subset of the most critically ill patients. The mortality rate in our cohort (42%) is consistent with the high case fatality rate for patients with COVID-19 receiving invasive mechanical ventilation.35 We identified older age, lower body temperature, higher lactate level, lower tidal volume, and vasopressor use as significant predictors of mortality in mechanically ventilated patients. In addition to high discriminative ability, these variables have high face validity for the prediction of mortality, our outcome of interest, increasing the utility of the model for clinicians. Older age has been well documented to be associated with adverse outcomes and higher mortality in COVID-19.7,10,11,15,16,35,36 Similarly, temperature, lactate level, and vasopressor use are known to be associated with poor outcomes in critical illness (including severe COVID-19 infection).10,16,17,37,38,39,40,41,42 Recent evidence suggests that impaired ability to regulate body temperature, particularly an inappropriately low body temperature, is a strong predictor of COVID-19 mortality.43
Approximately 90% of patients dying of COVID-19 have acute respiratory distress syndrome (ARDS), which is also the primary indication for intubation in the vast majority.2 Previously published predictive models for mortality in ARDS have found age, PaO2/FIO2, and plateau pressures to be predictive of mortality, with an AUC of 0.76 (95% CI, 0.70 to 0.81) in the derivation cohort compared with 0.63 (95% CI, 0.57 to 0.70) for the Acute Physiology and Chronic Health Evaluation (APACHE) II Score.(44) Our final selected variables generated a higher AUC in our derivation cohort, suggesting higher discriminative accuracy for the prediction of mortality in mechanically ventilated COVID-19 patients, the majority of which had a diagnosis of ARDS. For the outcome of hospital mortality, the AUC for the APACHE-II score for all patients in our cohort (those newly admitted to ICU as well as transfers) was 0.56 (95% CI, 0.46 to 0.66). As the APACHE-II score was designed to be used in patients newly admitted to ICU rather than institutional transfers, in the subset of patients within our cohort who were new ICU admissions, the predictive utility of the APACHE-II score remained low, with an AUC of 0.57 (95% CI, 0.40 to 0.74). Although the SOFA score has been advanced as a predictor of mortality in critically ill patients with COVID-19 and as a triage tool, recently its usefulness and accuracy have been questioned in this population, with age alone being a better predictor of outcome than the SOFA score.18 Other prognostic models developed specifically in COVID-19 patients have largely focused on static risk prediction in community or hospital in-patients, rather than dynamic risk prediction in the critically ill.45
The association of higher tidal volumes with decreased risk of mortality may be related to lower compliance with increasing severity of ARDS or differences in outcomes related to underlying heterogeneity in ARDS physiology.33,46,47 In our dataset, patients with ARDS receiving ECMO had a median [IQR] tidal volume of 305 [220–373] mL at admission to ICU compared with a larger median [IQR] tidal volume of 360 [308–400] mL in patients not receiving ECMO (P = 0.004). The median dynamic driving pressure of the group receiving ECMO was 18 cm H2O14,21 at the time of admission to ICU, which was nearly identical to the group not progressing to ECMO (17 cm H2O [12, 20]; P = 0.50). Given the known association between increases in driving pressure and adverse outcomes in ARDS,48,49 it appears that clinicians controlled driving pressure in our cohort, and thus decreases in tidal volume reflect deteriorating compliance and worsening severity of ARDS (ESM eTables 3 and 5). This is consistent with a recent study demonstrating that higher tidal volumes are associated with increased mortality when adjusted for respiratory compliance.36 Additionally, identification of high-compliance “L-type” ARDS in COVID-19 patients and low-compliance “H-Type” patterns may have led to different ventilation strategies, including larger tidal volumes in patients presenting with “L-type” physiology.47
We are currently developing an app for the model, which will allow mortality risk and other outcomes to be calculated rapidly and repeatedly in real time via a smartphone or tablet computer. Future work will seek to validate this model in a larger sample size.
Limitations of our study include the absence of external validation in other datasets, which is our future area of research. Our cohort of patients comprises the development cohort, and the accuracy of our model as assessed by the area under the ROC curve is high. Internal validation of accuracy using bootstrap resamples confirmed our findings. Nevertheless, to confirm widespread generalizability of our findings to other populations, data from patients and hospitals not included in the development cohort should be used as part of the external validation process, which will also confirm the accuracy of the model in other populations.7 While our cohort was inclusive of the majority of COVID-19 patients admitted to ICU at our institutions, on a global scale it remains a small sample with few mortality events. As such, further validation of this prognostic tool in larger datasets is required. While our multivariable model has a high area under the ROC curve, the odds ratios associated with individual risk factors should be interpreted with caution because of the possibility of residual confounding.50 Of note, since development of this risk scoring system, there has been adoption of various therapies, including tocilizumab and sarilumab, which may impact the outcomes of critically ill COVID-19 patients and were not accounted for in our model.51,52,53 For ease of calculation, we have included tidal volume not corrected for predicted body weight (PBW) as a model variable. The vast majority of patients in our cohort were ventilated using the ARDSNet strategy of 6–8 mL·kg-1 of predicted PBW, considered standard of care in patients with COVID-19.33,54 Correlation between the absolute tidal volume and the tidal volume expressed per kg of PBW was high in our sample for all days analyzed (Pearson rho ≥ 0.90; P < 0.001); nevertheless, our model may be less accurate for patients not ventilated according to ARDSNet strategies (ESM eTable 6). Lastly, while mortality is a highly important outcome for patients, other patient-centred outcomes such as long-term sequelae and quality of life should also be considered.55
Conclusion
In this analysis, we derived and internally validated a pragmatic, dynamic, clinical score that facilitates accurate prediction of mortality in ventilated patients with COVID-19. This tool may provide additional prognostic information allowing improved local resource planning and more accurate comparisons across patients treated with different therapies or in different ICUs. Future work is required to validate our results in other cohorts.
References
World Health Organization. Weekly epidemiological update on COVID-19 - 6 April 2021. Available from URL: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---6-april-2021 (accessed October 2021).
Tzotzos SJ, Fischer B, Fischer H, Zeitlinger M. Incidence of ARDS and outcomes in hospitalized patients with COVID-19: a global literature survey. Crit Care 2020; DOI: https://doi.org/10.1186/s13054-020-03240-7.
Public Health Ontario. Weekly Epidemiologic summary: COVID-19 and Severe Outcomes in Ontario. Toronto, Ontario: Queen's Printer for Ontario; 2020: 1-13. Available from URL: https://www.publichealthontario.ca/-/media/documents/ncov/epi/covid-19-severe-outcomes-ontario-epi-summary.pdf?la=en&sc_lang=en&hash=1A963A10F4D25CFEE59323B1451AF86F (accessed October 2021).
Public Health Ontario. COVID-19 in Ontario: January 15, 2020 to April 5, 2021. Available from URL: https://files.ontario.ca/moh-covid-19-report-en-2021-04-06.pdf (accessed October 2021).
Fowler RA, Abdelmalik P, Wood G, et al. Critical care capacity in Canada: results of a national cross-sectional study. Crit Care 2015; DOI: https://doi.org/10.1186/s13054-015-0852-6.
Liang W, Yao J, Chen A, et al. Early triage of critically ill COVID-19 patients using deep learning. Nat Communi2020; DOI: https://doi.org/10.1038/s41467-020-17280-8.
Liang W, Liang H, Ou L, et al. Development and validation of a clinical risk score to predict the occurrence of critical illness in hospitalized patients with COVID-19. JAMA Intern Med 2020; 180: 1081-9.
Chung H, Ko H, Kang WS, et al. Prediction and feature importance analysis for severity of COVID-19 in South Korea using artificial intelligence:model development and validation. J Med Internet Res 202; DOI: https://doi.org/10.2196/27060.
Gupta RK, Harrison EM, Ho A, et al. Development and validation of the ISARIC 4C deterioration model for adults hospitalised with COVID-19: a prospective cohort study. Lancet Respir Med 2021; 9: 349-59.
Heldt FS, Vizcaychipi MP, Peacock S, et al. Early risk assessment for COVID-19 patients from emergency department data using machine learning. medRxiv 2020; DOI: 2020.05.19.20086488.
Knight SR, Ho A, Pius R, et al. Risk stratification of patients admitted to hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: development and validation of the 4C Mortality Score. BMJ 2020; DOI: https://doi.org/10.1136/bmj.m3339.
Chen R, Liang W, Jiang M, et al. Risk factors of fatal outcome in hospitalized subjects with coronavirus disease 2019 from a nationwide analysis in China. Chest 2020; 158: 97-105.
Ko H, Chung H, Kang WS, et al. An artificial intelligence model to predict the mortality of COVID-19 patients at hospital admission time using routine blood samples: development and validation of an ensemble model. J Med Internet Res 2020; DOI: https://doi.org/10.2196/25442.
Beals J 4th, Barnes JJ, Durand DJ, et al. Stratifying deterioration risk by acuity at admission offers triage insights for coronavirus disease 2019 patients. Crit Care Explor 2021; DOI: https://doi.org/10.1097/CCE.0000000000000400.
Gue YX, Tennyson M, Gao J, Ren S, Kanji R, Gorog DA. Development of a novel risk score to predict mortality in patients admitted to hospital with COVID-19. Sci Rep 2020; DOI: https://doi.org/10.1038/s41598-020-78505-w.
Nicholson CJ, Wooster L, Sigurslid HH, et al. Estimating risk of mechanical ventilation and in-hospital mortality among adult COVID-19 patients admitted to Mass General Brigham: the VICE and DICE scores. EClinicalMedicine 2021; DOI: https://doi.org/10.1016/j.eclinm.2021.100765.
Ryan L, Lam C, Mataraso S, et al. Mortality prediction model for the triage of COVID-19, pneumonia, and mechanically ventilated ICU patients: a retrospective study. Ann Med Surg (Lond) 2020; 59: 207-16.
Raschke RA, Agarwal S, Rangan P, Heise CW, Curry SC. Discriminant accuracy of the SOFA score for determining the probable mortality of patients with COVID-19 pneumonia requiring mechanical ventilation. JAMA 2021; 325: 1469-70.
Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ 2015; DOI: https://doi.org/10.1136/bmj.g7594.
Liu T, Liang W, Zhong H, et al. Risk factors associated with COVID-19 infection: a retrospective cohort study based on contacts tracing. Emerg Microbes Infect 2020; 9: 1546-53.
Beals J, Barnes J, Durand D, et al. Identification on admission of COVID-19 patients at risk of subsequent rapid clinical deterioration. medRxiv 2020; DOI: https://doi.org/10.1101/2020.08.13.20171751.
Sadaka F, EthmaneAbouElMaali C, Cytron MA, Fowler K, Javaux VM, O'Brien J. Predicting mortality of patients with sepsis: a comparison of APACHE II and APACHE III scoring systems. J Clin Med Res 2017; 9: 907-10.
Rodriguez-Morales AJ, Cardona-Ospina JA, Gutierrez-Ocampo E, et al. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis 2020; DOI: https://doi.org/10.1016/j.tmaid.2020.101623.
Allison PD. Logistic Regression Using the SAS System: Theory and Application. SAS Publishing; 1999: 179-216.
Grant SW, Collins GS, Nashef SA. Statistical Primer: developing and validating a risk prediction model. Eur J Cardiothorac Surg 2018; 54: 203-8.
Rabe-Hesketh S, Everitt B. Statistical Analysis Using Stata. Chapman & Hall/CRC; 2000: 119-36.
Lyman GH, Kuderer NM. A primer in prognostic and predictive models: development and validation of neutropenia risk models. Support Cancer Ther 2005; 2: 168-75.
Katz MH. Multivariable analysis: a primer for readers of medical research. Ann Intern Med 2003; 138: 644-50.
Steyerberg EW, Eijkemans MJ, Harrell FE Jr, Habbema JD. Prognostic modeling with logistic regression analysis: in search of a sensible strategy in small data sets. Med Decis Making 2001; 21: 45-56.
Steyerberg EW, Harrell FE Jr, Borsboom GJ, Eijkemans MJ, Vergouwe Y, Habbema JD. Internal validation of predictive models: efficiency of some procedures for logistic regression analysis. J Clin Epidemiol 2001; 54: 774-81.
Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 1982; 143: 29-36.
McNeil BJ, Hanley JA. Statistical approaches to the analysis of receiver operating characteristic (ROC) curves. Med Decis Making 1984; 4: 137-50.
Slutsky AS, Ranieri VM. Mechanical ventilation: lessons from the ARDSNet trial. Respir Res 2000; 1: 73-7.
Shoukat A, Wells CR, Langley JM, Singer BH, Galvani AP, Moghadas SM. Projecting demand for critical care beds during COVID-19 outbreaks in Canada. CMAJ 2020; 192: E489-96.
Lim ZJ, Subramaniam A, Ponnapa Reddy M, et al. Case fatality rates for patients with COVID-19 requiring invasive mechanical ventilation. a meta-analysis. Am J Respir Crit Care Med 2021; 203: 54-66.
Botta M, Tsonas AM, Pillay J, et al. Ventilation management and clinical outcomes in invasively ventilated patients with COVID-19 (PRoVENT-COVID): a national, multicentre, observational cohort study. Lancet Respir Med 2021; 9: 139-48.
Rhodes A, Evans LE, Alhazzani W, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Crit Care Med 2017; 45: 486-555.
Shankar-Hari M, Phillips GS, Levy ML, et al. Developing a new definition and assessing new clinical criteria for septic shock: for the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016; 315: 775-87.
Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med 1996; 22: 707-10.
Wong DT, Crofts SL, Gomez M, McGuire GP, Byrick RJ. Evaluation of predictive ability of APACHE II system and hospital outcome in Canadian intensive care unit patients. Crit Care Med 1995; 23: 1177-83.
Roomi S, Shah SO, Ullah W, et al. Declining intensive care unit mortality of COVID-19: a multi-center study. J Clin Med Res 2021; 13: 184-90.
Auld SC, Caridi-Scheible M, Blum JM, et al. ICU and ventilator mortality among critically ill adults with coronavirus disease 2019. Crit Care Med 2020; 48: e799-804.
Tharakan S, Nomoto K, Miyashita S, Ishikawa K. Body temperature correlates with mortality in COVID-19 patients. Crit Care 2020; DOI: https://doi.org/10.1186/s13054-020-03045-8.
Villar J, Ambrós A, Soler JA, et al. Age, PaO2/FIO2, and plateau pressure score: a proposal for a simple outcome score in patients with the acute respiratory distress syndrome. Crit Care Med 2016; 44: 1361-9.
Wynants L, Van Calster B, Collins GS, et al. Prediction models for diagnosis and prognosis of covid-19: systematic review and critical appraisal. BMJ 2020; DOI: https://doi.org/10.1136/bmj.m1328.
Tsolaki V, Zakynthinos GE, Makris D. The ARDSnet protocol may be detrimental in COVID-19. Crit Care 2020; DOI: https://doi.org/10.1186/s13054-020-03081-4.
Fan E, Beitler JR, Brochard L, et al. COVID-19-associated acute respiratory distress syndrome: is a different approach to management warranted? Lancet Respir Med 2020; 8: 816-21.
Amato MB, Meade MO, Slutsky AS, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med 2015; 372: 747-55.
Urner M, Jüni P, Hansen B, Wettstein MS, Ferguson ND, Fan E. Time-varying intensity of mechanical ventilation and mortality in patients with acute respiratory failure: a registry-based, prospective cohort study. Lancet Respir Med 2020; 8: 905-13.
Sjoding MW, Luo K, Miller MA, Iwashyna TJ. When do confounding by indication and inadequate risk adjustment bias critical care studies? A simulation study. Crit Care 2015; DOI: https://doi.org/10.1186/s13054-015-0923-8.
REMAP-CAP Investigators; Gordon AC, Mouncey PR, Al-Beidh F, et al. Interleukin-6 receptor antagonists in critically ill patients with Covid-19. N Engl J Med 2021; 384: 1491-502.
Wu C, Hou D, Du C, et al. Corticosteroid therapy for coronavirus disease 2019-related acute respiratory distress syndrome: a cohort study with propensity score analysis. Crit Care 2020; DOI: https://doi.org/10.1186/s13054-020-03340-4.
Prescott HC, Rice TW. Corticosteroids in COVID-19 ARDS: evidence and hope during the pandemic. JAMA 2020; 324: 1292-5.
Marini JJ, Gattinoni L. Management of COVID-19 respiratory distress. JAMA 2020; 323: 2329-30.
Gaudry S, Messika J, Ricard J-D, et al. Patient-important outcomes in randomized controlled trials in critically ill patients: a systematic review. Ann Intensive Care 2017; 7: 28-.
Author contributions
Justyna Bartoszko, George Dranitsaris, M. Elizabeth Wilcox, Lorenzo Del Sorbo, Sangeeta Mehta, Miki Peer, Matteo Parotto, Isaac Bogoch, and Sheila Riazi contributed to all aspects of this manuscript, including conception and design; acquisition, analysis, and interpretation of data and drafting the article.
Acknowledgements
We thank Humara Poonawala, Kawalpreet Singh, and Shiva Khandadashpoor for data collection; Mr. Gordon Tait for database creation; and Ms. Jo Carroll for coordination across sites and supervision of the conduct of the study.
Disclosures
None.
Funding statement
Funded by Ontario Ministry of Health COVID-19 Rapid Research Fund, Grant # 703.
Editorial responsibility
This submission was handled by Dr. Philip M. Jones, Deputy Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is accompanied by an editorial. Please see Can J Anesth 2022; this issue.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bartoszko, J., Dranitsaris, G., Wilcox, M.E. et al. Development of a repeated-measures predictive model and clinical risk score for mortality in ventilated COVID-19 patients. Can J Anesth/J Can Anesth 69, 343–352 (2022). https://doi.org/10.1007/s12630-021-02163-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-021-02163-3