Abstract
Purpose of Review
We aim to review the appearance of ductal carcinoma in situ (DCIS) across the spectrum of imaging modalities used in common clinical practice.
Recent Findings
Changes in technology and clinical breast cancer screening patterns have impacted the imaging evaluation of DCIS. DCIS classically presents as asymptomatic calcifications in women undergoing screening mammography. The replacement of traditional 2D mammography with digital breast tomosynthesis has changed the typical appearance of screen-detected DCIS. Ultrasound is traditionally utilized to detect DCIS in women with clinical symptoms, but efforts to increase screening ultrasound rates for women with dense breasts makes it more important to identify the appearance of DCIS in asymptomatic women. Improvements in MRI technology have made MRI the most sensitive imaging modality to detect DCIS and define the extent of disease, which is increasingly important given greater utilization of MRI for high-risk screening and determination of extent of known disease. Finally, the emergence of active surveillance, or non-surgical management, for DCIS has increased the focus on presurgical identification of associated invasive cancer, with early results demonstrating promise via computer vision and deep learning approaches for this task.
Summary
DCIS has a highly variable imaging appearance which is subject to changes in imaging technology and clinical management.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ductal carcinoma in situ (DCIS) is a non-invasive stage 0 form of breast cancer [1]. DCIS classically presents as an asymptomatic incidental finding and the widespread adoption of organized screening mammography has resulted in a steady increase in the incidence of DCIS [2]. Although DCIS has been well-described in the literature over the last several decades, recent changes to clinical practice and imaging technology have shifted the focus of DCIS imaging. First, the rapid adoption of digital breast tomosynthesis (DBT), also referred to as 3D mammography, requires an understanding of the key similarities and differences in the appearance of DCIS on DBT from traditional 2D mammography. Second, recognizing the appearance of DCIS on ultrasound (US) is increasingly important due to widespread advocacy efforts and state legislation regarding supplemental ultrasound for women with dense breasts [3]. Third, new high-risk screening guidelines recommend annual MRI, which increases the population of women undergoing screening MRI [4]. Finally, ongoing clinical trials are exploring the feasibility of non-surgical treatment of DCIS, termed active surveillance. Safe enrollment in active surveillance requires differentiation of DCIS from invasive disease in the presurgical setting, which is a relatively novel task for radiologists. It is therefore important to have a comprehensive understanding of the multimodality appearance of DCIS.
Mammographic Appearance of DCIS
With the implementation of screening mammography, the incidence of DCIS has increased significantly and now accounts for approximately 25% of breast cancers in the USA [5]. Furthermore, improved mammographic technology and standards for reporting have resulted in mammographic sensitivity of 87–95% for the evaluation of DCIS (Table 1) [5]. DCIS most commonly (~ 75%) presents as asymptomatic calcifications on screening mammography (Fig. 1) and less often as a mass or architectural distortion (Fig. 2) [6]. In cases of symptomatic DCIS, the most common presentation is either a palpable lump or nipple discharge.
The underlying mechanisms responsible for the presence of associated calcifications in DCIS are not well established. Calcifications comprised of calcium oxalate (type I) are generally associated with benign non-DCIS pathology while those composed of calcium hydroxyapatite (type II) are more typical for DCIS [7]. Modeling based on physiologic bone mineralization has given insights into how these pathologic microcalcifications may be formed [8]. It is hypothesized that physiologic bone matrix proteins are expressed in mammary cells and demonstrate altered expression in the tumor microenvironment. For example, the phosphoprotein OPN responsible for regulating mineralization is abundant in bone but is also known to be expressed in breast cancer and associated with a worse prognosis. Nonetheless, even though mammographic calcifications have been evaluated for decades, our understanding of their genesis and clinical relevance remains an area of active investigation.
DCIS microcalcifications typically present with a suspicious morphology and/or distribution defined by the American College of Radiology Breast Imaging Reporting and Data System (BI-RADS) Atlas [9•]. The suspicious morphology descriptors in order of likelihood of malignancy are coarse heterogeneous (13%), amorphous (21%), fine pleomorphic (29%), and fine linear or fine-linear branching (70%) [9•]. In rare cases, typically benign morphologies, such as round, can be found with DCIS, but these are usually low grade cases without comedonecrosis [6]. The distribution of microcalcifications is also associated with the likelihood of malignancy: diffuse (0%), regional (26%), grouped (31%), linear (60%), and segmental (62%) [9•]. However, the utilization of these morphology and distribution descriptors is not evenly distributed and the majority of DCIS cases present as grouped pleomorphic calcifications [10]. Due to the notable inter- and intra-observer variability in the use of these BI-RADS descriptors, it is less important which suspicious descriptors are used, but rather to differentiate between the definitively benign and suspicious descriptors [11].
Microcalcifications may also provide prognostic information. DCIS is a heterogeneous disease process with discrete nuclear grades, varying levels of cellular differentiation, and potential comedonecrosis, all of which can affect the biology of the disease [5]. Several studies have linked microcalcifications demonstrating linear branching, coarse heterogeneous, and fine pleomorphic morphologies with an increased risk of local recurrence [10, 12, 13]. These morphologies are also associated with higher nuclear grade and comedonecrosis [10, 14]. Comedonecrosis is thought to demonstrate a greater invasive potential and proliferation rate indicating a more aggressive biology [15]. However, due to the significant overlap in mammographic appearance of different histological grades, the correlation between calcification morphology and histological grade may be somewhat variable [16, 17]. The number and extent of calcifications are also prognostic factors. Calcification numbers in excess of 20 correlate with higher nuclear grade and the presence of necrosis [6], while larger lesion size correlates with increased risk of occult microinvasion and multicentric disease [18].
Approximately one quarter of DCIS cases will present with an associated mass, asymmetry, or architectural distortion, either alone or in conjunction with calcifications [6, 19, 20]. These soft tissue components may represent distended and dilated ducts, periductal fibrosis, or elastosis. However, it may also represent associated invasive disease, as a mass or palpable abnormality increases the likelihood of upstaging to invasive disease at surgical excision [21••]. When DCIS does present as a soft tissue abnormality without calcifications, it is more likely to be grade 1 DCIS [6, 20]. Interestingly, the proportion of DCIS presenting as a soft tissue abnormality increases with age, which might reflect differences in DCIS biology or an obscuring of subtle masses in younger women with dense breasts [19, 22]. Finally, it is uncommon for DCIS to present as architectural distortion but this appearance is often found in association with sclerosing adenosis or radial scar with DCIS incidentally found in the adjacent Cooper’s ligaments [23].
Digital Breast Tomosynthesis Appearance of DCIS
Digital breast tomosynthesis (DBT) is rapidly replacing traditional 2D mammography as the primary breast cancer screening modality. Given the improved ability of DBT to evaluate masses, asymmetries, and architectural distortion, especially in women with dense breasts, DBT offers improved detection for non-calcified DCIS [24]. Similarly, DBT allows for improved detection of associated soft tissue abnormalities in cases of calcified DCIS, which may signify an underlying invasive disease component [25]. For calcified DCIS, the performance depends on whether DBT is performed in conjunction with mammography or whether synthetic mammograms (SM) generated from the tomosynthesis images are used. DBT plus mammography requires approximately double the radiation dose and multiple studies have shown that cancer detection rates are comparable whether traditional mammography or SM is used in conjunction with DBT [26, 27]. As a result, DBT is increasingly being performed alone with SM as a replacement for mammography.
SM are generated by vendor-specific proprietary algorithms created from the individual low-dose tomosynthesis acquisitions but this process changes the appearance of DCIS calcifications via the accentuation algorithms utilized to make abnormalities appear more conspicuous [28, 29••]. In general, SM offers comparable performance to traditional mammography for the detection of calcifications and to define their extent, although published series are conflicted [30,31,32,33]. However, the morphology of calcifications on SM can be distorted such that BI-RADS descriptors to differentiate benign from suspicious calcifications cannot be adequately assessed (Fig. 3). As a result, DCIS calcifications may be incorrectly dismissed as benign on SM and it is best practice to obtain additional standard 2D views, particularly magnification views, for any new calcifications.
Ultrasound Appearance of DCIS
While DCIS is most commonly identified through the presence of microcalcifications on mammography, ultrasound may be helpful in the detection of non-calcified DCIS and for further characterization of mammographic and MRI findings.
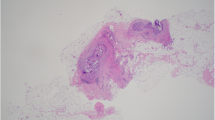
Non-calcified DCIS, often presenting as a mass or asymmetry, is thought to represent between 2 and 23% of DCIS cases [19, 34, 35••]. Clinical scenarios may include nipple discharge, abnormality detected at screening ultrasound, or a mammographically occult palpable lesion. The findings of non-calcified DCIS on ultrasound are heterogeneous—mass, ductal changes, distortion, cluster of cysts, vague hypoechoic area—with mass being the most commonly reported abnormality of those visible on ultrasound (Fig. 4) [20]. Masses may be somewhat benign in appearance with oval shape and circumscribed or indistinct margins with parallel orientation though also can be irregularly shaped with non-circumscribed, frequently microlobulated margins, and internal vascularity [19, 34, 36]. The presence of internal vascularity may be seen in up to 50% of masses and may heighten suspicion for malignancy when evaluating lesions [35••]. Ductal extension may be absent. A “pseudomicrocystic” appearance is a non-BI-RADS descriptor that has been coined for DCIS that appears as a predominantly cystic lesion with solid components [37•]. Ductal changes including abnormal duct enlargement and ducts with solid filling defects, without associated microcalcifications, can be seen with non-calcified DCIS.
DCIS may often be found in conjunction with other benign or high-risk pathologies and there is significant overlap in the appearance of DCIS and sclerosing adenosis, apocrine metaplasia, atypical ductal hyperplasia, intraductal papilloma, fibrocystic change, and secretory changes. When associated with an intraductal papilloma (Fig. 5) or radial scar, DCIS may present on ultrasound as a vague area of shadowing due to underlying desmoplastic reaction. Recent literature suggests that a significant portion of non-calcified DCIS presents sonographically as a vague hypoechoic area [36]. This reflects the more typical appearance of DCIS on MRI as a focal or segmental area of enhancement, rather than a discrete mass. When DCIS (non-calcified) is identified on screening ultrasound, it is associated with favorable prognostic factors including lower nuclear grade, smaller tumor size, less comedonecrosis, and more hormone receptor positivity, compared to mammographically detected calcified DCIS [38].
In the evaluation of calcified DCIS, ultrasound is typically used to further evaluate a mammographically apparent soft tissue component or to facilitate biopsy planning when a stereotactic biopsy is not feasible. Ultrasound may be able to visualize 23–45% of calcifications seen at mammography [39, 40], with one study reporting minimum detected size at 0.5 cm [35••]. The ultrasound appearance of calcifications includes echogenic foci within a mass or duct and less commonly echogenic foci without a hypoechoic area or duct changes. Associated masses are often irregularly shaped and mildly hypoechoic with indistinct or microlobulated borders and may demonstrate ductal extension due to spread along ducts [37•, 41]. Mammographic features of calcifications that facilitate ultrasound detection are extent of calcifications greater than 1 cm and segmental distribution [42]. Calcifications that are visible on ultrasound have a higher likelihood of being malignant compared to those not seen and when associated with a mass more likely to have an invasive component [42].
MRI Appearance of DCIS
Historically, DCIS detection with MRI was associated with high false-negative rates because of MRI’s inability to depict characteristic microcalcifications. With improvements in breast MRI spatial resolution over the past two decades, a distinct MRI abnormality, non-mass enhancement (NME), was found to commonly represent DCIS lesions. Upon integration of NME into the ACR BI-RADS lexicon, subsequent studies showed that MRI is in fact superior to mammography for DCIS identification, with particularly high sensitivity for high-grade lesions (Table 1) [43••, 44]. MRI is not only the most sensitive modality for identifying DCIS but also superior in extent of disease determination for treatment planning as shown by separate studies (Fig. 6) [45,46,47]. One study demonstrated that MRI estimated the correct size of DCIS to within 5 mm in 60% of cases compared to only 38% of cases for mammography [46]. Higher spatial resolution acquisitions achievable with 3 T systems are potentially providing even more accurate disease estimations [48•, 49].
On MRI, 60–80% of DCIS is described as segmentally or linearly distributed NME with clumped internal enhancement morphology (Fig. 7) [50,51,52]. NME is defined on MRI as an area of suspicious fibroglandular tissue enhancement that is not a mass (i.e., not space-occupying and no convex margins) and is of sufficient size that it would not be characterized as a focus (i.e., typically larger than 5 mm). Biologically, DCIS begins with intraductal tumor angiogenesis and proliferates locally through the breast ductal pathway recruiting abnormal periductal or stromal vascularity, which likely explains this unique enhancement pattern [5, 53]. Indeed, a mouse model suggests that DCIS enhancement is in part from the gadolinium contrast traveling across the milk duct basement membrane and collecting in the breast ducts, where DCIS resides [54]. This likely explains why linear (corresponding to a single duct) or segmental (triangular or conical with apex directed toward the nipple) distributions of NME are most commonly associated with DCIS pathology. In terms of NME internal enhancement, clumped (aggregates of small areas of enhancement forming a “cobblestone” pattern) is most often seen in DCIS, but clustered ring (thin rings of enhancement surrounding ducts, clustered together), a newer BI-RADS descriptor, is increasingly associated with DCIS and likely represents gadolinium accumulating peri- and intra-ductally (Fig. 8) [55, 56]. DCIS lesions less commonly present as masses or foci, where the growth pattern is more expansile. Local expansion thought to be a more indolent growth pattern and corresponds with several studies which have shown that DCIS presenting as foci [57] or masses [58, 59] rather than calcifications are more often associated with lower grade disease.
While NME is the most common MRI presentation of DCIS, it is not specific for DCIS since benign proliferative pathology, including fibrocystic changes and pseudoangiomatous stromal hyperplasia (PASH), invasive breast cancer (ductal more common than lobular), and even normal breast tissue, can all present as NME. On dynamic contrast enhancement (DCE) MRI, DCIS exhibits variable kinetic enhancement features, with only a minority (28–44% of cases) of DCIS exhibiting the typical malignant kinetic profile of fast initial phase (signal increase of at least 100%) and washout on delayed phase (subsequent signal decrease of at least 10%) [5, 50]. Thus, since there are generally no morphologic or kinetic features of sufficient negative predictive value to obviate the need for biopsy, most NME lesions identified on MRI should be sampled rather than observed. Furthermore, when NME is identified on MRI performed to evaluate the extent of a known breast cancer, it is essential the NME is sampled under image guidance rather than simply incorporated in the primary surgical so that unnecessarily extensive surgeries prompted by breast MRI are avoided.
While it is well established that MRI has exceptional sensitivity for DCIS detection, its clinical role remains controversial. For newly diagnosed DCIS by conventional imaging, disagreements remain regarding the value of preoperative MRI to improve surgical outcomes. Many have raised concerns that MRI leads to unnecessary mastectomies without a clear operative advantage, although it should be noted that most of the historical studies evaluating its use have been relatively small and retrospective in nature [60]. A recently completed prospective single arm multi-center trial (ECOG-ACRIN 4112) demonstrated that MRI accounts for a minority of conversions to mastectomy with most mastectomies performed due to patient preference, genetic testing outcomes, or positive margins on breast conservation surgery (BCS) [61•]. Furthermore, this trial demonstrated a very high rate (96.1%) of successful BCS for women who had wide local excision performed after MRI, which was corroborated by a recently published retrospective study by Lam and colleagues [62]. However, a small randomized trial of preoperative MRI failed to show a significant reduction in DCIS reoperation rates in the MRI-arm based on intention-to-treat analysis, although MRI did demonstrate a significant surgical benefit in the per-protocol analysis [63].
While the immediate surgical value of MRI to evaluate DCIS remains controversial, MRI may hold its greatest merit in facilitating individualized treatments [64]. Currently, the majority of DCIS lesions are likely overtreated with either excessive surgery, radiation, or medical therapy. Although MRI is superior for high-grade DCIS detection, its strength in assisting with treatment de-escalation remains largely unexplored. The aforementioned ECOG-ACRIN 4112 trial demonstrated a high level of patient acceptance for MRI in conjunction with a 12 gene assay (Oncotype DX-DCIS) to determine the need for radiation therapy [61•]. Additionally, smaller individual studies have demonstrated the intriguing potential of approaches using MRI radiomics to predict DCIS biology and recurrence likelihood [65, 66]. The future direction of MRI research should not only evaluate short-term surgical outcomes but also determine meaningful long-term outcomes, such as breast cancer recurrence and survival rates.
Active Surveillance for DCIS
Active surveillance is an alternative management strategy for DCIS that avoids surgical excision for select women with LOw Risk DCIS in order to address issues of overdiagnosis and overtreatment associated with the current standard of care surgical excision approach [67, 68].
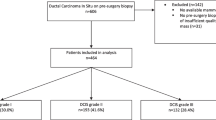
There are currently three randomized prospective active surveillance trials in progress: The Comparison of Operation versus Monitoring with or without Endocrine Therapy for LOw Risk DCIS trial (COMET) in the USA [69], the LOw Risk DCIS trial (LORIS) in the UK [70], and the Management of LOw Risk DCIS trial (LORD) in the Netherlands [71]. Although the inclusion and exclusion criteria differ slightly between the trials, the success of active surveillance as a management strategy for DCIS requires improved methods to identify associated invasive disease at the time of initial diagnosis as these women will not have surgical excision and undetected invasive disease could grow and metastasize.
The average upstaging rate of DCIS to invasive cancer at surgical excision is approximately 25% according to a large meta-analysis published in 2011, with several radiological (e.g., mass), clinical (e.g., symptomatic), and pathological (e.g., high nuclear grade) factors associated with higher upstaging rates (Fig. 9) [21••]. The application of multiple risk factors can reduce the upstaging rate to as low as 10%, but further efforts are needed to maximize the safety of active surveillance [21••, 72, 73]. Radiologists are not trained to differentiate DCIS from invasive disease as it is not currently a routine part of clinical focus for breast imagers, and research efforts have demonstrated that radiologists are only moderately successful at this task [74, 75••]. Changes to routine DCIS workflows to include ultrasound and MRI to evaluate for potential invasive disease may be needed for women eligible for active surveillance, while being mindful that additional imaging could increase the extent of intervention. Furthermore, different imaging modalities may be evaluating different aspects of DCIS, as exemplified by the CALGB 40903 trial which demonstrated that women with estrogen receptor positive DCIS treated with endocrine therapy had a decrease in tumor size on MRI but no appreciable change in size was noted on mammography [76]. The use of image analytics via computer derived features as well as deep learning features applied to both mammography and MRI have demonstrated preliminary success [75••, 77, 78]. However, larger datasets are needed to test the utility of these approaches given the sample size demands of advanced quantitative image analysis. Ultimately, a combination of imaging, clinical, and pathological advances will likely prove to be the most successful at reducing upstaging rates for patients potentially eligible for an active surveillance approach.
Conclusion
DCIS has a highly variable appearance on all imaging modalities. As technology improves, the relative strengths and weaknesses of each imaging modality will evolve for future evaluation of DCIS. Furthermore, changing clinical practice patterns, including screening ultrasound for women with dense breasts, high-risk screening MRI, and active surveillance will alter the most common clinical presentations of DCIS. Although mammography detects over 80% of DCIS, clinicians must recognize which imaging modality or combinations of imaging modalities to use in the appropriate clinical context for detection, evaluation, and surveillance of DCIS.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
American Joint Committee on Cancer. Breast Cancer Staging 7th edition. In: American Cancer Society.
Cancer facts & figures 2017. In: American Cancer Society,
Hooley RJ. Breast density legislation and clinical evidence. Radiol Clin N Am. 2017;55:513–26. https://doi.org/10.1016/j.rcl.2016.12.006.
Monticciolo DL, Newell MS, Moy L, Niell B, Monsees B, Sickles EA. Breast cancer screening in women at higher-than-average risk: recommendations from the ACR. J Am Coll Radiol. 2018;15:408–14. https://doi.org/10.1016/j.jacr.2017.11.034.
Yamada T, Mori N, Watanabe M, et al. Radiologic-pathologic correlation of ductal carcinoma in situ. Radiographics. 2010;30:1183–98. https://doi.org/10.1148/rg.305095073.
Barreau B, de Mascarel I, Feuga C, et al. Mammography of ductal carcinoma in situ of the breast: review of 909 cases with radiographic-pathologic correlations. Eur J Radiol. 2005;54:55–61. https://doi.org/10.1016/j.ejrad.2004.11.019.
O'Grady S, Morgan MP. Microcalcifications in breast cancer: from pathophysiology to diagnosis and prognosis. Biochim Biophys Acta Rev Cancer. 1869;2018:310–20. https://doi.org/10.1016/j.bbcan.2018.04.006.
Cox RF, Morgan MP. Microcalcifications in breast cancer: lessons from physiological mineralization. Bone. 2013;53:437–50. https://doi.org/10.1016/j.bone.2013.01.013.
• D’Orsi CJSE, Mendelson EB, Morris EA. ACR BI-RADS® Atlas, Breast Imaging Reporting and Data System. Reston: American College of Radiology; 2013. Primary lexicon by which breast radiologists interpret breast imaging studies.
Rauch GM, Hobbs BP, Kuerer HM, et al. Microcalcifications in 1657 patients with pure ductal carcinoma in situ of the breast: correlation with clinical, histopathologic, biologic features, and local recurrence. Ann Surg Oncol. 2016;23:482–9. https://doi.org/10.1245/s10434-015-4876-6.
Lee AY, Wisner DJ, Aminololama-Shakeri S, et al. Inter-reader variability in the use of BI-RADS descriptors for suspicious findings on diagnostic mammography: a multi-institution study of 10 academic radiologists. Acad Radiol. 2017;24:60–6. https://doi.org/10.1016/j.acra.2016.09.010.
Holmberg L, Wong YN, Tabar L, et al. Mammography casting-type calcification and risk of local recurrence in DCIS: analyses from a randomised study. Br J Cancer. 2013;108:812–9. https://doi.org/10.1038/bjc.2013.26.
Malik HZ, Wilkinson L, George WD, Purushotham AD. Preoperative mammographic features predict clinicopathological risk factors for the development of local recurrence in breast cancer. Breast. 2000;9:329–33. https://doi.org/10.1054/brst.1999.0148.
Stomper PC, Connolly JL. Ductal carcinoma in situ of the breast: correlation between mammographic calcification and tumor subtype. AJR Am J Roentgenol. 1992;159:483–5. https://doi.org/10.2214/ajr.159.3.1323923.
Evans A, Pinder S, Wilson R, et al. Ductal carcinoma in situ of the breast: correlation between mammographic and pathologic findings. AJR Am J Roentgenol. 1994;162:1307–11. https://doi.org/10.2214/ajr.162.6.8191988.
Dinkel HP, Gassel AM, Tschammler A. Is the appearance of microcalcifications on mammography useful in predicting histological grade of malignancy in ductal cancer in situ? Br J Radiol. 2000;73:938–44. https://doi.org/10.1259/bjr.73.873.11064645.
Slanetz PJ, Giardino AA, Oyama T, et al. Mammographic appearance of ductal carcinoma in situ does not reliably predict histologic subtype. Breast J. 2001;7:417–21.
Leonard GD, Swain SM. Ductal carcinoma in situ, complexities and challenges. J Natl Cancer Inst. 2004;96:906–20.
Stomper PC, Connolly JL, Meyer JE, Harris JR. Clinically occult ductal carcinoma in situ detected with mammography: analysis of 100 cases with radiologic-pathologic correlation. Radiology. 1989;172:235–41. https://doi.org/10.1148/radiology.172.1.2544922.
Yang WT, Tse GM. Sonographic, mammographic, and histopathologic correlation of symptomatic ductal carcinoma in situ. AJR Am J Roentgenol. 2004;182:101–10. https://doi.org/10.2214/ajr.182.1.1820101.
•• Brennan ME, Turner RM, Ciatto S, et al. Ductal carcinoma in situ at core-needle biopsy: meta-analysis of underestimation and predictors of invasive breast cancer. Radiology. 2011;260:119–28. https://doi.org/10.1148/radiol.11102368A large meta-analysis demonstrating upstaging rates for DCIS to invasive disease and presurgical factors associated with upstaging.
Hermann G, Janus C, Schwartz IS, Papatestas A, Hermann DG, Rabinowitz JG. Occult malignant breast lesions in 114 patients: relationship to age and the presence of microcalcifications. Radiology. 1988;169:321–4. https://doi.org/10.1148/radiology.169.2.2845470.
Sekine K, Tsunoda-Shimizu H, Kikuchi M, Saida Y, Kawasaki T, Suzuki K. DCIS showing architectural distortion on the screening mammogram—comparison of mammographic and pathological findings. Breast Cancer. 2007;14:281–4.
Su X, Lin Q, Cui C, et al. Non-calcified ductal carcinoma in situ of the breast: comparison of diagnostic accuracy of digital breast tomosynthesis, digital mammography, and ultrasonography. Breast Cancer. 2017;24:562–70. https://doi.org/10.1007/s12282-016-0739-7.
Xu Y, Miyake KK, Liu YI, et al. The Milky Way Sign: a new diagnostic finding of ductal carcinoma in situ on digital breast tomosynthesis. Breast J. 2016;22:349–51. https://doi.org/10.1111/tbj.12583.
Bernardi D, Macaskill P, Pellegrini M, et al. Breast cancer screening with tomosynthesis (3D mammography) with acquired or synthetic 2D mammography compared with 2D mammography alone (STORM-2): a population-based prospective study. Lancet Oncol. 2016;17:1105–13. https://doi.org/10.1016/S1470-2045(16)30101-2.
Caumo F, Zorzi M, Brunelli S, et al. Digital breast tomosynthesis with synthesized two-dimensional images versus full-field digital mammography for population screening: outcomes from the Verona screening program. Radiology. 2018;287:37–46. https://doi.org/10.1148/radiol.2017170745.
Kopans DB. Digital breast tomosynthesis from concept to clinical care. AJR Am J Roentgenol. 2014;202:299–308. https://doi.org/10.2214/AJR.13.11520.
•• Horvat JV, Keating DM, Rodrigues-Duarte H, Morris EA, Mango VL. Calcifications at digital breast tomosynthesis: imaging features and biopsy techniques. Radiographics. 2019;39:307–18. https://doi.org/10.1148/rg.2019180124A review of the appearance of calcifications on digital breast tomosynthesis.
Hwang E, Szabo J, Sonnenblick EB, Margolies LR. Variable appearances of ductal carcinoma in situ calcifications on digital mammography, synthesized mammography, and tomosynthesis: a pictorial essay. Can Assoc Radiol J. 2018;69:2–9. https://doi.org/10.1016/j.carj.2017.04.005.
Berger N, Schwizer SD, Varga Z, Rageth C, Frauenfelder T, Boss A. Assessment of the extent of microcalcifications to predict the size of a ductal carcinoma in situ: comparison between tomosynthesis and conventional mammography. Clin Imaging. 2016;40:1269–73. https://doi.org/10.1016/j.clinimag.2016.09.003.
Bernardi D, Caumo F, Macaskill P, et al. Effect of integrating 3D-mammography (digital breast tomosynthesis) with 2D-mammography on radiologists’ true-positive and false-positive detection in a population breast screening trial. Eur J Cancer. 2014;50:1232–8. https://doi.org/10.1016/j.ejca.2014.02.004.
Tagliafico A, Mariscotti G, Durando M, et al. Characterisation of microcalcification clusters on 2D digital mammography (FFDM) and digital breast tomosynthesis (DBT): does DBT underestimate microcalcification clusters? Results of a multicentre study. Eur Radiol. 2015;25:9–14. https://doi.org/10.1007/s00330-014-3402-8.
Ikeda DM, Andersson I. Ductal carcinoma in situ: atypical mammographic appearances. Radiology. 1989;172:661–6. https://doi.org/10.1148/radiology.172.3.2549563.
•• Horvat JV, Keating DM, Rodrigues-Duarte H, Morris Wang LC, Sullivan M, Du H, et al. US appearance of ductal carcinoma in situ. Radiographics. 2013;33:213–28. https://doi.org/10.1148/rg.331125092A review of the appearance of DCIS on ultrasound.
Watanabe T, Yamaguchi T, Tsunoda H, et al. Ultrasound image classification of ductal carcinoma in situ (DCIS) of the breast: analysis of 705 DCIS lesions. Ultrasound Med Biol. 2017;43:918–25. https://doi.org/10.1016/j.ultrasmedbio.2017.01.008.
• Mesurolle B, El-Khoury M, Khetani K, Abdullah N, Joseph L, Kao E. Mammographically non-calcified ductal carcinoma in situ: sonographic features with pathological correlation in 35 patients. Clin Radiol. 2009;64:628–36. https://doi.org/10.1016/j.crad.2008.12.013Unique ultrasound presentation of DCIS.
Moon HJ, Kim EK, Kim MJ, Yoon JH, Park VY. Comparison of clinical and pathologic characteristics of ductal carcinoma in situ detected on mammography versus ultrasound only in asymptomatic patients. Ultrasound Med Biol. 2019;45:68–77. https://doi.org/10.1016/j.ultrasmedbio.2018.09.003.
Moon WK, Im JG, Koh YH, Noh DY, Park IA. US of mammographically detected clustered microcalcifications. Radiology. 2000;217:849–54. https://doi.org/10.1148/radiology.217.3.r00nv27849.
Yu PC, Lee YW, Chou FF, et al. Clustered microcalcifications of intermediate concern detected on digital mammography: ultrasound assessment. Breast. 2011;20:495–500. https://doi.org/10.1016/j.breast.2011.05.003.
Moon WK, Myung JS, Lee YJ, Park IA, Noh DY, Im JG. US of ductal carcinoma in situ. Radiographics. 2002;22:269–80; discussion 280-261. https://doi.org/10.1148/radiographics.22.2.g02mr16269.
Soo MS, Baker JA, Rosen EL. Sonographic detection and sonographically guided biopsy of breast microcalcifications. AJR Am J Roentgenol. 2003;180:941–8. https://doi.org/10.2214/ajr.180.4.1800941.
•• Kuhl CK, Schrading S, Bieling HB, et al. MRI for diagnosis of pure ductal carcinoma in situ: a prospective observational study. Lancet. 2007;370:485–92. https://doi.org/10.1016/S0140-6736(07)61232-XDemonstrates the excellent sensitivity of MRI for the detection of DCIS, using modern MRI equipment.
Lehman CD, Gatsonis C, Kuhl CK, et al. MRI evaluation of the contralateral breast in women with recently diagnosed breast cancer. N Engl J Med. 2007;356:1295–303. https://doi.org/10.1056/NEJMoa065447.
Berg WA, Gutierrez L, NessAiver MS, et al. Diagnostic accuracy of mammography, clinical examination, US, and MR imaging in preoperative assessment of breast cancer. Radiology. 2004;233:830–49. https://doi.org/10.1148/radiol.2333031484.
Marcotte-Bloch C, Balu-Maestro C, Chamorey E, et al. MRI for the size assessment of pure ductal carcinoma in situ (DCIS): a prospective study of 33 patients. Eur J Radiol. 2011;77:462–7. https://doi.org/10.1016/j.ejrad.2009.09.003.
Proulx F, Correa JA, Ferre R, et al. Value of pre-operative breast MRI for the size assessment of ductal carcinoma in situ. Br J Radiol. 2016;89:20150543. https://doi.org/10.1259/bjr.20150543.
• Pickles MD, Gibbs P, Hubbard A, Rahman A, Wieczorek J, Turnbull LW. Comparison of 3.0 T magnetic resonance imaging and X-ray mammography in the measurement of ductal carcinoma in situ: a comparison with histopathology. Eur J Radiol. 2015;84:603–10. https://doi.org/10.1016/j.ejrad.2014.12.016Improved estimates of the extent of disease using 3T MRI systems compared to mammography.
Rahbar H, DeMartini WB, Lee AY, Partridge SC, Peacock S, Lehman CD. Accuracy of 3 T versus 1.5 T breast MRI for pre-operative assessment of extent of disease in newly diagnosed DCIS. Eur J Radiol. 2015;84:611–6. https://doi.org/10.1016/j.ejrad.2014.12.029.
Jansen SA, Newstead GM, Abe H, Shimauchi A, Schmidt RA, Karczmar GS. Pure ductal carcinoma in situ: kinetic and morphologic MR characteristics compared with mammographic appearance and nuclear grade. Radiology. 2007;245:684–91. https://doi.org/10.1148/radiol.2453062061.
Menell JH, Morris EA, Dershaw DD, Abramson AF, Brogi E, Liberman L. Determination of the presence and extent of pure ductal carcinoma in situ by mammography and magnetic resonance imaging. Breast J. 2005;11:382–90. https://doi.org/10.1111/j.1075-122X.2005.00121.x.
Rosen EL, Smith-Foley SA, DeMartini WB, Eby PR, Peacock S, Lehman CD. BI-RADS MRI enhancement characteristics of ductal carcinoma in situ. Breast J. 2007;13:545–50. https://doi.org/10.1111/j.1524-4741.2007.00513.x.
Buadu LD, Murakami J, Murayama S, et al. Breast lesions: correlation of contrast medium enhancement patterns on MR images with histopathologic findings and tumor angiogenesis. Radiology. 1996;200:639–49. https://doi.org/10.1148/radiology.200.3.8756909.
Jansen SA, Paunesku T, Fan X, et al. Ductal carcinoma in situ: X-ray fluorescence microscopy and dynamic contrast-enhanced MR imaging reveals gadolinium uptake within neoplastic mammary ducts in a murine model. Radiology. 2009;253:399–406. https://doi.org/10.1148/radiol.2533082026.
D’Orsi CJSE, Mendelson EB, Morris EA, et al. ACR BI-RADS® atlas, breast imaging reporting and data system. Reston: American College of Radiology; 2013.
Tozaki M, Igarashi T, Fukuda K. Breast MRI using the VIBE sequence: clustered ring enhancement in the differential diagnosis of lesions showing non-masslike enhancement. AJR Am J Roentgenol. 2006;187:313–21. https://doi.org/10.2214/ajr.05.0881.
Esserman LJ, Kumar AS, Herrera AF, et al. Magnetic resonance imaging captures the biology of ductal carcinoma in situ. J Clin Oncol. 2006;24:4603–10. https://doi.org/10.1200/JCO.2005.04.5518.
Baur A, Bahrs SD, Speck S, et al. Breast MRI of pure ductal carcinoma in situ: sensitivity of diagnosis and influence of lesion characteristics. Eur J Radiol. 2013;82:1731–7. https://doi.org/10.1016/j.ejrad.2013.05.002.
Liu H, Peng W. MRI morphological classification of ductal carcinoma in situ (DCIS) correlating with different biological behavior. Eur J Radiol. 2012;81:214–7. https://doi.org/10.1016/j.ejrad.2010.12.084.
Fancellu A, Turner RM, Dixon JM, Pinna A, Cottu P, Houssami N. Meta-analysis of the effect of preoperative breast MRI on the surgical management of ductal carcinoma in situ. Br J Surg. 2015;102:883–93. https://doi.org/10.1002/bjs.9797.
• Lehman CD, Gatsonis C, Romanoff J, et al. Association of magnetic resonance imaging and a 12-gene expression assay with breast ductal carcinoma in situ treatment. JAMA Oncol. 2019. https://doi.org/10.1001/jamaoncol.2018.6269A prospective multi-center trial demonstrating that MRI alone accounts for a minority of conversion to mastectomy.
Luo J, Hippe DS, Rahbar H, Parsian S, Rendi MH, Partridge SC. Diffusion tensor imaging for characterizing tumor microstructure and improving diagnostic performance on breast MRI: a prospective observational study. Breast Cancer Res. 2019;21:102. https://doi.org/10.1186/s13058-019-1183-3.
Balleyguier C, Dunant A, Ceugnart L, et al. Preoperative breast magnetic resonance imaging in women with local ductal carcinoma in situ to optimize surgical outcomes: results from the randomized phase III trial IRCIS. J Clin Oncol. 2019;37:885–92. https://doi.org/10.1200/JCO.18.00595.
Esserman L, Yau C. Rethinking the standard for ductal carcinoma in situ treatment. JAMA Oncol. 2015;1:881–3. https://doi.org/10.1001/jamaoncol.2015.2607.
Chou SS, Gombos EC, Chikarmane SA, Giess CS, Jayender J. Computer-aided heterogeneity analysis in breast MR imaging assessment of ductal carcinoma in situ: correlating histologic grade and receptor status. J Magn Reson Imaging. 2017;46:1748–59. https://doi.org/10.1002/jmri.25712.
Luo J, Johnston BS, Kitsch AE, et al. Ductal carcinoma in situ: quantitative preoperative breast MR imaging features associated with recurrence after treatment. Radiology. 2017;285:788–97. https://doi.org/10.1148/radiol.2017170587.
Grimm LJ, Hwang ES. Active surveillance for DCIS: the importance of selection criteria and monitoring. Ann Surg Oncol. 2016;23:4134–6. https://doi.org/10.1245/s10434-016-5596-2.
Kuerer HM. Ductal carcinoma in situ: treatment or active surveillance? Expert Rev Anticancer Ther. 2015;15:777–85. https://doi.org/10.1586/14737140.2015.1043897.
Comparison of operative versus medical endocrine therapy for LOw Risk DCIS: the COMET Trial. In: Patient-Centered Outcomes Research Institute.
LORIS A phase III trial of surgery versus active monitoring for low risk ductal carcinoma in situ (DCIS). In: University of Birmingham.
Management of LOw-Risk DCIS (LORD). In: The Netherlands Cancer Institute.
Grimm LJ, Ryser MD, Partridge AH, et al. Surgical upstaging rates for vacuum assisted biopsy proven DCIS: implications for active surveillance trials. Ann Surg Oncol. 2017;24:3534–40. https://doi.org/10.1245/s10434-017-6018-9.
Soumian S, Verghese ET, Booth M, et al. Concordance between vacuum assisted biopsy and postoperative histology: implications for the proposed LOw Risk DCIS Trial (LORIS). Eur J Surg Oncol. 2013;39:1337–40. https://doi.org/10.1016/j.ejso.2013.09.028.
Aminololama-Shakeri S, Flowers CI, McLaren CE, et al. Can radiologists predict the presence of ductal carcinoma in situ and invasive breast cancer? AJR Am J Roentgenol. 2017;208:933–9. https://doi.org/10.2214/AJR.16.16073.
•• Shi B, Grimm LJ, Mazurowski MA, et al. Can occult invasive disease in ductal carcinoma in situ be predicted using computer-extracted mammographic features? Acad Radiol. 2017;24:1139–47. https://doi.org/10.1016/j.acra.2017.03.013The first study to apply deep learning techniques to the task of predicting upstaging of DCIS to invasive cancer.
Hwang E, Duong S, Bedrosian I, et al. Abstract GS5-05: primary endocrine therapy for ER-positive ductal carcinoma in situ (DCIS) CALGB 40903 (Alliance). Cancer Research. 2018;78:GS5-05-GS05-05. https://doi.org/10.1158/1538-7445.Sabcs17-gs5-05.
Shi B, Grimm LJ, Mazurowski MA, et al. Prediction of occult invasive disease in ductal carcinoma in situ using deep learning features. J Am Coll Radiol. 2018;15:527–34. https://doi.org/10.1016/j.jacr.2017.11.036.
Harowicz MR, Saha A, Grimm LJ, et al. Can algorithmically assessed MRI features predict which patients with a preoperative diagnosis of ductal carcinoma in situ are upstaged to invasive breast cancer? J Magn Reson Imaging. 2017;46:1332–40. https://doi.org/10.1002/jmri.25655.
Funding
R01CA203883 (Rahbar)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Habib Rahbar reports grants from National Cancer Institute during the conduct of the study. Lars Grimm reports grants from Alliance Foundation Trial outside the submitted work. Nancy Ballantyne and Yun An Chen declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Disclaimer
The funders had no role in the manuscript design, data analysis, decision to publish, or preparation of the manuscript.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Nancy Ballantyne and Yun An Chen are co-first authors.
This article is part of the Topical Collection on Non-Invasive Breast Cancer Diagnosis and Treatment
Rights and permissions
About this article
Cite this article
Ballantyne, N., Chen, Y.A., Rabhar, H. et al. Multimodality Imaging of Ductal Carcinoma In Situ. Curr Breast Cancer Rep 12, 26–35 (2020). https://doi.org/10.1007/s12609-019-00349-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12609-019-00349-9