Abstract
Purpose of Review
The aim of this review is to give an overall idea of Cryptococcus biology paying special attention to its capacity to adapt through its morphogenetic program to the hostile host environment. This morphogenetic program consists of a significant increase in capsule size and the formation of Titan cells.
Recent Findings
Research on Titan cells had been hampered by the need of obtaining these cells from the lungs of infected mice. The production of Titan cells in vitro has supposed a major step in understanding the role of this morphotype in the virulence of Cryptococcus.
Summary
In this regard, Cryptococcus has acquired the capacity of inducing a heterogeneous population during infection that allows it to evade the host immune system attack, proliferate, and disseminate to the CNS where it produces meningoencephalitis which is fatal if not treated properly.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cryptococcosis is a systemic disease caused by yeasts that belong to the genus Cryptococcus. Despite its high prevalence in immunocompromised patients especially in HIV-positive individuals in sub-Saharan Africa, and its high associated mortality rate, it is somehow a forgotten disease. In this review, we aim to offer the reader an overview of Cryptococcus biology, focusing on its main phenotypic characteristics and paying special attention to its unique morphological program during interaction with hosts.
Cryptococcus and Cryptococcosis
Cryptococcus is included in the Basidiomycota division and contains at least 40 species, out of which, Cryptococcus neoformans and Cryptococcus gattii are the most frequent causative agents of cryptococcosis [1]. The most common clinical presentation of the disease is a pulmonary infection and further dissemination to the central nervous system producing meningitis. The most important phenotypic characteristic in C. neoformans and C. gattii is the presence of a capsule that surrounds the cell body.
Initially, C. neoformans and C. gattii were classified as one species and were distinguished by their antigenic differences. However, the discovery of two different teleomorphs together with whole-genome sequence data lead to the recognition of C. neoformans and C. gattii as two different species. More recently, it was proposed to classify C. neoformans in two different species, and C. gattii in five different species [2]. Although no consensus among the scientific community has been yet achieved [3].
Cryptococcus neoformans and C. gattii share many characteristics but the type of infection and their epidemiology are different. In this section, we will briefly review the main characteristics of each species. In the rest of this review, we will focus on C. neoformans, unless otherwise is stated.
Cryptococcus neoformans
Cryptococcus neoformans infects mainly immunosuppressed individuals. The principal risk factor associated with this pathogen is advanced HIV. Other risk factors are organ transplantation and receipt of immunosuppressive medications (e.g., corticosteroids). This yeast is cosmopolitan, with worldwide distribution, and can be isolated from multiple sources including pigeon excreta and soil [1].
Cryptococcus neoformans is typically acquired by inhalation of spores, and therefore, the lungs are usually the first organs to be colonized. In immunocompetent individuals, the infection is almost always controlled by the host immune system. However, in immunosuppressed individuals, especially those with reduced numbers of T cells such as those with advanced HIV, C. neoformans can induce an invasive infection with dissemination through the blood vessels to preferentially the central nervous system, where it causes meningoencephalitis with a high associated mortality rate if not treated properly.
The incidence of cryptococcal meningoencephalitis has decreased thanks to the availability of the effective HIV therapy, but continues being high with an estimated > 223,100 new cases per year that resulted in 181,100 deaths in 2014 [4••]. Cryptococcal disease remains a leading cause of mortality in developing countries, where access to antiretroviral therapy is limited and HIV prevalence is high [5].
Cryptococcus gattii
Initial studies suggested that C. gattii was predominantly found in tropical and subtropical areas [6]. However, more recent studies show that C. gattii has a much more widespread distribution and is often associated with eucalyptus trees [7].
Similar to C. neoformans, C. gattii is acquired by inhalation. However, C. gattii and C. neoformans are genetically and biochemically different. Cryptococcus gattii infects both immunocompromised and immunocompetent individuals [8]. In some countries, such as in Brazil, C. gattii is endemic and responsible for the 60% of all cryptococcosis infections [9].
The most characteristic clinical outcome is pneumonia. Only a minority of cases develop meningitis, and often as a result of some immunodeficiency [10, 11].
Despite C. gattii infections constitute only 1% of the worldwide cryptococcosis cases, this species gained importance for the scientific community and health professionals starting around 1999 due to an outbreak of infection in Vancouver Island, Canada [12].
Host Interaction
The interaction of Cryptococcus with the host immune system is very complex and has been widely studied [13]. Cryptococccus has developed different strategies that allow him to survive within the host, produce damage, and disseminate preferentially to the central nervous system [14••].
Intracellular Lifestyle
The first site of infection is the lungs where cryptocococcal cells encounter resident macrophages. The outcome of this interaction determines the course of infection [15, 16].
Macrophages and neutrophils are the frontline of the immune system defense of the host. The phagocytosis process depends on the activation of phagocytic receptors that can be divided in opsonic and non-opsonic.
Early studies proved that phagocytosis was inhibited by the capsule, and that acapsular mutants were easily phagocytosed [17]. The phagocytosis can be mediated through the union of phagocytic receptors located on macrophages’ surface and the epitopes located at cryptococcal cell wall (non-opsonic mechanisms). Therefore, the capsule impairs the recognition of these epitopes and thus, inhibits the phagocytosis [18]. Interestingly, the C-type lectin Dectin-2 recognizes the mannans at the cell wall and induces a non-protective Th2 response [19]. Besides, other antiphagocytic mechanisms that do not depend on the capsule have been described, such as the secretion of the antiphagocytic protein App1 [20, 21] and the transcription regulator Gat201 [22].
Phagocytosis can also be antibody/complement mediated (opsonic mechanism) and it depends on capsule size and on the location of the complement binding protein [23]. Despite all these mechanisms, Cryptococcus is phagocytosed in vivo. Cryptococcus is found predominantly within macrophages few hours after the infection [24]. After phagocytosis, an antimicrobial environment is produced in the phagosomes, which includes the production of reactive oxygen (ROS) and nitrogen species (NOS), alteration of pH, production of antimicrobial peptides, and limitation of nutrients in an attempt to kill Cryptococcus [25, 26]. The killing of the fungus is one of the possible outcomes; however, Cryptococcus can survive within the macrophage, proliferate, and eventually lyse the macrophages [27].
Macrophage activation occurs through distinct types of immune response: pro-inflammatory Th1 and Th17 responses and anti-inflammatory Th2 response. During Cryptococcus infection, the Th1 and Th17 responses lead to a protective response while the Th2 is associated with exacerbation of disease, supporting intracellular survival and cryptococcal proliferation [28••, 29•, 30]. Interestingly, Cryptococcus virulence factors such as the polysaccharide capsule, melanin and urease production, and the formation of Titan cells promote a dominant anti-inflammatory Th2 response, decreasing significantly the production of inflammatory cytokines and facilitating the intracellular survival and proliferation of the fungus [31, 32•, 33, 34].
If macrophage attack is evaded, Cryptococcus is able to proliferate within the phagosome where nutrient uptake is of great importance. Iron, for example, is an extremely important nutrient to the fungus. Indeed, low levels of iron within macrophages induce morphological changes in Cryptococcus such as capsule enlargement, Titan cells formation, and melanin production. Besides, Cryptococcus increases the expression of a siderophore iron transporter (SIT1) and of an iron permease (FTR1) that allow the fungus to increase its iron storage and survive [35, 36].
Cryptococcus can lyse the macrophages and evade killing. The mechanisms involved in this process remain poorly known. It is hypothesized that Cryptococcus can mechanically lyse the cells by simple proliferation or by an exaggerated production of polysaccharide. Besides, it is known that Cryptococcus can induce the apoptosis of the host cells via the alternative NF-kB pathway [37].
Interestingly, Cryptococcus has developed different ways to exit the macrophages without lysing them, such as lateral transfer to another macrophage and “vomocytosis” that is a non-lytic process of expulsion of the yeast from macrophages, allowing Cryptococcus to disseminate without inducing local inflammation [16, 38].
Dissemination to the Central Nervous System
Dissemination to the central nervous system (CNS) causing cryptococcal meningitis is a major cause of HIV-related deaths worldwide [39].
Cryptococcus has developed different strategies that allow it to cross the blood-brain barrier (BBB). One of these strategies is the so-called “Trojan horse” mechanism, by which Cryptococcus can cross the BBB inside macrophages [40, 41]. Cryptococcus can also directly invade the BBB and enter in the brain tissue by a mechanism called transcytosis [42, 43]. In this process, Cryptococcus induces the formation of microvillus-like membrane protrusions in the BBB cells, where it adheres and gets internalized reaching the brain parenchyma without affecting the integrity of the host cells [44]. Recently, Aaron et al. found that the EPH-EphrinA1 (EphA2) tyrosine kinase receptor-signaling pathway mediates the transcytosis across the BBB in a CD44 host receptor dependent manner [45]. Therefore, silencing or inhibiting EphA2 prevents Cryptococcus from crossing the BBB.
However, Cryptococcus can reach the CNS producing damage to the endothelial cells that compose the BBB by altering their cytoskeleton, which has been named paracellular penetration [46,47,48]. Indeed, Cryptococcus urease enzyme also plays a role in its dissemination, since urease-deficient strains are less efficient in transmigrating the BBB. It is hypothesized that urease degradation produces ammonia that can damage the endothelium and increase the permeability of Cryptococcus through the BBB or that cryptococcal urease possesses substrate specificity that facilitates the transcytosis [49, 50].
Interestingly, none of these mechanisms are mutually exclusive, and indeed there are increasing evidences that all of them contribute to the invasion and colonization of the central nervous system.
Latency and Reactivation
Besides causing disseminated infection in immunocompromised patients, Cryptococcus can also cause a latent asymptomatic infection and stay in the host for long periods of time. Epidemiological studies have revealed patients in which these latent cells could restart infection under adequate stimuli [51].
Little is known about the mechanisms involved in the latency/reactivation of Cryptococcus. When in experimental latency, Cryptococcus displays low or almost undetectable metabolism being able to enhance its metabolic activity under favored conditions. In vivo, rats are the best models to study latency of Cryptococcus, since they are intrinsically resistant to cryptococcosis. In this model, yeasts are not eliminated and a chronic infection is developed with the formation of granulomas where Cryptococcus is found mostly inside macrophages [52, 53].
Virulence Determinants
Cryptococcus spp. are yeasts of special interest to study fungal pathogenesis since they have developed different adaptation mechanisms to the host but also virulence factors, which are defined as those that produce damage to the host.
Melanin
Production of melanin is one of the most characteristic features of Cryptococcus. Melanin is a negatively charged dark pigment, hydrophobic, and extensively spread in the environment. There are different types of melanin: eumelanins, pheomelanin, alomelanins, and piomelanins. In particular, Cryptococcus synthesizes eumelanin using diphenol, aminophenol, and diaminobenzene compounds as substrates [54]. Some of these compounds, such as L-DOPA, are present in the central nervous system, and therefore, it is thought that melanization confers an adaptative advantage to infect that organ [55].
Melanin is synthesized by a phenoloxidase enzyme called laccase encoded by LAC1 gene [56]. The expression of this gene is regulated by the ion, cupper, and glucose concentration [57, 58]. Laccase enzyme is located at the cell wall and it is important for Cryptococcus survival since it contributes to keep its cell wall integrity.
Melanin protects Cryptococcus from stress factors such as UV, free radicals, and high temperature, which facilitate its survival in the host. Furthermore, in mice, infection of melanin particles induces an inflammatory response, suggesting that this pigment could modulate the immune response and therefore it could have an important role in virulence.
Growth at 37 °C, Adaptation to Alkaline pH, and Expression of Urease and Phospholipases Enzymes
The capacity to grow at 37 °C is essential for any human pathogen. Cryptococcus is able to grow at a wide range of temperatures, from 25 until 37 °C. Therefore, it can infect both environmental hosts and mammals.
In the environment, Cryptococcus is found in pigeon excreta. However, birds do not get infected, probably because their body temperature is around 40–42 °C.
In the last years, many proteins required for growing at 37 °C have been identified. These proteins are involved in stress response, cell wall assembly, plasma membrane integrity, basal metabolism, and polarized growth [59,60,61,62].
Once in the lungs, Cryptococcus has to adapt to an alkaline environment. To accomplish that, the Rim alkaline response pathway is activated which leads to expression of Rim101 that directly regulates genes required for various stress responses including low iron, high salt concentration, and proper cell wall maintenance [63,64,65].
Another characteristic of Cryptococcus is the expression of a urease enzyme, which allows it to use exogenous sources of urea. Urease is important for Cryptococcus virulence because it promotes dissemination to the central nervous system [49, 66] and a Th2 response, impairing the elimination of the yeasts. More recently, it has been described how urease alters phagolysosomes, delaying intracellular replication and thus facilitating Cryptococcus dissemination when transported within macrophages to the central nervous system [67].
Finally, two phospholipases B (Plb1 and Plb2) and a phospholipase C have been associated with survival, maintenance of the homeostasis, and intracellular replication of Cryptococcus within macrophages in vitro [68,69,70]. In parallel, another phospholipase with only lysophospholipase activity has been characterized in C. gattii, which could help to understand the differences in virulence in these two species [71].
Capsule
The polysaccharide capsule is the main phenotypic characteristic of Cryptococcus. This structure can be easily observed when yeasts are suspended in India ink as refringent white halo. The capsule confers Cryptococcus protection against phagocytic cells and also interferes with the host immune system. Indeed, the capsule is its principal virulence factor and therefore it is the most studied structure of this pathogen. Apart from its contribution to virulence, the capsule is important medically since its polysaccharide (PS) is the cryptococcal antigen used in diagnosis [72].
When observed in India ink suspension, the capsule looks a homogenous structure. However, it exhibits different densities in different regions being the inner layer denser, more rigid, and less permeable than the outer layer [73,74,75].
The polysaccharide is composed approximately 90% of glucuronoxylomannan (GXM) formed by a (1,3) mannose backbone with ß(1,2) and ß(1,4) xylose and ß(1,2) glucuronic acid substitutions [76]. The other two minor components of the capsule are GalXM and mannoproteins [77, 78]. In addition to the PS components, the capsule contains lipid structures whose function is unknown [79, 80].
Cryptococcus capsule is a key component for its atypical morphogenetic program, which will be extensively reviewed in the following section.
Morphogenesis
Unlike other well-known fungi that transition from a yeast form to an invasive filament form, such as Candida albicans, Cryptococcus does not change its shape, but its size. This morphological transition is important regarding adhesion, invasion, dissemination, and evasion of the immune system [81••].
Cryptococcus only forms filaments during sexual reproduction although pseudohyphae have occasionally been observed in tissues [82]. However, Cryptococcus is characterized by inducing other types of changes during infection that involve exclusively a change in size. Cryptococcus can increase its size in two different ways: by increasing only the size of the capsule or by increasing both capsule and the cell body sizes. These changes produce a very heterogeneous yeast population in the lungs, which contribute to evade the immune response.
Changes in Capsule Size
The increase in capsule size of Cryptococcus is one of the most characteristic features and can be observed in vitro in different media [83, 84]. In rich media, the size of the capsule is around 1–2 μm but there are conditions that induce a drastic increase in size. This phenomenon was first described in the 50s. Afterwards, it was shown that CO2 and iron limitation induce the growth of the capsule [85, 86]. More recently, other factors that induce this process have been described, such as mammalian serum, medium with low concentration of nutrients at neutral pH, or mannitol [83, 84, 87]. Conversely, other factors such as osmotic pressure or high glucose concentrations reduce the size of the capsule. Little is known about the regulation and the molecular mechanisms responsible for this process [88]. However, there is a correlation between ex vivo capsule size and the intracranial pressure of patients [89].
The growth of the capsule occurs mainly in the G1 phase of the cell cycle [90]. It has been shown that the increase in size of the capsule requires the accumulation of a significant amount of new polysaccharide [91, 92]. It has been estimated that the weight increase of the cells due to the growth of the capsule is about 20% of the total weight of the cells and this process occurs in a few hours being an energy-cost process for the cell [74, 93], which is particularly interesting because it occurs in nutrient-limiting conditions. The capsule growth is one of the first responses of Cryptococcus after reaching the lungs, and thus, it is considered an early morphological response [94]. Cells with larger capsules are more resistant to stress factors, such as free radicals or antimicrobial peptides [26], so it has been postulated that it is a mechanism that allows the survival of Cryptococcus within macrophages [23].
Formation of Titan Cells
Another characteristic change of Cryptococcus occurs when there is massive growth of the capsule and the cell body. In this way, blastoconidia of a total size greater than 30 μm can be formed and those are called “Titan cells,” although these cells can reach up to 70 μm in vivo [94,95,96,97]. This change is considered a late morphological response, since these cells are observed several days after the infection. These cells were described in clinical samples [98] but had not been extensively characterized until 2010 [95, 96]. Titan cells are polyploid, have a thickened cell wall, and have a denser capsule than normal-sized cryptococcal cells. In addition, these cells can proliferate and have a progeny of normal size [99, 100]. Both, Titan cells and their progeny, are more resistant to stress factors, which provide a mechanism of adaptation to the host and evasion of the immune response. Recent studies have shown differences in mannose content and the distribution of specific epitopes in Cryptcoccus neoformans capsule [101, 102].
The main pathway that has been linked to the formation of Titan cells is signaling through cAMP since mutants of adenylate cyclase do not form these cells [96]. In this way, two receptors coupled to G proteins that are important for the induction of Titan cells have been described: Ste3a (pheromone receptor α) and Grp5 protein. Both receptors control the formation of Titan cells through the elements of the cAMP pathway. The signaling by this metabolite regulates the activation of the PKA-regulated Rim101 transcription factor that is necessary to induce Titan cell formation [103]. Interestingly, mutants of phospholipase B1 that show a clear defect in intracellular proliferation can form Titan cells within macrophages, which could be a strategy to survive within the host [104].
Host Factors Involved in Titan Cell Formation
Little is known about the function of Titan cells during infection and which host factors regulate this morphological transition. Titan cells contribute to the permanence of the yeast in the lungs since they cannot be phagocytosed nor be eliminated easily. In addition, they inhibit the phagocytosis of other cells of regular size and induce a Th2 type immune response [105, 106]. It has been shown that the proportion of this type of cells is particularly high in models of asymptomatic infection, which suggests that these cells participate in the latency phase of the infection [96]. Interestingly, it has been observed that a Th2-polarization of the immune response correlates with a higher proportion of Titan cells in the lungs [33]. Furthermore, the proportion of these cells increases when co-infections are made with strains of MATa and MATα sexual alleles, which indicates that the sexual type plays an important role in the induction of Titan cells [95].
What Happens In Vitro?
One of the major limitations to investigate Titan cells is the difficulty of reproducing this phenomenon in vitro. However, last year, three independent groups published in the same journal different in vitro conditions that result in the appearance of Titan cells [107•, 108•, 109•]. Despite that the in vitro Titan cells do not reach the size of the titan cells found in the lungs of infected mice, they have an average cell body size of 15 μm and share many phenotypic characteristics with the in vivo Titan cells. Briefly, Trevijano-Contador et al and Dambuza et al agree on the importance of incubation in limited nutrient conditions containing serum for an overnight at 37 °C in a CO2 enriched environment and at a low cell density. However, Hommel et al describe a protocol where longer incubations up to 120 h are required and no presence of serum nor of CO2-enriched environment is necessary [107•, 108•, 109•], showing that multiple pathways may be involved in this morphological change during Cryptococcus infection. For a more detailed comparison and analysis of the three protocols to induce Titan cells in vitro, we suggest the reading of this very recent review [110••].
Conclusions
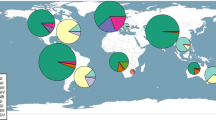
Cryptococcus has developed different strategies to survive and proliferate within the host. Its intracellular lifestyle together with its capacity to undergo a complex morphological program constitutes the main characteristics of this fungal pathogen (as represented in Fig. 1). Little is known about the molecular mechanisms involved in some of the processes described above. Research on this field has been complicated due to the difficulties of performing molecular modifications on Cryptococcus. However, in the last years there have been several important additions to the molecular toolbox of Cryptococcus that for sure will enable deeper studies at the molecular and cellular level. Furthermore, the recent discovery of the conditions for producing Titan cells in vitro will enlarge the knowledge of this peculiar morphogenetic transition and their full consequences for the development of the infection and the immune response of the host.
Infection, intracellular lifestyle, and dissemination of Cryptococcus. The lungs are the first site of infection, where alveolar macrophages phagocytose yeast cells (I). However, Cryptococcus can also become a Titan cell, increasing its body and/or capsule size, outside the macrophage and impair its phagocytosis (II). If phagocytosis does occur, then Cryptococcus cells undergo morphological changes such as capsule enlargement, transition to Titan cell, and melanin production that protect against different stresses elicited by the macrophage (III). These morphological changes lead to a dominant anti-inflammatory non-protective Th2 immune response in the macrophages (IV). In this permissive environment, Cryptococcus can replicate intracellularly (V) and different outcomes are possible: Yeast cells can exit the macrophage without lysing it, a process named “vomocytosis” (VI), Cryptococcus can be transfered to a second non-infected macrophage by lateral transfer (VII) or lyse the macrophage and exit to the extracellular environment (VIII). All of these outcomes contribute not only to the establishment of the infection but also to the dissemination. Furthermore, depending the immunological response achieved by the host, Cryptococcus can reduce its metabolism and enter a state of latency (IX), from which infection can be reactivated under more favorable conditions for Cryptococcus proliferation (X)
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Casadevall A, Perfect J. Cryptococcus neoformans. Washington DC: ASM; 1998.
Hagen F, Khayhan K, Theelen B, Kolecka A, Polacheck I, Sionov E, et al. Recognition of seven species in the Cryptococcus gattii/Cryptococcus neoformans species complex. Fungal Genet Biol: FG & B. 2015;78:16–48. https://doi.org/10.1016/j.fgb.2015.02.009.
Kwon-Chung KJ, Bennett JE, Wickes BL, Meyer W, Cuomo CA, Wollenburg KR, et al. The case for adopting the “species complex” nomenclature for the etiologic agents of cryptococcosis. mSphere. 2017;2(1). https://doi.org/10.1128/mSphere.00357-16.
•• Rajasingham R, Smith RM, Park BJ, Jarvis JN, Govender NP, Chiller TM, et al. Global burden of disease of HIV-associated cryptococcal meningitis: an updated analysis. Lancet Infect Dis. 2017;17(8):873–81. https://doi.org/10.1016/S1473-3099(17)30243-8 . Update on the global burden of cryptococcosis cases.
Jarvis JN, Harrison TS. HIV-associated cryptococcal meningitis. Aids. 2007;21(16):2119–29. https://doi.org/10.1097/QAD.0b013e3282a4a64d.
Kwon-Chung KJ, Bennett JE. Epidemiologic differences between the two varieties of Cryptococcus neoformans. Am J Epidemiol. 1984;120(1):123–30.
Ellis DH, Pfeiffer TJ. Natural habitat of Cryptococcus neoformans var. gattii. J Clin Microbiol. 1990;28(7):1642–4.
Sorrell TC. Cryptococcus neoformans variety gattii. Med Mycol. 2001;39(2):155–68.
Nishikawa MM, Lazera MS, Barbosa GG, Trilles L, Balassiano BR, Macedo RC, et al. Serotyping of 467 Cryptococcus neoformans isolates from clinical and environmental sources in Brazil: analysis of host and regional patterns. J Clin Microbiol. 2003;41(1):73–7.
Harris JR, Lockhart SR, Debess E, Marsden-Haug N, Goldoft M, Wohrle R, et al. Cryptococcus gattii in the United States: clinical aspects of infection with an emerging pathogen. Clin Infect Dis : Off Publ Infect Dis Soc Am. 2011;53(12):1188–95.
Ngamskulrungroj P, Chang Y, Sionov E, Kwon-Chung KJ. The primary target organ of Cryptococcus gattii is different from that of Cryptococcus neoformans in a murine model. mBio. 2012;3(3).
Hoang LM, Maguire JA, Doyle P, Fyfe M, Roscoe DL. Cryptococcus neoformans infections at Vancouver Hospital and Health Sciences Centre (1997-2002): epidemiology, microbiology and histopathology. J Med Microbiol. 2004;53(Pt 9):935–40.
Vecchiarelli A, Pericolini E, Gabrielli E, Kenno S, Perito S, Cenci E, et al. Elucidating the immunological function of the Cryptococcus neoformans capsule. Future Microbiol. 2013;8(9):1107–16. https://doi.org/10.2217/fmb.13.84.
•• Esher SK, Zaragoza O, Alspaugh JA. Cryptococcal pathogenic mechanisms: a dangerous trip from the environment to the brain. Mem Inst Oswaldo Cruz. 2018;113(7):e180057. https://doi.org/10.1590/0074-02760180057 Detailed description of the establishment of Cryptococcus infection.
Garcia-Rodas R, Zaragoza O. Catch me if you can: phagocytosis and killing avoidance by Cryptococcus neoformans. FEMS Immunol Med Microbiol. 2012;64(2):147–61.
Johnston SA, May RC. Cryptococcus interactions with macrophages: evasion and manipulation of the phagosome by a fungal pathogen. Cell Microbiol. 2013;15(3):403–11. https://doi.org/10.1111/cmi.12067.
Kozel TR, Gotschlich EC. The capsule of Cryptococcus neoformans passively inhibits phagocytosis of the yeast by macrophages. J Immunol. 1982;129(4):1675–80.
Small JM, Mitchell TG. Strain variation in antiphagocytic activity of capsular polysaccharides from Cryptococcus neoformans serotype A. Infect Immun. 1989;57(12):3751–6.
Nakamura Y, Sato K, Yamamoto H, Matsumura K, Matsumoto I, Nomura T, et al. Dectin-2 deficiency promotes Th2 response and mucin production in the lungs after pulmonary infection with Cryptococcus neoformans. Infect Immun. 2015;83(2):671–81. https://doi.org/10.1128/IAI.02835-14.
Luberto C, Martinez-Marino B, Taraskiewicz D, Bolanos B, Chitano P, Toffaletti DL, et al. Identification of App1 as a regulator of phagocytosis and virulence of Cryptococcus neoformans. J Clin Invest. 2003;112(7):1080–94.
Stano P, Williams V, Villani M, Cymbalyuk ES, Qureshi A, Huang Y, et al. App1: an antiphagocytic protein that binds to complement receptors 3 and 2. J Immunol. 2009;182(1):84–91.
Chun CD, Brown JC, Madhani HD. A major role for capsule-independent phagocytosis-inhibitory mechanisms in mammalian infection by Cryptococcus neoformans. Cell Host Microbe. 2011;9(3):243–51.
Zaragoza O, Taborda CP, Casadevall A. The efficacy of complement-mediated phagocytosis of Cryptococcus neoformans is dependent on the location of C3 in the polysaccharide capsule and involves both direct and indirect C3-mediated interactions. Eur J Immunol. 2003;33(7):1957–67.
Feldmesser M, Kress Y, Novikoff P, Casadevall A. Cryptococcus neoformans is a facultative intracellular pathogen in murine pulmonary infection. Infect Immun. 2000;68(7):4225–37.
Brown SM, Campbell LT, Lodge JK. Cryptococcus neoformans, a fungus under stress. Curr Opin Microbiol. 2007;10(4):320–5. https://doi.org/10.1016/j.mib.2007.05.014.
Zaragoza O, Chrisman CJ, Castelli MV, Frases S, Cuenca-Estrella M, Rodriguez-Tudela JL, et al. Capsule enlargement in Cryptococcus neoformans confers resistance to oxidative stress suggesting a mechanism for intracellular survival. Cell Microbiol. 2008;10(10):2043–57. https://doi.org/10.1111/j.1462-5822.2008.01186.x.
Del Poeta M. Role of phagocytosis in the virulence of Cryptococcus neoformans. Eukaryot Cell. 2004;3(5):1067–75.
•• Garelnabi M, May RC. Variability in innate host immune responses to cryptococcosis. Mem Inst Oswaldo Cruz. 2018;113(7):e180060. https://doi.org/10.1590/0074-02760180060 Review of the host immune response against Cryptococcus.
• Leopold Wager CM, Hole CR, Wozniak KL, Wormley FL Jr. Cryptococcus and phagocytes: complex interactions that influence disease outcome. Front Microbiol. 2016;7:105. https://doi.org/10.3389/fmicb.2016.00105 Depiction of the possible outcomes during Cryptococcus interaction with macrophages.
Rohatgi S, Pirofski LA. Host immunity to Cryptococcus neoformans. Future Microbiol. 2015;10(4):565–81. https://doi.org/10.2217/fmb.14.132.
Almeida GM, Andrade RM, Bento CA. The capsular polysaccharides of Cryptococcus neoformans activate normal CD4(+) T cells in a dominant Th2 pattern. J Immunol. 2001;167(10):5845–51.
• Campuzano A, Wormley FL. Innate immunity against Cryptococcus, from recognition to elimination. Journal of Fungi. 2018;4(1). https://doi.org/10.3390/jof4010033 Recapitulation of the immune response during the different stages of Cryptococcus infection.
Garcia-Barbazan I, Trevijano-Contador N, Rueda C, de Andres B, Perez-Tavarez R, Herrero-Fernandez I, et al. The formation of titan cells in Cryptococcus neoformans depends on the mouse strain and correlates with induction of Th2-type responses. Cell Microbiol. 2016;18(1):111–24. https://doi.org/10.1111/cmi.12488.
Osterholzer JJ, Surana R, Milam JE, Montano GT, Chen GH, Sonstein J, et al. Cryptococcal urease promotes the accumulation of immature dendritic cells and a non-protective T2 immune response within the lung. Am J Pathol. 2009;174(3):932–43.
Lian T, Simmer MI, D’Souza CA, Steen BR, Zuyderduyn SD, Jones SJ, et al. Iron-regulated transcription and capsule formation in the fungal pathogen Cryptococcus neoformans. Mol Microbiol. 2005;55(5):1452–72. https://doi.org/10.1111/j.1365-2958.2004.04474.x.
Tangen KL, Jung WH, Sham AP, Lian T, Kronstad JW. The iron- and cAMP-regulated gene SIT1 influences ferrioxamine B utilization, melanization and cell wall structure in Cryptococcus neoformans. Microbiology. 2007;153(Pt 1):29–41. https://doi.org/10.1099/mic.0.2006/000927-0.
Ben-Abdallah M, Sturny-Leclere A, Ave P, Louise A, Moyrand F, Weih F, et al. Fungal-induced cell cycle impairment, chromosome instability and apoptosis via differential activation of NF-kappaB. PLoS Pathog. 2012;8(3):e1002555. https://doi.org/10.1371/journal.ppat.1002555.
DeLeon-Rodriguez CM, Casadevall A. Cryptococcus neoformans: tripping on acid in the phagolysosome. Front Microbiol. 2016;7:164. https://doi.org/10.3389/fmicb.2016.00164.
Williamson PR, Jarvis JN, Panackal AA, Fisher MC, Molloy SF, Loyse A, et al. Cryptococcal meningitis: epidemiology, immunology, diagnosis and therapy. Nat Rev Neurol. 2017;13(1):13–24. https://doi.org/10.1038/nrneurol.2016.167.
Charlier C, Nielsen K, Daou S, Brigitte M, Chretien F, Dromer F. Evidence of a role for monocytes in dissemination and brain invasion by Cryptococcus neoformans. Infect Immun. 2009;77(1):120–7.
Kim KS. Mechanisms of microbial traversal of the blood-brain barrier. Nat Rev Microbiol. 2008;6(8):625–34.
Casadevall A. Cryptococci at the brain gate: break and enter or use a Trojan horse? J Clin Invest. 2010;120(5):1389–92. https://doi.org/10.1172/JCI42949.
Stie J, Fox D. Blood-brain barrier invasion by Cryptococcus neoformans is enhanced by functional interactions with plasmin. Microbiology. 2012;158(Pt 1):240–58. https://doi.org/10.1099/mic.0.051524-0.
Chang YC, Stins MF, McCaffery MJ, Miller GF, Pare DR, Dam T, et al. Cryptococcal yeast cells invade the central nervous system via transcellular penetration of the blood-brain barrier. Infect Immun. 2004;72(9):4985–95.
Aaron PA, Jamklang M, Uhrig JP, Gelli A. The blood-brain barrier internalises Cryptococcus neoformans via the EphA2-tyrosine kinase receptor. Cell Microbiol. 2018;20(3):e12811. https://doi.org/10.1111/cmi.12811.
Charlier C, Chretien F, Baudrimont M, Mordelet E, Lortholary O, Dromer F. Capsule structure changes associated with Cryptococcus neoformans crossing of the blood-brain barrier. Am J Pathol. 2005;166(2):421–32.
Chen SH, Stins MF, Huang SH, Chen YH, Kwon-Chung KJ, Chang Y, et al. Cryptococcus neoformans induces alterations in the cytoskeleton of human brain microvascular endothelial cells. J Med Microbiol. 2003;52(Pt 11):961–70.
Vu K, Eigenheer RA, Phinney BS, Gelli A. Cryptococcus neoformans promotes its transmigration into the central nervous system by inducing molecular and cellular changes in brain endothelial cells. Infect Immun. 2013;81(9):3139–47. https://doi.org/10.1128/IAI.00554-13.
Olszewski MA, Noverr MC, Chen GH, Toews GB, Cox GM, Perfect JR, et al. Urease expression by Cryptococcus neoformans promotes microvascular sequestration, thereby enhancing central nervous system invasion. Am J Pathol. 2004;164(5):1761–71.
Shi M, Li SS, Zheng C, Jones GJ, Kim KS, Zhou H, et al. Real-time imaging of trapping and urease-dependent transmigration of Cryptococcus neoformans in mouse brain. J Clin Invest. 2010;120(5):1683–93.
Alanio A, Vernel-Pauillac F, Sturny-Leclere A, Dromer F. Cryptococcus neoformans host adaptation: toward biological evidence of dormancy. mBio. 2015;6(2). https://doi.org/10.1128/mBio.02580-14.
Goldman D, Lee SC, Casadevall A. Pathogenesis of pulmonary Cryptococcus neoformans infection in the rat. Infect Immun. 1994;62(11):4755–61.
Goldman DL, Lee SC, Mednick AJ, Montella L, Casadevall A. Persistent Cryptococcus neoformans pulmonary infection in the rat is associated with intracellular parasitism, decreased inducible nitric oxide synthase expression, and altered antibody responsiveness to cryptococcal polysaccharide. Infect Immun. 2000;68(2):832–8.
Nurudeen TA, Ahearn DG. Regulation of melanin production by Cryptococcus neoformans. J Clin Microbiol. 1979;10(5):724–9.
Eisenman HC, Mues M, Weber SE, Frases S, Chaskes S, Gerfen G, et al. Cryptococcus neoformans laccase catalyses melanin synthesis from both D- and L-DOPA. Microbiology. 2007;153(Pt 12):3954–62.
Williamson PR. Biochemical and molecular characterization of the diphenol oxidase of Cryptococcus neoformans: identification as a laccase. J Bacteriol. 1994;176(3):656–64.
Alspaugh JA, Perfect JR, Heitman J. Cryptococcus neoformans mating and virulence are regulated by the G-protein alpha subunit GPA1 and cAMP. Genes Dev. 1997;11(23):3206–17.
Jiang N, Sun N, Xiao D, Pan J, Wang Y, Zhu X. A copper-responsive factor gene CUF1 is required for copper induction of laccase in Cryptococcus neoformans. FEMS Microbiol Lett. 2009;296(1):84–90.
Ballou ER, Selvig K, Narloch JL, Nichols CB, Alspaugh JA. Two Rac paralogs regulate polarized growth in the human fungal pathogen Cryptococcus neoformans. Fungal Genet Biol: FG & B. 2013;57:58–75. https://doi.org/10.1016/j.fgb.2013.05.006.
Kraus PR, Boily MJ, Giles SS, Stajich JE, Allen A, Cox GM, et al. Identification of Cryptococcus neoformans temperature-regulated genes with a genomic-DNA microarray. Eukaryot Cell. 2004;3(5):1249–60.
Rosas AL, Casadevall A. Melanization affects susceptibility of Cryptococcus neoformans to heat and cold. FEMS Microbiol Lett. 1997;153(2):265–72.
Steen BR, Zuyderduyn S, Toffaletti DL, Marra M, Jones SJ, Perfect JR, et al. Cryptococcus neoformans gene expression during experimental cryptococcal meningitis. Eukaryot Cell. 2003;2(6):1336–49.
O’Meara TR, Xu W, Selvig KM, O’Meara MJ, Mitchell AP, Alspaugh JA. The Cryptococcus neoformans Rim101 transcription factor directly regulates genes required for adaptation to the host. Mol Cell Biol. 2014;34(4):673–84. https://doi.org/10.1128/MCB.01359-13.
Ost KS, Esher SK, Leopold Wager CM, Walker L, Wagener J, Munro C, et al. Rim pathway-mediated alterations in the fungal cell wall influence immune recognition and inflammation. mBio. 2017;8(1). https://doi.org/10.1128/mBio.02290-16.
Ost KS, O’Meara TR, Huda N, Esher SK, Alspaugh JA. The Cryptococcus neoformans alkaline response pathway: identification of a novel rim pathway activator. PLoS Genet. 2015;11(4):e1005159. https://doi.org/10.1371/journal.pgen.1005159.
Singh A, Panting RJ, Varma A, Saijo T, Waldron KJ, Jong A, et al. Factors required for activation of urease as a virulence determinant in Cryptococcus neoformans. mBio. 2013;4(3):e00220–13. https://doi.org/10.1128/mBio.00220-13.
Fu MS, Coelho C, De Leon-Rodriguez CM, Rossi DCP, Camacho E, Jung EH, et al. Cryptococcus neoformans urease affects the outcome of intracellular pathogenesis by modulating phagolysosomal pH. PLoS Pathog. 2018;14(6):e1007144. https://doi.org/10.1371/journal.ppat.1007144.
Chen SC, Wright LC, Santangelo RT, Muller M, Moran VR, Kuchel PW, et al. Identification of extracellular phospholipase B, lysophospholipase, and acyltransferase produced by Cryptococcus neoformans. Infect Immun. 1997;65(2):405–11.
Cox GM, McDade HC, Chen SC, Tucker SC, Gottfredsson M, Wright LC, et al. Extracellular phospholipase activity is a virulence factor for Cryptococcus neoformans. Mol Microbiol. 2001;39(1):166–75.
Lev S, Desmarini D, Li C, Chayakulkeeree M, Traven A, Sorrell TC, et al. Phospholipase C of Cryptococcus neoformans regulates homeostasis and virulence by providing inositol trisphosphate as a substrate for Arg1 kinase. Infect Immun. 2013;81(4):1245–55. https://doi.org/10.1128/IAI.01421-12.
Wright LC, Payne J, Santangelo RT, Simpanya MF, Chen SC, Widmer F, et al. Cryptococcal phospholipases: a novel lysophospholipase discovered in the pathogenic fungus Cryptococcus gattii. Biochem J. 2004;384(Pt 2):377–84. https://doi.org/10.1042/BJ20041079.
Kabanda T, Siedner MJ, Klausner JD, Muzoora C, Boulware DR. Point-of-care diagnosis and prognostication of cryptococcal meningitis with the cryptococcal antigen lateral flow assay on cerebrospinal fluid. Clin Infect Dis:Off Publ Infect Dis Soc Am. 2014;58(1):113–6. https://doi.org/10.1093/cid/cit641.
Bryan RA, Zaragoza O, Zhang T, Ortiz G, Casadevall A, Dadachova E. Radiological studies reveal radial differences in the architecture of the polysaccharide capsule of Cryptococcus neoformans. Eukaryot Cell. 2005;4(2):465–75. https://doi.org/10.1128/EC.4.2.465-475.2005.
Maxson ME, Cook E, Casadevall A, Zaragoza O. The volume and hydration of the Cryptococcus neoformans polysaccharide capsule. Fungal Genet Biol: FG & B. 2007;44(3):180–6.
Maxson ME, Dadachova E, Casadevall A, Zaragoza O. Radial mass density, charge, and epitope distribution in the Cryptococcus neoformans capsule. Eukaryot Cell. 2007;6(1):95–109.
Cherniak R, Cheeseman MM, Reyes GH, Reiss E, Todaro F. Enhanced binding of capsular polysaccharides of Cryptococcus neoformans to polystyrene microtitration plates for enzyme-linked immunosorbent assay. Diagn Clin Immunol. 1988;5(6):344–8.
Jesus MD, Nicola AM, Chow SK, Lee IR, Nong S, Specht CA, et al. Glucuronoxylomannan, galactoxylomannan, and mannoprotein occupy spatially separate and discrete regions in the capsule of Cryptococcus neoformans. Virulence. 2010;1(6):500–8.
Zaragoza O, Rodrigues ML, De Jesus M, Frases S, Dadachova E, Casadevall A. The capsule of the fungal pathogen Cryptococcus neoformans. Adv Appl Microbiol. 2009;68:133–216.
Madu UL, Ogundeji AO, Pohl CH, Albertyn J, Sebolai OM. Elucidation of the role of 3-hydroxy fatty acids in Cryptococcus-amoeba interactions. Front Microbiol. 2017;8:765. https://doi.org/10.3389/fmicb.2017.00765.
Nicola AM, Frases S, Casadevall A. Lipophilic dye staining of Cryptococcus neoformans extracellular vesicles and capsule. Eukaryot Cell. 2009;8(9):1373–80. https://doi.org/10.1128/EC.00044-09.
•• Trevijano-Contador N, Rueda C, Zaragoza O. Fungal morphogenetic changes inside the mammalian host. Semin Cell Dev Biol. 2016;57:100–9. https://doi.org/10.1016/j.semcdb.2016.04.008 Monograph on the importance of fungal changes during host interaction.
Kozubowski L, Heitman J. Profiling a killer, the development of Cryptococcus neoformans. FEMS Microbiol Rev. 2012;36(1):78–94.
Zaragoza O, Casadevall A. Experimental modulation of capsule size in Cryptococcus neoformans. Biol Proced Online. 2004;6:10–5.
Zaragoza O, Fries BC, Casadevall A. Induction of capsule growth in Cryptococcus neoformans by mammalian serum and CO2. Infect Immun. 2003;71(11):6155–64.
Granger DL, Perfect JR, Durack DT. Virulence of Cryptococcus neoformans. Regulation of capsule synthesis by carbon dioxide. J Clin Invest. 1985;76(2):508–16.
Vartivarian SE, Anaissie EJ, Cowart RE, Sprigg HA, Tingler MJ, Jacobson ES. Regulation of cryptococcal capsular polysaccharide by iron. J Infect Dis. 1993;167(1):186–90.
Guimaraes AJ, Frases S, Cordero RJ, Nimrichter L, Casadevall A, Nosanchuk JD. Cryptococcus neoformans responds to mannitol by increasing capsule size in vitro and in vivo. Cell Microbiol. 2010;12(6):740–53.
O’Meara TR, Alspaugh JA. The Cryptococcus neoformans capsule: a sword and a shield. Clin Microbiol Rev. 2012;25(3):387–408.
Robertson EJ, Najjuka G, Rolfes MA, Akampurira A, Jain N, Anantharanjit J, et al. Cryptococcus neoformans ex vivo capsule size is associated with intracranial pressure and host immune response in HIV-associated cryptococcal meningitis. J Infect Dis. 2014;209(1):74–82. https://doi.org/10.1093/infdis/jit435.
Garcia-Rodas R, Cordero RJ, Trevijano-Contador N, Janbon G, Moyrand F, Casadevall A, et al. Capsule growth in Cryptococcus neoformans is coordinated with cell cycle progression. mBio. 2014;5(3):e00945–14. https://doi.org/10.1128/mBio.00945-14.
Pierini LM, Doering TL. Spatial and temporal sequence of capsule construction in Cryptococcus neoformans. Mol Microbiol. 2001;41(1):105–15.
Zaragoza O, Telzak A, Bryan RA, Dadachova E, Casadevall A. The polysaccharide capsule of the pathogenic fungus Cryptococcus neoformans enlarges by distal growth and is rearranged during budding. Mol Microbiol. 2006;59(1):67–83.
Trevijano-Contador N, Rossi SA, Alves E, Landin-Ferreiroa S, Zaragoza O. Capsule enlargement in Cryptococcus neoformans is dependent on mitochondrial activity. Front Microbiol. 2017;8:1423. https://doi.org/10.3389/fmicb.2017.01423.
Feldmesser M, Kress Y, Casadevall A. Dynamic changes in the morphology of Cryptococcus neoformans during murine pulmonary infection. Microbiology. 2001;147(Pt 8):2355–65.
Okagaki LH, Strain AK, Nielsen JN, Charlier C, Baltes NJ, Chretien F, et al. Cryptococcal cell morphology affects host cell interactions and pathogenicity. PLoS Pathog. 2010;6(6):e1000953.
Zaragoza O, Garcia-Rodas R, Nosanchuk JD, Cuenca-Estrella M, Rodriguez-Tudela JL, Casadevall A. Fungal cell gigantism during mammalian infection. PLoS Pathog. 2010;6(6):e1000945.
Zaragoza O, Nielsen K. Titan cells in Cryptococcus neoformans: cells with a giant impact. Curr Opin Microbiol. 2013;16(4):409–13. https://doi.org/10.1016/j.mib.2013.03.006.
Wang JM, Zhou Q, Cai HR, Zhuang Y, Zhang YF, Xin XY, et al. Clinicopathological features of pulmonary cryptococcosis with cryptococcal titan cells: a comparative analysis of 27 cases. Int J Clin Exp Pathol. 2014;7(8):4837–46.
Garcia-Rodas R, Casadevall A, Rodriguez-Tudela JL, Cuenca-Estrella M, Zaragoza O. Cryptococcus neoformans capsular enlargement and cellular gigantism during Galleria mellonella infection. PLoS One. 2011;6(9):e24485.
Gerstein AC, Fu MS, Mukaremera L, Li Z, Ormerod KL, Fraser JA, et al. Polyploid titan cells produce haploid and aneuploid progeny to promote stress adaptation. mBio. 2015;6(5):e01340–15. https://doi.org/10.1128/mBio.01340-15.
Mukaremera L, Lee KK, Wagener J, Wiesner DL, Gow NAR, Nielsen K. Titan cell production in Cryptococcus neoformans reshapes the cell wall and capsule composition during infection. The Cell Surface. 2018;1:15–24.
Probert M, Zhou X, Goodall M, Johnston SA, Bielska E, Ballou ER, et al. A glucuronoxylomannan epitope exhibits serotype-specific accessibility and redistributes towards the capsule surface during titanization of the fungal pathogen Cryptococcus neoformans. Infect Immun. 2019;87(4). https://doi.org/10.1128/IAI.00731-18.
Okagaki LH, Wang Y, Ballou ER, O’Meara TR, Bahn YS, Alspaugh JA, et al. Cryptococcal titan cell formation is regulated by G-protein signaling in response to multiple stimuli. Eukaryot Cell. 2011;10(10):1306–16.
Evans RJ, Li Z, Hughes WS, Djordjevic JT, Nielsen K, May RC. Cryptococcal phospholipase B1 is required for intracellular proliferation and control of titan cell morphology during macrophage infection. Infect Immun. 2015;83(4):1296–304. https://doi.org/10.1128/IAI.03104-14.
Crabtree JN, Okagaki LH, Wiesner DL, Strain AK, Nielsen JN, Nielsen K. Titan cell production enhances the virulence of Cryptococcus neoformans. Infect Immun. 2012;80(11):3776–85.
Okagaki LH, Nielsen K. Titan cells confer protection from phagocytosis in Cryptococcus neoformans infections. Eukaryot Cell. 2012;11(6):820–6.
• Dambuza IM, Drake T, Chapuis A, Zhou X, Correia J, Taylor-Smith L, et al. The Cryptococcus neoformans Titan cell is an inducible and regulated morphotype underlying pathogenesis. PLoS Pathog. 2018;14(5):e1006978. https://doi.org/10.1371/journal.ppat.1006978 Description of the conditions that lead to Titan cell formation in vitro avoiding the bioethical issues associated with research on Titan cells obtained from infected mice.
• Hommel B, Mukaremera L, Cordero RJB, Coelho C, Desjardins CA, Sturny-Leclere A, et al. Titan cells formation in Cryptococcus neoformans is finely tuned by environmental conditions and modulated by positive and negative genetic regulators. PLoS Pathog. 2018;14(5):e1006982. https://doi.org/10.1371/journal.ppat.1006982 Description of the conditions that lead to Titan cell formation in vitro avoiding the bioethical issues associated with research on Titan cells obtained from infected mice.
• Trevijano-Contador N, de Oliveira HC, Garcia-Rodas R, Rossi SA, Llorente I, Zaballos A et al. Cryptococcus neoformans can form titan-like cells in vitro in response to multiple signals. PLoS Pathog 2018;14(5):e1007007. doi:10.1371/journal.ppat.1007007. Description of the conditions that lead to Titan cell formation in vitro avoiding the bioethical issues associated with research on Titan cells obtained from infected mice.
•• Garcia-Rodas R, de Oliveira HC, Trevijano-Contador N, Zaragoza O. Cryptococcal titan cells: when yeast cells are all grown up. Curr Top Microbiol Immunol. 2018. https://doi.org/10.1007/82_2018_145 Summary of the three novel methods to produce cryptococcal Titan cells in vitro.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Fungal Genomics and Pathogenesis
Rights and permissions
About this article
Cite this article
de Oliveira, H.C., Trevijano-Contador, N. & Garcia-Rodas, R. Cryptococcal Pathogenicity and Morphogenesis. Curr Fungal Infect Rep 13, 67–76 (2019). https://doi.org/10.1007/s12281-019-00340-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12281-019-00340-y