Abstract
Due to its high and increasing prevalence, type 2 diabetes mellitus is becoming more and more of a global public health burden. Effective measures are required to prevent diabetes-related morbidity and the resulting premature death. The effect of long-term glycemic fluctuations in patients with diabetes mellitus, referred to as HbA1c variability, has been the subject of intensive discussion. Whereas the mean HbA1c value is already established as a risk factor for vascular complications, an accumulation of findings makes a compelling case that HbA1c variability adds further predictive value. Recent studies raise the possibility that a reduced HbA1c variability may inhibit hyperglycemia-related diseases without increasing the risk of hypoglycemia. Taken as a whole, the present evidence demonstrates a clear association between HbA1c variability and cardiovascular events in patients with type 1 and type 2 diabetes. Nevertheless, there exists to date no standardized definition or method of measuring HbA1c variability. To advance further research, it would be helpful to reach consensus on a precise definition of HbA1c variability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As a result of its high and increasing prevalence, type 2 diabetes mellitus is becoming more and more of a global public health burden with the potential to impact upon economies worldwide. Type 2 diabetes was once a disease of concern almost exclusively in western developed countries but it is now increasingly an issue in developing countries. The desire to minimize the risks of well-known micro- and macrovascular complications such as retinopathy, nephropathy, neuropathy, ischemic heart disease, peripheral vascular disease, and cerebrovascular disease motivates further research in the field of diabetes management. Recent clinical evidence has raised the possibility that long-term fluctuations in glycated hemoglobin levels (HbA1c) play an important role in the prediction of vascular complications and mortality in patients with type 1 and 2 diabetes.
Epidemiology and Importance of Glucose Control
The International Diabetes Federation currently estimates that at least 415 million people worldwide live with diabetes, and it is expected that this number will reach 642 million people by the year 2040 [1]. Globally, healthcare costs continue to increase, with 12 % of health expenditure dedicated to the treatment of diabetes and its complications. The increase in future health expenditure is likely to be driven by the expected population growth in developing countries and the increasing trend of urbanization and the resulting lifestyle changes. At the same time, up to one half of all diabetes cases in adults are undiagnosed, with these individuals at high risk of developing complications. Due to associated vascular complications such as chronic renal disease, diabetic retinopathy, coronary artery disease, and peripheral artery disease, diabetes impacts strongly upon both patient quality of life and the economic state of healthcare systems. It is increasingly evident that early diagnosis and optimal long-term treatment are critical components required to control the condition. Effective prevention of diabetes-related premature death and morbidity requires better long-term management and long-term glycemic control.
HbA1c Variability
HbA1c has proven to be both a valid measure of long-term glycemic status and a useful indicator with which to monitor the treatment of diabetes. To date, it is well known that the level of HbA1c is highly associated with the degree of micro- and macrovascular damage in patients with diabetes [2, 3]. However, recent findings have further demonstrated that the variability of HbA1c measures over time might be a reliable additional measure of glycemic control and perhaps even a stronger predictor of complications than measures of average HbA1c. The association between long-term fluctuation in HbA1c and the development of long-term complications continues to be the subject of intensive discussion. Several studies and systematic reviews have demonstrated that, in patients with type 1 and type 2 diabetes, HbA1c variability is an independent risk factor for micro- and macrovascular complications [4••, 5•, 6–9, 10•].
Definition of HbA1c Variability
The term “glycemic variability” may be defined in different ways. It can refer to within-day fluctuations in an individual’s glucose level as it rises and falls in response to factors such as food, physical activity, and diabetes therapy. Additionally, it can relate to changes in the mean glucose concentration as assessed by HbA1c values measured over several months. This concept is referred to as “HbA1c variability.” The distinction between these definitions is of relevance because they may be related to different pathophysiological mechanisms [11]. To date, however, there is no standardized definition or method of measuring the HbA1c variability.
Most studies have expressed HbA1c variability based on the standard deviation or coefficient of variation of all HbA1c measurements in the period of investigation, sometimes with statistical correction when only few measurements are available per patient [6–9, 12•, 13]. However, in routine practice, and therefore also in most observational studies, patients often have irregular follow-up intervals with unequally spaced measurements. For this reason, the standard deviation would appear to be problematic as a measure of variability. For example, if HbA1c measurements are widely spaced, the available data may not be representative of the periods of fluctuation and/or stability between measurements. The standard deviation may also amplify large differences because it is based on the squared difference of the measurements to their average value.
A fundamentally different concept of HbA1c variability was applied by Skriver and colleagues [14•], who considered the residuals of HbA1c measurements from a straight line connecting the first and last measurements. Patients whose HbA1c level increased or decreased at a stable rate were considered to have zero HbA1c variability. Like other definitions, the resulting statistic measures the extent to which the HbA1c level is under control. Unlike other definitions, it does not measure whether HbA1c is stable over the period of investigation. This approach is therefore more suited to the investigation of deviation from an optimum therapy as opposed to the effect of HbA1c variability in the usual sense of the term. One potential problem is that, if the first or last values in a series of patient measurements are unusually high or low, the resulting statistic may not provide an appropriate summary of the actual HbA1c variability.
Bonke et al. [10•] used a novel approach to calculate and measure HbA1c variability based on the absolute difference between successive measurements. These were scaled according to the time between measurements to obtain a series of values that represented the rate of change in HbA1c over a 3-month interval. As HbA1c measurements are generally taken at irregular intervals, this approach reflects the understanding that a standardized time interval is required in order to yield a uniform, clinically useful definition of HbA1c variability. Such a measure could provide suitable information for risk stratification and might influence future therapeutic targets. Nevertheless, it is unclear whether the rescaling of HbA1c differences to form a rate of change accurately reflects the underlying physiological processes.
Interestingly, a recently published meta-analysis [4••] found that, irrespective of the utilized method of measuring HbA1c variability, the effect sizes and directions were remarkably similar.
Pathophysiology
Generally speaking, HbA1c variability is an indication of unstable glucose control and can also be a marker of therapy adherence and patient compliance [14•, 15]. The exact pathophysiological mechanisms linking HbA1c variability to diabetes complications are however still not well understood, with a lack of firm evidence to support one or more of the numerous theories proposed.
Basic science studies and animal experiments have shown several detrimental effects of oscillating glucose levels [16, 17]. One possibility relates to the theory of metabolic memory, promoting a mechanism of non-enzymatic glycation of cellular proteins and lipids and an excess of cellular reactive oxygen and nitrogen species. A resulting disturbance in signal transduction and cellular communication as well as oxidative and inflammatory stress reactions have been suggested as potential molecular consequences [18]. Repeated glycemic fluctuation generates higher levels of inflammatory cytokines and consequently leads to endothelial dysfunction [19]. It has been shown that daily glycemic fluctuations are strongly predictive for a higher oxidative stress [20] and endothelial dysfunction [21] and for an increase in carotid intimal thickness and ventricular mass [22]. The inadequate antioxidant cellular defense caused by the oscillating glucose might be an underlying explanation [18], causing a downregulation of genes involved in free radical detoxification [23].
Other authors have emphasized the effect of hypoglycemia which can be a consequence of higher glucose variability. For example, activation of the sympatho-adrenal system induced by low blood-sugar levels leads to transient cardiac stress by substantially increasing cardiac workload through heart rate and stroke volume. The effects are dangerous, especially in older patients and those with chronic illnesses [24, 25].
Other explanations postulate that HbA1c variability is a statistical artifact without any implication of causality. This relates to the finding that higher HbA1c levels are associated with an exponential increase in the risk of complications. For example, let us consider a hypothetical situation of two patients, A and B, who both have a mean HbA1c value of 8 %, with patient A having no HbA1c variation (i.e., always 8 %) and patient B having high variation in measurements. When patient B experiences periods with higher HbA1c, the risk of complications increases exponentially relative to patient A. Because of the exponential risk relationship, these periods of higher risk are not counterbalanced by episodes of substantially lower risk when the HbA1c value is less than the mean [11]. Such an explanation would suggest that high HbA1c levels are the cause of the adverse effects, with the measurement of HbA1c variability merely compensating for the incomplete information contained in the mean value.
Another possibility is that patients with a higher HbA1c variability may generally be characterized by poor management of diabetes and associated complications. Patients with poor compliance with respect to their diabetes management may be less likely to persist with lifestyle interventions such as weight management or regular intake of medication such as antihypertensive therapy and lipid-lowering therapy. This would regard HbA1c variability as a common effect of lifestyle issues and not as a cause of cardiovascular events [26].
Current Evidence
Several studies have suggested that increased HbA1c variability has a detrimental effect on survival [12•, 14•, 27]. As a result, HbA1c variability is emerging as a measure of glycemic control and could be a reliable predictor of diabetes-related vascular complications. A recent systematic review by Gorst et al. [4••] reinforced this view after evaluating the association between HbA1c variability, vascular complications, and mortality in patients with type 1 and type 2 diabetes. This meta-analysis was based on 20 studies in 87,641 patients and indicated that a higher HbA1c variability was associated with a higher risk for cardiovascular events, both for type 1 diabetes (risk ratio 1.98; 95 % CI 1.39–2.82) and for type 2 diabetes (risk ratio 1.27; 95 % CI 1.15–1.40).
The focus of most previously conducted studies has been on the impact of glycemic variability on microvascular complications rather than macrovascular outcomes [28]. Nevertheless, Yang et al. [29•] demonstrated an association between HbA1c variability and subclinical coronary atherosclerosis, finding that HbA1c variability was a stronger predictor of premature subclinical coronary atherosclerosis than mean HbA1c.
Recent studies showed HbA1c variability to be associated with cardiovascular events and mortality independent of the baseline HbA1c level [9, 10•, 12•, 14•, 30]. These observations raise the possibility that interventions that reduce long-term fluctuations in HbA1c may help to avoid hyperglycemia-related diabetes complications while minimizing the risk of hypoglycemia.
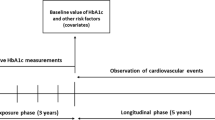
However, studies differ greatly with respect to their methodological approaches. A recent study by Bonke et al. [10•] evaluated the association of HbA1c variability with non-fatal cardiovascular events in a cohort of patients with type 2 diabetes mellitus who were starting insulin. This patient group was expected to experience relatively large fluctuation in HbA1c. HbA1c variability was defined as the rate of change in HbA1c values between the observations, measured in percentage points per quarter (i.e., per 90-day period). A cohort of 13,777 patients with observed transition to insulin therapy was analyzed for a period of at least 5 years. They found a non-linear U-shaped relationship between HbA1c variability and cardiovascular events, with the lowest risk being seen with a rate of change of HbA1c of approximately 0.5 % (5.5 mmol/mol) per quarter. Furthermore, predicted survival curves revealed that increasing HbA1c variability in all patients from 0.5 to 1.5 % HbA1c percentage points per quarter would lead to an increase in the proportion experiencing myocardial infarction within 2 years from 1 to 10 % and for stroke from 1 to 29 %. The cumulated evidence would therefore suggest that rapidly changing HbA1c levels are associated with an increased risk of cardiovascular events. Such results should therefore find consideration in the future management of diabetes mellitus.
While some studies have identified a linear association between HbA1c and the risk of cardiovascular disease (CVD) [31, 32], others have revealed a non-linear (U- or J-shaped) relationship ([33–35•]). This may in part be a result of the differing methodologies applied. Especially with observational data, differences in data collection and patient collective may also impact upon the nature of the associations identified. For example, Currie et al. [34] found a U-shaped relationship with low and high HbA1c values that were associated with increased all-cause mortality and CVD. Within an observational cohort study of 27.965 patients with type 2 diabetes whose treatment had been intensified from oral monotherapy to a combination therapy, they showed that the minimum risk for all-cause mortality and CVD was associated with a mean HbA1c of 7,5 %. In contrast, Eeg-Olofsson et al. [31] showed a linear increasing risk of CVD and mortality with higher HbA1c levels. They found no risk increase at low HbA1c values.
Finally, it must be considered that observational studies are fundamentally limited in their interpretation. The lack of randomisation and control mean that it is impossible to fully separate the effect of interest from that of observed and unobserved confounding variables. There is also a risk that observations have occurred as a result of reverse causality. Clinical trials are therefore indispensable and would be beneficial to identify the optimal clinical HbA1c targets and optimal levels of glucose variability. If confirmed by such trials, low HbA1c variability could be established as an important treatment target in diabetes management.
Recommendations for Future Research
In order to formulate clinical guidelines, it would appear necessary to develop a standardized definition of HbA1c variability, appropriate for use both in clinical studies and in everyday practice. This should take account of statistical simulations to test the robustness of the various proposed measures and consider the possible causal mechanisms. The aim would be to establish a simple measure that most precisely reflects the aspect of HbA1c variability deemed to be of greatest relevance. This would also ensure compatibility of results among studies.
Conclusion
Current compelling findings show that increased HbA1c variability is associated with all-cause mortality and cardiovascular events independent of the mean HbA1c level. Moreover, strong indications are emerging that HbA1c variability is a better predictor of cardiovascular diseases than mean HbA1c. Among patients with type 1 and type 2 diabetes, HbA1c variability is associated with a higher risk for cardiovascular events and mortality. Further research and especially clinical studies are necessary to test the hypotheses generated from recent observational studies and ascertain whether the reduction of HbA1c variability should be a further treatment target.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
International Diabetes Federation. IDF diabetes atlas. Brussels, Belgium: International Diabetes Federation; 2015.
Moss SE, Klein R, Klein BE, Meuer SM. The association of glycemia and cause-specific mortality in a diabetic population. Arch Intern Med. 1994;154:2473–9.
Selvin E, Marinopoulos S, Berkenblit G, Rami T, Brancati FL, Powe NR, et al. Meta-analysis: glycosylated hemoglobin and cardiovascular disease in diabetes mellitus. Ann Intern Med. 2004;141:421–31.
Gorst C, Kwok CS, Aslam S, Buchan I, Kontopantelis E, Myint PK, et al. Long-term glycemic variability and risk of adverse outcomes: a systematic review and meta-analysis. Diabetes Care. 2015;38:2354–69. Current strongest evidence in this field; first all-embracing meta-analysis on micro- and macrovascular outcomes.
Cheng D, Fei Y, Liu Y, Li J, Xue Q, Wang X, et al. HbA1C variability and the risk of renal status progression in diabetes mellitus: a meta-analysis. PLoS ONE. 2014;9:e115509. First meta-analysis on microvascular outcomes.
Sugawara A, Kawai K, Motohashi S, Saito K, Kodama S, Yachi Y, et al. HbA(1c) variability and the development of microalbuminuria in type 2 diabetes: Tsukuba Kawai Diabetes Registry 2. Diabetologia. 2012;55:2128–31.
Penno G, Solini A, Bonora E, Fondelli C, Orsi E, Zerbini G, et al. HbA1c variability as an independent correlate of nephropathy, but not retinopathy, in patients with type 2 diabetes: the Renal Insufficiency And Cardiovascular Events (RIACE) Italian multicenter study. Diabetes Care. 2013;36:2301–10.
Hsu CC, Chang HY, Huang MC, Hwang SJ, Yang YC, Lee YS, et al. HbA1c variability is associated with microalbuminuria development in type 2 diabetes: a 7-year prospective cohort study. Diabetologia. 2012;55:3163–72.
Luk AOY, Ma RCW, Lau ESH, Yang X, Lau WWY, Yu LWL, et al. Risk association of HbA1c variability with chronic kidney disease and cardiovascular disease in type 2 diabetes: prospective analysis of the Hong Kong Diabetes Registry. Diabetes Metab Res Rev. 2013;29:384–90.
Bonke FC, Donnachie E, Schneider A, Mehring M. Association of the average rate of change in HbA with severe adverse events: a longitudinal evaluation of audit data from the Bavarian Disease Management Program for patients with type 2 diabetes mellitus. Diabetologia 2015. Biggest study on hba1c variability in micro- and macrovascular outcomes with an improved methodological approach of hba1c variability
Kilpatrick ES. The rise and fall of HbA(1c) as a risk marker for diabetes complications. Diabetologia. 2012;55:2089–91.
Hirakawa Y, Arima H, Zoungas S, Ninomiya T, Cooper M, Hamet P, et al. Impact of visit-to-visit glycemic variability on the risks of macrovascular and microvascular events and all-cause mortality in type 2 diabetes: the ADVANCE trial. Diabetes Care. 2014;37:2359–65. Important findings on hba1c variability in micro- and macrovascular outcomes as well on all-cause mortality within the ADVANCE population.
Rodriguez-Segade S, Rodriguez J, Garcia Lopez JM, Casanueva FF, Camina F. Intrapersonal HbA(1c) variability and the risk of progression of nephropathy in patients with type 2 diabetes. Diabet Med. 2012;29:1562–6.
Skriver MV, Sandbaek A, Kristensen JK, Stovring H. Relationship of HbA1c variability, absolute changes in HbA1c, and all-cause mortality in type 2 diabetes: a Danish population-based prospective observational study. BMJ Open Diabetes Res Care. 2015;3:e000060. First fundamentally different methodological concept of hba1c variability and important findings on hba1c variability and all-cause mortality.
Frontoni S, Di Bartolo P, Avogaro A, Bosi E, Paolisso G, Ceriello A. Glucose variability: an emerging target for the treatment of diabetes mellitus. Diabetes Res Clin Pract. 2013;102:86–95.
Ceriello A. Postprandial hyperglycemia and diabetes complications: is it time to treat? Diabetes. 2005;54:1–7.
Ceriello A, Ihnat MA. ‘Glycaemic variability’: a new therapeutic challenge in diabetes and the critical care setting. Diabet Med. 2010;27:862–7.
Ihnat MA, Thorpe JE, Ceriello A. Hypothesis: the ‘metabolic memory’, the new challenge of diabetes. Diabet Med. 2007;24:582–6.
Esposito K, Nappo F, Marfella R, Giugliano G, Giugliano F, Ciotola M, et al. Inflammatory cytokine concentrations are acutely increased by hyperglycemia in humans: role of oxidative stress. Circulation. 2002;106:2067–72.
Monnier L, Mas E, Ginet C, Michel F, Villon L, Cristol J, et al. Activation of oxidative stress by acute glucose fluctuations compared with sustained chronic hyperglycemia in patients with type 2 diabetes. JAMA. 2006;295:1681–7.
Ceriello A, Esposito K, Piconi L, Ihnat MA, Thorpe JE, Testa R, et al. Oscillating glucose is more deleterious to endothelial function and oxidative stress than mean glucose in normal and type 2 diabetic patients. Diabetes. 2008;57:1349–54.
Di Flaviani A, Picconi F, Di Stefano P, Giordani I, Malandrucco I, Maggio P, et al. Impact of glycemic and blood pressure variability on surrogate measures of cardiovascular outcomes in type 2 diabetic patients. Diabetes Care. 2011;34:1605–9.
Meugnier E, Faraj M, Rome S, Beauregard G, Michaut A, Pelloux V, et al. Acute hyperglycemia induces a global downregulation of gene expression in adipose tissue and skeletal muscle of healthy subjects. Diabetes. 2007;56:992–9.
Frier BM, Schernthaner G, Heller SR. Hypoglycemia and cardiovascular risks. Diabetes Care. 2011;34 Suppl 2:S132–7.
Hsu P, Sung S, Cheng H, Yeh J, Liu W, Chan W, et al. Association of clinical symptomatic hypoglycemia with cardiovascular events and total mortality in type 2 diabetes: a nationwide population-based study. Diabetes Care. 2013;36:894–900.
Waden J, Forsblom C, Thorn LM, Gordin D, Saraheimo M, Groop P. A1C variability predicts incident cardiovascular events, microalbuminuria, and overt diabetic nephropathy in patients with type 1 diabetes. Diabetes. 2009;58:2649–55.
Bonds DE, Miller ME, Bergenstal RM, Buse JB, Byington RP, Cutler JA, et al. The association between symptomatic, severe hypoglycaemia and mortality in type 2 diabetes: retrospective epidemiological analysis of the ACCORD study. BMJ. 2010;340:b4909.
Kilpatrick ES, Rigby AS, Atkin SL. A1C variability and the risk of microvascular complications in type 1 diabetes: data from the Diabetes Control and Complications Trial. Diabetes Care. 2008;31:2198–202.
Yang HK, Kang B, Lee S, Yoon K, Hwang B, Chang K, Han K, Kang G, Cho JH. Association between hemoglobin A1c variability and subclinical coronary atherosclerosis in subjects with type 2 diabetes. J Diabetes Complications. 2015. Important findings on hba1c variability and macrovascular outcomes
Takao T, Matsuyama Y, Yanagisawa H, Kikuchi M, Kawazu S. Association between HbA1c variability and mortality in patients with type 2 diabetes. J Diabetes Complications. 2014;28:494–9.
Eeg-Olofsson K, Cederholm J, Nilsson PM, Zethelius B, Svensson A, Gudbjornsdottir S, et al. New aspects of HbA1c as a risk factor for cardiovascular diseases in type 2 diabetes: an observational study from the Swedish National Diabetes Register (NDR). J Intern Med. 2010;268:471–82.
Pfister R, Sharp SJ, Luben R, Khaw K, Wareham NJ. No evidence of an increased mortality risk associated with low levels of glycated haemoglobin in a non-diabetic UK population. Diabetologia. 2011;54:2025–32.
Selvin E, Steffes MW, Zhu H, Matsushita K, Wagenknecht L, Pankow J, et al. Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med. 2010;362:800–11.
Currie CJ, Peters JR, Tynan A, Evans M, Heine RJ, Bracco OL, et al. Survival as a function of HbA(1c) in people with type 2 diabetes: a retrospective cohort study. Lancet. 2010;375:481–9.
Kontopantelis E, Springate DA, Reeves D, Ashcroft DM, Rutter MK, Buchan I, et al. Glucose, blood pressure and cholesterol levels and their relationships to clinical outcomes in type 2 diabetes: a retrospective cohort study. Diabetologia. 2015;58:505–18. First in-depth description of different relationships between hba1c and clinically important outcomes.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Drs. Mehring, Donnachie and Schneider report no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the author.
Additional information
This article is part of the Topical Collection on Diabetes + Insulin Resistance
Rights and permissions
About this article
Cite this article
Mehring, M., Donnachie, E. & Schneider, A. HbA1c Variability and Cardiovascular Events. Curr Cardiovasc Risk Rep 10, 18 (2016). https://doi.org/10.1007/s12170-016-0501-x
Published:
DOI: https://doi.org/10.1007/s12170-016-0501-x