Opinion statement
Proper diagnosis of dementia with Lewy bodies (DLB) in clinical practice remains suboptimal as many cases are misdiagnosed, usually as Alzheimer disease (AD) or Parkinson’s disease (PD) and, in rare cases, psychosis. Therefore, it is important for patients with dementia to be thoroughly evaluated by a specialist who is familiar with current diagnostic tests and treatment options. New diagnostic criteria from the Dementia with Lewy Bodies Consortium have been developed to increase diagnostic sensitivity for DLB (Diagnosis and management of dementia with Lewy bodies: fourth consensus report of the DLB Consortium; McKeith et al.; Neurology, 89(1): 88–100). REM sleep behavior disorder (RBD) has been studied more thoroughly in correlation with DLB and is now considered a core feature. D2 receptor blocking antipsychotics, which can cause severe antipsychotic sensitivity, are now rarely prescribed for treatment. Therefore, severe antipsychotic sensitivity, which was a suggestive criterion for DLB diagnosis, is now listed as a supportive feature. Reduced DAT uptake in basal ganglia demonstrated by SPECT or PET imaging has high specificity (90%) for distinguishing DLB from AD. Reduced uptake on metaiodobenzylguanidine myocardial scintigraphy correlates with reduced postganglionic sympathetic cardiac innervation in Lewy body diseases, which can increase specificity for discriminating probable DLB from probable AD in milder cases of dementia. However, the latter is more commonly used in Japan and is not used in the USA. The evidence supporting the benefit of other therapeutic modalities is limited in DLB due to lack of extensive studies. There are no FDA-approved medications for the treatment of DLB, although some effective drugs have been used off label to treat various symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The term “Lewy body disease” was first proposed by Kosaka [1] in the 1980, and the first diagnostic criteria for dementia with Lewy bodies (DLB) was set forth in 1996. Since then, our understanding of this disorder has increased dramatically . Substantial new knowledge about REM sleep behavior disorder (RBD) and diagnostic biomarkers has been gained. Color vision impairment is a new finding, which has been reported in DLB patients and MCI-DLB patients [2,3,4]. The fourth consensus report of the Dementia with Lewy Bodies Consortium recently revised its recommendations for diagnosis and management of DLB [5••] (Table 1). The new criteria distinguishes between clinical features and diagnostic biomarkers and gives more diagnostic weight to REM sleep behavior disorder and 123iodine-metaiodobenzylguanidine (MIBG) myocardial scintigraphy [5••]. In this review, we will discuss the diagnosis of cognitive and behavioral symptoms of DLB and comment on the current treatment options for DLB (Table 2).
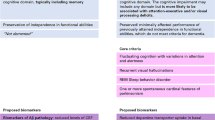
To be diagnosed with DLB, dementia must be present. Dementia is defined as a progressive cognitive decline of sufficient magnitude to interfere with social or occupational functions or with daily activities [5••] (Fig. 1).
Diagnostic algorithm for the clinical diagnosis of probable and possible dementia with Lewy bodies (DLB) based on revised criteria 2017. DA, dopamine; I-MIBG, iodine metaiodobenzylguanidine; RBD, REM sleep behavior disorder; DaT scan, dopamine transporter (DAT) single photon emission computerized tomography (SPECT) imaging technique; PSG, polysomnography.
The core clinical features of the disease have been extended to include RBD in addition to fluctuating cognition, recurrent visual hallucinations, and parkinsonism. Basically, dementia in the presence of polysomnogram-confirmed RBD suggests possible DLB.
Although there is no direct biomarker of DLB, there are three indicative biomarkers: reduced dopamine transporter uptake in the basal ganglia as demonstrated by SPECT or PET, polysomnographic confirmation of REM sleep without atonia, and low uptake iodine-MIBG myocardial scintigraphy which has gained more recognition in Japan and East Asia [6] but is not used clinically in the USA.
Possible DLB can be diagnosed in the presence of dementia with one or more indicative biomarkers or only one core feature [5••]. Probable DLB diagnosis requires dementia in the presence of two core clinical features or one core feature and at least one indicative biomarker (Fig. 2).
Probable DLB should not be diagnosed on the basis of biomarkers alone [5••]. DLB should only be diagnosed when dementia occurs before or concurrently with parkinsonism. (For research purposes, a 1-year period between the onset of dementia and parkinsonism continues to be recommended to separate DLB from PDD [5••].) If parkinsonism is the only core clinical feature and it appears for the first time with severe dementia, DLB is less likely.
The management of DLB requires a multifaceted approach. There are currently no effective Food and Drug Administration (FDA)-approved treatments for DLB. Evidenced-based recommendations are limited. The information provided in the following sections discusses the pharmacological management of disease symptoms; it is based on limited randomized trials, case series, and expert opinion.
Cognition
In early stage disease, memory loss may not be prominent but there are usually deficits in attention, visual-spatial tasks, and executive function. Deficits on tests of attention, executive function, and visuoperceptual ability may occur early. DLB patients perform similarly to those with AD in episodic and semantic memory [7], language performance (naming and verbal fluency), and orientation [8]. They perform worse on executive function and attention tests [7, 9], visual-spatial skills, and perceptual ability and better in delayed recall [8, 10, 11]. Prominent memory impairment may not occur in the early stages but becomes more evident as the disease progresses [5••].
The following tests are recommended for brief cognitive screening in DLB: Montreal Cognitive Assessment (MoCA), Parkinson’s Disease Cognitive Rating Scale, Parkinson’s Neuropsychometric Dementia Instrument, and Scales for Outcomes in Parkinson’s Disease—Cognition [10, 12].
Currently, no medication has been approved for use in the USA for cognition in DLB but there is class I evidence suggesting that donepezil and rivastigmine improve cognition and global function [13, 14•]. Donepezil at 10 mg dose, but not 5 mg, improved cognitive function and also fluctuations in cognition [14•, 15]. Donepezil has been approved for the treatment of DLB in Japan.
Memantine seems to be well tolerated in most cases. Memantine had a positive impact on global impression and behavioral symptoms, but its efficacy on cognitive function is less clear [16]. In a small study, a positive clinical response to early treatment with memantine, as measured by the Clinical Global Impression of Change (CGIC), predicted longer survival in patients with DLB [17] (Table 2).
Donepezil
Standard dose
10 mg daily
Contraindication
Use with caution in patients with cardiac conduction; especially first-degree AV block, QT prolongation, obstructive pulmonary disease, severe asthma, or bladder outflow obstruction.
Main side effects
Gastrointestinal (GI) symptoms: diarrhea, nausea, vomiting, loss of appetite and weight loss; nightmare
Major drug interactions
-
Drugs with a possible risk for QT prolongation should be used cautiously and with monitoring when prescribed concomitantly with donepezil. Combined use with beta blockers increases the risk of bradycardia. Concurrent use of cholinergic agonists and cholinesterase inhibitors should be avoided.
-
Cholinesterase inhibitors may also prolong the neuromuscular blocking effects if given with neuromuscular blockers [18].
Special points
-
5 mg once daily initially. Upward titration to 10 mg once daily. Caution with donepezil 23 mg as GI symptoms are more common.
-
Patients with nightmares may benefit from daytime dose with meal. But patient with GI sensitivity benefit from bedtime dosing.
-
Use donepezil with caution in those with a history of ulcer disease. The author avoids using donepezil in patients with history of peptic ulcer bleeding over the past 6 months.
Rivastigmine
Standard dose
Oral 3–6 mg twice a day, transdermal 9.5–13.3 mg/24 h
Main side effects
See donepezil side effects.
Major drug interaction
-
Concurrent use of cholinergic agonists and cholinesterase inhibitors such as rivastigmine should be avoided.
-
Cholinesterase inhibitors may also prolong the neuromuscular blocking effects if given with neuromuscular blockers.
-
The risk of extrapyramidal effects may be increased during concurrent use of metoclopramide and rivastigmine [19].
Special points
Oral: Start 1.5 mg twice a day, increase by 1.5 mg/dose every 2 weeks to maximum tolerated dose.
Transdermal: Apply 4.6 mg/24 h patch per day for 4 weeks, then increase every 4 weeks to maximum tolerated dose.
-
Advise patients to remove rivastigmine transdermal patch before undergoing magnetic resonance imaging (MRI) as some patches contain metal components and can overheat causing skin burns [19].
-
Rivastigmine has favorable cardiac safety profile compared to donepezil [20].
-
Concurrent use of sedating H1 blockers and rivastigmine should be avoided if possible [19].
-
Discontinue rivastigmine patch if there is allergic contact dermatitis suggested by spreading of application site reaction beyond the patch size or severe local reactions [19].
Memantine
Standard dose
10 mg twice a day immediate-release formulation; 28 mg/day PO extended-release formulation
Main side effects
Restlessness, dizziness, somnolence, hypertension, headache, hallucinations, and increased confusion
Major drug interaction
-
It has a major drug interaction with quinidine, procainamide, and dofetilide.
-
Dextromethorphan, amantadine, and ketamine are also NMDA antagonists which may lead to additive adverse effects if combined with memantine [21].
Special points
-
Patients who take memantine must be advised to avoid diphenhydramine or most over-the-counter sleep aids except for melatonin as they can worsen confusion.
-
For patients with creatinine clearance of 5–29, a target dose of 5 mg twice daily of immediate-release formulations and a target dose of 14 mg/day of the extended-release capsule is recommended [22].
Parkinsonism
Parkinsonian symptoms occur less often in DLB patients than in PD patients [23] and maybe milder or absent entirely in DLB [15, 24,25,26].Subsequently, many patients with DLB may fall short of the definition of parkinsonism in Parkinson’s disease, which is bradykinesia in combination with rest tremor and/or rigidity. Thus, only one of these core parkinsonian features suffices to meet the core feature for DLB.
When there is a doubt about parkinsonism in the case of tremor, ioflupane uptake scan by SPECT or PET (DaT scan) can be helpful in making a diagnosis. Parkinsonian symptoms are usually less responsive to levodopa in DLB than in PD [27] with less rest tremor and more myoclonus [28]. Dopaminergic treatment commonly used for parkinsonism has a modest effect but may increase the risk of psychosis.
Carbidopa-levodopa
Standard dose
1–3 tablets of 25–100 mg three times a day
Main side effects
Nausea, vomiting, hypotension, dyskinesia, axonal neuropathy, sudden sleep onset, impulse control symptoms, depression, suicidal ideation, and hallucinations
Major drug interaction
-
Avoid concomitant use of levodopa with medications with dopamine antagonist activity such as antipsychotics (i.e., phenothiazine-type drug).
-
Use bupropion cautiously in patients taking levodopa.
Special points
-
Levodopa therapy should be started at a low dose (carbidopa-levodopa 25–100 mg half tablet twice a day for 2 days) with slow titration (to one tablet three times a day). Patients are recommended to take this medication 30–60 min before or 1–2 h after eating a high-protein meal because protein reduces the absorption of levodopa.
-
Avoid abrupt discontinuation of carbidopa- levodopa therapy.
-
Carbidopa-levodopa combinations are contraindicated for use in patients with closed-angle glaucoma and in patients with a history of melanoma [21].
-
Iron salts should be separated from levodopa by at least 2 h [21].
Neuropsychiatric symptoms
Anxiety and depression
Anxiety is more common in patients with DLB than in patients with AD [29]. In one study, patients with DLB were more likely to have a history of anxiety and depression prior to diagnosis of dementia; anxiety is considered a risk factor for DLB [30]. Anxiety was not found to be a critical factor for the rate of cognitive decline in patients with DLB [31]. Interestingly, self-reported anxiety was associated with slower cognitive decline [31]. Anxiety can occur secondary to psychosis in some cases, and addressing the latter may improve behavioral symptoms.
DLB patients with symptoms of anxiety report more falls irrespective of whether they are taking an antidepressant [32]. This finding is similar to a study of cognitively intact elderly, which noted that people with anxiety do less, and that leads to deconditioning and increased risk of falls [32].
There is insufficient evidence to support the use of antidepressants in DLB. Selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors, and mirtazapine can be considered for the treatment of depression and anxiety in DLB. These medications, especially venlafaxine and mirtazapine, may worsen RBD. As such, physicians should inquire specifically about this adverse effect at follow-up visits because the patient may not report them.
Among SSRIs, sertraline maybe a better first choice because daytime sleepiness is common in DLB patients and escitalopram and citalopram can be considered for patients with difficulty sleeping. Donepezil at 10 mg dose was also reported to improve depression [15] (Table 2).
Sertraline
Standard dosage
25–200 mg daily
Contraindications
Concomitant use with MAO inhibitors or within 14 days of stopping treatment with sertraline is contraindicated because of an increased risk of serotonin syndrome.
Main side effects
Nausea, diarrhea, insomnia, dry mouth, tremor, ejaculatory dysfunction
Main drug interactions
-
QT prolonging medications, serotonergic medications, and drugs metabolized by cytochrome p450
Special points
-
Start at 12.5 or 25 mg daily. Increase the dose gradually over 1-week interval.
-
Sertraline may be a better first choice for treatment of depression and anxiety because daytime sleepiness is common in DLB patients.
Escitalopram
Standard dosage
5–10 mg daily
Contraindications
See sertraline contraindications.
Main side effects
Nausea, diarrhea, insomnia, dry mouth, tremor, ejaculatory dysfunction
Main drug interactions
See sertraline drug interactions.
Special points
-
Initiate 5 mg/day and increased to 10 mg/day after the first week. Titrate in 5 mg increments up to a maximum of 20 mg/day.
-
Escitalopram and citalopram can be considered for treating depression and anxiety in DLB patients with difficulty sleeping.
Citalopram
Standard dosage
10–20 mg daily
Contraindications
Like sertraline
Main drug interactions
Like sertraline
Main side effects
Nausea, diarrhea, insomnia, dry mouth, tremor, ejaculatory dysfunction
Special points
-
Initiating 10 mg once daily with titration to 20 mg once daily, if needed, has been used. Dosages above 20 mg/day are not recommended in those over 60 years of age due to an association with QT prolongation.
-
Citalopram can be considered for treating depression and anxiety in DLB patients with difficulty sleeping.
-
Advise patients that are therapeutically stable on citalopram not to alter their consumption of grapefruit juice.
-
Citalopram is also available in liquid form and can be mixed with water, orange juice, or apple juice before drinking [22]. This formulation is suitable for patients who cannot or do not take tablets.
Hallucinations and delusions
Hallucinations in DLB can be simple such as the following: passage (feeling a shadow passed by), presence (sensation that someone is behind the shoulder), or illusion (misperception based on actual objects, such as seeing an armchair as a sitting man). Complex hallucinations are mostly visual. They are not necessarily terrifying to the patient, especially in the beginning [33]. They commonly take the form of little people, children, and pets. All other forms of auditory, tactile, olfactory, and gustatory hallucinations have been reported but tend to occur less frequently.
Delusions are false beliefs that run contrary to the evidence. They range from misidentification to paranoia, infidelity, and abandonment. Capgras syndrome, which is the belief that a familiar person (spouse or children) has been replaced by an imposter, is common in patients with DLB. Patients with Capgras delusions reported more anxiety and had worse behavioral ratings. They are less likely to tolerate cholinesterase inhibitors [34].
Hallucinations or delusions do not necessarily require pharmacological treatment unless they interfere with the patient’s safety, another person’s safety, or the patient’s care. No FDA-approved medication for the management of neuropsychiatric symptoms of dementia is available. Typical antipsychotics such as haloperidol and atypical antipsychotics with strong D2 receptor antagonism such as risperidone and olanzapine, which worsen parkinsonism, should be avoided.
A case series of quetiapine in DLB showed reduction of psychiatric symptoms for six of nine patients [35]. However, a randomized placebo-controlled in Lewy body dementia could not show significant difference between two groups [36]. The following antipsychotics with potential morbidity have been used off label to treat severe hallucinations and delusions that have failed to respond adequately to non-pharmacological and pharmacological strategies.
Quetiapine
Standard dosage
25–50 mg once or twice daily
Contraindications
Quetiapine should be used with caution in patients with pre-existing hypotension or cerebrovascular disease.
Caution in patients with cardiac disease or other conditions that may increase the risk of QT prolongation.
Main side effects
Somnolence, insomnia, orthostatic hypotension, dizziness, confusion, weight gain, dry mouth, hypercholesterolemia, hypertriglyceridemia
Main drug interactions
-
Potent CYP3A4 inducers may result in decreased exposure to quetiapine. When given concomitant with CYP3A4 inhibitors (i.e., ketoconazole), the dose of quetiapine should be reduced [37].
-
Caution is advisable during concurrent use of quetiapine and QT-prolonging medications.
Special points
-
Starting dose of 12.5 mg at bedtime or 1–2 h prior to time of delusion or hallucinations (sundowners), with gradual titration can be considered. The author avoids doses above 200 mg/day because they can cause anticholinergic adverse effects and worsen confusion.
-
High doses may also worsen autonomic symptoms (orthostatic hypotension).
-
The patient’s QT interval must be checked at baseline and periodically, especially if this medication is given in combination with cholinesterase inhibitors.
Clozapine
Standard dosage
6.25–50 mg once or twice daily
Contraindications
-
Myeloproliferative disorders, agranulocytosis, bone marrow suppression, chemotherapy, infection, leukemia, leukopenia, neutropenia
-
Patients with coma or severe CNS depression from any cause, paralytic ileus
Main side effects
Geriatric patients are more likely to experience anticholinergic effects, movement disorders, depression, bone marrow suppression, and agranulocytosis. Other main side effects are drowsiness, confusion, urinary incontinence or retention, tachycardia, and syncope [38].
Main drug interactions
-
Medications known to cause QT prolongation
Special points
-
There is some evidence of efficacy in PD psychosis but it is rarely used in DLB and only if all other therapies including quetiapine and cholinesterase inhibitors failed.
-
The starting dose is 6.25 mg; the patient’s complete blood cell count must be checked weekly to avoid agranulocytosis.
-
Clozapine lowers the seizure threshold in a dose-dependent manner [38].
Pimavanserin
Pimavanserin, a non-dopaminergic antipsychotic, is a new class of antipsychotics. This is the first FDA-approved medication for neurobehavioral symptoms (psychosis) in patients with a neurodegenerative disease (PD) [39•]. There is good evidence supporting the use of pimavanserin in PD psychosis, but controlled clinical trial data in DLB are needed. Limited case report suggests that it is safe and effective in DLB patients [40]. QT prolongation remains to be a concern when using this medication.
Sleep disorders
DLB patients frequently have several sleep problems that occur simultaneously; they can be multifactorial due to degeneration of the brain area that regulates sleep and/or due to parkinsonism by itself, which causes difficulty with mobility in bed. Some medications may also affect sleep such as cholinesterase inhibitors, which can cause nightmares. The presence of any sleep disorder was associated with more neuropsychiatric symptoms, higher morbidity, more parkinsonian symptoms, and excessive daytime sleepiness [41]. Poor sleep quality and daytime sleepiness have been associated with depressive symptoms in DLB [42].
Excessive daytime sleepiness in DLB
Hypersomnia can manifest as continuous sleepiness during the day or only early in the evening followed by insomnia in the early morning. Hypersomnia can be managed by promoting good sleep hygiene habits such as going to bed and waking at the same time every day and avoiding long naps or naps in the afternoon or evening. If tremor and anxiety are not prominent disturbing complaints, patients may consume one or two cups of coffee in the morning and/or early afternoon [43].
Case studies of stimulants such as modafinil and armodafinil have produced inconsistent results [44]. Armodafinil has been associated with increased wakefulness but may exacerbate agitation and hallucinations [45].
Limited case series suggest that donepezil treatment reduces sleep disturbances in DLB patients, including daytime sleepiness [46].
REM sleep behavior disorder
REM sleep behavior disorder is characterized by dream-enacting behaviors with excessive motor activity due to loss of normal skeletal muscle atonia during REM sleep. DLB patients might have experienced dream-enacting behavior for decades prior to their cognitive decline, although it may become less prominent over time. REM sleep behavior disorder is now considered a core clinical feature for the diagnosis of DLB.
RBD may occur infrequently and not be bothersome to the patient or bed partner when it does occur. But over time, it may become severe, interrupting sleep and possibly causing injury to the patient or his/her bed partner.
Physicians can screen patients for the presence of classic dream-enactment behavior by asking them a single question: “Have you ever been told, or suspected yourself, that you seem to ‘act out your dreams’ while asleep (for example, punching, flailing your arms in the air, making running movements, etc.)?” This single question has high sensitivity of 94 and 87% specificity [3]. The diagnosis can be confirmed essentially by polysomnography.
RBD has two main aspects: abnormal vocalization and abnormal motor activity. Abnormal vocalizations tend to be loud (shouting or screaming). The motor activity may begin as repetitive jerking followed by more purposeful activity such as punching, running, and flailing the arms as if the patient is trying to protect herself/himself. Dream content often involves chasing or being attacked.
It is critical to prevent sleep-related injuries that may include padding furniture, placing the mattress on the floor, and installation of doorway alarms.
The best investigated medications to treat RBD are melatonin and clonazepam (Table 2).
Melatonin
Standard dosage
3–12 mg at bedtime
Contraindications
Use with caution in lactose intolerance or liver impairment.
Main side effects
Headache, joint pain, daytime sleepiness
Main drug interactions
-
CNS depressants interacts with melatonin.
Special points
Clonazepam
Numerous cohort studies have demonstrated good efficacy at a dose of 0.5–2 mg30 min before bedtime for patient with RBD with and without dementia [49•].
Standard dosage
0.25–0.5 mg at bedtime
Contraindications
Liver impairment, acute angle glaucoma
Main side effects
Sedation, confusion, agitation
Main drug interactions
-
Concomitant use of opioids with benzodiazepines may cause respiratory depression, hypotension, profound sedation, and death [50].
-
CNS depressants such as phenobarbital
Special points
-
Clonazepam is a long-acting benzodiazepine, with low abuse potential [51]. Clonazepam is not a preferred benzodiazepine for the treatment of insomnia in the elderly, and its use for this purpose should generally be avoided. For DLB patients with RBD, the author recommends initiating treatment with a low dose of 0.25 mg followed by slow titration of 0.25 mg weekly to a dose of 0.5–1 mg at bedtime.
-
Use caution when combining melatonin with the benzodiazepines or avoid if possible. Melatonin can increase benzodiazepine binding to receptor sites. When the benzodiazepine is used for sleep, concomitant use of melatonin may result in increased impairment of attention, memory, and coordination [50].
-
Use caution in patients with obstructive pulmonary disease or obstructive apnea and renal failure.
-
It may worsen cognition and gait.
Ramelteon
Ramelteon is a selective melatonin receptor agonist with very limited evidence (one case series) for treatment of sleep disturbance in DLB [52].
Standard dosage
8 mg at bedtime
Contraindications
Use of ramelteon is not recommended in patients with severe hepatic impairment (Child-Pugh class C).
Use with caution in lactose intolerance or liver impairment.
Main side effects
Somnolence, headache, dizziness, insomnia
Main drug interactions
-
CYP1A2 inducers such as barbiturates, CYP1A2 inhibitors like ciprofloxacin, grapefruit juice, cimetidine [53]
Special points
-
Concurrent use of donepezil and ramelteon results in increased ramelteon exposure.
Emerging concepts
Steady progress in the study of DLB has led to a better diagnostic approach, which means we no longer must solely rely on studies done on AD or PD.
Ligands for detecting dopamine transport activity and beta-amyloid have been developed and those for detecting alpha synuclein are in development, which can further help with early diagnosis. Evidence is building to support EEG as a diagnostic tool and DLB biomarker, not only in patients with dementia [5••, 54] but also MCI stage [5••].
Much attention has been given to prodromal signs and symptoms of Lewy body disease. RBD is a good target to identify those who maybe at a prodromal stage of the disease. Color vision impairment is a new finding, which has been reported in many DLB patients and MCI-DLB patients [2,3,4].
Emerging therapies
Pimavanserin is the first of its class which is FDA approved for treatment of PD psychosis [39•], which may be used for DLB. This selective inverse agonist of 5-HT2A maybe the first of many more to follow in its class.
Nelotanserin is another 5-HT2A inverse agonist that is under study for possible treatment of insomnia [55] and sleep disorders in DLB [56].
Investigational drugs (5-HT6 receptor antagonists) are currently being studied as cognitive enhancers in DLB and other types of dementia [57].
Cannabidiol was reported to reduce the frequency of RBD-related events in four patients with PD, but further studies are needed to confirm if this controlled medication is effective and safe in patients with DLB [58].
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kosaka K, Matsushita M, Oyanagi S, Mehraein P. A cliniconeurophathological study of the “Lewy body disease”. Seishin Shinkeigaku Zasshi. 1980;82(5):292–311.
Tousi B, Flanigan P, Khosravi M. Impaired Color Vision in Patients with DLB or Prodromal DLB. [abstract]. Mov Disord. 2017;32(2). http://www.mdsabstracts.org/abstract/impaired-color-vision-in-patients-with-dlbor-prodromal-dlb/. Accessed September 20, 2017.
Postuma RB, Arnulf I, Hogl B, et al. A single-question screen for rapid eye movement sleep behavior disorder: a multicenter validation study. Mov Disord. 2012;27(7):913–6.
Postuma RB, Gagnon JF, Vendette M, Desjardins C, Montplaisir JY. Olfaction and color vision identify impending neurodegeneration in rapid eye movement sleep behavior disorder. Ann Neurol. 2011;69(5):811–8.
•• McKeith IG, Boeve BF, Dickson DW, et al. Diagnosis and management of dementia with Lewy bodies: fourth consensus report of the DLB Consortium. Neurology. 2017;89(1):88–100. This guideline provides an up to date diagnostic criteria for dementia with Lewy bodies.
Manabe Y, Inui Y, Toyama H, Kosaka K. 123I-Metaiodobenzylguanidine myocardial scintigraphy with early images alone is useful for the differential diagnosis of dementia with Lewy bodies. Psychiatry Res. 2017;261:75–9.
Park KW, Kim HS, Cheon SM, Cha JK, Kim SH, Kim JW. Dementia with Lewy bodies versus Alzheimer’s disease and Parkinson’s disease dementia: a comparison of cognitive profiles. J Clin Neurol. 2011;7(1):19–24.
Noe E, Marder K, Bell KL, Jacobs DM, Manly JJ, Stern Y. Comparison of dementia with Lewy bodies to Alzheimer’s disease and Parkinson’s disease with dementia. Mov Disord. 2004;19(1):60–7.
Calderon J, Perry RJ, Erzinclioglu SW, Berrios GE, Dening TR, Hodges JR. Perception, attention, and working memory are disproportionately impaired in dementia with Lewy bodies compared with Alzheimer’s disease. J Neurol Neurosurg Psychiatry. 2001;70(2):157–64.
Yamamoto E, Mourany L, Colleran R, Whitman C, Tousi B. Utility of Montreal Cognitive Assessment in differentiating dementia with Lewy bodies from Alzheimer’s dementia. Am J Alzheimers Dis Other Demen. 2017;1:1533317517725811.
Aarsland D, Litvan I, Salmon D, Galasko D, Wentzel-Larsen T, Larsen JP. Performance on the dementia rating scale in Parkinson’s disease with dementia and dementia with Lewy bodies: comparison with progressive supranuclear palsy and Alzheimer’s disease. J Neurol Neurosurg Psychiatry. 2003;74(9):1215–20.
Walker Z, Possin KL, Boeve BF, Aarsland D. Lewy body dementias. Lancet. 2015;386(10004):1683–97.
McKeith I. Top cited papers in international psychogeriatrics: 1. Long-term use of rivastigmine in patients with dementia with lewy bodies: an open-label trial. Int Psychogeriatr. 2009;21(1):5. discussion 5-6
• Ikeda M, Mori E, Matsuo K, Nakagawa M, Kosaka K. Donepezil for dementia with Lewy bodies: a randomized, placebo-controlled, confirmatory phase III trial. Alzheimers Res Ther. 2015;7(1):4. This manuscript provides information regarding the first large randomized clinical trial of donepezil in dementia with Lewy bodies.
Mori E, Ikeda M, Nagai R, Matsuo K, Nakagawa M, Kosaka K. Long-term donepezil use for dementia with Lewy bodies: results from an open-label extension of phase III trial. Alzheimers Res Ther. 2015;7(1):5.
Emre M, Tsolaki M, Bonuccelli U, et al. Memantine for patients with Parkinson’s disease dementia or dementia with lewy bodies: a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2010;9(10):969–77.
Stubendorff K, Larsson V, Ballard C, Minthon L, Aarsland D, Londos E. Treatment effect of memantine on survival in dementia with lewy bodies and Parkinson’s disease with dementia: a prospective study. BMJ Open. 2014;4(7):e005158.
Donepezil. http://www.pdr.net. Updated 2017. Accessed Sept 2017.
Rivastigmine. http://www.pdr.net. Updated 2017. Accessed Sept 2017.
Inglis F. The tolerability and safety of cholinesterase inhibitors in the treatment of dementia. Int J Clin Pract Suppl. 2002;127:45–63.
Levodopa. http://www.pdr.net. Accessed Sept 2017.
MHRA. Citalopram 40mg/ml oral drops, solution. www.mhra.gov.uk/home/groups/par/documents/websiteresources/con049076.pdf. Updated 2017. Accessed Sept 2017.
Kosaka K. Diffuse Lewy body disease in Japan. J Neurol. 1990;237(3):197–204.
Forstl H, Burns A, Luthert P, Cairns N, Levy R. The Lewy-body variant of Alzheimer’s disease. Clinical and pathological findings. Br J Psychiatry. 1993;162:385–92.
Hansen L, Salmon D, Galasko D, et al. The Lewy body variant of Alzheimer’s disease: a clinical and pathologic entity. Neurology. 1990;40(1):1–8.
McKeith IG. Consensus guidelines for the clinical and pathologic diagnosis of dementia with lewy bodies (DLB): report of the consortium on DLB international workshop. J Alzheimers Dis. 2006;9(3 Suppl):417–23.
Apaydin H, Ahlskog JE, Parisi JE, Boeve BF, Dickson DW. Parkinson disease neuropathology: later-developing dementia and loss of the levodopa response. Arch Neurol. 2002;59(1):102–12.
Luis CA, Mittenberg W, Gass CS, Duara R. Diffuse Lewy body disease: clinical, pathological, and neuropsychological review. Neuropsychol Rev. 1999;9(3):137–50.
Borroni B, Agosti C, Padovani A. Behavioral and psychological symptoms in dementia with Lewy-bodies (DLB): frequency and relationship with disease severity and motor impairment. Arch Gerontol Geriatr. 2008;46(1):101–6.
Boot BP, Orr CF, Ahlskog JE, et al. Risk factors for dementia with lewy bodies: a case-control study. Neurology. 2013;81(9):833–40.
Breitve MH, Hynninen MJ, Bronnick K, et al. A longitudinal study of anxiety and cognitive decline in dementia with lewy bodies and Alzheimer’s disease. Alzheimers Res Ther. 2016;8:3.
Tousi B, Mourany L. Correlation between neuro-behavioral symptoms, cognition and gait in patients with dementia with Lewy bodies (DLB) [abstract]. Mov Disord. 2016;31(2). http://www.mdsabstracts.org/abstract/correlation-between-neuro-behavioralsymptoms-cognition-and-gait-in-patients-with-dementia-with-lewy-bodies-dlb/. Accessed September 20, 2017.
Factora RM, Tousi B. Don’t forget non-Alzheimer dementias. Cleve Clin J Med. 2014;81(4):243–54.
Thaipisuttikul P, Lobach I, Zweig Y, Gurnani A, Galvin JE. Capgras syndrome in dementia with Lewy bodies. Int Psychogeriatr. 2013;25(5):843–9.
Takahashi H, Yoshida K, Sugita T, Higuchi H, Shimizu T. Quetiapine treatment of psychotic symptoms and aggressive behavior in patients with dementia with lewy bodies: a case series. Prog Neuro-Psychopharmacol Biol Psychiatry. 2003;27(3):549–53.
Kurlan R, Cummings J, Raman R, Thal L. Alzheimer’s disease cooperative study group. Quetiapine for agitation or psychosis in patients with dementia and parkinsonism. Neurology. 2007;68(17):1356–63.
Quetiapine. http://www.pdr.net. Updated 2017. Accessed Sept 2017.
Clozapine. http://www.pdr.net. Updated 2017. Accessed Sept 2017.
• Cummings J, Isaacson S, Mills R, et al. Pimavanserin for patients with Parkinson’s disease psychosis: a randomised, placebo-controlled phase 3 trial. Lancet. 2014;383(9916):533–40. This article provides the results of the pivotal study for pimavanserine as first FDA-approved treatment for neuropsychiatric symptom of a neurodegenerative disease.
Friedman JH. A retrospective study of pimavanserin use in a movement disorders clinic. Clin Neuropharmacol. 2017;40:157–9.
Chwiszczuk L, Breitve M, Hynninen M, Gjerstad MD, Aarsland D, Rongve A. Higher frequency and complexity of sleep disturbances in dementia with lewy bodies as compared to Alzheimer’s disease. Neurodegener Dis. 2016;16(3–4):152–60.
Elder GJ, Colloby SJ, Lett DJ, et al. Depressive symptoms are associated with daytime sleepiness and subjective sleep quality in dementia with Lewy bodies. Int J Geriatr Psychiatry. 2016;31(7):765–70.
Gomperts SN. Lewy body dementias: dementia with Lewy bodies and Parkinson disease dementia. Continuum (Minneap Minn). 2016;22(2 Dementia):435–63.
Prado E, Paholpak P, Ngo M, et al. Agitation and psychosis associated with dementia with Lewy bodies exacerbated by modafinil use. Am J Alzheimers Dis Other Demen. 2012;27(7):468–73.
Lapid MI, Kuntz KM, Mason SS, et al. Efficacy, safety, and tolerability of armodafinil therapy for hypersomnia associated with dementia with Lewy bodies: a pilot study. Dement Geriatr Cogn Disord. 2017;43(5–6):269–80.
Kazui H, Adachi H, Kanemoto H, et al. Effects of donepezil on sleep disturbances in patients with dementia with Lewy bodies: an open-label study with actigraphy. Psychiatry Res. 2017;251:312–8.
McGrane IR, Leung JG, St Louis EK, Boeve BF. Melatonin therapy for REM sleep behavior disorder: a critical review of evidence. Sleep Med. 2015;16(1):19–26.
St Louis EK, Boeve AR, Boeve BF. REM sleep behavior disorder in Parkinson’s disease and other synucleinopathies. Mov Disord. 2017;32(5):645–58.
Aurora RN, Zak RS, Maganti RK, et al. Best practice guide for the treatment of REM sleep behavior disorder (RBD). J Clin Sleep Med. 2010;6(1):85–95.
Clonazepam. http://www.pdr.net. Updated 2017. Accessed Sept 2017.
Schenck CH, Milner DM, Hurwitz TD, Bundlie SR, Mahowald MW. A polysomnographic and clinical report on sleep-related injury in 100 adult patients. Am J Psychiatry. 1989;146(9):1166–73.
Kasanuki K, Iseki E, Nishida Y, et al. Effectiveness of ramelteon for treatment of visual hallucinations in dementia with lewy bodies: a report of 4 cases. J Clin Psychopharmacol. 2013;33(4):581–3.
Ramelteon. http://www.pdr.net. Accessed Sept 2017.
Bonanni L, Thomas A, Tiraboschi P, Perfetti B, Varanese S, Onofrj M. EEG comparisons in early Alzheimer’s disease, dementia with lewy bodies and Parkinson’s disease with dementia patients with a 2-year follow-up. Brain. 2008;131(Pt 3):690–705.
Al-Shamma HA, Anderson C, Chuang E, et al. Nelotanserin, a novel selective human 5-hydroxytryptamine2A inverse agonist for the treatment of insomnia. J Pharmacol Exp Ther. 2010;332(1):281–90.
Wen W, Friedhoff L, Kishnani K, Ramaswamy S, Piscitelli S, Sanchez M, Shanahan W. Safety of nelotanserin in a randomized placebo-controlled phase 2 study [abstract]. Mov Disord. 2016;31(2). http://www.mdsabstracts.org/abstract/safety-of-nelotanserin-in-a-randomizedplacebo-controlled-phase-2-study. Accessed September 20, 2017.
Lombardo I, Ramaswamy G, Piscitelli S, Friedhoff L. The efficacy of RVT-101, a 5-ht6 receptor antagonist, as an adjunct to donepezil in adults with mild-to-moderate Alzheimer’s disease: completer analysis of a phase 2b study. Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association. 2015;11(7):332.
Chagas MH, Eckeli AL, Zuardi AW, et al. Cannabidiol can improve complex sleep-related behaviours associated with rapid eye movement sleep behaviour disorder in Parkinson’s disease patients: a case series. J Clin Pharm Ther. 2014;39(5):564–6.
Acknowledgements
The author thanks Amy Slugg Moore, BA, for her critical reading of the manuscript and editorial support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Babak Tousi has received grants and personal fees from Axovant and Grifols, personal fees from Lilly, and grants from the Alzheimer’s Drug Discovery Foundation and Neuronix.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Dementia
Rights and permissions
About this article
Cite this article
Tousi, B. Diagnosis and Management of Cognitive and Behavioral Changes in Dementia With Lewy Bodies. Curr Treat Options Neurol 19, 42 (2017). https://doi.org/10.1007/s11940-017-0478-x
Published:
DOI: https://doi.org/10.1007/s11940-017-0478-x