Abstract
Purpose of Review
The purpose of this review is to frame the discussion of the potential use of probiotics for the management of rheumatoid arthritis (RA) in the historical and scientific context linking the human microbiota to the etiology, pathogenesis, and treatment of RA. Given this context, the review then details the clinical trials that have been carried out so far that have tried to address the question.
Recent Findings
A variety of laboratory and clinical observations link the flora of the oral cavity and lower gastrointestinal tract with citrullination, as well as immunological alterations that may contribute to the risk of developing RA. Clinical trials to date have been small and mostly short term.
Summary
Statistically significant change in certain disparate clinical endpoints has been reported, but these endpoints have varied from study to study and have been of limited clinical significance. No consistent, robust impact on patient reported, or laboratory outcome measures has emerged from clinical trials so far. There remain theoretical reasons to further investigate the use of probiotics as adjunctive therapies for autoimmune disease, but changes in trial design may be needed to reveal the benefit of this intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The concept that microorganisms play a role in the etiology, pathogenesis, and treatment of rheumatoid arthritis (RA) has been advanced for over one hundred years [1•]. Initial proponents espoused the view that microbes in the oral cavity could play a role in a variety of diseases [2], but millennia before bacteria were discovered, ancient healers speculated about the relationship between oral health and disease elsewhere in the body. Hippocrates himself observed that a case of rheumatism was cured by tooth extraction long before it became fashionable in the early twentieth century to remove teeth as a treatment for RA [3].
Our understanding of the relationship between the bacteria present not only in our mouths but throughout the gastrointestinal tract and elsewhere, the human microbiome, and our state of health and disease has become considerably more sophisticated in recent decades. The human microbiome is a term that encompasses all microorganisms living in and on the human body, as well as the interactions that have arisen from the co-evolution of microbial life with other microbes and with us, their human hosts. In 2008, the National Institutes of Health (NIH) began a large research initiative known as the Human Microbiome Project (HMP) designed to improve our knowledge and understanding of this rapidly growing field. The decades leading up to the launch of the HMP were marked by revolutionary scientific developments advancing molecular approaches to the study of genomics followed by breakthrough data covering the genomic sequences of myriad microorganisms and, finally, of the human genome when the first draft sequence was published in 2001 by two research teams [4, 5]. One of the key findings that emerged from this large international collaboration was the observation that a large number of human genes appeared to have been derived from horizontal transfer of bacteria or from transposable elements at some point in the vertebrate lineage. This information, together with prior estimates of the massive number of bacteria residing in and on the human body, fueled the ongoing drive to better understand the composition, diversity, and relationship of the microorganisms within our bodies. Several years later, the Second Human Genome Project followed, having been called to specifically identify the microbial genomes associated with the human body and to use this data to fill in crucial gaps in knowledge of its potential role in normal human functioning, as well as in the etiology of disease [6].
Of the various microbial communities that our bodies host, the largest resides in the colon. The early studies identifying the human intestinal microbiome exposed its complexity and characterized the remarkable inter-subject variability in gene content and encoded functional attributes [7, 8]. Understanding the metabolic potential associated with these differences among various human populations became a priority in the drive to better predict individual predispositions to certain diseases through misdirected or maladapted host immune responses in the gut. The NIH-led Human Microbiome Project launched more than a dozen case control studies to determine whether there were characteristic microbiomes associated with specific presumed microbiome-associated diseases [9]. These included multiple auto-immune diseases, such as inflammatory bowel disease and psoriasis, and suggested that particular diseases are associated with certain key microbiome functions. Although this type of approach does not prove causality, it has commonly been used to hypothesize a role for the microbiome in disease mechanisms.
The Microbiome and Rheumatoid Arthritis
A more specific link between the microbiome and RA has been postulated on the basis of both animal data and basic science investigations of the microbiome of patients with the disease. The case for a relationship between periodontitis and RA can be made on numerous grounds [10, 11••]. Chronic periodontitis affects over 10% of the world’s population and is a disease in which the commensal microflora on the tooth surface is replaced by a dysbiotic group of bacteria that promote chronic inflammatory destruction of periodontal tissue. Both periodontitis and RA share etiologic links to aging and smoking, as well as pathogenesis based in cytokine-mediated inflammation, tissue breakdown, and bony erosions. Periodontitis arises when Gram negative bacteria, including Porphyromonas gingivalis, Treponema denticola, and Tannerella forsythia, colonize the gingival sulcus, shifting the composition of the local microbiota and provoking an immune response. P gingivalis, the primary periodontal pathogen, has been discovered to uniquely express peptidylarginine deiminase (designated PPAD to distinguish it from human peptidylarginine deiminases, PAD). PPAD can mediate protein citrullination at inflamed periodontal sites that could potentially initiate a cascade of events that culminate in the production of anti-citrullinated protein antibodies (ACPAs) and the clinical picture of RA. Interestingly, the genes that encode PADs have been identified by genome-wide association studies to occur within the RA susceptibility locus. Thus, it had been thought that PADs might lead to increased citrullination of proteins in a gingival cytokine-rich, inflammatory milieu leading to a break in tolerance to citrullinated epitopes presented by specific HLAs. Some, but not all, epidemiologic and case-controlled studies have demonstrated that periodontitis is more prevalent in patients with active RA than in the normal population and that the prevalence of RA is greater in those with periodontitis than those without. Furthermore, recent clinical work has suggested that serum immunity to P gingivalis PPAD can affect the clinical response to biologics used to treat RA [12]. This sort of observation has raised the possibility that interrupting or reversing the shift in the oral microbiota with probiotics could improve outcomes in RA.
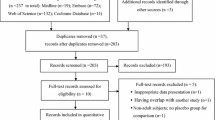
The gut, too, can be a site of dysbiosis and, presumably, citrullination, as well as other potential alterations that heighten the risk of developing RA and other autoimmune diseases [1•, 13, 14]. Studies in mice have shown that the gut microbiota is required for normal immune system maturation and the development of tolerance. Should subsequent breaches in the epithelial barrier of the gut occur, a cascade of responses can result with a potential loss of tolerance. These include engagement of innate immune cells via pattern recognition receptors, cytokine generation, and activation of the adaptive immune system. Both T helper 17 lymphoctyes (Th17) and regulatory T cells (Treg) are found in abundance in the normal gut, and animal studies demonstrate that both alteration of the intestinal microflora and administration of antibiotics can affect Th17 and Treg numbers and function. Gut organisms can induce the expression of IgA-secreting B cells and IgA can, in turn, regulate the composition and function of the gut microbiota. In the collagen-induced arthritis model in mice, susceptibility to the development of arthritis has been related to the species composition of the gut microbiota. Newly diagnosed RA patients, too, may have alterations in the predominant gut bacteria compared to healthy individuals, which may correlate with IL-17 production [15]. Adding to the complexity of the interpretation of these findings is the fact that not all investigators who have explored the question of which gut bacteria are present in RA patients have gotten the same answer. Nonetheless, influencing the composition of the gut microflora as a therapeutic intervention remains intriguing. It has been known for some time that antibiotics might influence the course of RA. Both sulfasalazine [16, 17] and minocycline [18, 19] have been reported to reduce the number of swollen and tender joints and improve laboratory markers of inflammation. Probiotics have been proposed to offer another way in which gut flora could be manipulated to reduce both the risk of developing RA and treating it once diagnosed. A handful of studies (Table 1.) have been published testing the hypothesis of whether ingesting probiotics can alter outcomes in RA.
Clinical Trials
The earliest study to assess the efficacy of probiotics in RA was published in 2003 [20]. The authors suggested that evidence supported a relationship between manipulation of the gut microbiota and the level of disease activity of RA. In this pilot study, 25 RA patients who fulfilled the American Rheumatism Association 1987 criteria for RA [25] were recruited from the outpatient practices of two university hospitals in Finland. Patients were excluded if they were on disease-modifying anti-rheumatic drugs (DMARDs), though these were not specified, sulfasalazine or > 7.5 mg of prednisone daily. Participants were randomized to receive either two capsules of a Lactobacillus rhamnosus product or placebo twice daily for a year. Subjects were evaluated by swollen and tender joint counts, health assessment questionnaire (HAQ), inflammatory markers, pro-inflammatory and anti-inflammatory cytokines, and patient and physician global assessments at 0, 1, 4, 8, and 12 months. The composition of food eaten during the study was assessed by three-day food records on seven occasions. Compliance was assessed by fecal testing for the presence Lactobacillus and for fecal urease as a measure of alteration of the intestinal flora at 0, 1, and 12 months. Five subjects dropped out for unspecified reasons prior to the first follow-up visit. Overall, no statistically significant differences were seen between the intervention and the placebo groups. Both groups had a decline in tender and swollen joints (Lactobacillus group from 8.3 to 4.6; placebo from 5.5 to 4.8). Patient and physician global scores improved in the Lactobacillus group but not significantly. Mean erythrocyte sedimentation rates and C-reactive protein levels were normal to begin with and remained so in both groups. Unexpectedly, the interleukin 1β (IL-1β) levels rose in those treated with Lactobacillus, but there were no significant changes in IL-6, IL-10, IL-12, tumor necrosis factor α (TNF-α), or myeloperoxidase (MPO). This increase in IL-1β was not associated with any detectable change in disease status and was considered clinically insignificant. Fecal sampling showed an increase in the presence of Lactobacillus from a baseline value of 25% in the probiotic group to 86% at one year, suggesting reasonable compliance. A fall in fecal Lactobacillus in the control group from 23% at baseline to 0% was not explained. Furthermore, fecal urease levels increased in both groups but by three times as much in the placebo group (34%) as in the probiotic group (10%). The authors concluded that this L rhamnosus preparation did not alter RA activity. However, they noted that the study was small and included subjects with low disease activity at the outset, making the detection of a difference with treatment difficult. No adverse events were reported.
A different probiotic preparation was studied by a private practitioner in Ohio whose work was funded by the manufacturer of the product [21]. In this pilot study, 45 patients meeting ARA criteria for RA were recruited from the practice. Baseline medications were not specified but subjects were excluded if they were being treated with > 10 mg of prednisolone. Four subjects were noted to not be taking any medication for RA. Participants were randomized to receive either one caplet of a Bacillus coagulans product or placebo once daily for two months. They were evaluated at baseline and at one and two months using the American College of Rheumatology (ACR) criteria, HAQ, patient global, physician global, total painful joints, total swollen joints, ESR, and CRP, as well as functional parameters. At the conclusion of the trial, eight of 22 subjects in the Bacillus group and six of 22 in the placebo group attained an ACR20 response. The only statistically significant difference between the Bacillus and placebo-treated groups was a difference in the means of an unspecified pain scale (p = 0.46). Reported adverse events included an upper respiratory tract infection requiring antibiotic treatment that resulted in the participant dropping out of the trial. Other events (shingles, poison ivy, cold, leg edema, reflux, urinary tract infection) were thought to be unrelated to the use of the experimental product.
A year later, a group from the University of Western Ontario, reported on the use of a product containing both Lactobacillus ramnosus and L reuteri [26]. Participants were recruited from a health center rheumatology clinic. They met ACR criteria for the diagnosis of RA, had at least four swollen and tender joints, and were on stable DMARDs, steroids and nonsteroidal anti-inflammatory drugs (NSAIDs) for a month prior to enrollment. They could not have received an intra-articular steroid injection in the month prior. No further information on the medications used by subjects was given. Fifteen individuals were randomized to receive the Lactobacillus preparation and 14 to the placebo group. During the trial, the subjects took one capsule of study drug or placebo twice daily for three months. Participants were assessed at days 0, 45, and 90 for swollen and tender joint counts, HAQ, patient global score, visual analog score for pain, ESR, CRP, and a variety of cytokines. As with previous studies, the investigators concluded that, overall, probiotics had no beneficial effect in the management of RA. They found that there was no statistically significant difference between how many subjects in each group achieved an ACR20 response (three in Lactobacillus, one in placebo), their primary outcome measure. Participants treated with the probiotic had 9.5 swollen joints and 13.6 tender joints at the outset and 9.1 swollen joints and 13.7 tender joints at the completion of the trial, which did not differ from the results in the placebo group. There were no significant differences in levels of IL-1α, IL-1β, KL-6, IL-8, TNF-α, IL-12p70, IL-15, IL-10, GM-CSF, C-CSF, IL-17, sCD40 ligand, MIP-1α, MIP-1β, or MCP-1 though, interestingly, both groups showed declines in pro-inflammatory cytokines. The only positive trend was a within group improvement in HAQ in the probiotic group. The authors interpreted this as in line with the finding in the Finnish study that well-being measured by global scores trended positively. No adverse events occurred. The investigators noted that, by requiring an active joint count, they may have selected for patients with chronic, rather than acute, synovitis that was not likely to change and that they may have evaluated patients over too short a time span.
A final study of probiotics for RA was carried out by a group of investigators from Iran and results were reported in a series of three publications [22, 23, 27]. Sixty women were recruited over a three-month period from a rheumatology clinic and a general clinic in Tabriz. They met ACR criteria for the diagnosis of RA with a duration of greater than one year and had “inactive to moderate levels of disease”. Subjects were on methotrexate, hydroxychloroquine, and < 10 mg of prednisolone, but not NSAIDs or biologics, and were without change in their medication for 3 months prior to the trial. Participants took one capsule once daily containing a Lactobacillus casei preparation or placebo for 2 months. All participants were told that they were receiving probiotic capsules. Subjects were assessed at the outset and at the end of the study for swollen and tender joints, the Disease Activity Score 28 (DAS28), patient global score, high sensitivity CRP, cytokine levels, dietary intake measured by dietary recall at the beginning and end of the study, and six food questionnaires throughout the course of the study. Fourteen participants dropped out for unspecified reasons, leaving 22 in the probiotics group and 24 in the placebo group. While statistically significant changes were reported for many parameters, the magnitude of these changes and their clinical significance might be questioned. For instance, in the probiotic group, mean hs-CRP (normal 0–3 mg/L) fell from 3.1 to 2.8 mg/L, while in the control group, it rose from 2.3 to 3.5 mg/L (p = 0.001). The mean number of tender joints was reported as zero at the start and end of the study for both groups but the mean difference was reported to be statistically significant (p = 0.026). Placebo recipients had a mean of a single swollen joint at the beginning and end of the study; probiotic recipients had a mean of zero at both time points and this difference was reported as significant (p = 0.034). No subject in either group had a good response measured by European League Against Rheumatism (EULAR) criteria. A significantly higher number of low disease activity (DAS28 < 3.2) probiotic group members had a moderate EULAR response (four) than did placebo group members (none) (p = 0.03). A higher number of moderate disease activity (DAS28 > 3.2–< 5.1) probiotic group members also had a moderate EULAR response (four) than did placebo group members (one), but the difference was not significant (p = 0.19). However, the minimum important difference in the DAS28 is often defined as 1.2 units [28], while the mean change for the probiotic group was 0.49 and for the control group 0.09 units. Unlike prior studies, some significant differences in cytokine levels emerged. The probiotics groups had a significant decline IL-6, IL-12, TNFα, and IL-10 (p < 0.05) compared to placebo and the percent decrease was significantly greater for IL-12 and TNF-α (p < 0.05). The authors noted that their study differed from all previous studies in that clinical and biochemical measures showed significant differences attributable to probiotic use. They suggested that this might be due to the use of the different strain or lower dose of Lactobacillus which might have resulted in a different immunological effect. They concluded that their preparation may help improve disease activity and inflammatory cytokines in RA.
Two subsequent publications highlighted additional data obtained on this same group of Iranian women. In a 2014 report [23], the 23% drop out rate was noted to be due to being unwilling to participate, going on vacation, moving or protocol violations. Newly reported were state and trait anxiety and physical activity measures and energy and macronutrient intake (protein, fat, poly- and mono-unsaturated fatty acids, fiber) which did not differ between groups or vary during the study in either the intervention or control group. In a 2016 report [27], measures of oxidative stress (serum malondialdehyde, total antioxidant capacity, erythrocyte superoxide dismutase, glutathione peroxidase, catalase) and micronutrients (vitamins A, E, C, B6, iron, zinc, cooper, selenium calcium, phosphorus) were similarly shown to be unaffected by treatment with the L casei preparation.
A second Iranian group reported on the use of a different probiotic containing Lactobacillus acidophilus, Lactobacillus casei, and Bifidobacterium bifidum [24]. Outcome measures in this study reflected the authors’ interest in previously published evidence that changes in intestinal microbiota and resultant immune dysregulation could be linked to autoimmune disease that insulin resistance and oxidative stress could be involved in the pathogenesis of RA, and that patients with RA have increased risk of cardiovascular disease and diabetes. They enrolled 60 patients with RA from outpatient rheumatology and internal medicine practices at a university hospital in Kashan. Patients met the ACR criteria for the diagnosis but, in contrast to previous studies, had moderate to severe disease as measured by DAS28 (> 3.2). More than 90% of patients were taking methotrexate and prednisolone and about 70% were also taking hydroxychloroquine at entry. All participants took one capsule daily of either probiotic or placebo for two months, in addition to their usual medications. At baseline and completion, tender and swollen joint counts, VAS for pain, DAS28, and a variety of blood tests were assessed. The DAS28 improved in both groups (probiotic 4.0 ± 0.7 to 3.7 ± 0.7, p < 0.001; control 4.1 ± 0.7 to 4.0 ± 0.7, p = 0.31) and the improvement was statistically significantly better in the probiotic group than in the placebo group (p = 0.01) but did not represent a clinically meaningful change in either group. There was no significant change in the number of tender or swollen joints. The hs-CRP fell in the probiotic group (7.27 ± 6.24 to 6.61 ± 6.03, p = 0.25) and rose in the control group (6.02 ± 5.78 to 9.09 ± 7.46, p = 0.001) and the difference was statistically significant (p < 0.001). The insulin level and homeostatic model assessment B (HOMA-B), a measure of beta cell function, declined in the probiotic group and rose in the control group (p = 0.3). There were no significant changes in VAS pain, fasting glucose, HOMA-estimated insulin resistance (HOMA-IR), quantitative insulin sensitivity check index, total, LDL, HDL or VLDL cholesterol, triglycerides, nitric oxide, total antioxidant capacity, total glutathione, or malondialdehyde. No adverse effects were seen. The authors concluded that a two-month course of probiotics could be beneficial in RA patients.
Conclusion
A limited number of studies have investigated the role of probiotics in the management of RA in human subjects. As the volume of data has expanded concerning the positive effects of probiotics in animal models of arthritis, so has the desire to translate these benefits into human clinical practice. As reviewed in this article, the data that exist regarding probiotic supplementation in the management of RA patients provide little definitive evidence of efficacy. Only a very limited number of outcome measures have been positively affected by the use of probiotics in trials carried out so far. And, given the small number of participants and short duration of most trials, most must be considered pilot studies awaiting confirmation. Nevertheless, the broad, worldwide interest in enhancing our understanding of the beneficial role of the massive population of organisms that reside on and in us will likely continue to drive the search for new ways to manipulate that population to improve human health.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Scher JU, Abramson SB. The microbiome and rheumatoid arthritis. Nat Rev Rheumatol. 2011;7:569–78. Provides both historical perspective and up to date summary of links between the gastrointestinal tract and experimental arthritis and human disease.
Hunter W. Oral sepsis as a cause of disease. Br Med J. 1900;2:215–6.
O’Reilly PG, Claffey NM. A history of oral sepsis as a cause of disease. Periodontology. 2000;23:13–8.
Venter JC, Adams MD, Myers EW, Li PW, Mural RJ, Sutton GG, et al. The sequence of the human genome. Science. 2001;291:1304–51.
International Human Genome Sequencing Consortium. Initial sequencing and analysis of the human genome. Nature. 2001;409:860–921.
Relman DA, Falkow S. The meaning and impact of the human genome sequence for microbiology. Trends Microbiol. 2001;9:206–8.
Eckburg PB, Bik EM, Bernstein CN, Purdom E, Dethlefsen L, Sargent M, et al. Diversity of the human intestinal microbial flora. Science. 2005;308(5728):1635–8.
Gill SR, Pop M, Deboy RT, Eckburg PB, Turnbaugh PJ, Samuel BS, et al. Meta- genomic analysis of the human distal gut microbiome. Science. 2006;312(5778):1355–9.
Proctor LM. The National Institutes of Health Human Microbiome Project. Semin Fetal Neonatal Med. 2016;21:368–72.
Rosenstein ED, Greenwald RA, Kushner LJ, Weissmann G. Hypothesis: the humoral immune response to oral bacteria provides a stimulus for the development of rheumatoid arthritis. Inflammation. 2004;28:311–8.
•• Potempa J, Mydel P, Koziel J. The case for periodontitis in the pathogenesis of rheumatoid arthritis. Nat Rev Rheumatol. 2017;13(10):606–620. Recent summary of data supporting the hypothesis that links periodontitis to the pathogenesis of rheumatoid arthritis.
Kobayashi T, Ito S, Kobayashi D, Shimada A, Narita I, Murasawa A, et al. Serum immunoglobulin G levels to Porphyromonas gingivalis peptidylarginine deiminase affect clinical response to biological disease-modifying antirheumatic drug in rheumatoid arthritis. PLoS One. 2016;11:e0154182.
de Oliveira GLV, Leite AZ, Higuchi BS, Gonzaga MI, Mariano VS. Intestinal dysbiosis and probiotic applications in autoimmune diseases. Immunology. 2017;152:1–12.
Sandhya P, Danda D, Sharma D, Scaria V. Does the buck stop with the bugs?: an overview of microbial dysbiosis in rheumatoid arthritis. Internat J Rheum Dis. 2016;19:8–20.
Kang Y, Cai Y, Zhang X, Kong X, Su J. Altered gut microbiota in RA: implications for treatment. Z Rheumatol. 2017;76:451–7.
Hannonen P, Mottonen T, Hakola M, Oka M. Sulfasalazine in early rheumatoid arthritis. A 48-week double-blind, prospective, placebo-controlled study. Arthritis Rheum. 1993;36(11):1501–9.
Weinblatt ME, Reda D, Henderson W, Giobbie-Hurder A, Williams D, Diani A, et al. Sulfasalazine treatment for rheumatoid arthritis: a meta-analysis of 15 randomized trials. J Rheumatol. 1999;26(10):2123–30.
O’Dell JR, Paulsen G, Haire CE, Blakely K, Palmer W, Wees S, et al. Treatment of early seropositive rheumatoid arthritis with minocycline: four-year follow-up of a double-blind, placebo-controlled trial. Arthritis Rheum. 1999;42(8):1691–5.
O’Dell JR, Blakely KW, Mallek JA, Eckhoff PJ, Leff RD, Wees SJ, et al. Treatment of early seropositive rheumatoid arthritis: a two-year, double-blind comparison of minocycline and hydroxychloroquine. Arthritis Rheum. 2001;44(10):2235–41.
Hattaka K, Martio J, Korpela M, Herranen M, Poussa T, Laasanen T, et al. Effects of probiotic therapy on the activity and activation of mild rheumatoid arthritis—a pilot study. Scand J Rheumatol. 2003;32:211–5.
Mandel D, Eichas K, Holmes J. Bacillus coagulans: a viable adjunct therapy for relieving symptoms of rheumatoid arthritis according to a randomized, controlled trial. BMC Complement Altern Med. 2010;10:1–7.
Alipour B, Homayouni-Rad A, Vaghef-Mehrabany E, Sharif SK, Vaghef-Mehraany L, Asghari-Jafarabadi M, et al. Effects of Lactobacillus casei supplementation on disease activity and inflammatory cytokines in rheumatoid arthritis patients: a randomized double-blind clinical trial. Int J Rheum Dis. 2014;17:519–27.
Vaghef-Mehrabany E, Alipour B, Homayouni-Rad A, Sharif SK, Asghari-Jafarabadi M, Zavvari A. Probiotic supplementation improves inflammatory status in patients with rheumatoid arthritis. Nutrition. 2014;30:430–5.
Zamani B, Golkar HR, Farshbaf, S, Emadi-Baygi M, Tajabadi-Ebrahimi M, Jafari P, et al. Clinical and metabolic response to probiotic supplementation in patients with rheumatoid arthritis: a randomized, double-blind, placebo-controlled trial. Int J Rheum Dis. 2016;19(9):869–179.
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31(3):315–24.
Pineda M, Thompson SF, Summers K, de Leon F, Pope J, Reid G. A randomized, double-blinded, placebo-controlled pilot study of probiotics in active rheumatoid arthritis. Med Sci Monit. 2011;17(6):CR347–54.
Vaghef-Mehrabany E, Homayouni-Rad A, Alipour B, Sharif SK, Vaghef-Mehrabany L, Alipour-Ajiry S. Effects of probiotic supplementation on oxidative stress indices in women with rheumatoid arthritis: a randomized double-blind clinical trial. J Am Coll Nutr. 2016;35(4):291–9.
Van der Heijde D, Keystone EC, Curtis JR, Landewe RB, Schiff MH, Khanna D, et al. Timing and magnitude of initial change in disease activity score 28 predicts the likelihood of achieving low disease activity at 1 year in rheumatoid arthritis patients treated with certolizumab pegol: a post-hoc analysis of the RAPID 1 trial. J Rheumatol. 2012;39:1326–33.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Complementary and Alternative Medicine
Rights and permissions
About this article
Cite this article
Schorpion, A., Kolasinski, S.L. Can Probiotic Supplements Improve Outcomes in Rheumatoid Arthritis?. Curr Rheumatol Rep 19, 73 (2017). https://doi.org/10.1007/s11926-017-0696-y
Published:
DOI: https://doi.org/10.1007/s11926-017-0696-y