Abstract
Purpose of Review
To examine current trends in suicide and self-injury in the USA, as well as potential contributors to their change over time, and to reflect on innovations in prevention and intervention that can guide policies and programs to reduce the burden of suicide and self-injury in the USA.
Recent Findings
Suicide and non-fatal self-injury are on the rise in the USA. Reasons for such trends over time remain speculative, although they seem linked to coincident increases in mood disorders and drug use and overdose. Promising innovative prevention and intervention programs that engage new technologies, such as machine learning–derived prediction tools and computerized ecologic momentary assessments, are currently in development and require additional evidence.
Summary
Recent increases in fatal and non-fatal self-harm in the USA raise questions about the causes, interventions, and preventive measures that should be taken. Most innovative prevention efforts target individuals seeking to improve risk prediction and access to evidence-based care. However, as Durkheim pointed out over 100 years ago, suicide rates vary enormously between societal groups, suggesting that certain causal factors of suicide act and, hence, should be targeted at an ecological level. In the next generation of suicide research, it is critical to examine factors beyond the proximal and clinical to allow for a reimagining of prevention that is life course and socially focused.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Suicide continues to be a central contributor to lives lost across the globe and among the most common causes of death, especially in young adults. The sequelae of suicide for families and communities reverberate in grief, stigma, and increases in psychiatric conditions. The present paper outlines current trends in suicide and self-injury in the USA, as well as hypotheses and evidence regarding contributors to changes over time in the suicide rate. Further, we examine evidence for innovations in prevention and intervention that can guide policies and programs to reduce the burden of suicide and self-injury in the USA.
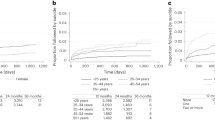
Trends in Suicide and Non-fatal Self-Injury Among Adolescents and Adults
Suicide rates in the USA were generally declining among most age groups of adults throughout the late 1980s and 1990s [1]. However, since 1999, suicide rates began to increase in almost all states and in almost every age group. Analyses from the CDC indicate that from 1999 to 2016, suicides significantly increased in 44 of 50 US states and that the rate of increase was heterogeneous by location and demographics [2]. For example, suicide increased by more than 30% in 25 states, with the highest increase in suicide occurring in North Dakota (an increase of 57.6%). However, states such as Nevada, which already had the highest rates of suicide in the country, did not observe a significant increase [2]. Trends towards increased suicide rates continued in 2017 [3], as the overall suicide rate in the USA increased from 13.5 per 100,000 to 14.0 per 100,000.
While the rate of suicide is increasing across all age and gender groups, there have been particularly high absolute increases in suicide among men aged 45 to 64 (https://www.cdc.gov/nchs/data/databriefs/db241.pdf). Relative increases in suicide are greatest among those at young ages, due in part to a lower overall base rate. For example, the suicide rate among girls aged 10–14, among whom the suicide rate was 0.5 per 100,000 in 1999, tripled by 2016 [4••]. Suicide is currently the second leading cause of death among those aged 10–14, 15–24, and 25–34, with unintentional injury being the leading cause of death, indicative of the contribution of both unintentional injury and suicide to the declining life expectancy in the USA, given the young age of decedents (https://www.nimh.nih.gov/health/statistics/suicide.shtml).
Available evidence indicates that regions of the USA with high suicide rates and high correlation among suicides per geographic area are those with high elevation [5], as well as those with high concentrations of demographic groups at risk of suicide such as those with indigenous populations (https://www.cdc.gov/mmwr/volumes/67/wr/mm6708a1.htm). Further, the strength of correlation among suicides in particular geographic areas over time is also increasing, suggesting that as suicides become more common, the overall size of areas with particular high suicide rates is also increasing [6]. Occupational exposures also influence suicide: the risk is markedly salient among members of the US military, especially those exposed to active combat and traumatic events in the field [7]. While members of the military historically had lower death rates than the general population, including suicide, death by suicide increased among US army members beginning in 2004 [8], and rates are now approximately equal to the general population, due to the unprecedented increases among both civilians and military members [9].
The increasing trends in completed suicide lead to the question of whether there are increases in non-fatal self-injury as well, or whether the trends reflect rather lethality of attempts. Available data indicate that non-fatal self-injury is also increasing in the USA across age. Olfson et al. examined self-reported suicide attempts across two cross-sectional surveys of adults completed 10 years apart with similar sampling frames and measures and found modest increases in the rate of self-reported attempted suicide, from 0.62% in 2001–2001 to 0.79% in 2012–2013 [10••]. Across demographic and clinical groups, those with the highest increases included young adults aged 21–34, those with high school or less education, and those with psychiatric disorders. Hospital-treated self-harm events increased from 5.1 to 7.1 per 10,000 population from 2001 to 2011 among middle-aged individuals, an increase larger than any other age group [11]. Other analyses of hospitalization data also demonstrate increasing trends in self-injury [12,13,14].
Non-fatal self-injury is increasing among youth. The prevalence of adolescents reporting that they “seriously considered attempting suicide” in the past 12 months in the USA increased from 14.5% in 2009 to 17.2% in 2017, an increase that was statistically significant (https://www.cdc.gov/healthyyouth/data/yrbs/pdf/trends/2017_suicide_trend_yrbs.pdf). However, it should be noted that overall trends since the mid-1990s suggest declines (e.g., prevalence was 29% in 1991). Emergency department visits and inpatient hospitalizations coded for suicidal ideation or attempt across 49 children’s hospitals in the USA increased from 0.66% of all encounters in 2008 to 1.82% in 2015 [15], and significant increases were observed across age, gender, and race, with the largest increases observed for 12–14 and 15–17 year olds, girls, and non-Hispanic whites. Further, among youth less than age 18 in the USA, emergency department visits coded for suicide attempts and suicidal ideation doubled between 2007 and 2015, from 580,000 to 1.12 million, with no corresponding increase in total emergency department visits [16].
Trends in Mood Disorders Among Adolescents and Adults
Mood disorders, particularly depression, are strong risk factors for self-injury and suicide. Psychiatric autopsy studies of suicide decedents compared with living controls range in the prevalence of mood disorders, with a median estimate based on systematic review of 59% (range from 30 to 93%) [17]. Meta-analytic estimate from 3275 suicide decedents indicated a pooled prevalence of affective disorders, including depression and bipolar disorders, of 43.2% [18]. Prospective data from the Danish registry among those with contact with the health system for a psychiatric disorder found an absolute risk of suicide after first contact of 6.67% [19]. Given the increased risk of suicide associated with depressive and other affective disorders, it is also worth interrogating the evidence for recent increases in mood disorders.
Mood disorders are substantially increasing in recent years among adolescents, especially adolescent girls. Mojtabai et al. found that the prevalence of DSM-IV major depressive episodes increased from 8.7% in 2002 to 11.3% in 2014 (P < 0.001), with a greater increase among girls than boys [20]. Updated analyses of NSDUH through 2017 have demonstrated a continued upward trajectory of MDE among girls [21••]. Independent data sources confirm that depressive symptoms have increased among girls in national representative US studies, compared with no significant change among boys [22••]. These national studies are augmented in building the evidence by other studies among young adults, particularly those in college, among whom data indicate that anxiety and depressive disorders are increasing across the past decade [23, 24].
The increases in the prevalence of affective disorders in general population samples among adolescents are notable given the recent history of this epidemiology. Sales of prescription medication to treat depressive and related mood disorders, among both adolescents and adults, increased substantially starting in the mid-1990s [25], as did outpatient visits to psychiatric clinics for treatment of depression [26, 27]. These increases prompted questions about whether mood disorders were increasing, or whether identification and ascertainment of cases for treatment were increasing without any change in the underlying incidence and prevalence. Available reviews and meta-analyses published in the mid-2000s found no evidence for increasing incidence and prevalence of mood disorders in the community when prospective studies were analyzed [28, 29]. These reviews, however, were published before the recent, cross-study-consistent increases in mood disorders in general population samples, which began around 2010, suggesting that a new evidence base is needed as we enter a new era of mood disorders among US adolescents.
Evidence regarding changes in affective disorders among adults is more mixed, but suggested sustained increases are occurring predominately among those with low socio-economic status. Case and Deaton found that among middle-aged men with low education, the prevalence of non-specific psychological distress has been historically increasing from 1997–1999 to 2011–2013 [30]. Goldman et al. documented that life satisfaction, positive affect, and psychological well-being decreased from 2011 to 2014 compared with 1995–1996, and negative effect increased, but only for those who are socio-economically disadvantaged [31]. National survey data conducted annually has documented recent increases in psychological distress among adults and increases in major depressive episodes that are small in magnitude and primarily confined to young adults [21••], especially those with low levels of socio-economic status [20, 21••, 32]. These results are supported by other national data also documenting increases in moderate and severe depressive episodes, primarily among those with the lowest levels of education [33]. The range of increases is small, between 1 and 3 percentage points, and inconsistent across all levels of the life course, suggesting that continued surveillance is needed to determine whether these increases reflect temporary and time-limited noise in the data, or whether there is a sustained increase that may underlie changes in suicide risk in the USA.
Why Are Suicide Rates Increasing Among Adolescents and Adults?
The increases in suicide rates are occurring coincident with increases in mood and affective disorders among adolescents and, to an extent that is less well established, among adults. The reasons that these disorders are increasing in the population, as well as other potential reasons underlying suicide death, remain speculative. Suicide rates are increasing in tandem with unintentional injury deaths more broadly particularly due to opioid overdose, which was exponentially increasing since approximately 1999 in the USA (https://www.cdc.gov/nchs/data/health_policy/AADR_drug_poisoning_involving_OA_Heroin_US_2000-2014.pdf) [34], around the same time that suicides began increasing [35••]. Opioid overdose and suicide deaths share demographic correlates such as a greater preponderance of males, indigenous populations, and those in middle age, but the trends are to some extent discordant, given that there are different demographic groups that have had the largest increase in suicide compared with opioid overdose. Yet, some mechanisms linking the two epidemics could be that opioid use disorders increase both risk of overdose and suicide; available evidence finds that suicide among medical users of opioids increases with opioids dose [36], that communities ravaged by opioid overdoses may have collective trauma and psychological distress that would increase risk of suicide [37•], and that the availability of opioids could lead to greater access to lethal means. On the last point, there is limited evidence; currently, poisoning accounts for a minority of suicides in the USA (14.7% in 2015), and a minority of those poisoning suicides involved opioids [2]. That said, the number of deaths categorized as unintentional opioid overdoses that might have been suicides is difficult to adjudicate, given that the intentionality of death can be difficult to determine, especially among those with opioid use disorders which can increase the risk of suicidality.
Some have advanced the hypothesis that the increases in suicides, as well as overdose, alcohol consumption, and deaths due to alcohol, especially among middle-aged men and those with low educations, are the outcome of a long process that has included the erosion of a middle class with job stability for low-skill work, among other economic factors that may bring meaning to the lives of the working class [2, 37]. While such hypotheses are provocative, available analyses have largely been unable to provide compelling evidence. In a working paper by Ruhm [38], known measures of county economic decline such as home prices and unemployment predicted suicide, but explained less than 1% of the variation in rates over time. Further, Masters et al. reanalyzed vital statistics data by gender, age, and birth cohort and concluded that drug overdose rates increased across a wide range of age groups, especially those in young and middle adulthood, and did not mirror trends for other “despair”-related death such as suicide, suggesting that the drivers of opioid-related deaths in the USA were factors that could influence a broad range of age groups simultaneously, but may be separate from mechanisms that increase suicide rates [39].
Suicides would also be expected to increase with increased access to lethal means. The leading method of suicide in the USA is with a firearm, responsible for 56.6% of male suicides in 2015 and 32.1% of female suicides. Among men, suffocation is second most common with 26.1% of suicides, followed by poisoning (9.5%). Among women, poisoning is slightly more common than firearms as a means of suicide, at 33%, followed by suffocation, responsible for 25.3%. While firearms represent a plurality of suicide deaths in the USA, available data suggest that firearm ownership is decreasing in the USA, rather than increasing [40]. Further, comparing causes of suicide death between 1999–2007 and 2008–2015, while increases in suicide occurred for both firearm and suffocation suicides, the absolute and relative increase was higher for suffocation than for firearm suicides (https://www.cdc.gov/mmwr/volumes/66/wr/mm6610a2.htm). There is no evidence to suggest that means to suffocation are increasing in the USA; thus, increases in access to lethal means do not currently explain increases in suicide in the USA.
Innovations in Individual-Level Suicide Prevention: the Who and the When of Suicide Risk
Decades of research aimed at the identification of individuals at high risk of fatal and non-fatal self-harm have yielded an array of biological [41,42,43], behavioral [44], and social [45, 46] risk factors that decision-makers use, combined, for intervention purposes. However, suicide risk factor identification has contributed minimally to effective prevention efforts, and suicide risk reduction remains a largely unmet clinical need. Even the most widely used risk assessment scales, largely based on suicide risk factors, lack enough sensitivity, specificity, and predictive value to be clinically meaningful [47]: used alone, these scales are not useful to estimate an individual’s future risk of suicide [48].
A well-known reason for the lack of impact of suicide risk factor identification on suicide prediction is what Hawton termed a “base-rate problem” [49••] that leads to an excess of false positives in the clinical practice: on the one hand, most accepted risk factors for suicide, such as mood and substance abuse disorders or interpersonal conflict, are highly prevalent. On the other, suicide behaviors and specially death by suicide are relatively rare events over the lifetime of those classified as high risk. As a result, most people classified as “high risk” will never die by suicide, and a considerable amount of suicides will take place among people classified as “low risk,” as proved by substantial evidence from prospective studies. In 1983, Pokorny reported that, among a cohort of 4800 veterans, only 3.7% of high-risk predictions corresponded with true positives, and more than half of suicides took place in low-risk patients [50], a finding that has been replicated several times [51,52,53].
Notwithstanding, psychiatrists remain entrusted to conduct suicide risk assessments in a scientifically sound manner—e.g., using risk factors and scales, a phenomenon that Undrill sees as an approach to the management of the “institutional anxiety” suicide risk generates [54]. Notably, Mulder et al. have argued that risk categorization is not only clinically futile but also potentially harmful, in that it may “confuse clinical thinking” and lead to more coercive treatment options for those labeled “high risk” and a parallel misallocation of treatment intensity for those labeled “low risk” [55].
In the recent years, substantial attention within the field of suicide prediction has shifted towards new machine learning algorithms, derived from large databases of electronic health records. Tools derived from regression trees, neural networks, and other machine learning approaches have been shown repeatedly to outperform clinicians’ predictive assessments, generating new hopes in the suicide prevention field. Notable examples include Kessler and colleagues’ study featuring over 50,000 American soldiers discharged after a hospitalization [56], DelPozo-Banos et al.’s study using more than 2600 suicide cases and 52,000 paired controls from the UK [57], or Simon and colleagues’ study featuring 2,960,929 patients from seven American healthcare systems [58].
Critics with machine learning–derived predictive tools usually point out limitations regarding generalizability to different settings and transparency in the model developing process. The generalizability of predictions based on complex, data-driven statistical approaches tends to depend on how similar the training dataset is to the new population in terms of variable distribution—different populations often require different model calibrations. In a comprehensive review, Belsher et al. simulated the variation of the positive predictive value of a series of machine learning algorithms for suicide prediction when implemented in hypothetical populations with different suicide rates, reporting high classification accuracy but an extremely low predictive validity in most populations [59]. This finding has somewhat “deflated some of the exaggerated hopes” associated with big data analyses and machine learning statistical methods [60] and, more importantly, emphasized the need for more accurate data recording in the clinical practice, wide availability of training datasets when legally possible, and transparent sharing of the exact analytic methods used in order to enhance the recalibration of a model before implementing it in a different population [61].
Another, less explored explanation for the lack of clinical impact of suicide risk assessments is that little is known about when this risk is higher, although time-related considerations would provide key insights for intervention planning. Most consistently accepted risk factors correspond to correlates that either remain stable over time, such as gender or family history of suicide [62], or take long periods of time to establish and eventually resolve, like most psychiatric diagnoses or a disadvantaged socio-economic status [63]. However, suicide risk factors interact over time in complex hierarchical networks that are inherently difficult to capture using solely long-term assessments of the relation between baseline characteristics and subsequent suicide. For example, while people with schizophrenia with a low premorbid life adjustment tend to show high suicide rates right after the onset of the disease, their long-term suicide risk is low, as compared with counterparts with a better premorbid adjustment [64, 65]. In order to effectively act on suicide risk, we need to better understand short-term suicide risk factors and how they vary over time.
Suicidal ideation (SI), largely targeted as a way to prevent suicide as it usually precedes suicidal behaviors [66], is probably the most important time-varying risk factor for suicide. SI includes a spectrum of different experiences that range from passive ideas of death, through structured suicidal ideation, to the urge to attempt self-harm [67]. Most studies have measured suicidal thoughts using single-time-point measures, although recent evidence shows that SI undertakes dramatic within-person variations over short periods of time [68••]. Because single-point measures, like retrospective questionnaires, fail to capture such variation, past research has yielded interestingly mixed results. For example, while Kessler et al. estimated the risk of transition as 26% from ideation to an attempt and as 72% from a plan to an attempt [66], Baca-Garcia et al. found that passive and active suicidal ideation entailed the same lifetime suicide attempt risk [69], and Lee et al. estimated that, among suicidal ideators, making an attempt was in fact more frequent than planning it [70].
New technologies provide innovative measures of time-varying real-world determinants of suicide. In particular, computerized ecologic momentary assessment (EMA) allows for data collection “in the natural contexts of daily life” [71]. This technique measures participant’s domains of interest (whether these are emotions, cognitions, or behaviors) repeatedly, usually through smartphone-delivered assessments that can follow a timely schedule, or depend on the occurrence of a predefined behavior, or using both [72, 73••]. Hence, EMA assesses exposures and outcomes in a real-time, real-world manner and can accurately characterize daily suicidal thoughts and their external and internal triggers [74]. In addition, EMA assessments are technically feasible, enhance the participants’ compliance, and do not reactivate their negative thoughts [71]. Recent studies using this technology have successfully characterized the mentioned variation in suicidal thoughts that high-risk individuals can experience over short periods of time [75] and linked it to predictors such as life challenges and inner affect state changes [76, 77].
Apart from improving our ability to accurately determine who is at risk and when is this risk higher, the potential impact of suicide prevention efforts relies greatly on the development, implementation, and scalation of effective prevention strategies. Despite remaining key knowledge gaps, certain clinical strategies are considered effective and recommended, especially among specific subsamples of psychiatric patients with increased suicide risk [78,79,80]. With respect to pharmacotherapy, clozapine [81,82,83] and lithium [84,85,86] show the most promising results for preventing suicide attempts among people with schizophrenia and bipolar disorder, respectively.
Psychosocial strategies for suicide risk reduction among people at high risk often fall within two categories: interventions directed specifically towards suicide risk and interventions aimed at intensifying their contact with mental health care providers. Among the first group, several psychotherapeutic interventions have been shown to decrease the intensity and frequency of suicidal thoughts and/or behaviors, either among all people undergoing mental health struggles or when tailored for clients with specific psychiatric diagnoses [87,88,89]. In general, these interventions enhance the client’s ability to cope with suicidal thoughts through the acquisition and strengthening of specific strategies and skills. However, psychotherapy for suicide behaviors has been called into question when compared with more feasible programs aimed at simply enhancing contact maintenance with providers over a sustained period of time [90]. For example, in a recent RCT meta-analysis, the WHO Brief Intervention and Contact (BIC), a program of 9 follow-up contacts significantly lowered the odds of suicide after an attempt by 80%, whereas cognitive-behavioral therapy (CBT) was not significantly protective [91].
A key target for contact enhancement strategies is patients discharged from the hospital following a suicide attempt, because they entail an exceptionally high risk of subsequent suicide attempt and completion [92], and they tend to experience barriers in their access to proper, outpatient mental healthcare, favoring loss of adherence during follow-up [93]. Motto and Bostrom pioneered this method by randomly assigning 843 patients who refused follow-up visits to either receiving a total of 24 letters over the following 5 years or a control group [94]. Two years after inclusion to the study, suicide was less than half likely among those who received the contact intervention, and up to 25% recipients answered back with thankful expressions. Accordingly, substantial attention has been put towards these low-resource, nonintrusive brief contact interventions (BCI). In general, BCI use letters [95], postcards [96], telephone calls [97], and/or a combination of all of them [98] for contact maintenance. One particular brief intervention, the widely implemented safety planning intervention (SPI), includes prioritizing coping strategies, addressing access to suicidal means, and enhancing outreach to professionals if suicidal urges emerge [99]. SPI was recently combined with a telephone call strategy and showed almost 50% fewer suicidal behaviors than treatment as usual in a series of Veteran Affairs hospitals [100].
Population-Level Suicide Prevention: Suicidal Individuals Versus Suicidal Populations
Since Durkheim’s seminal book Le Suicide [101], it is accepted that suicide rates are determined, at least partially, by causal factors that act at an ecological level, “whose action is felt by society as a whole.” Using Rose’s words, “why some individuals have high blood pressure is a different question than why some populations have more burden of high blood pressure?” [102]. The use of group-level factors to model individual-level outcomes has been common in epidemiology, including psychiatric epidemiology, over the twentieth century. In an early example, Faris and Dunham documented that rates of psychosis were higher in urban areas of Chicago compared with rural areas [103], leading to a century of hypotheses about environmental determinants of schizophrenia risk [104].
Causal factors that are shared by a whole social group, such as urban dwelling, have been coined “integral variables” [105], and their effect cannot, by definition, be measured comparing individuals who are within the same group. Instead, they require between-group comparisons using ecologic designs that focus on groups of individuals as legitimate units of analysis [106, 107]. Several examples illustrate how suicide can be conceptualized from an ecological perspective: some countries, such as Latvia, have 5 times higher incidence rates than others, like Greece (https://data.oecd.org/healthstat/suicide-rates6), which prompts questions about the economic and cultural conditions that may be invariant across country but that can be examined to understand risk. In the USA, suicide rates in rural areas double those of urban areas [108]. Even within a city, like London, areas with higher ecological indices of social deprivation entail higher suicide rates [109].
However, suicide prevention efforts have characteristically tried to model suicide risk [110] and predict suicide relying solely on individual-level correlates. As mentioned, several current research initiatives seek to improve suicide prediction through machine learning algorithms based on datasets that include information from individuals’ medical records [58••], speech analysis [111], and real-world behaviors measured through cell phone geolocation [112].
In attempts to understand causation of suicide, researchers often choose a frame of reference that includes a finite set of potential causes [107] and depends mainly in their field of knowledge: for example, a psychiatrist and a sociologist will consider different potential causes. By discarding what is outside our frame of reference, we generate an asymmetry on the way we look at things that permits cause-effect directionality [112]. Hence, the frame of reference and the scope of interest of the researcher determine which potential causes are considered [107], and complex systems with dynamic interactions between ecological and individual factors and feedback loops are usually reduced to a simpler thought model. As a result, causal relations tend to be ascertained at a particular level of organization, usually the individual one in the field of suicidology, determined by the system delimited by our focus (factors within the system can be identified and related), and findings’ validity is often limited to such system.
However, “a system never exists in isolation” [107]. As a result, there is growing interest in the study of how macro-level characteristics affect outcomes independently of individual variables, as well as how both levels interact [113]. In psychiatry, the interaction of the molecular, the individual, and the social levels in shaping mental suffering, disease, and illness was famously acknowledged by the late Engels’s synthesis of the bio-psycho-social medical model [114]. Multilevel epidemiology has emerged as a response to this interest, as both a thinking framework and a set of tools that allow for the consideration of a hierarchy of multiple levels of causation for epidemiologic analyses. Tools and analyses to integrate and analyze a wide range of potential predictive factors through data science initiatives and machine learning are growing [115,116,117••], with potential to aid in prediction tools for suicide risk. These tools can be partnered with rich exploration of the social and political settings with which suicide risk also occurs in order to inform the broader environmental factors that predict risk.
There are three broad categories of interventions aimed at lowering the risk of suicide at the population level: universal and specific education campaigns, regulations in mass media coverage, and restriction of access to means.
Two evidence-based educational strategies stand out: the implementation of school-based suicide prevention and intervention programs [118, 119] and the identification and training of the so-called “emergent gatekeepers” [120], people who may have contact with those with suicidal thoughts without having been trained and designated as professionals (teachers, police, etc.).
The well-established influence of media reporting of suicide stories on subsequent suicide rates [121,122,123], usually referred to as the “Werther effect” and framed within the broader behavioral contagion theory [124], has provided an opportunity for intervention through a variety of reporting recommendation guidelines [125]. In general, these guidelines seek to foster responsible, non-sensationalist coverage of suicide and related events.
Theoretically, media also plays a role in means restriction, because it can reduce the population’s “cognitive-access” [126] to suicide by purposely avoiding the coverage of key news, like an emerging suicide method or the suicide of a celebrity [123, 127]. However, by restriction of the access to suicide means we usually refer to a series of evidence-based interventions to physically prevent the population from accessing potentially lethal means such as pesticides [128], medications [129], suicide hotspots [130••], or firearms. The means reduction approach builds on evidence suggesting that ease of access influences the risk of attempting suicide [131], especially in impulsive suicidal behaviors [132]—the most frequent type as nearly half suicide attempt survivors report a suicidal process, the interval between the onset of a suicidal thought and subsequent suicide attempting, of 10 min or less [133]. Accessibility also impacts method choice: up to 85% self-poisoning patients report that easy availability obtained their choice of poison [134].
Method substitution is the flip side of this coin. Reducing the access to lethal means tends to be even more effective if the alternative method available for substitution has a lower associated lethality, due to a lower inherent deadliness or to a higher ability to abort mid-attempt. For example, firearms, which can be found in roughly 33% of homes and account for 51% of total suicides in the USA, have twice the associated lethality of gas poisoning and 50 times that of drug overdose [131]. Accordingly, several studies using a variety of epidemiological designs have concluded higher risks of suicide for people who live in a household with firearms [135], after controlling for potential confounders [136], as well as higher suicide rates in states where gun ownership levels are higher [137].
Conclusion
In summary, suicide remains a substantial global contributor to causes of death, especially among those at younger age, and is increasing at an unprecedented rate in the USA. Non-fatal self-injury is also increasing, and together, the trends in self-injurious behavior raise questions about the causes, interventions, and preventive measures that should be taken. Prevention and treatment are often pointed towards high-risk groups, such as those with repeated suicide attempts, who are at increased risk of dying by suicide, but may miss the majority of suicide decedents who do not come into contact with the mental health care system and act impulsively. Conceptualizing suicide and its causes as a multilevel process that unfolds across the life course, with causes at higher geographic levels as well as individual levels, may be useful to develop programs that can have the most impact on population health, and innovative prevention and intervention programs that engage new technologies are in development but require additional evidence. Suicides are preventable and tragically destabilizing for individuals who recover from attempts, and for families of those affected. In the next generation of suicide research, it is critical to examine factors beyond the proximal and clinical to allow for a reimagining of prevention that is life course and socially focused.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
McKeown RE, Cuffe SP, Schulz RM. US suicide rates by age group, 1970-2002: an examination of recent trends. Am J Public Health. 2006;96:1744–51.
Stone DM, Simon TR, Fowler KA, Kegler SR, Yuan K, Holland KM, et al. Vital signs: trends in state suicide rates — United States, 1999–2016 and circumstances contributing to suicide — 27 states, 2015. MMWR. 2018;67(22):617–24.
Hedegaard H, Curtin SC, Warner M. Suicide mortality in the United States, 1999-2017. NCHS Data Brief 2018.
•• https://www.cdc.gov/nchs/data/databriefs/db309.pdf Provides updated data on suicide rates in the USA, and depicts increasing trends in the 2000–2016 period with comprehensive descriptive analyses.
Cheng D, Mendenhall TI, Brenner BE. Suicide rates strongly correlate with altitude. Acad Emerg Med. 2005;12(suppl. 1):141.
Sy K, Shaman J, Gould M, Keyes K. Spatiotemporal Clustering of suicide deaths from 1999 to 2016: a spatial epidemiological approach. Under Review.
Pompili M, Sher L, Serafini G, Forte A, Innamorati M, Dominici G, et al. Posttraumatic stress disorder and suicide risk among veterans: a literature review. J Nerv Ment Dis. 2013;201(9):802–12.
Armed Forces Health Surveillance Center (AFHSC). Deaths by suicide while on active duty, active and reserve components, US Armed Forces, 1998-2011. MSMR. 2012;19(6):7–10.
Naifeh JA, Herberman HB, Stein MB, Fullerton CS, Kessler RC, Ursano RJ. The Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS): progress toward understanding suicide among soldiers. Mol Psychiatry. 2019;24:34–48.
•• Olfson M, Blanco C, Wall M, Liu SM, Saha TD, Pickering RP, et al. National trends in suicide attempts among adults in the United States. JAMA Psychiatry. 2017;74(11):1095–103 Uses nationally representative surveys conducted in 2004–2005 and 2012–2013 to describe an increasing trend in suicide attempts among adults that disproportionally affected younger adults with less formal education and those with psychiatric disorders.
Olfson M, Wang S, Blanco C. National trends in hospital-treated self-harm events among middle-aged adults. Gen Hosp Psychiatry. 2015;37(6):613–9.
Mercado MC, Holland K, Leemis RW, Stone DM, Wang J. Trends in emergency department visits for nonfatal self-inflicted injuries among youth aged 10 to 24 years in the United States, 2001-2015. JAMA. 2017;318(19):1931–3.
Owens PL, Fingar KR, Heslin KC, Mutter R, Booth CL. Emergency department visits related to suicidal ideation, 2006–2013. 2017. Available at: https://www.Hcup-Us.Ahrq.Gov/Reports/Statbriefs/Sb220-Suicidal-Ideation-ED-Visits.Jsp.
Ting SA, Sullivan AF, Boudreaux ED, Miller I, Camargo CA. Trends in US emergency department visits for attempted suicide and self-inflicted injury, 1993-2008. Gen Hosp Psychiatry. 2012;34(5):557–65.
Plemmons G, Hall M, Doupnik S, Gay J, Brown C, Browning W, et al. Hospitalization for suicide ideation or attempt: 2008–2015. Pediatrics. 2018;141(6):e20172426.
Burstein B, Agostino H, Greenfield B. Suicidal attempts and ideation among children and adolescents in US emergency departments, 2007-2015. JAMA Pediatr. Published online April 08, 2019.
Cavanagh JT, Carson AJ, Sharpe M, Lawrie M. Psychological autopsy studies of suicide: a systematic review. Psychol Med. 2003;33:395–405.
Arsenault-Lapierre G, Kim C, Turecki G. Psychiatric diagnoses in 3275 suicides: a meta-analysis. BM Psychiatry. 2004;4:37.
Nordentoft M, Mortensen PB, Pedersen CB. Absolute risk of suicide after first hospital contact in mental disorder. Arch Gen Psychiatry. 2011;68:1058–64.
Mojtabai R, Olfson M, Han B. National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics. 2016;138(6):e20161878.
•• Twenge JM, Cooper AB, Joiner TE, Duffy ME, Bingayu SG. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005–2017. J Abnorm Psychol. 2019;128(3):185–99 Using data from the NSDUH, a nationally representative survey, they describe a 2005–2017 increase in the rate of depression among adolescents and young adults.
•• Keyes KM, Hamilton A, Gary D, O’Malley P, Schulenberg J. Age, period, and cohort effects in depressive symptoms among US adolescents from 1976 to 2018. Social Psychiatry and Psychiatric Epidemiology. 2019. In press. Using over 1 million yearly cross-sectional surveys covering the 1991–2018 period, they describe an increase of depressive symptoms among teenage girls.
Oswalt SB, Lederer AM, Chestnut-Steich K, Day C, Halbritter A, Ortiz D. Trends in college students’ mental health diagnoses and utilization of services, 2009-2015. J Am Coll Heal 2018, in press.
Ketchen-Lipson S, Lattie EG, Eisenberg A. Increased rates of mental health service utilization by US college students: 10-year population-level trends (2007-2017). Psychiatr Serv. 2019;70:1.
Olfson M, Marcus SC. National patterns in antidepressant medication treatment. Arch Gen Psychiatry. 2009;66(8):848–56.
Marcus SC, Olfson M. National trends in the treatment for depression from 1998 to 2007. Arch Gen Psychiatry. 2010;67(12):1265–73.
Olfson M, Marcus SC, Druss B, Ellinson L, Tanielian T, Pincus HA. National trends in the outpatient treatment of depression. JAMA. 2002;287(2):203–56.
Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry Allied Discip. 2015;56(3):345–65.
Costello EJ, Erkanli A, Angold A. Is there an epidemic of child or adolescent depression? J Child Psychol Psychiatry. 2006;47(12):1263–71.
Case A, Deaton A. Rising midlife morbidity and mortality, US whites. PNAS. 2015;112(49):15078–83.
Goldman N, Glei DA, Weinstein M. (2018). Declining mental health among disadvantaged Americans. PNAS. 2018;115(28):7290–5.
Weinberger A, Gbedemah M, Martinez A, Nash D, Galea S, Goodwin R. Trends in depression prevalence in the USA from 2005 to 2015: widening disparities in vulnerable groups. Psychol Med. 2018;48(8):1308–15.
Todd M, Teitler J. Darker days? Recent trends in depression disparities among US adults. Am J Ortrhopsychiatry 2018, in press.
Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G. Drug and opioid-involved overdose deaths—United States, 2013–2017. Morb Mortal Wkly Rep. 2019;67(5152):1419–27.
•• Bohnert ASB, Ilgen MA. Understanding links among opioid use, overdose, and suicide. N Engl J Med. 2019;380:71–9 Comprehensive review of the links between suicide and overdoses that covers issues of intent, risk factors, prevention strategies, and unresolved issues.
Ilgen MA, Bohnert AS, Ganoczy D, Bair MJ, McCarthy JF, Blow FC. Opioid dose and risk of suicide. Pain. 2016;157:1079–84.
• Case A, Deaton A. Mortality and morbidity in the 21st century. Brookings Papers on Economic Activity, 2017: 397–476. Available at https://www.brookings.edu/wp-content/uploads/2017/08/casetextsp17bpea.pdf Provides a plausible theoretical framework connecting cumulative disadvantage from one birth cohort to the next and progressively worsening labor opportunities and to mortality due to overdose, alcohol-related diseases, and suicide.
Ruhm CJ. Deaths of despair or drug problems? NBER Working Paper Series 2018: 24188.
Masters RK, Tilstra AM, Simon DH. Explaining recent mortality trends among younger and middle-aged White Americans. Int J Epidemiol. 2018;47(1):81–8.
Smith TW, Son J. Trends in gun ownership in the United States, 1972–2014. GSS Methodological Report No. 123. Chicago: NORC; 2014. Available at http://www.norc.org/PDFs/GSS%20Reports/GSS_Trends%20in%20Gun%20Ownership_US_1972-2014.pdf. Accessed 6 Jun 2019.
Pedersen MG, Mortensen PB, Norgaard-Pedersen B, Postolache TT. Toxoplasma gondii infection and self-directed violence in mothers. Arch Gen Psychiatry. 2012;69(11):1123–30.
Mann JJ, Oquendo M, Underwood MD, Arango V. The neurobiology of suicide risk: a review for the clinician. J Clin Psychol. 1999;60(suppl2):7–11.
Turecki G, Ernst C, Jollant F, Labonte B, Mechawar N. The neurodevelopmental origins of suicidal behavior. Trends Neurosci. 2012;1:14–23.
Brent DA, Perper JA, Moritz G, Allman C, Friend A, Roth C, et al. Psychiatric risk factors for adolescent suicide: a case-control study. J Am Acad Child Adolesc Psychiatry. 1993;32(3):521–9.
Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the adverse childhood experiences study. JAMA. 2001;286(24):3089–96. https://doi.org/10.1001/jama.286.24.3089.
Roy A. Risk factors for suicide in psychiatric patients. Arch Gen Psychiatry. 1982;39(9):1089–95.
Carter G, Milner A, McGill K, Pirkis J, Kapur N, Spittal MJ. Predicting suicidal behaviours using clinical instruments: systematic review and meta-analysis of positive predictive values for risk scales. Br J Psychiatry. 2017;210(6):387–95.
Chan MK, Bhatti H, Meader N, et al. Predicting suicide following self-harm: systematic review of risk factors and risk scales. Br J Psychiatry. 2016;209(4):277–83.
• Hawton K. Assessment of suicide risk. Br J Psychiatry. 1987;150:145–53 Seminal conference paper on the limitations of suicide risk assessments in the clinical setting.
Pokorny AD. Prediction of suicide in psychiatric patients. Report of a prospective study. Arch Gen Psychiatry. 1983;40(3):249–57.
Goldstein RB, Black DW, Nasrallah A, Winokur G. The prediction of suicide. Sensitivy, specificity and predictive value of a multivariate model applied to suicide among 1906 patients with affective disorders. Arch Gen Psychiatry. 1991;48(5):418–22.
Steeg S, Quinlivan L, Nowland R, et al. Accuracy of risk scales for predicting repeat self-harm and suicide: a multicentre, population-level cohort study using routine clinical data. BMC Psychiatry. 2018;18(1):113.
Nielssen O, Wallace D, Large M. Pokorny’s complaint: the insoluble problem of the overwhelming number of false positives generated by suicide risk assessment. BJPsych Bull. 2017;41(1):18–20.
Undrill G. The risks of risk assessment. Adv Psychiatr Treat. 2007;13:291–7.
Mulder R, Newton-Howes G, Coid JW. The futility of risk prediction in psychiatry. BJ Psych. 2016;209:271–2.
Kessler RC, Stein MB, Petukhova MV, et al. Predicting suicides after outpatient mental health visits in the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Mol Psychiatry. 2017;22(4):544–51.
DelPozo-Banos M, John A, Petkov N, Berridge DM, Southern K, LLoyd K, et al. Using neural networks with routine health records to identify suicide risk: feasibility study. JMIR Ment Health. 2018;5(2):e10144.
Simon GE, Johnson E, Lawrence JM, Rossom RC, Ahmedani B, Lynch FL, et al. Predicting suicide attempts and suicide deaths following outpatient visits using electronic health records. Am J Psychiatry. 2018;175(10):951–60.
Belsher BE, Smolenski DJ, Pruitt LD, et al. Prediction models for suicide attempts and deaths: a systematic review and simulation. JAMA Psychiatry. 2019;76(6):642–51 in press.
Belsher BE, Smolenski DJ, Pruitt LD. In reply. JAMA Psychiatry. 2019: in press.
Simon GE. Big data from health records in mental health care. Hardly clairvoyant but already useful. JAMA Psych. 2019;74(4):349–50.
Hawton K, Zahl D, Weatherall R. Suicide following deliberate self-harm: long-term follow-up of patients who presented to a general hospital. Br J Psychiatry. 2003;182(6):537–42.
Glenn CR, Nock MK. Improving the prediction of suicidal behavior in youth. Int J Behav Consult Ther. 2014;9(3):7–10.
Madsen T, Nordentoft M. Suicidal changes in patients with first episode psychosis: clinical predictors of increasing suicidal tendency in the early treatment phase. Early Intervention in Psychiatry. 2012;6:292–9.
Ayesa-Arriola R, Alcaraz EG, Hernández BV, Pérez-Iglesias R, López Moríñigo JD, Duta R, et al. Suicidal behaviour in first-episode non-affective psychosis: specific risk periods and stage-related factors. Eur Neuropsychopharmacol. 2015;25:2278–88.
Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56(7):617–26.
Oquendo MA, Halberstam B, Mann JJ. Risk factors for suicidal behavior: utility and limitations of research instruments. In: First MB, editor. Standardized evaluation in clinical practice. 1. American Psychiatric Publishing; Washington DC: 2003. pp. 103–130.
•• Kleiman EM, Turner BJ, Fedor S, Beale EE, Huffman JC, Nock MK. Examination of real-time fluctuations in suicidal ideation and its risk factors: results from two ecological momentary assessment studies. J Abnorm Psychol. 2017;126(6):726–38 Provides solid evidence on the remarkable variation in suicidal thoughts experienced over short periods of time, based on ecologic momentary assessments.
Baca-Garcia E, Perez-Rodriguez MM, Keyes KM, Oquendo MA, Hasin DS, Grant BF, et al. Suicidal ideation and suicide attempts in the United States: 1991-1992 and 2001-2002. Mol Psychiatry. 2010;15(3):250–9.
Lee S, Fung SC, Tsang A, Liu ZR, Huang YQ, He YL, et al. Lifetime prevalence of suicide ideation, plan, and attempt in metropolitan China. Acta Psychiatr Scand. 2007;116:429–37.
Husky M, Olie E, Guillaume S, Genty C, Swendsen J, Courtet P. Feasibility and validity of ecological momentary assessment in the investigation of suicide risk. Psychiatry Res. 2014;220(1–2):564–70.
Rodriguez-Blanco L, Carballo JJ, Baca-Garcia E. Use of ecological momentary assessment (EMA) in non-suicidal self-injury (NSSI): a systematic review. Psychiatry Res. 2018;263:212–9.
•• Davidson CL, Anestis MD, Gutierrez PM. Ecological momentary assessment is a neglected methodology in suicidology. Arch Suicide Res. 2017;1:1–11 Brief critical review of the potential uses of EMA for suicide research.
Chaudhury SR, Galfalvy H, Biggs E, Choo TH, Mann JJ, Stanley B. Affect in response to stressors and coping strategies: an ecological momentary assessment study of borderline personality disorder. Borderline Personal Disord Emot Dysregul. 2017;4:8.
Hallensleben N, Spangenberg L, Forkmann T, Rath D, Hegerl U, Kersting A, et al. Investigating the dynamics of suicidal ideation: preliminary findings from a study using ecological momentary assessments in psychiatric inpatients. Crisis. 2018;39(1):65–9.
Kleiman EM, Nock MK. Real-time assessment of suicidal thoughts and behaviors. Curr Opin Psychol. 2018;22:33–7.
Husky M, Swendsen J, Ionita A, Jaussent I, Genty C, Courtet P. Predictors of daily life suicidal ideation in adults recently discharged after a serious suicide attempt: a pilot study. Psychiatry Res. 2017;256:79–84.
Mann JJ, Apter A, Bertolote J, et al. Suicide prevention strategies: a systematic review. JAMA. 2005;294(16):2064–74. https://doi.org/10.1001/jama.294.16.2064.
van der Feltz-Cornelis CM, Sarchiapone M, Postuvan V, Volker D, Roskar S, Grum AT, et al. Best practice elements of multilevel suicide prevention strategies: a review of systematic reviews. Crisis. 2011;32(6):319–33. https://doi.org/10.1027/0227-5910/a000109.
Zalsman G, Hawton K, Wasserman D, van Heeringen K, Arensman E, Sarchiapone M, et al. Suicide prevention strategies revisited: 10-year systematic review. Lancet Psychiatry. 2016;3:646–59.
Munro J, O’Sullivan D, Andrews C, Arana A, Mortimer A, Kerwin R. Active monitoring of 12,760 clozapine recipients in the UK and Ireland: beyond pharmacovigilance. Br J Psychiatry. 1999;175:576–80.
Walker AM, Lanza LL, Arellano F, Rothman KJ. Mortality in current and former users of clozapine. Epidemiology. 1997;8:671–7.
Meltzer HY, Alphs L, Green AI, Altamura AC, Anand R, Bertoldi A, et al. Clozapine treatment for suicidality in schizophrenia: International Suicide Prevention Trial (InterSePT). Arch Gen Psychiatry. 2003;60(1):82–91.
Baldessarini RJ, Tondo L, David P, et al. Decreased risk of suicides and attempts during long-term lithium treatment: a meta-analytic review. Bipolar Disord. 2006;8(5):2.
Tondo L, Baldessarini RJ. Antisuicidal effects in mood disorders: are they unique to lithium? Pharmacopsychiatry. 2018;51:177–88. https://doi.org/10.1055/a-0596-7853.
Goodwin FK, Fireman B, Simon GE, Hunkeler EM, Lee J, Revicki D. Suicide risk in bipolar disorder during treatment with lithium and divalproex. JAMA. 2003;290(11):1467–73.
Brown GK, Ten Have T, Henriques GR, Xie SX, Hollander JE, Beck AT. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. JAMA. 2005;294(5):563–70.
Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, et al. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Arch Gen Psychiatry. 2006;63(7):757–66.
Heisel MJ, Talbot NL, King DA, Tu XM, Duberstein PR. Adapting interpersonal psychotherapy for older adults at risk for suicide. Am J Geriatr Psychiatry. 2015 Jan;23(1):87–98.
Martínez-Alés G, Angora R, Barrigón ML, et al. A real-world effectiveness study comparing a priority appointment, an enhanced contact intervention, and a psychotherapeutic program following attempted suicide. J Clin Psychiatry. 2019;80(2):18m12416.
Riblet NBV, Shiner B, Young-Xu Y, Watts BV. Strategies to prevent death by suicide: meta-analysis of randomized controlled trials. Br J Psychiatry. 2017;210(6):396–402.
Olfson M, Wall M, Wang S, Crystal S, Gerhard T, Blanco C. Suicide following deliberate self-harm. Am J Psychiatry. 2017;174:765–74.
Brenner LA, Barnes SM. Facilitating treatment engagement during high-risk transition periods: a potential suicide prevention strategy. Am J Public Health. 2012;102:S12–4.
Motto JA, Bostrom AG. A randomized controlled trial of postcrisis suicide prevention. Psychiatr Serv. 2001;52(6):828–33.
Hassanian-Moghaddam H, Sarjami S, Kolahi AA, Carter GL. Postcards in Persia: randomised controlled trial to reduce suicidal behaviours 12 months after hospital-treated self-poisoning. Br J Psychiatry. 2011;198(4):309–16.
Cebrià AI, Parra I, Pàmias M, Escayola A, García-Parés G, Puntí J, et al. Effectiveness of a telephone management programme for patients discharged from an emergency department after a suicide attempt: controlled study in a Spanish population. J Affect Disord. 2013;147(1–3):269–76.
Kapur N, Gunnell D, Hawton K, Nadeem S, Khalil S, Longson D, et al. Messages from Manchester: pilot randomised controlled trial following self-harm. Br J Psychiatry. 2013;203(1):73–4.
Vaiva G, Berrouiguet S, Walter M, et al. Combining postcards, crisis cards, and telephone contact into a decision-making algorithm to reduce suicide reattempt: a randomized clinical trial of a personalized brief contact intervention. J Clin Psychiatry. 2018;79(6):17m11631.
Stanley B, Brown GK. Safety planning intervention: a brief intervention to mitigate suicide risk. Cogn Behav Pract. 2012;19(2):256–64.
Stanley B, Brown GK, Brenner LA, et al. Comparison of the safety planning intervention with follow-up vs usual care of suicidal patients treated in the emergency department. JAMA Psychiatry. 2018;75(9):894–900.
Durkheim E. Suicide. Collier-Macmillan Canada Ltd, 1966, Toronto, Ontario.
Rose G. Sick individuals and sick populations. Int J Epidemiol. 2001;30(3):427–32 discussion 433-4.
Faris R, Dunham H. Mental disorders in urban areas: an ecological study of schizophrenia and other psychoses. New York: Hafner Publishing; 1939.
Plana-Ripoll O, Pedersen CB, McGrath JJ. Urbanicity and risk of schizophrenia—new studies and old hypotheses. JAMA Psychiatry. 2018;75(7):687–8.
Susser MW. The logic in ecological II. The logic of design. Am J Public Health. 1994;84:830–5.
Susser MW. The logic in ecological I. the logic of analysis. Am J Public Health. 1994;84:825–9.
Susser M. Causal thinking in the health sciences. New York: Oxford University Press; 1972.
Fontanella CA, Hiance-Steelesmith DL, Phillips GS, Bridge JA, Lester N, Sweeney HA, et al. Widening rural-urban disparities in youth suicides, United States, 1996–2010. JAMA Pediatr. 2015;169:466–73 7.
Rezaeian M, Dunn G, St Leger S, Appleby L. The ecological association between suicide rates and indices of deprivation in English local authorities. Soc Psychiat Epidemiol. 2005;40:785.8.
Ursano RJ, Colpe LJ, Heeringa SG, Kessler RC, Schoenbaum M, Stein MB, et al. The Army Study to Assess Risk and Resilience in Service members (Army STARRS). Psychiatry: Interpersonal and Biological Processes. 2014;77(2):107–19.
Vahabzadeh A, Sahin N, Kalali A. Digital suicide prevention: can technology become a game-changer? Innov Clin Neurosci. 2016;13(5–6):16–20.
Pearl J. The art and science of cause and effect. J. Pearl, Causality: models, reasoning, and inference. New York: Cambridge University Press; 2009. p. 401–28.
Diez-Roux AV. Bringing context back into epidemiology: varia-bles and fallacies in multilevel analysis. Am J Public Health. 1998;88:216–22.10.
Engel G. The need for a new medical model: a challenge for biomedicine. Science. 1977;196:129–36.
Torous J, Larsen ME, Depp C, Cosco TD, Barnett I, Nock MK, et al. Smartphones, sensors, and machine learning to advance real-time prediction and interventions for suicide prevention: a review of current progress and next steps. Curr Psychiatry Rep. 2018;20:51. https://doi.org/10.1007/s11920-018-0914-y.
Kessler RC, Van Loo HM, Wardenaar KJ, Bossarte RM, Brenner LA, Cai T, et al. Testing a machine-learning algorithm to predict the persistence and severity of major depressive disorder from baseline self-reports. Mol Psychiatry. 2016;21:1366–71.
•• Kessler RC, Bernecker SL, Bossarte RM, Luedtke AR, McCarthy JF, Nock MK, et al. The role of big data analytics in predicting suicide. In: Passos I., Mwangi B., Kapczinski F. (eds) Personalized psychiatry. Springer, Cham Critical comprehensive review on big data for suicide prediction.
Zenere FJ, Lazarus PJ. The decline of youth suicidal behavior in an urban, multicultural public school system following the introduction of a suicide prevention and intervention program. Suic Life Threat Behavior. 1997;27:387–402.
Wasserman D, Hoven CW, Wasserman C, Wall M, Eisenberg R, Hadlaczky G, et al. School-based suicide prevention programmes: the SEYLE cluster-randomised, controlled trial. Lancet. 2015;385:1536–44.
Isaac M, Elias B, Katz LY, Belik SL, Deane FP, Enns MW, et al. Gatekeeper training as a preventative intervention for suicide: a systematic review. Can J Psychiatr. 2009;54:260–26.
Sisask M, Varnik A. Media roles in suicide prevention: a systematic review. Int J Environ Res Public Health. 2012;9:123–38.
Pirkis JE, Burgess PM, Francis C, Blood RW, Jolley DJ. The relationship between media reporting of suicide and actual suicide in Australia. Soc Sci Med. 2006;62(11):2874–86.
Fink DS, Santaella-Tenorio J, Keyes KM. Increase in suicides the months after the death of Robin Williams in the US. PLoS One. 2018;13(2):e0191405.
Gould M. Suicide and the media. Ann N Y Acad Sci. 932:200–21.
American Asssociation of Suicidology. Suicide reporting recommendations: media as partners toolkit. Retrieved from: https://suicidology.org/reporting-recommendations/. Accessed 9 Sept 2019.
Florentine JB, Crane C. Suicide prevention by limiting access to methods: a review of theory and practice. Soc Sci Med. 2010;70:1626–32.
Williams K. Media influences on suicidal behaviour. In: Hawton K, editor. Prevention and treatment of suicidal behaviour: from science to practice. Oxford: Oxford University Press; 2005. p. 293–306.
Gunnell D, Eddleston M. Suicide by intentional ingestion of pesticides: a continuing tragedy in developing countries [published correction appears in Int J Epidemiol. 2004 Aug;33(4):920]. Int J Epidemiol. 2003;32(6):902–9.
Hawton K, Bergen H, Simkin S, Dodd S, Pocock P, Bernal W, et al. Long term effect of reduced pack sizes of paracetamol on poisoning deaths and liver transplant activity in England and Wales: interrupted time series analyses. BMJ. 2013;346:f403.
•• Pirkis J, Too LS, Spittal MJ, Krysinska K, Robinson J, Cheung YT. Interventions to reduce suicides at suicide hotspots: a systematic review and meta-analysis. Lancet Psychiatry. 2015;2:994–1001 Comprehensive review with current evidence on means restriction strategies.
Marzuk PM, Leon AC, Tardiff K, Morgan EB, Stajic M, Mann JJ. The effect of access to lethal methods of injury on suicide rates. Arch Gen Psychiatry. 1992;49:451–8.
Hawton K. Studying survivors of nearly lethal suicide attempts: an important strategy in suicide research. Suicide Life Threat Behav. 2001;32:76–84.
Deisenhammer EA, Ing CM, Strauss R, Kemmler G, Hinterhuber H, Weiss EM. The duration of the suicidal process: how much time is left for intervention between consideration and accomplishment of a suicide attempt? J Clin Psychiatry. 2009;70(1):19–24.
Eddleston M, Karunaratne A, Weerakoon M, Kumarasinghe S, Rajapakshe M, Sheriff MH, et al. Choice of poison for intentional self-poisoning in rural Sri Lanka. Clin Toxicol (Phila). 2006;44(3):283–6.
Brent DA, Perper JA, Moritz G, Baugher M, Schweers J, Roth C. Firearms and adolescent suicide. A community case-control study. Am J Dis Children. 1993;147(10):1066–71.
Kellermann AL, Rivara FP, Somes G, Reay DT, Francisco J, Banton JG, et al. Suicide in the home in relation to gun ownership. N Engl J Med. 1992;327(7):467–72.
Miller M, Lippmann SJ, Azrael D, Hemenway D. Household firearm ownership and rates of suicide across the 50 United States. J Trauma. 2007;62(4):1029–34.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Gonzalo Martínez-Alés reports a grant from La Caixa Foundation LCF/BQ/AA17/11610021. The other author declares that there are no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Mood Disorders
Rights and permissions
About this article
Cite this article
Martínez-Alés, G., Keyes, K.M. Fatal and Non-fatal Self-Injury in the USA: Critical Review of Current Trends and Innovations in Prevention. Curr Psychiatry Rep 21, 104 (2019). https://doi.org/10.1007/s11920-019-1080-6
Published:
DOI: https://doi.org/10.1007/s11920-019-1080-6