Abstract
Purpose of Review
This study aims to provide a review of the randomized controlled studies evaluating the effects of shared decision-making (SDM) intervention in comparison to care as usual in patients with mood disorders.
Recent Findings
Of the 14 randomized controlled studies identified, only three 6-month studies evaluated the interest of SDM interventions using decision aids in depressed patients. All of them showed that the intervention effectively improved patient satisfaction and engagement in the decision-making process. Only one study in patients with bipolar disorder (BD) showed improvement of depressive symptoms, functioning, and quality of life. Other included studies were collaborative care interventions using a SDM approach in patients with depression in specific populations depending on age, gender, income, and physical comorbidities. All of them showed significant improvement in depression outcomes or medication adherence.
Summary
SDM interventions using decision aids and collaborative care showed evidence of improvements in the management of depression. Stronger evidence of SDM interest in BD is needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mood disorders are severe and chronic diseases with an estimated prevalence of 9.5% during the last 12 months and are associated with disability [1], functional impairment, and negative impact on quality of life [2, 3].
Medication treatment represents the first-line therapy for the acute phase and the long-term prophylactic management of mood disorders [4, 5]. In spite of significant evidence on effective medications for the treatment of mood disorders, patient outcomes continue to be impacted by treatment adherence. In both bipolar disorder (BD) and major depressive disorder (MDD), treatment efficacy can be reduced by partial or complete non-adherence to treatment and premature discontinuation [6, 7], contributing to increase the risk of relapse and the use of healthcare services [8, 9].
Adherence to medication appears to be of prime importance and an integral part of the decision-making process. Effective physician-patient communication produces more favorable health outcomes, and treatment success can be increased when patients take an active role in their health care [10]. Thereby, during the last decade health care policies advocated a greater involvement of patients in clinical decisions, especially since the development of the concept of shared decision-making (SDM).
SDM can be defined as “an approach where clinicians and patients share the best available evidence when faced with the task of making decisions, and where patients are supported to consider options, to achieve informed preferences” [11]. This concept can be considered as a “meeting of experts”: the physician as a medical expert and the patient as expert in his or her own life, values, and circumstances [12]. SDM is a promising way for patient-centered medicine.
In 2010, a Cochrane systematic review showed positive significant associations between SDM intervention and improved knowledge, patient participation, and satisfaction with care in patients with mental health conditions [13]. Since its publication, new studies evaluating the effects of SDM intervention in patients with mood disorders have been performed and published [14, 15••].
To provide the existing body of evidence in mood disorders, the main aim of this article was to review the available randomized controlled published studies evaluating the effects of SDM intervention in comparison to care as usual in patients with dysthymia, MDD, and BD.
Methods
Search Process
We conducted a comprehensive systematic search of the literature using multiple scientific literature databases (MEDLINE, EMBASE, SCOPUS, and Google Scholar) employing the Boolean logic algorithm (“bipolar” OR “mood disorder*” OR “affective disorder” OR “depress*” OR “psychiatric*” OR “severe mental”) AND (“collaborative*” OR “shared decision-making” OR “decision aid*”). We restricted our search parameters to the abstracts or articles published in English between January 2000 and October 2017. Search results were last updated on November 1, 2017. Inclusion criteria contained articles with SDM intervention or collaborative care, which contained at least one module using a SDM process. Additionally, our search was only focused on randomized controlled trials or clustered randomized controlled trials comparing interventions and care as usual groups. The sample population studied had mood disorders: dysthymia, MDD, or BD type I and type II. The selection process followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) criteria.
Procedure and Data Extraction
Articles were independently title-screened by two authors (JG, LS) for duplicates or irrelevant papers. In case of ambiguity, abstracts were consulted. Secondarily, all abstracts and full texts were independently screened by the same two authors and were considered for inclusion only if they provided sufficient information. After conciliation, papers meeting underlying conditions were carefully reviewed and relevant data extracted for the review. Actually, there is no consensual definition of SDM but some concepts, such as patient values/preferences, therapeutic options, patient engagement and participation, and patient education, seem to be essential to determine a SDM intervention [16]. Consequently, selected articles had to contain interventions, which integrated actively the patient in the medical process through these concepts. For instance, several studies with collaborative care programs have been included in this review, because they contained at least one module that met the definition of SDM intervention.
Results
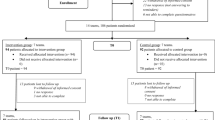
More than 600 potential entries matching the search criteria were identified, and 152 articles were available after the removal of duplicates and papers excluded by titles. Ninety-six more were excluded after reading the abstract, and we assessed the full text in 56 studies. Subsequently and after careful manual review, we excluded 39 of the retrieved articles: 34 did not meet SDM criteria, 6 did not meet population inclusion criteria, and 2 for other reasons. A total of 14 original studies met our inclusion criteria (Fig. 1). Therefore, we divided the studies into two categories: (1) Interventions in patients with mood disorder and (2) Interventions in patients with depressive disorder in specific populations.
SDM Interventions in Patients With Mood Disorder
Four randomized controlled trials evaluated the effects of SDM intervention in patients with mood disorders (Table 1).
Among them, only three assessed specifically the impact of SDM in a population of patients with dysthymia and/or MDD. First, Loh et al. (2007) conducted a multi-faceted program based on SDM. It included physician training, a decision board for use during the consultation and printed patient information that combined evidence-based knowledge about depression care and specific encouragement for patients to be active in the decision-making process [10]. This cluster randomized controlled intervention study enrolled 405 patients with newly diagnosed depression and found significant improvement of physician facilitation of patient participation (p = .005) in the intervention group compared to the control group. Patient satisfaction at post-intervention was also higher in the intervention group (p = .014), but no intervention effect for depression severity reduction was found. The consultation duration did not differ between groups.
Secondly, Aljumah et al. (2015) evaluated the effectiveness of SDM-based pharmacist intervention for improving adherence and outcomes in MDD patients [18]. This 6-month randomized controlled trial included 239 patients (intervention group, n = 119; control group, n = 120). The intervention enhanced patients’ involvement in decision-making by assessing their beliefs and knowledge about antidepressants and using a decision aid specifically designed for depressed patients. After 6 months, patients in the intervention group had significantly more favorable medication adherence (p < .001), treatment satisfaction (p < .001), general overuse (p = .029), and specific concern beliefs (p = .024). The authors did not find significant differences in severity of depression or health-related quality of life between groups.
Thirdly, LeBlanc et al. (2015) conducted a cluster randomized controlled trial in which they allocated primary care practices to treat depression with or without a depression decision aid (Depression Medication Choice) [17••]. This decision aid used a series of laminated cards that presented general considerations about antidepressant efficacy and side effects in terms that matter to patients (i.e., weight change, sleep, sexual issues, stopping approach, and cost). Clinicians in the intervention group were to use the decision aid during their consultations. A total of 297 patients were enrolled and compared to care as usual. Use of a specific decision aid significantly improved patients’ decisional comfort (p = .02), knowledge (p = .03), satisfaction (RR = 1.25, p = .81 to RR = 2.4, p = .002), and involvement (p < .001) in the decision-making process. It also improved clinicians’ decisional comfort (p < .0001) and satisfaction (RR = 1.64, p = .02). On the other hand, there were no differences in encounter duration, medication adherence, or improvement of depression control between groups.
van der Voort et al. (2015) performed a collaborative care multi-component intervention including a SDM approach for BD patients [19, 20••]. Patients in severe depressive or manic episode at the time of inclusion and patients with a stable course of illness over the past year were excluded. All decisions concerning treatment were made by a collaborative care team including the patient, considering his preferences and involving him in decision-making process. The collaborative care group (n = 56) showed more improvement in overall functioning compared to the care as usual group (n = 82), with a small effect size (ES = .3, p = .01). In certain domains of functioning (autonomy and leisure time), a medium effect was found in favor of collaborative care (autonomy: ES = .5, p = .004; leisure time: ES = .4, p = .02). Concerning quality of life, patients in the intervention group were only improved more in the physical health domain (ES = .4, p = .01) compared to the care as usual group [19]. Collaborative care had a significant and clinically relevant effect on number of months with depressive symptoms, both at 6 months (p = .01) and at 12 months (p = .002), as well as on the severity of depressive symptoms at 12 months (p = .004) [20••].
SDM Interventions in Patients With Depressive Disorder in Specific Populations
The 10 remaining studies evaluated SDM interventions in patients with dysthymia or MDD in specific populations depending on age, gender, income, and physical comorbidities. No results were found for BD patients (Table 2).
SDM Interventions in Adolescent and Elderly Populations
Unützer et al. (2002) performed a 12-month randomized controlled trial to determine the effectiveness of the Improving Mood-Promoting Access to Collaborative Treatment (IMPACT) collaborative care program versus care as usual in 1801 patients with late-life depression [23]. The IMPACT intervention [33] consisted of a care management where a depression clinical specialist supports the patient’s regular primary care provider to treat depression. Each participant received an initial education and an engagement session (20-min educational videotape and a booklet about late-life depression). The SDM approach facilitated patient decision-making between antidepressant medications. The authors reported improvement in depressive symptoms (50% or greater reduction from baseline) at 12 months in the intervention group (p < .001) and also greater rates of antidepressant use (p < .001), more satisfaction with depression care (p < .001), lower depression severity (p < .001), less functional impairment (p < .001), and greater quality of life (p < .001).
Similarly, Richardson et al. (2014) investigated the IMPACT intervention in adolescents with MDD [22]. They conducted a 12-month randomized controlled trial enrolling 101 adolescents aged 13 to 17 years who met criteria for MDD. The adapted collaborative care intervention was based on the IMPACT model and included SDM concepts, such as an initial education and engagement session, and an active discussion for the choice of treatment depending on patient and parents preferences or values. Intervention youth (n = 50), compared with those randomized to care as usual (n = 51), showed greater improvement in depressive symptoms according to the Children Depression Rating Scale at 12 months (p < .001). This intervention also appeared to be cost-effective [21].
SDM Interventions in Women Population During Pregnancy or Gynecological Care
Grote et al. designed an 18-month multi-site randomized controlled trial in pregnant women who met criteria for dysthymia and/or MDD to evaluate the efficacy of MOMCare, a collaborative care intervention for perinatal depression, in comparison to care as usual (intensive maternity support services) [24]. MOMCare included patient education, a pre-treatment engagement session to help resolve practical, psychological, and cultural barriers to care and the choice of treatment between brief interpersonal psychotherapy and/or antidepressant. Depression specialist encouraged women requesting antidepressants as an initial treatment to engage in a risk-benefit decision-making process with their obstetrician. From before birth to 18 months post baseline, MOMCare (n = 83) compared to care as usual participants (n = 85) showed significantly higher rates of depression remission (p = .05), lower levels of depression severity (p = .01), and greater adherence to antidepressants (p < .01).
In 2014, Melville et al. evaluated another evidence-based collaborative depression care intervention adapted to women follow-up in obstetrics and gynecology clinics compared to care as usual [26]. This multi-site randomized controlled trial enrolled women (pregnant or not) who met criteria for MDD, dysthymia, or both. The three-part intervention included the following: enhanced education, engagement of patients and patient choice of initial antidepressant medication or problem solving treatment, and behavioral activation. Intervention (n = 102) compared to care as usual (n = 103) patients had greater improvement in depressive symptoms at 12 months (p < .001) and 18 months (p = .004) and improved functioning over 18 months (p < .05).
SDM Interventions in Low-Income Population
In 2008, Ell et al. conducted a randomized controlled trial using collaborative care management of depression (MDD and/or dysthymia) among 472 low-income patients with cancer. This collaborative care program, as well as study recruitment and intervention protocols, was specifically adapted for low-income patients [27]. The Alleviating Depression Among Patients With Cancer (ADAPt-C) intervention adapted the IMPACT stepped care model, including the following SDM components: initial patient engagement and patient education about depression, antidepressant treatment and psychotherapy, and consideration of initial patient treatment choice. At 12 months, 63% of patients in the intervention group had a 50% or greater reduction in depressive symptoms from baseline compared with 50% of patients in the care as usual group (p = .01). Patients in the intervention group also experienced greater rates of depression treatment (72.3 vs. 10.4%, p < .0001) and significantly better quality of life outcomes, including social/family (p < .001), emotional (p = .01), functional (p = .04), and physical well-being (p = .02).
A couple of years later, Ell et al. also investigated a sociocultural adapted collaborative care among 387 low-income, predominantly Hispanic diabetes patients with MDD [28]. The intervention took into account patient initial choice of treatment for depression according to different options. At 24 months, patients in the intervention group were significantly more likely to be receiving antidepressant medication (38 vs. 25%, p = .02) and experienced significantly more sustained depression symptom improvement (adjusted OR = 2.06, p = .03).
Dwight-Johnson et al. (2010) investigated equally a low-income population predominantly Latino with MDD and examined whether a collaborative care intervention that included SDM approaches, as patient education and patient treatment preferences, would increase the likelihood that patients received preferred treatment [29]. The results showed that patients preferred counseling or counseling plus medication over antidepressant medication alone and they were 21 times (OR = 20.7, p < .001) as likely to receive preferred care.
SDM Interventions in Populations With Physical Comorbidities
Two studies presented in the previous section (i.e., low-income population) included depressed patients with physical comorbidities (i.e., cancer and diabetes) and showed that the interventions were significantly associated with greater improvement in depression outcomes.
However, other studies assessing the impact of interventions including a SDM approach in depressed patients with physical comorbidities, especially cardiovascular diseases, have been identified. These studies make it possible to determine if the effect of the intervention is similar without the low-income variable.
One of them, a single-blind randomized controlled trial in 14 primary care clinics, involved 214 participants with poorly controlled diabetes, coronary heart disease, or both and coexisting depression [30]. Patients were randomized to the collaborative care group or the care as usual group. Patients in the intervention group received self-care materials, including a depression “Helpbook,” a video compact disk on depression care, a booklet, and other materials on chronic disease management. Patients worked collaboratively with nurses and primary care physicians to establish individualized clinical and self-care goals and best treatment options. As compared with controls, patients in the intervention group significantly improved control of medical disease and had greater 12-month improvement in depressive symptoms (p < .001). They reported better quality of life (p < .001) and greater satisfaction with care for diabetes, coronary heart disease, or both (p < .001) and with care for depression (p < .001).
In 2011, Huffman et al. conducted another randomized controlled trial comparing collaborative care and care as usual in depressed cardiac patients who were admitted to cardiac units [31]. In this collaborative care program, the SDM approach included respect of patient treatment preferences and a part of patient education. Patients in the intervention group were significantly more likely to be receiving antidepressant medication at discharge (71.9% collaborative care vs. 9.5% usual care, p < .001).
Stewart et al. (2014) compared the IMPACT collaborative care program and care as usual, in 235 patients aged greater than 60 years with MDD or dysthymia and with or without baseline cardiovascular disease (CVD) during an 8-year follow-up study [32]. The results showed that among patients without baseline CVD, the intervention group had a greater reduction in depressive symptoms than the care as usual group (p < .001) and were more likely to have taken antidepressants during the trial. Inversely, there was no difference in depression score between groups of patients with baseline CVD. IMPACT patients without baseline CVD had a 48% lower risk of a CVD event than patients in the care as usual group (28 vs. 47%, HR = .52, 95% CI .31–.86). Collaborative care in MDD patients before CVD onset reduced by half the occurrence risk of new CVD events during follow-up.
Discussion
This systematic review found 14 randomized controlled studies evaluating the effects of SDM intervention in patients with mood disorders. Table 3 presents a summary of the main results from these included studies.
Only three 6-month studies evaluated the interest of specific SDM intervention using decision aids in patients with MDD and/or dysthymia [10, 17,18]. All of them showed that the intervention effectively improved patient satisfaction, knowledge, and engagement in the decision-making process. There were no differences in the duration of medical consultations and also no differences in terms of improvement of depressive symptoms between groups. However, none of these studies were designed to assess the efficacy of SDM intervention on depressive symptoms as a primary outcome. Inconsistent results in medication adherence were found. These results were consistent with a systematic review of 115 randomized controlled studies in patients facing treatment in which decision aids compared to care as usual improved patients’ knowledge and engagement with treatment [34•]. They also expressed comfort with the decision-making process. Interestingly, implementation of SDM by pharmacist appeared feasible and was associated with positive outcomes [18], highlighting their potential role in providing regular care to patients with mood disorders.
Only one study in BD patients was found and showed improvement of depressive symptoms, functioning, and quality of life [19, 20••]. For now, the level of evidence is too weak to conclude that SDM is beneficial in BD. As BD treatment addresses two distinct and sometimes co-occurring symptoms (depression and (hypo)mania) one may wonder if BD patients are not expected to differ from other mental health users, especially in mood disorders, in terms of preferences and engagement in treatment decision-making.
Other included studies investigated collaborative care intervention in patients with dysthymia/MDD in specific populations depending on age, gender, income, and physical comorbidities. Collaborative care could be considered as an extended model of SDM, in which other physical and mental health professionals and patients’ families will be involved too. This model aims to improve the physical and mental health of people with mental illness in primary care [35]. If the key features of this model have been described [36], the available collaborative care studies varied significantly in the exact nature of their intervention. As a consequence, numerous collaborative care studies have been excluded from this review, because they did not contain SDM principles such as patient values/preferences, therapeutic options, patient engagement or participation, and patient education. However, all the collaborative care studies included in our review, whatever the specific populations (i.e., adolescents, elderly patients, pregnant women, patients with low-income, and patients with physical comorbidities), showed that the interventions were significantly associated with greater improvement in depression outcomes or medication adherence. These results are consistent with a recent Cochrane systematic review including 79 randomized controlled studies assessing the effectiveness of collaborative care for patients with depression and anxiety, which found significantly greater improvement of depression in the short term, medium term, and long term [37].
As previously highlighted by authors, collaborative care seems to be particularly useful in the management of patients with comorbidity and multi-morbidity, especially depression and long-term conditions [35]. This model of care could also facilitate accessibility to health care for patients with low income.
In comparison with studies evaluating specific SDM interventions using decision aids in MDD patients, collaborative care interventions including a SDM approach showed stronger evidence of their interest and effectiveness in the management of depression.
Limitations
SDM is positioned midway between informed choice and paternalistic model explaining in part the important overlap between definitions surrounding the concept of SDM, which vary substantially from one author to another [16]. The lack of a consensual definition leads to different bias, including an inconsistent measurement of SDM impact. Moreover, due to the significant variation in severity of mood disorders, contexts, comparators, and design of the included studies, their results have to be interpreted carefully.
Conclusions
SDM interventions using decision aids appear to improve patient satisfaction and engagement in the decision-making process. Extended models of SDM as collaborative care also demonstrated interest in the management of depression in primary care.
SDM represents a useful patient-centered approach easily feasible and applicable for clinical practice.
Stronger evidence about the use of SDM in mood disorders, especially in BD, is needed. Future studies should be designed to assess more clinical primary outcomes such as medication adherence, symptomatology, functioning, or quality of life.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R). Arch Gen Psychiatry. 2005;62(6):617–27.
Grande I, Berk M, Birmaher B, Vieta E. Bipolar disorder. Lancet. 2016;387(10027):1561–72.
Samalin L, de Chazeron I, Vieta E, Bellivier F, Llorca PM. Residual symptoms and specific functional impairments in euthymic patients with bipolar disorder. Bipolar Disord. 2016;18(2):164–73.
Malhi GS, Bassett D, Boyce P, Bryant R, Fitzgerald PB, Fritz K. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for mood disorders. Aust N Z J Psychiatry. 2015;49(12):1087–206.
Samalin L, Murru A, Vieta E. Management of inter-episodic periods in patients with bipolar disorder. Expert Rev Neurother. 2016;16(6):659–70.
Berk L, Hallam KT, Colom F, Vieta E, Hasty M, Macneil C, et al. Enhancing medication adherence in patients with bipolar disorder. Hum Psychopharmacol. 2010;25(1):1–16.
Akincigil A, Bowblis JR, Levin C, Walkup JT, Jan S, Crystal S. Adherence to antidepressant treatment among privately insured patients diagnosed with depression. Med Care. 2007;45(4):363–9.
Sheehan DV, Keene MS, Eaddy M, Krulewicz S, Kraus JE, Carpenter DJ. Differences in medication adherence and healthcare resource utilization patterns: older versus newer antidepressant agents in patients with depression and/or anxiety disorders. CNS Drugs. 2008;22(11):963–73.
Leclerc E, Mansur RB, Brietzke E. Determinants of adherence to treatment in bipolar disorder: a comprehensive review. J Affect Disord. 2013;149(1–3):247–52.
Loh A, Simon D, Wills CE, Kriston L, Niebling W, Härter M. The effects of a shared decision-making intervention in primary care of depression: a cluster-randomized controlled trial. Patient Educ Couns. 2007;67(3):324–32.
Elwyn G, Laitner S, Coulter A, Walker E, Watson P, Thomson R. Implementing shared decision making in the NHS. BMJ. 2010;341:c5146.
Tuckett D, Boulton M, Olson C, Williams A. Meeting between experts: an approach to sharing ideas in medical consultations. New York: Routledge; 1986.
Duncan E, Best C, Hagen S. Shared decision making interventions for people with mental health conditions. Cochrane Database Syst Rev. 2010;1:CD007297.
Tlach L, Wüsten C, Daubmann A, Liebherz S, Härter M, Dirmaier J. Information and decision-making needs among people with mental disorders: a systematic review of the literature. Health Expect. 2015;18(6):1856–72.
•• Fisher A, Manicavasagar V, Klin F, Juraskova I. Communication and decision-making in mental health: a systematic review focusing on bipolar disorder. Patient Educ Couns. 2016;99(7):1106–20. Very comprehensive review of studies of communication and decision-making in mental health-based samples including BD patients.
Makoul G, Clayman ML. An integrative model of shared decision making in medical encounters. Patient Educ Couns. 2006;60(3):301–12.
•• LeBlanc A, Herrin J, Williams MD, Inselman JW, Branda ME, Shah ND et al. Shared decision making for antidepressants in primary care: a cluster randomized trial. JAMA Intern Med. 2015;175(11):1761–70. One of the major studies evaluating a SDM intervention in MDD patients.
Aljumah K, Hassali MA. Impact of pharmacist intervention on adherence and measurable patient outcomes among depressed patients: a randomised controlled study. BMC Psychiatry. 2015;15:219.
van der Voort TY, van Meijel B, Hoogendoorn AW, Goossens PJ, Beekman AT, Kupka RW. Collaborative care for patients with bipolar disorder: effects on functioning and quality of life. J Affect Disord. 2015;179:14–22.
•• van der Voort TY, van Meijel B, Goossens PJ, Hoogendoorn AW, Draisma S, Beekman A, et al. Collaborative care for patients with bipolar disorder: randomised controlled trial. Br J Psychiatry. 2015;206(5):393–400. The only available study evaluating a collaborative care intervention that included a SDM approach for BD patients.
Wright DR, Haaland WL, Ludman E, McCauley E, Lindenbaum J, Richardson LP. The costs and cost-effectiveness of collaborative care for adolescents with depression in primary care settings: a randomized clinical trial. JAMA Pediatr. 2016;170(11):1048–54.
Richardson LP, Ludman E, McCauley E, Lindenbaum J, Larison C, Zhou C. Collaborative care for adolescents with depression in primary care: a randomized clinical trial. JAMA. 2014;312(8):809–16.
Unützer J, Katon W, Callahan CM, Williams JW Jr, Hunkeler E, Harpole L, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA 2002;288(22):2836–2845.
Grote NK, Katon W, Russo JE, Lohr MJ, Curran M, Galvin E. Collaborative care for perinatal depression in socioeconomically disadvantaged women: a randomized trial. Depress Anxiety. 2015;32(11):821–34.
Katon W, Russo J, Reed SD, Croicu CA, Ludman E, LaRocco A, et al. A randomized trial of collaborative depression care in obstetrics and gynecology clinics: socioeconomic disadvantage and treatment response. Am J Psychiatry 2015;172(1):32–40
Melville JL, Reed SD, Russo J, Croicu CA, Ludman E, LaRocco-Cockburn A, et al. Improving care for depression in obstetrics and gynecology: a randomized controlled trial. Obstet Gynecol. 2014;123(6):1237–46.
Ell K, Xie B, Quon B, Quinn DI, Dwight-Johnson M, Lee PJ. Randomized controlled trial of collaborative care management of depression among low-income patients with cancer. J Clin Oncol. 2008;26(27):4488–96.
Ell K, Katon W, Xie B, Lee PJ, Kapetanovic S, Guterman J, et al. One-year postcollaborative depression care trial outcomes among predominantly Hispanic diabetes safety net patients. Gen Hosp Psychiatry. 2011;33(5):436–42.
Dwight-Johnson M, Lagomasino IT, Hay J, Zhang L, Tang L, Green JM, et al. Effectiveness of collaborative care in addressing depression treatment preferences among low-income Latinos. Psychiatr Serv. 2010;61(11):1112–8.
Katon WJ, Lin EH, Von Korff M, Ciechanowski P, Ludman EJ, Young B, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363(27):2611–20.
Huffman JC, Mastromauro CA, Sowden GL, Wittmann C, Rodman R, Januzzi JL. A collaborative care depression management program for cardiac inpatients: depression characteristics and in-hospital outcomes. Psychosomatics. 2011;52(1):26–33.
Stewart JC, Perkins AJ, Callahan CM. Effect of collaborative care for depression on risk of cardiovascular events: data from the IMPACT randomized controlled trial. Psychosom Med. 2014;76(1):29–37.
Unützer J, Katon W, Williams JW Jr, Callahan CM, Harpole L, Hunkeler EM et al. Improving primary care for depression in late life: the design of a multicenter randomized trial. Med Care 2001;39(8):785–799.
• Stacey D, Légaré F, Col NF, Bennett CL, Barry MJ, Eden KB, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2014;(1):CD001431. Comprehensive review on decision aids for people facing health treatment or screening decisions.
Ivbijaro GO, Enum Y, Khan AA, Lam SS, Gabzdyl A. Collaborative care: models for treatment of patients with complex medical-psychiatric conditions. Curr Psychiatry Rep. 2014;16(11):506.
Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27(10):1361–7.
Archer J, Bower P, Gilbody S, Lovell K, Richards D, Gask L, et al. Collaborative care for depression and anxiety problems. Cochrane Database Syst Rev. 2012;10:CD006525.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Jean-Baptiste Genty, Laurent Boyer, Jorge Lopez-Castroman, and Mocrane Abbar declare no conflict of interest.
Ludovic Samalin has received grants, honoraria, or consulting fees from AstraZeneca, Bristol-Myers Squibb, Janssen-Cilag, Lundbeck, Otsuka, Sanofi-Aventis, and Takeda.
Pierre-Michel Llorca has received grants, honoraria, or consulting fees from AstraZeneca, Bristol-Myers Squibb, Janssen-Cilag, Lundbeck, and Otsuka.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Mood Disorders
Rights and permissions
About this article
Cite this article
Samalin, L., Genty, JB., Boyer, L. et al. Shared Decision-Making: a Systematic Review Focusing on Mood Disorders. Curr Psychiatry Rep 20, 23 (2018). https://doi.org/10.1007/s11920-018-0892-0
Published:
DOI: https://doi.org/10.1007/s11920-018-0892-0