Abstract
Purpose of Review
While clinicians have been using antidepressants for off-label indications in the treatment of chronic pain in recent years, newer studies have proven effectiveness and provided additional mechanistic understanding and defined potential adverse effects. As depression and chronic pain are frequently comorbid conditions, the use of antidepressants has allowed for treatment of both conditions concomitantly in the same patient population.
Recent Findings
The most commonly used antidepressants for chronic pain are tricyclic antidepressants (TCAs), though selective serotonin or noradrenaline reuptake inhibitors and other atypical antidepressants have been shown to be effective at treating chronic pain. In addition to neuropathic pain, bupropion has also demonstrated effectiveness in treating chronic pain caused by inflammatory bowel disease. Selective norepinephrine receptor inhibitors (SNRIs), including duloxetine, serve to suppress neuropathic pain by altering recovery of the noradrenergic descending inhibitory system in the spinal cord. While the direct mechanism of action is largely unknown, TCAs may suppress the noradrenergic descending inhibitory system to produce an antihyperalgesic effect.
Summary
The use of antidepressants offers alternative and adjunctive therapy options for patients suffering from chronic pain from various modalities. TCAs, mono-amine oxidase inhibitors, selective serotonin receptor inhibitors, SNRIs, and atypical antidepressants have been shown to have analgesic and sometimes antiinflammatory capabilities that are independent of their mood-stabilizing effects. Further studies are warranted to establish better safety profiles and efficacy of antidepressant use in chronic pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic pain is one of the leading cost burdens to the US healthcare system, estimated to exceed over $100 billion annually [1]. There are many different treatment options available for patients that suffer from chronic pain, ranging from pharmacological therapy to surgical interventions. As science has developed a better appreciation of the physiologic and psychologic causes of pain, additional understanding has evolved as to potential treatment modalities and strategies. While clinicians have prescribed antidepressants for many decades, off-label use for treating chronic pain has significantly increased in the past decade. In this regard, recent studies have proven their effectiveness and given further understanding of their mechanisms, drug-drug interactions, and adverse effects.
Neuropathic pain is defined by the International Association for the Study of Pain (IASP) as pain caused by a lesion or disease of the somatosensory nervous system [2]. Pain typically develops from an injury or pathology affecting the somatosensory pathways in the peripheral or central nervous system. Nociceptive stimuli that originate in the periphery are transported by primary sensory neurons through the dorsal horn of the personal cord and then to many brain structures throughout the ascending pain pathway. The descending fibers that originate in the brainstem suppress pain neurotransmission and act as a homeostatic regulator [3]. These descending fibers release serotonin and noradrenaline as their neurotransmitters and dysfunction of these systems is likely to induce dysfunctional descending serotonin or noradrenaline antinociceptive pathways. This explains why pain and depression are often comorbid conditions and helps to clarify why patients with chronic pain often develop depression in their disease burden [4]. As depression and chronic pain are frequently comorbid conditions, antidepressants have been used to treat both conditions concomitantly in the same patient population [3]. The most commonly used antidepressants for chronic pain are tricyclic antidepressants (TCAs), but selective serotonin or noradrenaline reuptake inhibitors and other atypical antidepressants have been proven to be effective in the treatment of chronic pain [3].
The proposed mechanism behind the analgesic properties of antidepressant drugs is typically described to result from the inhibition of monoamine reuptake in the CNS, which leads to increased activity of the descending pathways and their antinociceptive effects on pain homeostasis [3]. Antidepressants have analgesic effects that are independent of their effect on depression. This partly may be because dosages needed to achieve optimal analgesia are significantly lower than dosages used to treat depressed mood [5]. Additionally, evidence for their independence is that there are differences in analgesic effectiveness between different classes of antidepressants and that the delay in onset of analgesic effects after administration appears after a shorter time than their given antidepressant effect [6, 7]. Further, antidepressants have been shown to have a different risk profile and set of adverse effects when used at dosages used of analgesia [8].
Bupropion
Bupropion is a second-generation atypical antidepressant that is distinct from other classes of antidepressant that include SSRIs, SNRIs, TCAs, and monoamine oxidase inhibitors. The precise mechanism of action remains unknown but it has been hypothesized that bupropion acts via norepinephrine-dopamine reuptake inhibition [9]. It blocks the reuptake of dopamine twice as much as that of norepinephrine reuptake. While bupropion does not inhibit monoamine oxidase or serotonin reuptake, it has been shown to indirectly enhance the firing of serotonergic neurons by activation of downstream norepinephrine reuptake [10]. Additionally, bupropion acts as a noncompetitive nicotinic acetylcholine receptor antagonists [11].
Bupropion is indicated for the treatment of major depression, seasonal affective disorder, attention deficit hyperactivity disorder (ADHD), tobacco dependence, hypoactive sexual disorder, and obesity [9]. It may also be preferred by patients who want to minimize the risk of antidepressant-induced sexual dysfunction. Bupropion also has a relatively benign safety profile but does have some serious complications including a risk for seizures. The risk for seizures is dose-dependent and ranges from 0.1 to 4.0% at higher doses of up to 600 mg per day [12]. Moreover, bupropion’s risk for seizures is greatly increased in patients with eating disorders and eating disorders are considered a contraindication. Overall, bupropion’s risk for seizures is similar to the other typical antidepressants [13]. The most common side effects of buproprion include dry mouth nausea and insomnia [9]. The treatment of neuropathic pain with bupropion has been well established. A double-blind, randomized trial of bupropion SR for the treatment of various forms of neuropathic pain demonstrated a significant decrease in the interference of pain on quality of life while patients were receiving bupropion SR compared with a placebo [14].
In addition to neuropathic pain, bupropion has also shown some effectiveness in treating chronic pain that is caused by inflammatory bowel disease (IBD). IBD is a group of relapsing incurable diseases of the gastrointestinal tract and is comprised of two major disorders; ulcerative colitis and Crohn’s disease that have two distinct pathological processes [10]. Pain may arise from several different mechanisms, including partial blockage and gut distention as well as severe intestinal inflammation [15]. While most patients suffer from pain during acute flares of IDB that typically improve as disease activity decreases, a significant percentage of IDB patients will continue to have pain despite resolved inflammation and achieving what appears to be clinical remission. Evidence suggests that sensory and pain pathways sensitize during an acute flair of inflammation that causes chronic changes in afferent neurons and the CNS pain processing [15]. As a result, IBD can suffer from chronic pain. While current treatment is aimed at decreasing the number of relapses and lengthening remission, treating and addressing chronic and possible neuropathic pain that is caused by IBD is also needed to improve the quality of life.
A systematic review showed that the use of antidepressants did not have a statistically relevant impact on the course of inflammatory bowel disease; still, the treatment of IBD with bupropion has shown some promise. Recent studies have demonstrated that bupropion may have antiinflammatory properties in addition to analgesic capabilities that could have added benefit in the treatment in IBD [16]. Bupropion has also been shown to lower the levels of an inflammatory mediator TNF-α by increasing the intracellular cAMP that inhibits TNF-α synthesis [17]. It also reduces the levels of interferon-γ [18]. Additionally, recent animal studies have shown that bupropion possesses analgesic and antiinflammatory properties that are likely mediated via inhibition of prostaglandin synthesis and a probable central inhibitory mechanism [19]. Bupropion shows promise as a potential therapy for IBD as it has both analgesic and potential antiinflammatory properties. Further research is needed to elucidate the efficacy of bupropion for the treatment IBD in human models and clinical trials.
Serotonin-Norepinephrine Reuptake Inhibitors
Serotonin-norepinephrine reuptake inhibitors (SNRIs) are a widely used class of medications that are primarily used for treating depression. SNRIs are also used for managing anxiety disorders, obsessive compulsive disorder, attention deficit disorder, and chronic pain conditions [20]. In the treatment of chronic pain, SNRIs are used in musculoskeletal and low back pain as well as in neuropathic pain, fibromyalgia, and more recently postoperative pain. SNRIs are part of the antidepressant class of drugs that specifically target the presynaptic norepinephrine and serotonin transporters. This leads to increased concentrations of serotonin and norepinephrine in the synaptic clefts, and therefore increased stimulation of postsynaptic receptors [21]. Duloxetine serves to suppress neuropathic pain by altering the recovery of noradrenergic descending inhibitory system in the spinal cord [22]. Despite its wide efficacy, there are certain challenges that SNRIs pose to providers. The most common side effects reported with SNRIs are nausea, dry mouth, insomnia, constipation, fatigue, and increased blood pressure. In addition, SNRIs usually take from 8 to 14 weeks in order to achieve the maximal effect and finding the correct and effective dose that often takes multiple trials and monitoring. Discontinuation has been associated with a multitude of withdrawal symptoms; discontinuation syndrome most commonly causes dizziness, nausea, and headaches, among others [23]. There are currently five SNRIs that are used in practice: venlafaxine, desvenlafaxine, duloxetine, levomilnacipran, and milnacipran.
Duloxetine
Duloxetine is a serotonin-norepinephrine reuptake inhibitor (SNRIs) that has been used for managing depression. It has also widely been studied as a pharmacological option for the treatment of chronic pain conditions. Osteoarthritis is the most common joint disorder in the USA and can cause patients significant pain and physical impairment. Duloxetine has been studied as a pharmacological agent that can help with the management of osteoarthritic pain. A Japanese study recently has shown that in patients with chronic knee osteoarthritis, treatment with duloxetine (60 mg/day for 48 weeks) sustained improvement in pain [24]. It was also shown in this trial that long-term treatment with duloxetine improved physical, mental, and emotional health reported by both the patients and physicians [24]. Another study evaluated the efficacy of treatment with pregabalin and duloxetine and its effect on hand osteoarthritis. Duloxetine was reported to have a mild improvement in patient’s reported pain [25].
Neuropathic pain can negatively affect a patient’s quality of life. Diabetic peripheral neuropathy (DPN) is the most common cause of neuropathic pain in the world and affects nearly 50% of patients with diabetes [26]. Duloxetine has been demonstrated to be efficacious at reducing neuropathic pain; in a systematic review of three randomized clinical trials duloxetine (60 mg or 120 mg) effectively treated diabetic neuropathic pain [27]. In addition, studies have revealed the utility of duloxetine for cancer-related neuropathic pain; a randomized, double-blind clinical study using duloxetine on taxane-induced sensory neuropathy in breast cancer patients demonstrated effective pain relief [28]. For chemotherapy-related pain, duloxetine was shown to be effective in decreasing motor neuropathy and neuropathic pain reported by patients [29]. In addition, an ongoing Japanese study is currently testing the efficacy of duloxetine in cancer-related neuropathic pain, refractory to gabapentinoids and opioids [30].
Chronic low back pain (CLBP) is a very common condition that can drastically impact a patient’s quality of life physically, emotionally, and financially. Treatment options usually consist of NSAIDS and spinal interventions/therapies. If the pain is refractory, treatment options are limited. Duloxetine has been studied extensively for the treatment of CLBP and has been shown to be efficacious in reducing pain in multiple studies. One study demonstrated that duloxetine (60 mg) is effective at treating CLBP regardless of sex, age, duration, or pain severity [31]. The study also demonstrated that multiple sites of pain responded better to duloxetine than one isolated spot of CLBP [31].
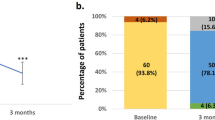
Another study has shown that significant reduction in pain within the first 4 weeks of duloxetine treatment or experiencing adverse effects from the duloxetine medication (nausea, somnolence, constipation) may be an important indicator in finding patients that will respond the greatest to duloxetine [32]. Depression can occur commonly with CLBP. A Japanese study recently has distinguished that duloxetine significantly improved pain in patients with CLBP. Their path analysis suggested that 91.1% of the analgesic effect occurred through direct analgesic affect, while 8.9% occurred by the antidepressant qualities of duloxetine [33].
Fibromyalgia is a condition that causes widespread musculoskeletal pain associated with poor sleep, cognitive disturbance, paresthesia, and fatigue. Current treatment often revolves around physical exercise and drug therapy with SSNRIs. Multiple studies have shown the ability of duloxetine to help with fibromyalgia pain; however, substantial efficacy is not consistently seen. One study has shown that although duloxetine’s role in treating somatic physical pain is unclear, the greatest effects may come from the treatment of the mental symptoms in fibromyalgia [34]. A Japanese phase 3 clinical trial has shown results suggesting that duloxetine is associated with improvement in pain and quality of life in Japanese patients [35]. A recent review study has shown that only a minority of patients will experience substantial benefit from treatment with duloxetine. The review stated that the majority of patients will experience minor but not substantial relief from fibromyalgia symptoms and often times the adverse effect of duloxetine outweighed the benefits [36]. A randomized control trial has shown that combining pregabalin and duloxetine improved multiple clinical outcomes versus just monotherapy with duloxetine; however, more research needs to be done to further characterize the effect [37].
Effective management of postoperative pain is vital in surgical patients and often can be very difficult. Postoperative pain has long been managed with opioids; however, their use carries substantial risk. A recent randomized double-blind study has explored the use of duloxetine in the management of postoperative pain after a lumbar laminectomy. The study showed that perioperative use of duloxetine and etoricoxib reduced postoperative pain and reduced the administration of opioids [38]. This study demonstrated that duloxetine/etoricoxib may be a useful adjuvant in the postoperative patient needing a multimodal analgesic approach. Another triple-blinded randomized control trial used duloxetine (60 mg/day for 14 days) after knee arthroplasty, and the results failed to reduce pain by postoperative day 14 [39]. Thus, additional studies need to be conducted in order to find and narrow the patient base to utilize duloxetine in the postoperative basis.
Chronic pain can be a difficult task to manage for a clinician. The initiative to look for alternative and a multimodal approach to managing pain has led to advancements and better understanding of pain. Duloxetine has demonstrated efficacy in a variety of chronic pain settings. Duloxetine has been shown to be effective in chronic musculoskeletal pain such as osteoarthritis and low back pain. It is also effective in treating neuropathic pain and may be effective in treating fibromyalgia. Thus, duloxetine can be a useful adjuvant to existing pain treatments and further studies need to be conducted to definitively understand the utility and therapeutic value of duloxetine. Table 1 summarizes recent studies which evaluate the efficacy of duloxetine for the management of various chronic pain conditions.
Milnacipran
Milnacipran is a selective serotonin and norepinephrine reuptake inhibitor (SNRI) that is FDA approved for the treatment of fibromyalgia [40]. Milnacipran is not currently FDA approved for the treatment of major depression. However, this is a frequent off-label application both within the USA and internationally [41]. Formulations include oral tablets available in 12.5-mg, 25-mg, 50-mg, or 100-mg dosages [41]. Use of milnacipran is contraindicated with concomitant or recent monoamine oxidase inhibitor (MAOI) use, uncontrolled narrow-angle glaucoma, and in children or adolescents [41]. It should be used cautiously among patients experiencing depression or suicidal ideation, a history of serotonin syndrome or neuroleptic malignant syndrome-like reactions, or with uncontrolled hypertension, seizures, or hepatoxicity. Conservative tapering is necessary to avoid withdrawal related adverse effects. The most commonly reported adverse effects include nausea and vomiting, headache, dizziness, insomnia, and palpitations [41].
A 2012 Cochrane update reviewed milnacipran independently for its use in both fibromyalgia and neuropathic pain [42, 43]. This update concluded that milnacipran contributed to moderate pain relief among patients experiencing fibromyalgia but was associated with increased incidence of adverse events and events related to withdrawal relative to alternate medications [43]. To evaluate the use of milnacipran in chronic neuropathic pain, the Cochrane update identified as a single study comprised of 40 participants. Reviewers concluded that milnacipran was nonsuperior to placebo and that evidence did not support the use of milnacipran among chronic neuropathic pain patients [42].
Since the Cochrane update, several recent studies continue to evaluate milnacipran as a fibromyalgia treatment modality. In a randomized, controlled, double-blind study, Pickering et al. evaluate the impact of conditioned pain modulation [44]. This study enrolled 54 women randomized to receive 100 mg of milnacipran or placebo for 1 month. The study reported no significant difference between milnacipran and placebo in conditioned pain modulation, global pain thresholds, or allodynia [44]. In a second randomized, controlled, double-blinded study, Petzke et al. assessed the effect of milnacipran on pressure-evoked pain sensitivity and cerebral processing of pain among patients with fibromyalgia [45]. Ninety-two patients were enrolled in this study and fMRI analysis demonstrated milnacipran-associated increases in cerebral activity within the caudatus nucleus, anterior insula, and amygdala, which are areas associated with pain inhibition. Researchers found that patients receiving milnacipran trended towards decreased pain sensitivity, but these results did not reach significance after adjustment for multiple comparisons [45]. Table 2 summarizes recent studies which evaluate the efficacy of milnacipran for the management of various chronic pain conditions.
Venlafaxine
Venlafaxine is a structurally novel antidepressant that is believed to improve depressive symptoms by potentiating neurotransmitter activity within the central nervous system and by inhibiting the synaptic reuptake of serotonin, norepinephrine, and dopamine [46]. Venlafaxine is extensively metabolized by the liver, and its active metabolite, O-desmethylvenlafaxine (ODV), also acts as a serotonin, norepinephrine, and dopamine reuptake inhibitor [46]. Formulations of venlafaxine include compressed oral tablets in 25-mg, 37.5-mg, 50-mg, 75-mg, or 100-mg dosages [46]. Venlafaxine is contraindicated in patients with hypersensitivity to venlafaxine hydrochloride or in patients who are concomitantly taking monoamine oxidase inhibitors (MAOIs) [46]. Caution should be used in pediatric patients and in patients with narrow-angle glaucoma, liver disease, or renal impairment. Patients with major depressive disorder should also be monitored for worsening depression, suicidal ideation, and changes in behavior. Commonly reported adverse effects included sustained hypertension, mydriasis, anxiety, nervousness, insomnia, and weight loss [46].
Emerging research assesses the utility of venlafaxine in the management of chronic neuropathic pain. In a 2017 systematic review, Aiyer et al. evaluated 13 studies assessing the treatment of neuropathic pain with venlafaxine [47]. The authors concluded that venlafaxine was generally well tolerated and, when compared witho placebo, venlafaxine demonstrated notable reductions in neuropathic pain. However, venlafaxine was nonsuperior to alternate, currently available medications for the treatment of neuropathic pain [47]. In a second review of existing literature, Trouvin et al. assessed the quality of 11 randomized clinical trials related to treatment of neuropathic pain with venlafaxine [48]. The authors found that eight trials compared venlafaxine with placebo and only one study incorporated a large number or participants (> 200) with control groups receiving pregabalin or carbamazepine. Furthermore, though most studies reported that venlafaxine was well tolerated with few reports of adverse effects, these studies had many internal limitations and were short in duration [48]. Venlafaxine may have utility in specific subpopulations. Farshchain et al. reported that venlafaxine reduced chemotherapy-induced peripheral neuropathy but had less effect on motor, cranial, sensory, or neuropathic pain than duloxetine [49].
Existing clinical evidence suggests that venlafaxine is well tolerated and effective in the treatment of neuropathic pain. However, while venlafaxine has a role in the treatment of neuropathic pain, the superior performance of readily available alternate medications such as pregabalin, carbamazepine, and duloxetine, venlafaxine suggests that the optimal clinical role for venlafaxine has yet to be defined. Furthermore, most existing randomized controlled trials involve small sample sizes, short durations, and are subject to internal biases. A large-scale randomized controlled trial may benefit patients taking venlafaxine and continued shared reporting of adverse events may increase awareness of rare and delayed complications.
Tricyclic Antidepressants
Tricyclic antidepressants (TCAs) are a class of medications that have primary been used for the treatment of refractory depression, dysthymia, and anxiety disorders. It also has been used in personality disorders, obsessive compulsive disorder, nocturnal enuresis, and more recently chronic pain. The mechanism of action of these drugs is through serotonin and norepinephrine transporter blockade, increasing the neurotransmitter concentration in the synaptic cleft [50]. Moreover, TCAs act on many other receptors, antagonizing the 5HT2, alpha, NMDA, histamine, and muscarinic receptors. In addition, TCAs are also potent inhibitors of sodium and calcium channels [50]. This broad mechanism of action has largely restricted the use of TCAs due to the side effect profile of the drugs. Many of the side effects are due to the antimuscarinic actions of the drugs, such as dry mouth, tachycardia, and urinary retention [51]. The alpha-blocking nature of the drugs may result in postural hypotension. TCA is commonly avoided given the serious and life-threating nature of overdose, which can cause cardiac toxicity, CNS toxicity, and anticholinergic poisoning [52]. TCA use in the elderly is often restricted given the high incidence of anticholinergic side effects such as confusion and hallucinations [52].
TCAs have been utilized in chronic pain conditions, most notably in neuropathic pain. The direct mechanism of action is unknown; however, studies have shown that TCA suppresses the noradrenergic descending inhibitory system producing an antihyperalgesic effect [53]. Amitriptyline has been used to treat neuropathic pain for years; however, unbiased evidence has yet to be seen. A recent review, including 17 studies, failed to demonstrate consistent benefit for amitriptyline for neuropathic pain [54]. Given the amount of success amitriptyline has had in practice, it still remains first line [54]. Another review study investigated the use of nortriptyline on neuropathic pain, and found little evidence to support the use of nortriptyline as first-line treatment [55]. In addition, a recent study compared the effectiveness of amitriptyline and nortriptyline for peripheral neuropathy. The study showed that both amitriptyline and nortriptyline are equivalent, providing a 23–26% reduction of pain based on a visual analog scale [56]. Thus, although the robust clinical evidence remains to be seen, TCAs have been used in practice successfully to treat neuropathic pain. Clinicians should quantify the potential benefit to be gained against the substantial side effect profile and risk of overdose when trying to treat neuropathic pain with TCA.
SSRIs
Selective serotonin reuptake inhibitors (SSRIs) are a class of medication frequently used to treat major depressive disorder and anxiety. The exact mechanism of action for SSRIs has yet to be conclusively described; however, several prevailing theories exist. SSRIs work by inhibiting the reuptake of serotonin from the synaptic cleft by the presynaptic neuron. The accumulation of serotonin within the synaptic cleft ultimately results in downregulation of 5HT1A receptors, which are inhibitory auto-receptors that decrease activation of serotonergic receptors when they are stimulated [57]. As a result of the downregulation of 5HT1A receptors, there is a net increase in firing of serotonergic neurons, which may improve depressive symptoms [57]. Alternatively, SSRIs may provide clinical benefit through varying degrees of inhibiting presynaptic reuptake of norepinephrine and dopamine, increased cyclic adenosine monophosphate levels (cAMP), or by increasing levels of brain derived neurotrophic factor (BDNF) in the hippocampus [58, 59]. BDNF has been linked to phosphorylation and stabilization of hippocampal NMDA receptors in rat models as well as inhibition of GABAergic signaling in mice [58, 59]. BDNF is hypothesized to alleviate depressive symptoms and promote emotional plasticity or resilience [60].
Despite an elusive mechanism of action, SSRIs have become essential pharmaceutical agents and are commonly used in the treatment of many medical conditions including anxiety, depression, obsessive compulsive disorder, posttraumatic stress disorder, and chronic pain conditions. Many drugs exist within this class including citalopram, escitalopram, fluoxetine, fluvoxamine, paroxetine, sertraline, and vilazodone. Dosing and adverse effects vary by medication. However, SSRIs are generally well tolerated with a promising safety profile. Common adverse effects include sexual dysfunction, cognitive dysfunction, alterations in energy levels, and QT prolongation among certain agents, most notably citalopram [61]. Furthermore, the US Food and Drug Association issued a 2011 warning that the use of SSRIs during pregnancy may be associated with persistent pulmonary hypertension of the newborn [62].
SSRIs have a poorly defined role in chronic pain management. Changes in the 5-hydroxytryptophan (5HT) have been reported in chronic pain, suggesting a role for SSRIs in the attenuation of related pain [63]. However, existing clinical trials evaluating the use of SSRIs in the treatment of chronic pain report inconclusive and inconsistent results. Patetos et al. conducted a review of 36 clinical trials investigating the role of SSRIs in chronic pain [63]. These studies included a heterogenous blend of cimetidine, escitalopram, fluvoxamine, sertraline, citalopram, paroxetine, and fluoxetine. The authors conclude that SSRIs may be effective in the management of chronic pain but report inconsistent findings and identify many internal biases and flaws in methodology that are often necessary in preliminary research. Further, large-scale randomized controlled studies will benefit this patient population and may help clarify the role and mechanism of action of SSRIs in chronic pain.
To evaluate the role of the SSRI fluoxetine as a potential morphine adjuvant in the management of nociceptive pain, Hamdy et al. conducted a controlled animal study involving 84 mice [64]. The group administered a combination of morphine 5 mg/kg, fluoxetine 1 mg/kg, or an equivalent volume of normal saline for nine consecutive days in mice weighing 20–30 g. Naloxone was administered to all mice on day 10 to investigate levels of morphine dependence. The group investigates the proposed inherent antinociceptive effect of fluoxetine, as well as the agent’s capacity to enhance morphine analgesia, reduce morphine tolerance, and prevent morphine dependence and its associated abstinence syndrome. The authors concluded that fluoxetine did not demonstrate antinociceptive properties either as a solitary agent or in combination with morphine. However, results indicate that fluoxetine use was associated with reduced morphine tolerance and dependence as well as decreased morphine-induced inflammation and improved stabilization of glutamate and norepinephrine neurotransmitter levels [64]. This suggests a potential role for SSRIs as opioid adjuncts, particularly in the management of inflammatory pain. Table 3 summarizes recent studies which evaluate the efficacy of SSRIs for the management of various chronic pain conditions.
Conclusion
The use of antidepressants offers alternative and adjunctive therapy options for patients suffering from chronic pain from various etiologies. TCAs, MAO inhibitors, SSRIs, SNRIs, and atypical antidepressants have been shown to have analgesic and sometimes antiinflammatory capabilities that are independent to their mood-stabilizing abilities. It is believed that antidepressants are able to increase the activity of the descending pathways and their antinociceptive effects on pain homeostasis. They are thought to accomplish this by inhibiting monoamine reuptake in the CNS and increasing the amount of monoamines that are available in the synaptic cleft. While the different antidepressants share a similar mechanism in relieving pain, it has been shown that there are differences in analgesic effectiveness between different classes of antidepressants. Additionally, antidepressants need much lower dosages for their antinociceptive effects and have different side effects and safety profiles when used at these dosages. Further studies are still needed to establish better safety profiles and efficacy of antidepressant use in chronic pain patients.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Jackson KC, St. Onge EL. Antidepressant pharmacotherapy: considerations for the pain clinician. Pain Pract. 2003;3:135–43.
Murnion BP. Neuropathic pain: current definition and review of drug treatment. Aust Prescr NPS Med Wise. 2018;41:60–3.
Mika J, Zychowska M, Makuch W, Rojewska E, Przewlocka B. Neuronal and immunological basis of action of antidepressants in chronic pain – clinical and experimental studies. Pharmacol Reports. 2013;65(6):1611–21.
Morris DW, Trivedi MH, Fava M, Wisniewski SR, Balasubramani GK, Khan AY, et al. Diurnal mood variation in outpatients with major depressive disorder. Depress Anxiety. 2009;26:851–63.
Goldstein DJ, Lu Y, Detke MJ, Lee TC, Iyengar S. Duloxetine vs. placebo in patients with painful diabetic neuropathy. Pain. 2005;116:109–18.
Hirschfeld RMA, Mallinckrodt C, Lee TC, Detke MJ. Time course of depression-symptom improvement during treatment with duloxetine. Depress Anxiety. 2005;21:170–7.
Mico J, Ardid D, Berrocoso E, Eschalier A. Antidepressants and pain. Trends Pharmacol Sci. 2006;27:348–54.
•• Riediger C, Schuster T, Barlinn K, Maier S, Weitz J, Siepmann T. Adverse effects of antidepressants for chronic pain: a systematic review and meta-analysis. Front Neurol. 2017;8:307. A systematic review of adverse effects of antidepressants.
Fava M, Rush AJ, Thase ME, Clayton A, Stahl SM, Pradko JF, Johnston JA. 15 years of clinical experience with bupropion HCl: from bupropion to bupropion SR to bupropion XL. Prim Care Companion J Clin Psychiatry. 2005;7(3):106–13.
Mikocka-Walus AA, Turnbull DA, Moulding NT, Wilson IG, Andrews JM, Holtmann GJ. Antidepressants and inflammatory bowel disease: a systematic review. Clin Pract Epidemiol Ment Health Bentham Science Publishers. 2006;2:24.
Arias HR. Is the inhibition of nicotinic acetylcholine receptors by bupropion involved in its clinical actions? Int J Biochem Cell Biol. 2009;41:2098–108.
Dhillon S, Yang LPH, Curran MP. Bupropion: a review of its use in the management of major depressive disorder. Drugs. 2008;68:653–89.
Montgomery SA. Antidepressants and seizures: emphasis on newer agents and clinical implications. Int J Clin Pract. 2005;59:1435–40.
Semenchuk MR, Sherman S, Davis B. Double-blind, randomized trial of bupropion SR for the treatment of neuropathic pain. Neurology. 2001;57:1583–8.
Bielefeldt K, Davis B, Binion DG. Pain and inflammatory bowel disease. Inflamm Bowel Dis NIH Public Access. 2009;15:778–88.
Sadeghi H, Hajhashemi V, Minaiyan M, Movahedian A, Talebi A. Further studies on anti-inflammatory activity of maprotiline in carrageenan-induced paw edema in rat. Int Immunopharmacol. 2013;15:505–10.
Kast RE, Altschuler EL. Remission of Crohn’s disease on bupropion. Gastroenterology. 2001;121:1260–1.
Brustolim D, Ribeiro-dos-Santos R, Kast RE, Altschuler EL, Soares MBP. A new chapter opens in anti-inflammatory treatments: the antidepressant bupropion lowers production of tumor necrosis factor-alpha and interferon-gamma in mice. Int Immunopharmacol. 2006;6:903–7.
Hajhashemi V, Khanjani P. Analgesic and anti-inflammatory activities of bupropion in animal models. Res Pharm Sci Wolters Kluwer -- Medknow Publications. 2014;9:251–7.
Spina E, Trifirò G, Caraci F. Clinically significant drug interactions with newer antidepressants. CNS Drugs. Springer International Publishing. 2012;26:39–67.
Debonnel G, Saint-André E, Hébert C, de Montigny C, Lavoie N, Blier P. Differential physiological effects of a low dose and high doses of venlafaxine in major depression. Int J Neuropsychopharmacol. 2007;10:51–61.
• Ito S, Suto T, Saito S, Obata H. Repeated administration of duloxetine suppresses neuropathic pain by accumulating effects of noradrenaline in the spinal cord. Anesth Analg. 2018;126:298–307. A mechanism of action by which duloxetine serves to reduce neuropathic pain.
Fava GA, Benasi G, Lucente M, Offidani E, Cosci F, Guidi J. Withdrawal symptoms after serotonin-noradrenaline reuptake inhibitor discontinuation: systematic review. Psychother Psychosom Karger Publishers. 2018;87:195–203.
Uchio Y, Enomoto H, Ishida M, Tsuji T, Ochiai T, Konno S. Safety and efficacy of duloxetine in Japanese patients with chronic knee pain due to osteoarthritis: an open-label, long-term, phase III extension study. J Pain Res. 2018;11:1391–403.
Sofat N, Harrison A, Russell MD, Ayis S, Kiely PD, Baker EH, et al. The effect of pregabalin or duloxetine on arthritis pain: a clinical and mechanistic study in people with hand osteoarthritis. J Pain Res Dove Press. 2017;10:2437–49.
Iqbal Z, Azmi S, Yadav R, Ferdousi M, Kumar M, Cuthbertson DJ, et al. Diabetic peripheral neuropathy: epidemiology, diagnosis, and pharmacotherapy. Clin Ther. 2018;40:828–49.
Lunn MP, Hughes RA, Wiffen PJ. Duloxetine for treating painful neuropathy or chronic pain. In: Lunn MP, editor. Cochrane database Syst Rev. Chichester: John Wiley & Sons, Ltd; 2009. p. CD007115.
Avan R, Janbabaei G, Hendouei N, Alipour A, Borhani S, Tabrizi N, et al. The effect of pregabalin and duloxetine treatment on quality of life of breast cancer patients with taxane-induced sensory neuropathy: a randomized clinical trial. J Res Med Sci Wolters Kluwer -- Medknow Publications. 2018;23:52.
Farshchian N, Alavi A, Heydarheydari S, Moradian N. Comparative study of the effects of venlafaxine and duloxetine on chemotherapy-induced peripheral neuropathy. Cancer Chemother Pharmacol. Springer Berlin Heidelberg. 2018;82:787–93.
Matsuoka H, Ishiki H, Iwase S, Koyama A, Kawaguchi T, Kizawa Y, et al. Study protocol for a multi-institutional, randomised, double-blinded, placebo-controlled phase III trial investigating additive efficacy of duloxetine for neuropathic cancer pain refractory to opioids and gabapentinoids: the DIRECT study. BMJ Open British Medical Journal Publishing Group. 2017;7:e017280.
Alev L, Fujikoshi S, Yoshikawa A, Enomoto H, Ishida M, Tsuji T, Ogawa K, Konno S Duloxetine 60 mg for chronic low back pain: post hoc responder analysis of double-blind, placebo-controlled trials. J Pain Res. Dove Press; 2017;10:1723–1731.
Tsuji T, Itoh N, Ishida M, Ochiai T, Konno S. Response to duloxetine in chronic low back pain: exploratory post hoc analysis of a Japanese phase III randomized study. J Pain Res. 2017;10:2157–68.
Enomoto H, Fujikoshi S, Funai J, Sasaki N, Ossipov M, Tsuji T, et al. Assessment of direct analgesic effect of duloxetine for chronic low back pain: post hoc path analysis of double-blind, placebo-controlled studies. J Pain Res. 2017;10:1357–68.
Lunn MP, Hughes RA, Wiffen PJ. Duloxetine for treating painful neuropathy or chronic pain. In: Lunn MP, editor. Cochrane Database of Systematic Reviews. Chichester, UK: John Wiley & Sons, Ltd; 2009. p. CD007 115.
Murakami M, Osada K, Mizuno H, Ochiai T, Alev L, Nishioka K. A randomized, double-blind, placebo-controlled phase III trial of duloxetine in Japanese fibromyalgia patients. Arthritis Res Ther BioMed Central. 2015;17:224.
Welsch P, Üçeyler N, Klose P, Walitt B, Häuser W. Serotonin and noradrenaline reuptake inhibitors (SNRIs) for fibromyalgia. Cochrane Database Syst Rev Wiley-Blackwell. 2018;2:CD010292.
Gilron I, Chaparro LE, Tu D, Holden RR, Milev R, Towheed T, et al. Combination of pregabalin with duloxetine for fibromyalgia. Pain. 2016;157:1532–40.
Attia JZ, Mansour HS. Perioperative duloxetine and etoricoxibto improve postoperative pain after lumbar laminectomy: a randomized, double-blind, controlled study. BMC Anesthesiol BioMed Central. 2017;17:162.
YaDeau JT, Brummett CM, Mayman DJ, Lin Y, Goytizolo EA, Padgett DE, et al. Duloxetine and subacute pain after knee arthroplasty when added to a multimodal analgesic regimen. Anesthesiology The American Society of Anesthesiologists. 2016;125:561–72.
Forest Pharmaceuticals I. SAVELLA® Tablets (milnacipran HCl) [Internet]. PRESCRIBING INFORMATION. 2011. p. 1–27.
Keks NA, Hope J, Keogh S, Copolov DL. Milnacipran: serotonin-noradrenaline reuptake inhibitor approved for fibromyalgia may be a useful antidepressant. Australas Psychiatry. 2018;26:537–40.
Derry S, Phillips T, Moore RA, Wiffen PJ. Milnacipran for neuropathic pain in adults. Cochrane Database Syst Rev. 2015;(7):CD011789.
Cording M, Derry S, Phillips T, Moore RA, Wiffen PJ. Milnacipran for pain in fibromyalgia in adults. Cochrane Database Syst Rev. 2015;(10):CD008244.
Pickering G, Macian N, Delage N, Picard P, Cardot J-M, Sickout-Arondo S, et al. Milnacipran poorly modulates pain in patients suffering from fibromyalgia: a randomized double-blind controlled study. Drug Des Devel Ther. 2018;12:2485–96.
Petzke F, Jensen KB, Kosek E, Choy E, Carville S, Fransson P, et al. Using fMRI to evaluate the effects of milnacipran on central pain processing in patients with fibromyalgia. Scand J Pain. 2013;4:65–74.
Wyeth Pharmaceuticals. EFFEXOR - venlafaxine hydrochloride tablet [Internet]. Wyeth Pharmaceuticals Inc. 2008. p. 1–21.
Gallagher HC, Gallagher RM, Butler M, Buggy DJ, Henman MC. Venlafaxine for neuropathic pain in adults. Cochrane Database Syst Rev. 2015;(8):CD011091.
Trouvin A-P, Perrot S, Lloret-Linares C. Efficacy of venlafaxine in neuropathic pain: a narrative review of optimized treatment. Clin Ther. 2017;39:1104–22.
Farshchian N, Alavi A, Heydarheydari S, Moradian N. Comparative study of the effects of venlafaxine and duloxetine on chemotherapy-induced peripheral neuropathy. Cancer Chemother Pharmacol. 2018;82:787–93.
Kerr GW, McGuffie AC, Wilkie S. Tricyclic antidepressant overdose: a review. Emerg Med J. 2001;18(4):236–41.
Trindade E, Menon D, Topfer LA, Coloma C. Adverse effects associated with selective serotonin reuptake inhibitors and tricyclic antidepressants: a meta-analysis. CMAJ. 1998;159(10):1245–52.
Lynch R. Tricyclic antidepressant overdose. Emerg Med J. 2002;19:596.
Hiroki T, Suto T, Saito S, Obata H. Repeated administration of amitriptyline in neuropathic pain. Anesth Analg. 2017;125:1281–8.
Moore RA, Derry S, Aldington D, Cole P, Wiffen PJ. Amitriptyline for neuropathic pain in adults. Cochrane Database Syst Rev. 2015;(7):CD008242.
Derry S, Wiffen PJ, Aldington D, Moore RA. Nortriptyline for neuropathic pain in adults. Cochrane Database Syst Rev. 2015;1:CD011209.
Liu W-Q, Kanungo A, Toth C. Equivalency of tricyclic antidepressants in open-label neuropathic pain study. Acta Neurol Scand Wiley/Blackwell (10.1111). 2014;129:132–41.
Blier P, Abbott F. Putative mechanisms of action of antidepressant drugs in affective and anxiety disorders and pain. J Psychiatry Neurosci. 2001;26:37–43.
Slack SE, Pezet S, McMahon SB, Thompson SWN, Malcangio M. Brain-derived neurotrophic factor induces NMDA receptor subunit one phosphorylation via ERK and PKC in the rat spinal cord. Eur J Neurosci. 2004;20:1769–78.
Henneberger C, Jüttner R, Rothe T, Grantyn R. Postsynaptic action of BDNF on GABAergic synaptic transmission in the superficial layers of the mouse superior colliculus. J Neurophysiol. 2002;88:595–603.
Lee B-H, Kim Y-K. The roles of BDNF in the pathophysiology of major depression and in antidepressant treatment. Psychiatry Investig. 2010;7:231–5.
U.S. Food and Drug Administration (FDA). Abnormal heart rhythms associated with high doses of Celexa (citalopram hydrobromide) [Internet]. FDA Drug Safety Communication. 2017. p. 1.
Research. C for DE and. Drug safety and availability - FDA drug safety communication: selective serotonin reuptake inhibitor (SSRI) antidepressant use during pregnancy and reports of a rare heart and lung condition in newborn babies. U S food drug Adm home page. Cent Drug Eval Res. 2011.
Patetsos E, Horjales-Araujo E. Treating chronic pain with SSRIs: what do we know? Pain Res Manag. 2016;2016:2020915.
Hamdy MM, Elbadr MM, Barakat A. Fluoxetine uses in nociceptive pain management: a promising adjuvant to opioid analgesics. Fundam Clin Pharmacol. 2018;32:532–46.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Ivan Urits, Jacquelin Peck, Mariam Salisu Orhurhu, John Wolf, Riki Patel, Vwaire Orhurhu, and Omar Viswanath declare no conflict of interest. Alan D. Kaye discloses that he is on the Speakers Bureau for Depomed, Inc. and Merck.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Topical Collection on Other Pain
Rights and permissions
About this article
Cite this article
Urits, I., Peck, J., Orhurhu, M.S. et al. Off-label Antidepressant Use for Treatment and Management of Chronic Pain: Evolving Understanding and Comprehensive Review. Curr Pain Headache Rep 23, 66 (2019). https://doi.org/10.1007/s11916-019-0803-z
Published:
DOI: https://doi.org/10.1007/s11916-019-0803-z