Abstract
Purpose of Review
Osteoporosis ranks high among morbidities in the elderly as it is a natural process to lose bone, making them susceptible to fractures from minor falls. The cost of managing these patients is staggering. The fractures can be prevented with better care of the elderly, and by treating the major predisposing factor, osteoporosis. Clinicians and scientists, in general, constantly look for early diagnostic and prognostic indicators for osteopenia and osteoporosis to proactively prevent fractures. Dental panoramic radiography (DPR) is a rotational pantomography used for identifying dental pathology in patients. Early signs of osteopenia and osteoporosis can be identified in DPR. The usefulness of notable jaw changes in DPR to predict osteopenia and osteoporosis is still evolving as more studies continue to delve into this concept. The purpose of this review is to present advances made in the practical application of DPR for predicting early onset of osteopenia and osteoporosis.
Recent Findings
Dental panoramic radiography, a form of tomography commonly used by dental practitioners, has been the standard of care for decades for detecting dento-alveolar pathology. Several technological advancements have taken place with respect to the use of DPR. These include conversion from plain film to digital radiography, advancements in the manufacture of flat panel detectors, and accurate imaging of the layers of mandible and maxilla that has become possible with appropriate patient positioning within the focal trough of the machine. Improvements in the software infrastructure make it easier to view, enhance, and save the radiographic images. The radiographic appearance of the trabecular bone within the mandible and indices measured from the dental panoramic radiographs focusing on the inferior cortex of the mandible are considered useful tools for identifying asymptomatic individuals with osteoporosis or at risk for developing osteoporosis. These indices apparently correlate with risks of fragility fractures of osteoporosis in other parts of the body.
Summary
Dental panoramic radiography (DPR) is a commonly used radiographic procedure in dentistry for evaluation of teeth and associated maxillofacial structures. The evaluation of the inferior border of the mandible for reduction or loss of cortical thickness and evaluation of the trabecular bone within the mandible are helpful markers for early signs of osteopenia to identify patients at risk for osteoporosis. This review focused on research advancements on practical application of DPR in early identification of osteopenia and osteoporosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ten million people already have osteoporosis and 18 million have low bone mass and an increased risk for osteoporosis [1]. Although osteoporosis is most prevalent in postmenopausal Caucasian women, it occurs in all populations, affects all ages, and it induces substantial physical, emotional, and financial burden. There are significant geographic disparities in the occurrence of osteoporosis worldwide [2]. Osteoporosis predisposes to wrist, vertebral, and hip fractures with consequent severe pain and disability. Early identification of the risk factors contributing to osteoporosis is vital for minimizing osteoporotic fractures, prolonged hospitalization due to fragility fractures, and financial burden of long-term recovery. [2]. This review explores the use of a dental healthcare setting and practical application of dental panoramic radiograph to identify undiagnosed osteoporosis patients and individuals at risks for developing osteoporosis so the oral healthcare provider can refer for further testing, diagnosis, and treatment.
Osteoporotic Changes in Orofacial Bones
Osteoporosis ranks high among morbidities in the elderly as it is a natural process to lose bone, making them susceptible to fractures from minor falls. An estimated 10 million people age 50 years and above have osteoporosis in the USA [3]. Among them, 80% are women and 20% are men [3]. Hip and vertebral fragility fractures incur enormous costs for treatment and rehabilitation, so early identification of osteoporosis, a leading cause of fragility fractures, is an important public health masterplan. The high cost of managing osteoporosis suggests a need for early diagnosis and preventive therapies to reduce healthcare costs. Improvements in tools amenable to early diagnostic and prognostic indicators for osteopenia and osteoporosis are ways to proactively prevent debilitating osteoporotic fractures. Early signs of osteopenia and osteoporosis can be readily identified in dental panoramic radiography (DPR).
The entire skeleton physiologically balances bone formation and resorption to maintain bone homeostasis [4]. Increased bone remodeling and dysregulated bone remodeling resulting in changes in bone matrix and mineral composition are the hallmarks of osteoporosis. [4]. Bone mesenchymal stem cells (MSCs) are central to the bone formation process; they also play distinctive functions in orofacial bone modeling and remodeling. Increased age-related cellular senescence of MSCs and osteoblast lineage cells support the decrease in bone mass in osteoporosis [5] and these changes are assessable in the orofacial bones. In the jaws, orofacial MSCs (OFMSCs) are distinctly different phenotypically and functionally from MSCs residing in non-oral skeletal sites [6]. OFMSCs are highly proliferative with much higher population doubling capacity. The jaw bones are also not spared from age-related skeletal changes [6, 7] because craniofacial bones, especially the mandible, readily display radiological features of osteoporosis. The mandible has a well-defined cortical border so that the increased bone remodeling rate coupled with negative remodeling balance and microarchitectural deterioration present in the mandible as increased cortical porosity and loss of cortical thickness. Both maxilla and mandible also display thinning and loss of bone trabeculae [7, 8]. Another unique characteristic of orofacial bones is the high occurrence of medication-related osteonecrosis of the jaws (MRONJ) [9]. Antiresorptive medications like bisphosphonates and denosumab that are highly efficacious in the treatment of osteoporosis are actually the leading causes for MRONJ. Why the jaw bones are highly susceptible to MRONJ is yet to be fully defined [10, 11]
Fracture Risk Assessment Tool (FRAX) [12] is based on the individual patient data or modeling including bone mineral density (BMD) at the femoral neck. Many tools and indices have been developed using tomographic images obtained to evaluate teeth and jaws but not osteoporosis specifically. The DPR risk assessment tool is an added benefit for patients undergoing routine dental care because any suspected cases of osteoporosis can be referred to their primary care physician for more specific BMD assessment via additional risk assessment tools and dual energy X-ray absorptiometry (DEXA) scans [13••].
Practical Application of Panoramic Radiography for Osteoporosis
Panoramic radiographic technique captures sections of orofacial anatomy within the required plane and displays the image as a continuous structure. Since mandible and maxilla are significantly curved bones, the rotational tomography is also curved but the images acquired appear flat. In theory, there are two midlines for the panoramic image—an anterior midline and a posterior midline. Due to the type of radiographic technique, various position-related and unrelated (“ghosts”) artifacts form within the displayed image. All panoramic radiographic machines currently available are based on digital imaging platforms. The acquisition, storage, and display are all digitally captured data. Due to better understanding of the physics and the focal trough (image layer), current panoramic radiographic machines can deliver consistently high-quality digital images suitable for research and clinical applications. However, there are certain factors that cannot be changed including the “focal trough” which is a fixed area within the machine path where the patient is positioned to acquire the tomographic slice. The focal trough is narrow anteriorly, so it corresponds with the narrow alveolar process in the anterior mandible and maxilla. The focal trough is wider posteriorly so that it also corresponds with the wider alveolar processes of the maxilla and mandible. Due to the nature of the focal trough and the fact that the patient is at a specific distance from both the X-ray beam source and the detector [digital detectors like charge coupled devices (CCD) or complementary metal oxide semiconductors (CMOS)], there occurs a magnification of image layer. In addition, variations in patient positioning within the focal trough may create uneven magnifications of the anatomy. Therefore, panoramic radiography is a highly technique-sensitive imaging method, but still provides very informative structural information. The bony anatomy displayed on the radiograph is a slice of the anatomy, so information pertinent to the cortical bone is better displayed than trabecular bone. The cortical bone within the focal trough presents a better indication of the actual mandibular thickness if the patient is positioned accurately within the panoramic X-ray machine and does not move during image exposure [14].
Alveolar Trabecular Bone Pattern
It has been reported that bone turnover in the trabecular bone of the general skeleton is eight times higher than that of the cortical bone; therefore, trabecular bone pattern of the femoral neck and the vertebral bodies can be used for diagnosis of osteoporosis [15]. However, in the mandible and maxilla, the trabecular bone pattern undergoes significant changes due to the presence of teeth and incidental changes to the alveolar bone caused by dental infections. These changes could make alveolar bone radiographically sclerotic to become an un-usable tool for assessment of osteoporosis like that of femoral neck or the vertebral body. Nevertheless, generalized significant loss of trabecular bone as would be noted on the panoramic radiographs (osteopenia) (Fig. 1) is still considered a useful marker in patients who were not previously tested for BMD or simply unaware of their condition. These patients are prime candidates for a referral to physicians for complete evaluation of their BMD and if necessary, interventional measures can be instituted to treat osteoporosis. Lindh and co-workers used intraoral radiography to propose a classification of jawbone trabecular pattern that is easy to use in clinical situations [16]. The trabecular patterns assessable on dental radiographs were classified as type 1- sparse trabeculation; type 2—heterogeneous or mixed trabeculation (sparse and dense); and type 3—dense homogeneous trabeculation. The usefulness of this mandibular alveolar trabecular classification pattern to identify individuals with osteopenia or osteoporosis was however rated as average and not good because 2 out of 5 studies showed low or no significance [17, 18]. Other studies that used standard quantitative methods as a prescreening tool to identify osteoporosis in the mandible did also not result in any consensus among the researchers regarding direct detection, but they were still useful for estimating risk for development of osteoporosis [16, 19, 20•]. There are still some challenges with development of accurate measurement indices because assessment of mandibular radiographic changes in mild to moderate postmenopausal women did not show any correlation with BMD [21] and other studies were inconclusive because the panoramic mandibular indices were not reliable [22].
Panoramic radiograph (A) shows several missing teeth. The mandibular cortical and trabecular bone changes consistent with moderate to severe osteopenia. The external oblique ridges bilaterally appear dense and isolated in the backdrop of reduced trabecular density (arrows). The inferior border of the mandible is not significantly impacted compared to the trabecular pattern and density. Several missing teeth, residual roots, and apical dental infections were noted in this radiograph. The pathognomonic sign is the disappearance of the cortical boundaries of the inferior alveolar nerve canal and hence identification of inferior alveolar nerve canal (IAN) becomes a task. Panoramic radiograph (B) shows partially edentulous maxilla and mandible and showing radiographic signs of decreased trabecular bone within the mandible suggestive of mild to moderate osteopenia. Note the thinning of inferior border of the mandible suggestive of reduced cortical width(arrows). An implant is planned in the region of left mandibular premolars. The IAN canal is indistinct here like other osteopenic scenarios. Panoramic radiograph (C) shows moderate to severe osteopenia with resorption of mandibular trabecular pattern and thinning of inferior cortex (arrows). The external oblique ridges are markedly dense in the backdrop of osteopenic trabecular bone (arrowheads). The patient is partially edentulous. Also, the IAN canal is very indistinct suggestive of significant bone resorption within the mandible
Evidence Linking Panoramic Morphometric Indices and Osteoporosis
Mandibular inferior cortex thickness and trabecular pattern noted on panoramic radiographs are useful tools for identification of individuals at risk for developing osteoporosis and low BMD. In addition, Taguchi and co-workers as well as Carmo and colleagues have concluded that individuals with thin inferior cortex of the mandible (< 3 mm) may be at risk for reduced BMD and osteoporosis but not fragility fractures [18, 23]. However, those with severely eroded inferior cortex of the mandible are at a higher risk of low skeletal BMD, osteoporosis, and fragility fractures. These assertions were based on studies within the last three decades (1990–2020) that validated the correlation of panoramic mandibular indices with DEXA and BMD assessments [24]. The findings were also independently supported by other groups [Kavitha et al., Kim et al., and Roberts et al.]. Additionally, Ren and colleagues developed a new static shape model after initial application of convoluted neural network based on trabecular pattern recognition to rule-in or rule-out osteoporosis [25•]. A definitive quantification of the methodology is still needed to support clinical application of the findings. Although artificial intelligence (AI)-related research is currently underway by researchers around the world, definitive approaches related to dental radiography are not yet solidified. AI-related work needs large samples of patient data (panoramic radiographs) for both machine learning and deep convoluted neural network recognition [25•]. Tanaka and colleagues reported that in Chinese females, a combination of age over 60 years and loss of 3.5 or more teeth, constitute risk factors for osteoporosis using panoramic radiograph radiomorphometric indices and artificial intelligence algorithms [26•]. However, a meta-analysis showed that fractal dimension, which represents a quantitative description of the degree of irregularity of complex surfaces within bone, failed to demonstrate a definitive diagnostic model for either osteoporosis detection or loss of BMD when compared with healthy controls. So, fractal dimension of bone is not considered a good indicator for risk assessment among asymptomatic individuals [27]. According to Calciolari and colleagues [28], indices like mandibular cortical index (MCI) or Klemetti index [29, 30] and panoramic mandibular index (PMI) [31] are tools that could be used to screen for individuals with low BMD. There are still some limitations on use of these indices mainly within the observer-based studies and the unreliable magnification noted on panoramic radiographs due to patient positioning [32].
Mandibular Cortical Index (MCI)
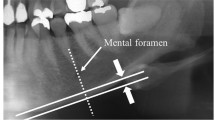
Mandibular cortical width has been established as a reliable marker to show that individuals with active loss of BMD are at a higher risk for osteoporosis. This index was initially proposed by Klemetti, Kolmakov, and Kröger in 1994 [29]. The mandibular cortical thickness was measured distally from the mental foramen and classified into the following three groups based on several criteria (Fig. 2):
-
C1: The endosteal margin of the cortex is even and sharp on both sides.
-
C2: The endosteal margin shows semilunar defects (lacunar resorption) and seems to form endosteal cortical residues on one or both sides.
-
C3: The cortical layer becomes porous and formed heavy endosteal cortical residues.
Panoramic radiograph (MCI-C1) shows a drawing depicting a normal mandibular cortical bone (inferior border) with even and sharp cortices bilaterally. Panoramic radiograph (MCI-C2) shows a drawing depicting the semilunar defects within the endosteal margin. Panoramic radiograph (MCI-C3) shows a drawing depicting the increased porosity of the endosteal margin with shallow and wider scalloped cortical margins. The drawing on the panoramic radiograph (PMI) depicts the cortical thickness measurement as well as the measurements of the distance between inferior margin of the mental foramen to the inferior border of the mandibular cortex. A ratio is calculated based on these two measurements which is considered the panoramic mandibular index
Reviews of the association between MCI and osteoporosis as was reported by Taguchi and associates [18, 19, 24] suggest that MCI may be helpful to identify individuals with low skeletal BMD or osteoporosis because of a strong correlation with spinal bone density measurements using DEXA.
Panoramic Mandibular Index (PMI) and Mental Index
PMI as proposed by Benson and colleagues [31] is a two-part index—panoramic mandibular index (superior) and panoramic mandibular index (inferior). Each is derived by dividing the thickness of mandibular cortex by the distance between either the superior margin of the mental foramen (PMI-superior) and the inferior border of the mandible or from the inferior margin of the mental foramen (PMI-inferior) to the inferior border of the mandible (Fig. 2). Since the superior border of the mental foramen is often radiographically difficult to identify in edentulous patients because of changes caused by the alveolar resorption, Benson and colleagues recommended that the measurements taken from the inferior border of the mental foramen (PMI-inferior) to the inferior border of the mandible should be the standard PMI [31] (Fig. 2). The precision of PMI was evaluated by Güngör and colleagues [33] who stated that the index appears to be consistent in an observer-based study. They recommended that more studies are needed to validate this information although prior research by Ledgerton and co-workers showed that this index was not reliable [34]. They proposed the use of the thickness of mandibular inferior cortex at the mental foramen and called it the mental index. It is measured bilaterally on a panoramic radiograph and the average is computed.
Taken together and based on review studies, MCI is universally used more than PMI. [35]. This is probably due to the wider discrimination of the measurements obtained between normal health individuals compared to osteoporotic patients. Haster and colleagues [35] reported that the mean MCI value was 2.88 mm in patients with osteoporosis compared to 3.70 mm in those without osteoporosis. However, the mean PMI value was 0.27 in patients with osteoporosis compared to 0.32 in those without osteoporosis.
Conclusion
Based on the current evidence from both large-scale studies and extensive reviews, it can be concluded that panoramic radiography may be a useful tool to demonstrate osteopenia in postmenopausal women at risk for osteoporosis. In a dental healthcare setting, the combined information gathered from the three assessment parameters including MCI, PMI, and trabecular pattern can be used to identify an individual with osteopenia and increased risk for osteoporosis. The reliability of these indices has been correlated with dual energy X-ray absorptiometry DEXA. Panoramic radiography is a technique sensitive imaging protocol and moreover, a type of tomography (rotational pantomography); hence, the slice layer dictates the amount of bone noted within the image. It is possible that the complexity of trabecular bone may not be captured within the image layer and could be a drawback in identifying patients with only mild loss of trabecular bone. The inferior border of the mandible showing the cortical border appears to be more accurate and consistent and can be used for evaluation of cortical bone width for the purposes of risk assessment.
There is definitive evidence from the literature that dental panoramic radiography can be used as an ancillary tool to assess the risk of post-menopausal osteoporotic women and elderly men. Since early diagnosis or detection is the key for successful initiation of therapy, all risk-assessment tools including panoramic radiographs are vital in the management of patients with loss of BMD and at risk for vertebral and hip fractures.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis, and Therapy. Osteoporosis prevention, diagnosis, and therapy. JAMA. 2001;285(6):785–95. https://doi.org/10.1001/jama.285.6.785.
Cauley JA, Chalhoub D, Kassem AM, Gel-H Fuleihan. Geographic and ethnic disparities in osteoporotic fractures. Nat Rev Endocrinol. 2014;10(6):338–51.
Wright NC, Looker AC, Saag KG, Curtis JR, Delzell ES, Randall S, Dawson-Hughes B. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res. 2014;29(11):2520–6. https://doi.org/10.1002/jbmr.2269.
Barnsley J, Buckland G, Chan PE, Ong A, Ramos AS, Baxter M, Laskou F, Dennison EM, Cooper C, Patel HP. Pathophysiology and treatment of osteoporosis: challenges for clinical practice in older people. Aging Clin Exp Res. 2021;33(4):759–73.
Föger-Samwald U, Dovjak P, Azizi-Semrad U, Kerschan-Schindl K, Pietschmann P. Osteoporosis: Pathophysiology and therapeutic options. EXCLI J. 2020;20(19):1017–37.
Akintoye SO, Lam T, Shi S, Brahim J, Collins MT, Robey PG. Skeletal site-specific characterization of orofacial and iliac crest human bone marrow stromal cells in same individuals. Bone. 2006;38(6):758–68. https://doi.org/10.1016/j.bone.2005.10.027.
Akintoye SO. The distinctive jaw and alveolar bone regeneration. Oral Dis. 2018;24(1–2):49–51.
Osyczka AM, Damek-Poprawa M, Wojtowicz A, Akintoye SO. Age and skeletal sites affect BMP-2 responsiveness of human bone marrow stromal cells. Connect Tissue Res. 2009;50(4):270–7.
Omolehinwa TT, Akintoye SO. Chemical and radiation-associated jaw lesions. Dent Clin North Am. 2016;60(1):265–77.
Akintoye S. Osteonecrosis of the jaw from bone anti-resorptives: impact of skeletal site-dependent mesenchymal stem cells. Oral Dis. 2014;20(2):221–2. https://doi.org/10.1111/odi.12181.
Sarin J, DeRossi SS, Akintoye SO. Updates on bisphosphonates and potential pathobiology of bisphosphonate-induced jaw osteonecrosis. Oral Dis. 2008;14(3):277–85.
FRAX®. Fracture risk assessment tool. Center for metabolic bone diseases, University of Sheffield, UK. Available at: https://www.sheffield.ac.uk/FRAX/. Accessed on 12 Nov 2022.
•• Yeung AWK, Mozos I. The innovative and sustainable use of dental panoramic radiographs for the detection of osteoporosis. Int J Environ Res Public Health. 2020;17(7):2449. (The work of Yeung and Mozos [2020] acknowledged the relevance of panoramic radiographic-based indices among researchers worldwide. They reiterated that although the literature from the 1970s and 1980s laid the groundwork for the investigation into the utilization of morphometric indices, more recent publications indicated that the dental panoramic radiography was a tool to identify subjects at risk of developing osteoporosis and can be used as a screening tool.)
Mupparapu M, Nadeau C. Oral and maxillofacial imaging. Dent Clin North Am. 2016;60(1):1–37.
Osterhoff G, Morgan EF, Shefelbine SJ, Karim L, McNamara LM, Augat P. Bone mechanical properties and changes with osteoporosis. Injury. 2016;47(Suppl 2):S11–20.
Lindh C, Nilsson M, Klinge B, Petersson A. Quantitative computed tomography of trabecular bone in the mandible. Dentomaxillofac Radiol. 1996;25(3):146–50.
Taguchi A, Ohtsuka M, Tsuda M, Nakamoto T, Kodama I, Inagaki K, Noguchi T, Kudo Y, Suei Y, Tanimoto K. Risk of vertebral osteoporosis in post-menopausal women with alterations of the mandible. Dentomaxillofac Radiol. 2007;36(3):143–8.
Taguchi A. Triage screening for osteoporosis in dental clinics using panoramic radiographs. Oral Dis. 2010;16(4):316–27.
Kavitha MS, Samopa F, Asano A, Taguchi A, Sanada M. Computer-aided measurement of mandibular cortical width on dental panoramic radiographs for identifying osteoporosis. J Investig Clin Dent. 2012;3(1):36–44.
• Nakamoto T, Hatsuta S, Yagi S, Verdonschot RG, Taguchi A, Kakimoto N. Computer-aided diagnosis system for osteoporosis based on quantitative evaluation of mandibular lower border porosity using panoramic radiographs. Dentomaxillofac Radiol. 2020;49(4):20190481. (The work of Nakamoto and colleagues [2020] investigated potential signs of osteopenia in panoramic radiographs via computer-aided detection specifically, mandibular lower border porosity. The mandibular cortical indices play a major role in determining the risk for osteoporosis. The authors tried to eliminate the subjectivity in assessment by utilizing computer-aided detection.)
Mohajery M, Brooks SL. Oral radiographs in the detection of early signs of osteoporosis. Oral Surg Oral Med Oral Pathol. 1992;73(1):112–7.
Kwon AY, Huh KH, Yi WJ, Lee SS, Choi SC, Heo MS. Is the panoramic mandibular index useful for bone quality evaluation? Imaging Sci Dent. 2017;47(2):87–92.
Carmo JZB, Medeiros SF. Mandibular inferior cortex erosion on dental panoramic radiograph as a sign of low bone mineral density in postmenopausal women. Rev Bras Ginecol Obstet. 2017;39(12):663–9.
Taguchi A, Suei Y, Sanada M, Ohtsuka M, Nakamoto T, Sumida H, Ohama K, Tanimoto K. Validation of dental panoramic radiography measures for identifying postmenopausal women with spinal osteoporosis. AJR Am J Roentgenol. 2004;183(6):1755–60.
• Ren J, Fan H, Yang J, Ling H. Detection of trabecular landmarks for osteoporosis prescreening in dental panoramic radiographs. Annu Int Conf IEEE Eng Med Biol Soc. 2020;2020:2194–7. (The work of Ren and colleagues [2020] investigated the use of trabecular changes noted in panoramic radiography that would determine the risk of an individual for osteoporosis.)
• Tanaka R, Tanaka T, Yeung AWK, Taguchi A, Katsumata A, Bornstein MM. Mandibular radiomorphometric indices and tooth loss as predictors for the risk of osteoporosis using panoramic radiographs. Oral Health Prev Dent. 2020;18(1):773–82. (Tanaka R and colleagues [2021] investigated the use of panoramic radiography-based radiomorphometric indices in combination with tooth loss for determination of the risk of osteoporosis. It is now known that tooth loss is also another factor in addition to signs of osteopenia in the dental panoramic radiographs alerting clinicians of the high risk for osteoporosis among these individuals.)
Franciotti R, Moharrami M, Quaranta A, Bizzoca ME, Piattelli A, Aprile G, Perrotti V. Use of fractal analysis in dental images for osteoporosis detection: a systematic review and meta-analysis. Osteoporosis Int. 2021;32(6):1041–52.
Calciolari E, Donos N, Park JC, Petrie A, Mardas N. Panoramic measures for oral bone mass in detecting osteoporosis: a systematic review and meta-analysis. J Dent Res. 2015;94(3 Suppl):17S-27S.
Klemetti E, Kolmakov S, Heiskanen P, Vainio P, Lassila V. Panoramic mandibular index and bone mineral densities in postmenopausal women. Oral Surg Oral Med Oral Pathol. 1993;75(6):774–9. https://doi.org/10.1016/0030-4220(93)90438-a.
Klemetti E, Kolmakov S, Kröger H. Pantomography in assessment of the osteoporosis risk group. Scand J Dent Res. 1994;102(1):68–72.
Benson BW, Prihoda TJ, Glass BJ. Variations in adult cortical bone mass as measured by a panoramic mandibular index. Oral Surg Oral Med Oral Pathol. 1991;71(3):349–56. https://doi.org/10.1016/0030-4220(91)90314-3.
Larheim TA, Svanaes DB. Reproducibility of rotational panoramic radiography: mandibular linear dimensions and angles. Am J Orthod Dentofacial Orthop. 1986;90(1):45–51.
Güngör K, Akarslan Z, Akdevelioglu M, Erten H, Semiz M. The precision of the panoramic mandibular index. Dentomaxillofac Radiol. 2006;35(6):442–6.
Ledgerton D, Horner K, Devlin H, Worthington H. Panoramic mandibular index as a radiomorphometric tool: an assessment of precision. Dentomaxillofac Radiol. 1997;26(2):95–100.
Hastar E, Yilmaz HH, Orhan H. Evaluation of mental index, mandibular cortical index and panoramic mandibular index on dental panoramic radiographs in the elderly. Eur J Dent. 2011;5(1):60–7.
Funding
This review was supported in part by grant R01CA259307 (awarded to S. O. A.) by the US Department of Health and Human Services/National Institutes of Health, Bethesda, MD.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Sunday O. Akintoye (author #2) is the co-section editor for the Craniofacial skeleton section of Current Osteoporosis Reports.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mupparapu, M., Akintoye, S.O. Application of Panoramic Radiography in the Detection of Osteopenia and Osteoporosis—Current State of the Art. Curr Osteoporos Rep 21, 354–359 (2023). https://doi.org/10.1007/s11914-023-00807-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-023-00807-5