Abstract
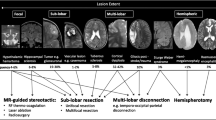
Medically refractory epilepsy is a significant cause of morbidity and mortality in pediatric neurology. Surgical intervention has been well established as a viable treatment option in certain cases. This article reviews the process of selecting appropriate patients using the latest advances in neuroimaging and electrophysiologic techniques. It also discusses the various surgical techniques currently available, including recent advances in minimally invasive approaches.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Epilepsy is one of the more common neurologic disorders in childhood. Unfortunately, a significant proportion of patients do not respond well to medications [1, 2]. Such medically refractory patients have significant morbidity from their epilepsy and/or multiple anti-epileptic medications. Ongoing seizures are known to be detrimental to the normal development of the pediatric brain [3–6]. In select cases, medically refractory patients may benefit from surgical intervention as treatment of their epilepsy. Outcome studies have proven that early intervention with surgery can significantly improve the development of children with refractory epilepsy [7–9]. Over the past 25 years, epilepsy centers have gained vast experience using surgery as treatment for epilepsy leading to well-established surgical techniques for specific patient populations. Patients with certain symptomatic epilepsies, such as focal cortical dysplasia (FCD), hemimegalencephaly (HME), and Rasmussen encephalitis, are known to be good surgical candidates (Table 1). Technological advances in neuroimaging and electrophysiology have allowed clinicians to better identify the epileptogenic zone (EZ) in a wide array of patients, even those without obvious anatomic abnormalities. More recently, less invasive surgical techniques are being used to decrease operative complications and hospital stays with good results.
Presurgical Evaluation
For surgery to be considered, a patient must be medically refractory, failing at least two appropriate anti-epileptic medications. Because pediatric patients often have very frequent seizures, as well as significant developmental disruptions, surgery is often considered earlier in the course of their epilepsy than is typical for adults [10•]. This is especially true for those patients with conditions mentioned above, e.g., FCD and HEM, and outlined in Table 1. Before a child is considered a candidate for epilepsy surgery, a comprehensive presurgical evaluation is required. The goal of this evaluation is twofold: identify the epileptogenic zone and differentiate it from eloquent/functional areas [11]. Every year, new technologies are added to the armamentarium to aide in this process (Table 2). In 2014, the ILAE commissioned a task force to provide guidelines on the evaluation process [12••]. Scalp video-EEG and structural imaging via MRI make-up the two core diagnostic tests. Non-invasive video-EEG may provide very useful data identifying the epileptogenic zone as well as confirming clinical semiology, especially in temporal lobe epilepsy [11]. In contrast to adults, however, pediatric patients may have complex ictal electrophysiology, with seemingly generalized onsets at times. It has been well documented that in cases with known early-life lesions, generalized EEG patterns do not exclude one from being a good surgical candidate [13•].
High quality structural imaging is a crucial aspect of the presurgical work-up. Advances in MRI techniques have allowed for the detection of subtle cortical malformations, which in the past had gone unnoticed [14]. This increased sensitivity is important since patients with MRI-positive lesions have a much better seizure-free rate following resective surgery. If possible, epilepsy protocol, high-resolution 3T MRI should be performed. Epilepsy protocol MRI includes axial and coronal sequences using both T1- and T2-weighted imaging [15]. Contrast-enhanced imaging should be considered for cases where tumor is in the differential. More recently, it has become commonplace to include diffusion tensor imaging (DTI), used in tractography. This technique allows better visualization of specific white matter tracts, which has become a helpful tool in both the detection of subtle cortical malformations as well as surgical planning [16–18]. In imaging-negative cases, the MRI should be re-reviewed during the surgical conference with a neuroradiologist skilled in pediatric epilepsy using the electrophysiologic data to look in close detail at areas of interest.
When EEG data and structural imaging are not conclusive, functional imaging is often used in an attempt to better define the EZ. Positron emission tomography (PET) and single photon emission computed tomography (SPECT) are the two most commonly used modalities and are felt to have relatively comparable utility [19]. FDG-PET is performed in the interictal state to assess areas of regional hypometabolism. Such areas are thought to correlate well with the epileptogenic zone. It appears to be of most use in lateralizing the EZ, particularly in very young children and infants. FDG-PET has been used in children with infantile spasms and normal MRI studies, in which the PET showed focal hypometabolism correlating to EEG onset [20, 21]. AMT-PET is being used to better define the most epileptogenic tuber in patients with tuberous sclerosis complex with good outcomes [22]. Due to technical reasons, AMT-PET is unfortunately not widely available. SPECT studies are obtained both ictally and interictally. SPECT scans are sensitive to shifts in regional perfusion of the cerebral cortex. During the interictal state, there is typically less perfusion around the EZ. In contrast, during a seizure, there is a regional increase in perfusion to the ictal cortex. By subtracting the two studies, one can locate the area with the largest difference in perfusion between the two states. The yield of the study is best with early ictal injection, occurring before the seizure has spread throughout the cortex. Subtraction ictal SPECT coregistered to MRI (SISCOM) may be used to aid in defining the EZ [23, 24]. The sensitivity of SISCOM has been reported between 60 and 80 % and appears most useful in cases with FCD [25, 26]. SISCOM has yet to become widely available, largely due to technical challenges such as isotope handling and timing of injection.
Magnetoencephalogram (MEG) and 3D EEG source localization are growing electrophysiologic tools. MEG is able to localize interictal discharges with better spatial resolution than scalp EEG [27]. It is also a more reliable localization technique when there are significant anatomic abnormalities such as skull defects or large cystic lesions [28]. Burgeoning data suggests the appearance and subsequent resection of tight dipole clusters on MEG may lead to improved surgical outcomes [29, 30].
Once the EZ is established via the above techniques, the functional zone must be delineated. Several non-invasive modalities are available, including fMRI, WADA, and TMS. In cooperative patients, fMRI can accurately identify cortical regions important for motor, sensory, language, vision, and memory functions [31, 32]. WADA is useful to lateralize language and, to a lesser extent, memory function, particularly when fMRI and other clinical data are discordant [33]. Transcranial magnetic stimulation is a new, non-invasive technique for performing non-invasive cortical stimulation. It has been used extensively for motor mapping, and now is beginning to be used for language mapping [34, 35]. In addition to the above functional tests, all patients undergoing epilepsy surgery should have a comprehensive preoperative neuropsychological or neurodevelopmental assessment [12••].
In some cases, non-invasive techniques are not sufficient to either delineate the EZ or outline the FZ. Intracranial EEG monitoring is considered the gold standard for localizing the seizure onset zone. This technique is not always feasible in the pediatric population nor is always required. When non-invasive EEG data is not concordant with the MRI lesion, non-lesional cases, or when the EZ is close to or overlapping eloquent cortex, intracranial EEG is strongly suggested [36••]. Subdural electrodes are typically placed broadly over the area of interest (Fig. 1). With deep lesions, a combination of subdural and depth electrodes may be used. The patient recovers in the ICU and seizure-monitoring unit and seizures are recorded. Invasive electrodes also allow for cortical stimulation to determine areas of cortex crucial for function. A comprehensive map can then be generated comparing the seizure onset area with the functional area, allowing the surgeon to perform a resection without causing significant deficit [37–39]. Stereotactic placement of depth electrodes (sEEG) is becoming more widely used in pediatric patients over the last 5 years. sEEG allows for better coverage of deep lesions without the need for craniotomy [40]. When there is need for broad or bilateral coverage, sEEG is an ideal method. Like subdural electrodes, depth electrodes may be used for cortical stimulation to define eloquent cortex. sEEG has been shown to be safe and effective even in patients under the age of 5 years [41, 42].
Focal Resection/Lobectomy
Focal resective surgery can be used to remove a wide variety of epileptic substrates such as cortical dysplasias, hippocampal sclerosis, cortical gliosis, atrophy/infarction, primary neoplasms, and arteriovenous malformations (AVM). The improvements in MRI imaging have allowed for a significant increase in the number of detectable focal lesions. Chern et al. found that 92.3 % of patients having surgical removal of FCDs have MRI-visible lesions prior to surgery [43]. Seizure-free rates following resection of cortical dysplasias have been around 60 %, with FCD type II more favorable than type I [38, 44, 45]. One of the primary indicators for seizure freedom seems to be extent of resection. Eighty-two percent of patients who underwent a complete resection, based on histological, MRI, or ECoG, achieved seizure freedom whereas only 24 % with incomplete resections were able to do so. The primary reason for incomplete resection was the dysplasia being in a location where there was significant risk of resection causing neurological deficits [46]. The location of resection appears to influence seizure outcomes as well, whereby 68 % of temporal resections achieve seizure freedom versus 50 % in extratemporal resections [43, 47•]. In a review of patients who underwent frontal lobe surgical resection, there was a 45 % seizure-free rate but those patients with non-lesional/idiopathic or postinfectious etiologies for frontal seizures had much worse rates of seizure freedom (21–32.7 %) [48]. There is no difference in age groups when comparing seizure freedom rate in patients under 18 years old and patients above 18 years old [47•]. When looking at other etiologies requiring focal resection, the rates of success vary. In patients with gangliogliomas or dysembryoplastic neuroepithelial tumors as a primary cause for seizures, there was an 80 % seizure freedom rate following resection. Again, there was no significant difference between adult and pediatric populations [49].
Hemispherectomy
Hemispheric disconnection has been a long used surgical tool in patients with multilobar or hemispheric epilepsy refractory to medical management. The ultimate goal of hemispherectomy is to remove or isolate an epileptogenic zone that is widely distributed in unilateral hemispheric syndromes. Hemispherectomy has been used since the 1920s to improve seizure frequency secondary to a variety of epileptic substrates. Hemispherectomy is an old surgical technique with success rates in the past ranging anywhere from 52 to 80 % [50].
Amenable lesions can be broken down into three main categories: acquired, developmental, and other. The majority of acquired lesions are due to cerebrovascular accidents. Other acquired lesions include sequelae of infections such as cysts or lesions from traumatic brain injury. The primary developmental hemispheric brain abnormalities that cause seizures are hemimegalencephaly and hemispheric cortical dysplasia, with hemimegalencephaly representing the most common epilepsy condition requiring hemispherectomy [51]. Other malformations of cortical development include polymicrogyria and schizencephaly. Finally, Rasmussen encephalitis and Sturge-Weber present with unilateral lesions and refractory epilepsy making patients with these conditions ideal candidates for hemispherectomy. In addition to epilepsy, patients with hemispheric dysfunction are at risk for significant developmental delay and neurologic hemideficits such as hemiparesis and hemianopia prior to surgery [53].
The anatomic hemispherectomy procedure was first performed in the 1920s and has been modified throughout the years to help reduce morbidity while still maintaining seizure control. Anatomic hemispherectomies have classically involved removal of the temporal, frontal, parietal, and occipital lobes, sparing the thalamus, basal ganglia, and insular cortex. The concept of the functional hemispherectomy arose in which the temporal lobe is removed, a corpus callosotomy is performed, and there is decortication of remaining tissue to disconnect the frontal and occipital lobes from the rest of the brain. There have been many modifications to the functional hemispherectomy procedure. Villemure was the first to introduce the concept of peri-insular hemispherectomy as a variant on the traditional functional hemispherectomy to reduce the amount of brain tissue removed [51]. Delalande proposed vertical parasagittal hemispherotomies, which result in complete disconnection at the level of the thalamus and avoid having to make incisions into the insula [53].
There is no clear consensus regarding which hemispherectomy technique is superior. Pinto et al. documented the largest proportion of anatomic hemispherectomies with 15 out of 36 patients who underwent hemispherectomy. Ten of those 15 (66 %) patients had hydrocephalus requiring a ventriculoperitoneal shunt (VPS) as an adverse outcome. Five other patients who had functional hemispherectomies required repeat surgery during which anatomic hemispherectomy was performed. Out of these, two patients (40 %) developed hydrocephalus requiring a VPS. The group recommended the peri-insular form as it resulted in fewer rates of reoperation and hydrocephalus [51]. Hemimegalencephaly and hemispheric cortical dysplasia were the etiologies that most frequently required anatomic hemispherectomy [50]. Dorfer et al. described 40 patients who underwent vertical hemispherotomy with very good results. Only one (2.5 %) patient required a VPS [53]. Overall, the trend has been to push for more disconnective procedures rather than anatomic hemispherectomies.
Following hemispherectomy, all patients have an improvement in seizure frequency. Seizure freedom was reported in 61–92 % [50–53]. It should be noted that the 92 % was seen in the sole study reviewed that used the Wieser rating scale as opposed to the more commonly used Engel criteria, which uses seizure rates at 1-year intervals [53]. All other studies reported a seizure freedom rate of 61–69 %. When we expand the criteria for success to Engel class 2 (rare disabling seizures), 80–87 % of patients achieve good outcomes. The greatest risk of seizure recurrence is within the first 6 months. If patients were seizure free after 6 months, the seizure freedom rate increased to 80 % [50]. A large percentage (20–80 %) of seizure-free patients is able to be weaned off AEDs. Moosa el al. had the largest cohort of patients and were able to take 67–82 % of patients off of AEDs. In patients with seizure recurrence, the majority (2/3) had epileptic activity that originated from the non-operated hemisphere [50].
Many predictors for seizure recurrence have been examined in the past including EEG findings, MRI findings, semiology, and etiology. There does not appear to be a correlation between seizure semiology or bilateral MRI findings and seizure freedom. Pinto et al. found that patients with developmental malformations such as hemimegalencephaly, and cortical dysplasia had the higher rates of seizure recurrence with rates of 37 % as compared to 21 % in patients with acquired lesions. It was thought that the difficulty in assessing anatomical landmarks in patients with developmental malformations led to difficulty with achieving complete disconnection [51]. Lee et al. presented similar findings with seizure control in 62.5 % of patients with developmental lesions versus 75 % in those with acquired lesions but none of their patients with hemimegalencephaly (n = 2) achieved seizure freedom [54]. Other studies did not find a significant relation between etiology and seizure freedom. Moosa et al. did, however, note poor outcomes in patients with abnormal EEG activity in the non-operated lobe, bilateral PET signal abnormalities, and acute postoperative seizures [50]. Ramantani et al. did not show a correlation between abnormal EEG in the normal lobe and seizure recurrence but had a smaller sample size (n = 52). Interestingly, they noted that patients who had surgery after a longer period of having seizures tended to have lower seizure recurrence rates [55]. The majority of those patients, however, had acquired lesions such as stroke.
The majority of patients who were candidates for hemispherectomy had some level of baseline hemiplegia. Moosa et al. looked at a total of 115 children over an average of 6 years follow-up to assess for changes in motor function. Following hemispherectomy, 83 % were able to walk unaided, an increase of 21 % from the preoperative cohort. Sixty-four percent had unchanged or improved hemiparesis [56]. Ramantani et al. provided similar rates with 67 % having unchanged or improved hemiparesis [55]. It does not seem like the improvement in motor function is symmetric. Hamad et al. reported an asymmetry in weakness with the upper extremities being more significantly affected than the lower extremities by surgery [57].
In regard to predictive factors, Moosa et al. noted abnormalities in the contralateral hemisphere on MRI, preexisting bilateral motor deficits, and postoperative seizures increased the risk for non-ambulation. In their cohort, 98 % of patients with a normal contralateral hemisphere were able to walk independently. Factors such as bilateral abnormal FDG PET signal, seizure semiology, or seizure etiology do not affect ambulation [56]. Bulteau et al. stated that patients with acquired lesions had better postoperative motor function but their patient cohort was focused on infants, which may explain the difference in outcomes [53].
Similar to the motor outcomes, seizure control was a very important factor in cognitive and developmental outcomes, with early postoperative seizures having the strongest negative effect on outcomes. Preexisting developmental problems were another common risk factor for postoperative developmental delays. About 10 % of patients had worsening of their development postoperatively [55].
Bilateral MRI abnormalities and preexisting language delay were risk factors for postoperative language problems. It was interesting to note that which hemisphere was removed did not seem to influence language outcomes. Patient’s reading skills seemed to follow a similar pattern as language involvement. Patients with bilateral hemisphere MRI abnormalities and preexisting reading problems were at higher risk of postoperative reading delay. In line with the preexisting reading problems, patients with a younger age at seizure onset were also at risk of reading delay, likely due to the devastating effect that seizures can have on cognitive development [56].
Corpus Callosotomy
Van Wagenen and Herren first introduced the corpus callosotomy as a treatment of refractory seizures in the 1940s [58]. Over the years, it has remained a palliative option for patients with atonic seizures in Lennox-Gastaut syndrome (LGS) or those with frequent rapidly secondarily generalized tonic-clonic seizures without a resectable lesion [59, 60]. In some rare cases, it has been helpful in lateralizing or even localizing the EZ, allowing the patients to subsequently have resective surgery. Newer surgical techniques, such as anterior callosotomy, have been developed to avoid the well-known adverse affect of disconnection syndrome [61]. Because of the possible adverse affects on learning, language, and memory, callosotomy is currently used somewhat sparingly. Long-term studies have shown superior seizure reduction in patients undergoing complete callosotomy. Drop attacks or atonic seizures appear to be best controlled with this procedure, with other seizures types to a lesser degree. In addition to a reduction in seizures, over half of patients will report an improvement in daily functioning, including reduction of hyperactivity, improved social interactions, speech, and memory [62–64].
MRI-Guided Laser Ablation
MRI-guided laser ablation is a form of stereotactic laser ablation that has recently been developed for use in epilepsy surgery, with the goal being to reduce injury to surrounding tissue compared to resective surgery. More specifically, the Visualase technique is a FDA-approved MRI-guided laser interstitial thermal therapy. It allows for real-time monitoring of the ablation as well as feedback control [65]. The system uses a 15 W, 980-nm diode laser and cooled laser applicator system with an image-processing center to provide real-time MRI guidance with thermal imaging.
The laser is inserted through a hole in the scalp and into the brain with the aid of a surgical navigation system called a stereotactic frame. MRI confirms the location prior to onset of treatment. While still in the MR scanner, the laser is turned on and the heat signature is monitored on MRI to evaluate the extent of damage produced. The procedure allows for a greater degree of precision due to improved MR visualization as well as a faster recovery time.
All studies reported success placing the probe and ablating the targeted lesion. Lesions that have been ablated include mesial temporal sclerosis, periventricular heterotopias, and hypothalamic hamartomas. Curry et al. were able to completely destroy their target lesion in 3 out of 5 patients. Complications reported include homonymous hemianopsia [66], memory impairment [65], and subdural hemorrhages and were dependent on the region of the brain ablated. Most patients were only in the hospital for 1–8 days with Wilfong et al. reporting a median and mode of only 1 day [67]. Follow-up imaging largely has shown non-enhancing cystic or pseudocystic atrophy confined to the areas of ablation. Others reported high FLAIR signal within the ablated region and no residual areas of damage outside of the target [65].
In regard to seizure resolution postoperatively, there appears to be varying degrees of success depending on the substrate being ablated. Esquenazi et al. attempted Visualase on patients with periventricular nodular heterotopias with good surgical success but poor seizure outcome. In one of their cases, it was found that seizure onset was from both the PVNH and the surrounding mesial temporal region and thus the area of ablation was too small to prevent seizure recurrence. The Visualase did provide an opportunity to attempt curative ablation prior to having to perform a larger surgical resection [66]. In patients with mesial temporal lobe epilepsy, Willie et al. reported a 77 % reduction in meaningful seizures with 54 % of patients being Engel 1 and 23 % being Engel 2 in regard to seizure control [68]. Patients with mesial temporal sclerosis had 67 % seizure-free rates after ablation. It is interesting that patients with mesial temporal epilepsy but not MTS had worse seizure control postoperatively. Some required open surgical removal of the temporal lobe and hippocampus for seizure freedom indicating a larger epileptic focus than previously thought. Surgical failures tended to occur within the first 6 months following surgery. It appears that there is no significant relationship between volume of ablation and seizure freedom. Also, it appears that there may be improved outcomes in neuropsychological testing and object recognition in non-invasive ablative procedures as compared to open procedures [69].
The greatest utility for laser ablation at this time appears to be in patients with hypothalamic hamartomas (HH). Wilfong et al. demonstrated a seizure freedom rate of 79 % in patients with HH after one round of Visualase treatment. In patients who had a second round of laser ablation therapy, the rates increased to 90 % seizure freedom. In patients who had previously undergone open removal of HH, seizure freedom rates were 50–60 %. No patients experienced postoperative diabetes insipidus, which was a common adverse event in patients who underwent open surgical removal [67].
There have only been a handful of studies reporting on MRI-guided laser ablation and the total number of subjects is still low. The initial data, however, suggests that there is good utility for MR-guided laser ablation in patients with hypothalamic hamartomas and to a lesser degree in patients with mesial temporal lobe epilepsy. In patients with mesial temporal lobe epilepsy, the seizure freedom rate was reasonable at 54 % but not up to the 60–70 % level that is normally associated with resective surgery. Visualase, does, however reduce the postoperative morbidities by being less invasive and removing less tissue.
Conclusion
For children with refractory epilepsy, surgery is a well-established treatment option and, in up to 70 % of certain populations, may even be curative [69]. Every case is approached individually with regard to presurgical diagnostic testing. In some cases, invasive monitoring should be considered when presurgical data is not definitive. The work-up and surgery should be performed at specialized epilepsy surgery centers to ensure the best outcomes. Future trends include more sensitive non-invasive diagnostic testing, minimally invasive surgery, and wider use of sEEG.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kwan P, Brodie MJ. Early identification of refractory epilepsy. N Engl J Med. 2000;342:314–9.
Camfield PR, Camfield CS. Antiepileptic drug therapy: when is epilepsy truly intractable? Epilepsia. 1996;37 Suppl 1:S60–5.
Laurent A, Arzimanoglou A. Cognitive impairment in children with nonidiopathic temporal lobe epilepsy. Epilepsia. 2006;47 Suppl 2:99–102.
Vasconcellas E, Wyllie E, Sullivan S, et al. Mental retardation in pediatric candidates for epilepsy surgery: the role of early seizure onset. Epilepsia. 2001;42:268–74.
Czochanska J, Langner-Tyszka B, Lowiowski Z, et al. Children who develop epilepsy in the first year of life: a prospective study. Dev Med Child Neurol. 1994;36:345–50.
Surges R, Saner JW. Sudden unexpected death in epilepsy: mechanisms, prevalence, and prevention. Curr Opin Neurol. 2012;25(2):201–7.
Wyllie E, Comair Y, Kotagal P, et al. Seizure outcome after epilepsy surgery in children and adolescents. Ann Neurol. 1998;44:740–8.
Mathern GW, Giza CC, Yudovin S, et al. Postoperative seizure control and antiepileptic drug use in pediatric epilepsy surgery patients: the UCLA experience 1986–1997. Epilepsia. 1999;40:1740–9.
Muhlebner A, Groppel G, Dressler A, et al. Epilepsy surgery in children and adolescents with malformations of cortical development—outcome and impact of new ILAE classification on focal cortical development. Epilepsy Res. 2014;108:1652–61.
Cross JH, Jayakar P, Nordli D, et al. Proposed criteria for referral and evaluation of children for epilepsy surgery: recommendations of the subcommision for pediatric epilepsy surgery. Epilepsia. 2006;47(6):952–9. Cross et al. provided a set of recommendations on when to refer a pediatric patient for epilepsy. Key points included emphasis upon early referral to avoid the negative developmental impact of refractory epilepsy. Certain conditions, such a TSC, FCD, and hypothalamic hamartoma were highlighted as populations where surgery should be strongly considered.
Obeid M, Wyllie E, Mikati M, et al. Approach to pediatric epilepsy surgery: state of the art, part I: general principles and presurgical workup. Eur J Pediatr Neurol. (2008) 1–13.
Jayakar P, Gaillard WD, Tripathi M, et al. Diagnostic test utilization in evaluation for resective epilepsy surgery in children. Epilepsia. 2014;55(4):507–18. Jayakar et al. reviewed the available diagnostic tests currently used during presurgical evaluations and provided recommendations on when to use each.
Wyllie E, Lachhwani DK, Gupta A, et al. Successful surgery for epilepsy due to early brain lesions despite generalized EEG findings. Neurology. 2007;69:389–97. Wyllie et al. retrospectively reviewed 50 cases with generalized EEG patterns who went on to have successful epilepsy surgery. All patients had a focal lesion on imaging and refractory epilepsy. This was the first major publication to show that generalized EEG is not a contraindication to epilepsy surgery, particularly in early-life lesions.
Goubran M, Hammond RR, de Ribaupierre S, et al. MRI and histology correlation in the neocortex of temporal lobe epilepsy. Ann Neurol. 2014 Nov Epub ahead of print.
Gaillard WD, Chiron C, Cross JH, et al. Guidelines for imaging infants and children with recent-onset epilepsy. Epilepsia. 2009;50:2147–53.
Kim H, Harrison A, Kankirawatana P, et al. Major white matter fiber changes in medically intractable neocortical epilepsy in children: a diffusion tensor imaging study. Epilepsy Res. 2013;103:211–20.
Piper RJ, Yoong MM, Kandasamy J, et al. Application of diffusion imaging and tractography of the optic radiation in anterior temporal lobe resection for epilepsy: a systematic review. Clin Neurol Neurosurg. 2014;124:59–65.
Winston GP, Micallef C, Symms MR, et al. Advanced diffusion imaging sequences could aid assessing patients with focal cortical dysplasia and epilepsy. Epilepsy Res. 2014;108:336–9.
Knowlton RC, Elgavish RA, Limdi N, et al. Functional imaging: I. Relative predictive value of intracranial electroencephalography. Ann Neurol. 2008;64:25–34.
Chugani HT, Shewmon DA, Khanna S, et al. Etiologic classification of infantile spasms in 140 cases: role of positron emission tomography. J Child Neurol. 1996;11:44–8.
Chugani HT, Asano E, Sood S. Infantile spasms: who are the ideal surgical candidates? Epilepsia. 2010;51 Suppl 1:94–6.
Chugani HT, Luat AF, Kumar A, et al. AMT-PET in 191 patients with tuberous sclerosis complex. Neurology. 2013;81:674–80.
Schneider F, Krsek P, Marusic P, et al. SISCOM and FDG-PET in patients with non-lesional extratemporal epilepsy: correlation with intracranial EEG, histology, and seizure outcome. Epileptic Disord. 2013;54:793–800.
Sulc V, Stykel S, Hanson DP, et al. Statistical SPECT processing in MRI-negative epilepsy surgery. Neurology. 2014;82:932–9.
Schneider F, Wang ZI, Alexopoulos, AV, et al. Magnetic source imaging and ictal SPECT in MRI-negative neocortical epilepsies: additional value and comparison with intracranial EEG. Epilepsia. 2013; 359–369.
Krsek P, Kudr P, Jahodova A, et al. Localizing value of ictal SPECT is comparable to MRI and EEG in children with focal conrtical dysplasia. Epilepsia. 2013;54:351–58.
Lau M, Yam D, Burneo JG. A systematic review on MEG and its use in the presurgical evaluation of localization-related epilepsy. Epilepsy Res. 2008;79:97–104.
Bennett-Back O, Ochi A, Widjaja E, et al. Magnetoencephalography helps delineate the extent of epileptogenic zone for surgical planning in children with intractable epilepsy due to porencephalic cyst/encephalomalacia. J Neurosurg Pediatr. 2014;14:271–8.
Tenney JR, Fujmara H, Horn PS, et al. Comparison of magnetic source estimation to intracranial EEG, resection area, and seizure outcome. Epilepsia. 2014;55:1854–63.
Almubarak S, Alexopoulos A, Von-Podewils F, et al. The correlation of magnetoencephalography to intracranial EEG in localizing the epileptogenic zone: a study of surgical resection outcome. Epilepsy Res. 2014;108:1581–90.
Shurtleff H, Warner M, Poliakov A, et al. Functional magnetic resonance imaging for presurgical evaluation of very young pediatric patients with epilepsy. J Neurosurg Pediatr. 2010;5:500–6.
Gaillard WD, Grandin CB, Xu B. Developmental aspects of pediatric fMRI: considerations for image acquisition and interpretation. Neuroimage. 2001;13:239–49.
Szabo CA, Wyllie E. Intracarotid amobarbitol testing for language and memory dominance in children. Epilepsy Res. 1993;15:239–46.
Picht T, Schmidt S, Brandt S, et al. Preoperative functional mapping for rolandic brain tumor surgery: comparison of navigated transcranial magnetic stimulation to direct cortical stimulation. Neurosurgery. 2011;69:581–8.
Zsoter A, Pieper T, Kudernatsch M, et al. Predicting hand function after hemispherectomy: TMS versus fMRI in hemispheric polymicrogyria. Epilepsia. 2012;53:e98–101.
Gonzalez-Martinez J, Najm IM. Indications and selection criteria for invasive monitoring in children with cortical dysplasia. Childs Nerv Syst. 2014;30:1823–29. Gonzalez-Martinez et al. outline the appropriate indications for when to use invasive electrocorticography in children. Non-lesional or multi-lesional cases, discordant MRI and EEG data, or need to map eloquent cortex were among the indications.
Bulacio JC, Jehi L, Wong C, et al. Long-term outcome after resective surgery in patients evaluated with intracranial electrodes. Epilepsia. 2012;53:1722–30.
Widdess-Walsh P, Jeha L, Nair D, et al. Subdural electrode analysis in focal cortical dysplasia: predictors of surgical outcome. Neurology. 2007;69:660–67.
Taussig D, Dorfmuller G, Fohlen M, et al. Invasive explorations in children younger than 3 years. Seizure. 2012;21:631–38.
Cossu M, Cardinale F, Castana L, et al. Stereoelectroencephalography in the presurgical evaluation of focal epilepsy: a retrospective analysis of 215 procedures. Neurosurgery. 2005;57:706–18.
Cossu M, Cardinale F, Castana L, et al. Stereo-EEG in children. Childs Nerv Syst. 2006;22:766–78.
Dorfmüller G, Ferrand-Sorbets S, Fohlen M, et al. Outcome of surgery in children with focal cortical dysplsia younger than 5 years explored by stereo-electroencephalography. Childs Nerv Syst. 2014;30:1875–83.
Chern JJ, Patel AJ, Curry DJ, et al. Surgical outcome for focal cortical dysplasia: an analysis of recent surgical series. J Neurosurg Pediatr. 2010;6:452–8.
Tassi L, Colombo N, Garbelli R, et al. Focal cortical dysplsia: neuropathological subtypes, EEG, neuroimaging and surgical outcome. Brain. 2002;125:1719–32.
Giulioni M, Marucci G, Martinoni M, et al. Seizure outcome in surgically treated drug-resistant mesial temporal lobe epilepsy based on the recent histopathological classifications. J Neurosurg. 2013;119:37–47.
Hauptman JS, Mathern GW. Surgical treatment of epilepsy associated with cortical dysplasia: 2012 update. Epilepsia. 2012;53 Suppl 4:98–104.
Rowland NC, Englot DJ, Chang EF, et al. A meta analysis of predictors of seizure freedom in the surgical management of focal cortical dysplasia. J Neurosurg. 2012;116:1035–41. Rowland et al. performed a meta-analysis of 37 different studies, including a total of 2014 patients with resection of focal cortical dysplasia. The strongest predictors of good outcome were complete resection of the MRI lesion, Palmini type II pathology, and temporal location.
Englot DJ, Wang DD, Chang EF, et al. Rates and predictors of long-term seizure freedom after frontal lobe epilepsy surgery: a systematic review and meta-analysis. J Neurosurg. 2012;11:1042.
Englot DJ, Berger MS, et al. Factors associated with seizure freedom in the surgical resection of glioneural tumors. Epilepsia. 2012;53(1):51–7.
Moosa ANV, Gupta A, Jehi L, et al. Longitudinal seizure outcome and prognostic predictors after hemispherectomy in 170 children. Neurology. 2013;80:253–60.
Pinto AL, Lohani S, Poduri A, et al. Surgery for intractable epilepsy due to unilateral brain disease: a retrospective study comparing hemispherectomy techniques. Pediatr Neurol. 2014;51:336–43.
Bulteau C, Otsuki T, Delalande O. Epilepsy surgery for hemispheric syndromes in infants: hemimegalencephaly and hemispheric cortical dysplasia. Brain and Development. 2013;35:742–7.
Dorfer C, Czech T, Feucht M, et al. Vertical perithalamic hemispherotomy: a single center experience in 40 pediatric patients with epilepsy. Epilepsia. 2013;54(11):1905–12.
Lee Y, Kim E, et al. Long term outcomes of hemispheric disconnection in pediatric patients with intractable epilepsy. J ClinNeurol. 2014;10(20):101–7.
Ramantani G, Kadish NE, Bast T, et al. Seizure control and developmental trajectories after hemispherotomy for refractory epilepsy in childhood and adolescence. Epilepsia. 2013;54(6):1046–55.
Moosa ANV, Jehi L, Gupta A, et al. Long term functional outcomes and their predictors after hemispherectomy in 115 children. Epilepsia. 2013;54(10):1771–9.
Hamad AP, Caboclo LO, Sakamoto AC, et al. Hemispheric surgery for refractory epilepsy in children and adolescents: outcome regarding seizures, motor skills and adaptive function. Seizure. 2013;22:752–6.
van Wagenen WP, Herren RY. Surgical division of commissural pathways in the corpus callosum: relation to spread of an epileptic attack. Arch Neurol Psychiatr. 1940;44:740–59.
Wong TT, Kwan SY, Chang KP, et al. Corpus callosotomy in children. Childs Nerv Syst. 2006;22:999–1011.
Maehara T, Shimizu H. Surgical outcome of corpus callosotomy in patients with drop attacks. Epilepsia. 2001;42:67–71.
Sakas DE, Phillips J. Anterior callosotomy in the management of intractable epileptic seizures: significance of the extent of the resection. Acta Neurochir. 1996;138:700–7.
Kasasbeh AS, Smyth MD, Steger-May K, et al. Outcomes after anterior or complete corpus callosotomy in children. Neurosurgery. 2014;74:17–28.
Asadi-Pooya AA, Sharan A, Nei M, et al. Corpus callosotomy. Epilepsy Behav. 2008;13:271–8.
Stigsdotter-Broman L, Olsson I, Flink R, et al. Long-term follow-up after callosotomy—a prospective, population based, observational study. Epilepsia. 2014;55:316–21.
Curry D, Gowda A, Wilfong AA. MR-guided stereotactic laser ablation of epileptogenic foci in children. Epilepsy Behav. 2012;24(4):408–12.
Esquenazi Y, Kalamangalam GP, Tandon N, et al. Stereotactic laser ablation of periventricular nodular heterotopia. Epilepsy Res. 2014;108:547–54.
Wilfong A, Curry D. Hypothalamic hamartomas: optimal approach to clinical evaluation and diagnosis. Epilepsia. 2013;54:109–14.
Willie J, Laxpati NG, Gross RE, et al. Real time magnetic resonance guided stereotactic laser amygalohippoampotomy for mesial temporal lobe epilepsy. Neurosurgery. 2014;74:569–84.
Cross JH. Epilepsy surgery in childhood. Epilepsia. 2012;43 Suppl 3:65–70.
Compliance with Ethics Guidelines
Conflict of Interest
Anuj Jayakar and Jeffrey Bolton declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Pediatric Neurology
Rights and permissions
About this article
Cite this article
Jayakar, A., Bolton, J. Pediatric Epilepsy Surgery. Curr Neurol Neurosci Rep 15, 31 (2015). https://doi.org/10.1007/s11910-015-0558-9
Published:
DOI: https://doi.org/10.1007/s11910-015-0558-9