Abstract
The perceived advantages of endovascular treatment for acute ischemic stroke in terms of recanalization, the multimodal and targeted approaches, and perhaps the more permissive rules on devices than on medications for their licensing favored the assumption that endovascular treatment is superior to intravenous thrombolysis for acute treatment of ischemic stroke, and its adoption in more advanced stroke centers. However, this assumption has been questioned by recent clinical trial experience showing that endovascular treatment is not superior to intravenous thrombolysis. The new evidence has changed the perception and the importance of conducting randomized trials in this area. This summary examines the background and outcomes of the latest experience with endovascular techniques in acute stroke treatment based on historical data. The new challenge is how to study the latest generation of devices called stent retrievers, which are faster in recanalizing and easier to use, in selected patients with acute ischemic stroke. In the meantime, the available evidence does not provide support for the use of endovascular treatment of acute ischemic stroke in clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intravenous (i.v.) recombinant tissue plasminogen activator (rt-PA) is the standard treatment for acute ischemic stroke, but more than half of the treated patients do not recover completely, or die [1]. Alternative recanalizing approaches, such as endovascular treatment (ET), have been employed for many years and have progressively gained favor thanks to the possibility of using a multimodal approach and to the evolving imaging and delivery technologies that have increased safety, speediness, and frequency of recanalization. We consider “ET” hereafter in the broad sense of all possible procedures that can be performed to recanalyze/reperfuse a symptomatic occluded cerebral artery via catheter [i.e., intra-arterial (i.a.) thrombolysis by delivery of plasminogen activators (PAs), and mechanical thrombus removal, including thrombectomy]. These may offer some advantages over the i.v. route, such as customizing the treatment strategy through angiographic planning, identifying the symptomatic occlusion(s), titering the PA dosage to effect high concentrations at the thrombus face, theoretically minimizing PA levels in the systemic circulation to achieve complete or partial recanalization, and/or facilitating recanalization by mechanical thrombus retrieval with devices that fragment/retrieve/aspirate the thrombus. Nonetheless, the results of three recently reported randomized controlled trials (RCTs) question the clinical efficacy of ET [2••, 3••, 4••], which, until now, has been considered by many interventional practitioners to be superior to i.v. rt-PA. With this review we consider possible reasons of these assumptions, summarize the actual evidence, and delineate the possible role(s) of ET for acute ischemic stroke.
A History of Local Intra-arterial PA Infusion Treatment
Initial reports of ET of ischemic stroke explored the feasibility of clearing symptomatic carotid artery territory thrombosis with i.a. plasmin, and other PAs, including urokinase (u-PA) or streptokinase (SK) [5]. A number of parallel i.v. (systemic) infusion studies recognized the feasibility of PA infusion, but lacked demonstrable thrombotic occlusion or feasibility [5]. In 1976, Fletcher and colleagues reported significant intracerebral hemorrhage and mortality in a small, single-institution series of ischemic stroke patients treated with u-PA systemically [5, 6]. That experience shed a pall over the use of PAs in the treatment of ischemic stroke, and supported a general contraindication to their use in this setting [7].
Hints of potential benefit with improved efficacy came from the treatment of vertebrobasilar territory thrombosis. Vertebrobasilar artery territory ischemia can be associated with considerable disability [8, 9]. Nenci et al. first demonstrated benefits after local i.a. treatment of symptomatic basilar artery thrombosis [10]. A contemporary retrospective comparison of the clinical outcome in 43 patients who received i.a. u-PA or SK to 22 patients who received heparin infusion suggested considerable survival benefit in those demonstrating recanalization (who had received the PA) [11].
Hence, the potential benefit of direct PA infusion at the face of symptomatic thrombi in the carotid artery territory was already being considered, which followed on the dissemination of carotid angiography and the wider availability of computed tomography (CT) scans to assess the presence of parenchymal hemorrhage as a cause of symptoms and the extent of the ischemic injury [5]. Indeed, the development of interventional techniques for endovascular recanalization has always preceded an understanding of the processes underlying evolution of ischemic injury.
Also highly relevant to the progress in the area was the move to acute intervention for rapid thrombus lysis in the cerebral arterial circuit [5], an approach initiated in three parts of the world simultaneously [5, 12••, 13••]. Ultimately, exchange of experience and personnel facilitated a more common approach in the early years [12••, 13••]. Elements essential for the early success with these methods were/are i) intervention within 3–6 hours of symptom onset; ii) use of CT imaging to exclude hemorrhage as a cause of focal ischemia; and iii) angiography to identify local arterial thrombotic occlusions thought responsible for the symptoms [12••, 13••]. Two general paths of study were undertaken: i) direct i.a. PA delivery and ii) systemic infusion delivery of the PA. The former relied upon u-PA and SK as agents. Zeumer, von Kummer, and others pursued testing of catheter-based delivery systems as the technical systems evolved (e.g., direct catheter delivery, balloon-assisted catheter projection, gold guide wire-directed) [14, 15].
The Prourokinase (Prolyse) in Acute Cerebral Thromboembolism (PROACT) study was the first and only prospective multi-center, randomized, double-blinded, placebo-controlled examination of a PA by direct i.a. infusion to be undertaken and to demonstrate benefit [16••]. In that phase II study, direct arterial infusion of recombinant single chain u-PA (rscu-PA, rpro-UK; dose 6 mg) at the thrombus face within 6 hours of symptom onset was compared with a placebo for recanalization of M1 and M2 middle cerebral artery (MCA) occlusions and safety outcomes [16••]. Overall, rscu-PA produced a significant increase in recanalization of the MCA occlusions and in hemorrhagic transformation, which were both heparin-dependent. A hint of clinical efficacy in the rscu-PA arm supported a follow-on phase III trial. Central to the phase II trial were the requirements that i) a true matched placebo for the PA be delivered directly at the thrombus face, ii) no passage of the guide wire into and through the thrombus was to take place (as this was a test of the efficacy of rscu-PA), and iii) the neurologist was to assure that the interventionalist followed the protocol exactly. The study was intended to test two doses of rscu-PA against placebo in a 2:1 randomization scheme, but was truncated by the sponsor after less than 1 year recruitment. A total of 40 patients was treated in that study. rscu-PA patients had a baseline National Institutes of Health Stroke Scale (NIHSS) of 17, while the placebo patients had an NIHSS of 19. The interventional procedures added about 1.25 hours to the overall treatment time.
PROACT II was a prospective multi-center open, un-blinded, uncontrolled, randomized multi-centre clinical outcome trial in which rscu-PA (9 mg) was delivered directly at the thrombus face or a catheter was placed in the patient distant from the occlusion (without a placebo agent) within 6 hours of symptom onset in patients with a proximal MCA occlusion [17]. Heparin was employed in both groups to maintain sheath patency. Clinical outcome was measured as disability outcome by the modified Rankin Scale (mRS) score at 3 months. Recanalization was significantly greater with intra-arterial rscu-PA (65.7%) than no intervention (18.0%), as was the frequency of symptomatic intracerebral hemorrhage. Whereas the proportion of patients with no or minimal disability (mRS = 0–1) was not significantly different between the two groups, rscu-PA was associated with a marginal improvement in outcome measured as mRS = 0–2. No further exploration of rscu-PA has ensued by the sponsor, and it is not available for clinical use. However, the marginally significant difference observed in mRS = 0–2 was taken as a demonstration of benefit of this endovascular technique. Other important considerations have been that i) there were virtually no patients treated within 3 hours of stroke onset because the use of i.v. rt-PA within the 3-hour time window was authorized by the US Food and Drug Administration (FDA) early after the study initiation, and ii) set-up and catheter delivery would have further restricted patient recruitment (which can require up to 1.0–1.25 hours). Recruitment was limited and slow in PROACT II [17]. The impact of the recruitment on outcomes, maintaining confidentiality, and outcome interpretation is not known; however, concerns regarding the variability in application of the direct infusions among patients have been raised.
In the subsequent years two other study attempts were made. MELT (Middle Cerebral Artery Embolism Local Fibrinolytic Intervention Trial), a RCT on local delivery of u-PA in documented M1 and M2 MCA ischemic stroke, was discontinued on the advice of its data monitoring committee when rt-PA was licensed in Japan in 2005 [18]. AUST (the Australian Urokinase Stroke Trial), an open label RCT of local delivery u-PA for ischemic stroke with a posterior circulation arterial occlusion, was discontinued on the basis of very slow recruitment after 24 patients of a planned sample of 200 had been included [19].
No study of any PA in this setting has been performed to demonstrate the clinical benefit of a direct PA delivery technique until recently.
A History of Mechanical Interventional Approaches
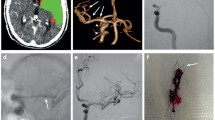
Coincident with the evolution of directed delivery of PAs, mechanical devices designed to capture and retrieve thrombi, or re-establish flow in the cerebral arterial circuit were devised. Apparent advantages of some of these devices are the rapid achievement of recanalization and application to refractory proximal thrombi, such as carotid “T” occlusions [20]. Available thombectomy devices work through aspiration (e.g., Penumbra System), entrapment and retrieval (e.g., Merci Retriever) or, as the last generation devices, through stenting and retrieval combined (e.g., Solitaire and Trevo). The latter combines the effect of radial displacement of the thrombus against the blood vessel wall with entrapment of the clot material into the stent struts that can be subsequently retrieved into a catheter placed in the internal carotid or vertebral arteries (Fig. 1). Only a few prospective clinical trials have assessed mechanical thrombectomy for acute ischemic stroke. These trials have historically been single-arm studies aiming to show the safety of recanalization for device regulatory approval purposes [20, 21, 22•, 23•]. The Merci Retriever and the Penumbra System were authorized on this basis by the FDA for use in the revascularization of patients with acute ischemic stroke secondary to intracranial large artery occlusive disease within 8 hours of symptom onset, and the Solitaire FR and Trevo Pro devices have received the CE Mark approval for patients with ischemic stroke due to large intracranial artery occlusion who are ineligible for or who fail i.v. rt-PA therapy.
Recently, the FDA has required for approval of new devices their comparison to approved predecessors. The results of two non-inferiority RCTs comparing old- and new-generation devices appeared in 2012. TREVO 2 compared the efficacy and safety of the Trevo Retriever with the Merci Retriever in 178 patients with angiographically-confirmed large cerebral artery occlusion strokes (e.g., with occlusions of the internal carotid artery, M1 and/or M2 MCA segments, or basilar and/or vertebral arteries) ineligible for or failure to respond to intravenous rt-PA, started within 8 hours of the time last assessed at baseline were eligible for the study [24•]. SWIFT compared the efficacy and safety of the Solitaire with Merci Retriever devices in 113 patients with inclusion critheria similar to those of the TREVO 2 study [23•, 24•]. Both trials demonstrated the superiority of the new-generation stent retriever devices Trevo and Solitaire over the previous generation Merci retriever in terms of reperfusion frequency and safety (86% of patients in Trevo group reached a TICI score of ≥2 or greater vs 60% with Merci retriever in TREVO 2; and, 61% in the Solitaire group obtained a TIMI 2 score or greater vs 24% in the Merci Retriever group in SWIFT) [24•, 25•].
No studies to date have demonstrated the superiority or equivalence of such devices to current acute medical treatment with intravenous rt-PA administration, and the two trials support the use of the Trevo and Solitaire Retrievers in a randomized trial of endovascular therapy against medical treatment alone.
Strategies that disrupt thrombus integrity can increase arterial perfusion. However, approaches that can provide flow through the thrombus increase the efficacy of the PA to provide thrombus lysis (“augmented fibrinolysis”). For instance, passage of the guide wire through the occluding thrombus increases the rapidity of thrombus lysis. PROACT prohibited penetration of the thrombus with guide wire or catheter [16••]. Recently, endovascular ultrasound techniques, based upon limited bench studies, and the direct application of 2 MHz diagnostic transcranial Doppler ultrasonography, developed in the clinical setting, appear to enhance thrombus lysis initiated by PAs [26, 27].
Despite the poverty of randomized studies in the last decade, the use of ET has become more widespread [20]. A major concern has been the many reports of single cases or case series that have extolled the safety of ET. Overall, those reports were in favor of ET. However, a recent meta-regression analysis of 54 studies including 5,019 patients with anterior circulation ischemic stroke treated with i.v., i.a., or combined i.v. plus i.a. thrombolysis found no evidence that one reperfusion strategy was superior to another with respect to efficacy or safety, accounting for differences in baseline covariates [28•]. The meta-analysis suggested the presence of a reporting bias in favor of the use of techniques enthusiastically received because of the substantial evidence for recanalization.
The Powerful Effect of ET
The power of the placebo effect was recognized early after the first RCTs, although the effect of the placebo was probably over-emphasized [29, 30]. An under-recognized powerful effect can be the health professionals’ perception of certain therapies. This could be the case of ET for ischemic stroke, according to the gap between low level evidence (case series instead of RCTs) and high perception of efficacy. Physicians’ perception of a therapy’s efficacy has value for the individual patient, but can be misleading when it becomes so pervasive as to be adopted in clinical practice without being subjected to verification. The possible reasons to explain the assumption of the superiority of ET are i) the high recanalization frequency obtained with the ET, that might give the impression that this method is effective in most cases, although, in fact, it may provide no clinical benefit in almost half the patients [31]; ii) the psychological impact of the complexity of the intervention on personnel, the patients, and their families; iii) the interventionalist’s experience linked with the patients they treat and not on the other patients with stroke; iv) the introduction of devices on the market without the need for properly randomized controlled studies; and v) the higher reimbursement for ET as compared to i.v. rt-PA.
A device for endovascular intervention could be marketed without the need for RCTs, but based on a series, sometimes with historical controls, showing only evidence of recanalization and of safety [21, 22•, 23•, 32–35]. As the mechanical endovascular procedures were reimbursed in this way, there was no convenience for the sponsor to risk with comparative randomized studies with i.v. rt-PA. Nonetheless, a comparison with i.v. rt-PA would have been reasonable because either the ET would be more effective as compared to i.v. rt-PA, and then it should have become available for most people, or, conversely, if not more effective, the use of the more invasive and expensive ET in place of i.v. rt-PA would have not been justified any more. This explains why the recent RCTs comparing ET to i.v. rt-PA were supported by the National Institutes of Health (IMSIII [2••] and MR RESCUE [4••]) and the Italian Medicines Agency (SYNTHESIS Expansion [3••]).
In Europe, the spread of the perception that the ET was the preferred treatment for stroke was also encouraged when interventional neuroradiology was considered a necessary component of a comprehensive stroke centre, although there may be differences in view and practice by territory [36]. The stroke units treating acute ischemic stroke patients with such an approach were considered those at a higher level, and the hub in a hub-and-spoke stroke treatment model [37]. Trials comparing devices of the first and second generation began to appear in the medical literature [24•, 25•], with the assumption that ET was better than i.v. rt-PA.
This powerful effect of the perception of ET has been a serious obstacle in organizing randomized trials in the last decade [38] and still hampers changes in clinical practice [39, 40].
New Evidence Regarding ET
The results of three RCTs of ET for acute ischemic stroke appeared on the scene at the beginning of 2013: the International Management of Stroke Study III (IMS III) [2••], SYNTHESIS Expansion [3••] and the Mechanical Retrieval and Recanalization of Stroke Clots Using Embolectomy (MR RESCUE) study [4••]. Overall, the three trials, the key features of which are summarized in Table 1, showed that ET is not superior to iv rt-PA for acute ischemic stroke.
IMS III
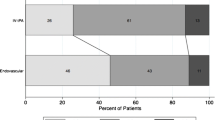
IMS III [2••] compared ET in patients treated with i.v. rt-PA within 3 hours of symptom onset with standard i.v. rt-PA. In this trial all study participants received a standard dose of i.v. rt-PA and were then randomized within 40 minutes of the initiation of the infusion. The patients assigned to the i.v. rt-PA group received the remainder of the standard dose, while those assigned to the ET group underwent angiography as soon as possible. Participants who had no angiographic evidence of a treatable occlusion received no additional treatment, while those with a treatable arterial occlusion received endovascular intervention with an approach chosen by the site neurointerventionalist (i.e., thrombectomy with the Merci retriever, Penumbra System, or Solitaire, or endovascular delivery of rt-PA by means of the Micro-Sonic SV infusion system or a standard microcatheter). This innovative scheme of bridging between iv rt-PA and ET proposed by the IMS III investigators had the advantage of initiating i.v. thrombolysis while ET was being organized, even if at the price of a sub-standard rt-PA dose to patients assigned to ET. However, the trial showed no significant difference in functional independence, as measured with the proportion of participants with a mRS = 0–2 at 3 months with endovascular therapy after i.v. rt-PA (40.8%) as compared to i.v. rt-PA alone (38.7%).
SYNTHESIS Expansion
In SYNTHESIS Expansion [3••] ET was directly compared with standard i.v. rt-PA, without pre-treatment with rt-PA.The trial hypothesis was that the disadvantage of the ET in terms of time spent, as compared with that required by i.v. rt-PA, might be offset by more rapid and effective revascularization achieved with the endovascular approaches. Another important difference with IMS III was the type of patients selected. In IMS III, patients with NIHSS scores of ≥10 were included and 92% of 306 patients who underwent baseline CT angiography had large artery occlusions while in SYNTHESIS Expansion there were no pre-specified criteria, such as an NIHSS cut-off or the demonstration of arterial occlusion with non-invasive procedures, to further select a patient already eligible for i.v. rt-PA, as the investigators aimed to produce evidence that would support the diffusion of ET to reduce the stroke burden nationwide, not in a subgroup of patients with ischemic stroke. As a consequence, the median baseline NIHSS in SYNTHESIS Expansion was 13, similarly to RCTs on i.v. rt-PA [1], while in IMS III and MR RESCUE it was 17. Moreover, the study pragmatically incorporated the use of the devices that were available on the market at the time of the study. In this trial, ET was not superior to standard treatment with i.v. rt-PA in terms of the proportion of patients with mRS = 0–1 at 3 months. To compare the results of SYNTHESIS Expansion with the other two trials, which used the mRS = 0–2 cut-off, the proportion of patients with mRS = 0–2 was 42.0% in the ET group versus 46.4% in the i.v. rt-PA group.
MR RESCUE
The main novelty of the smaller MR RESCUE study [4••], as compared with the other two trials, is that randomization was stratified according to whether the patient had a “favorable penumbral pattern” (substantial salvageable tissue and small infarct core) or a “non-penumbral pattern” (large core or small or absent penumbra) at pre-treatment multimodal CT or magnetic resonance imaging (MRI) of the brain. The theoretical basis, not yet validated, to use multimodal CT or MRI to select patients for recanalization therapies is that these examinations can identify areas of brain tissue with reduced blood flow that are at risk for infarction if flow is not restored. Large artery, anterior-circulation strokes, within 8 hours of onset, were selected to undergo mechanical embolectomy (Merci Retriever or Penumbra System) or standard care. A “favorable penumbral pattern” on neuroimaging did not identify patients who would differentially benefit from endovascular therapy for acute ischemic stroke, nor was embolectomy shown to be superior to standard care (the proportion of participants with a mRS = 0–2 at 3 months: endovascular therapy, 14% in “penumbral” group and 9% in “non-penumbral” group; standard care, 23% in “penumbral” group and 10% in “non-penumbral” group).
Of note, none of the trials raised issues of safety. The results did not deny a benefit of ET, but were neutral (i.e., the superiority of ET over i.v. rt-PA was not shown), indicating that the perception of some benefit of ET was not erroneous. The two US trials took many years to complete (8 years for MR RESCUE, and 7 years for IMS III, which stopped recruitment early because of futility). Among the reasons that could explain poor recruitment are i) reluctance in recruiting and ii) the preference for using ET outside the trial. This obstacle to the trials, and the slowdown that resulted, was a problem because technology in the field of endovascular intervention advances quickly and endovascular approaches and devices considered valid when these trials were initiated are now obsolete. Overall, the invalidated use of a treatment as ET makes it more difficult to obtain evidence of its validation compared with a standard. The question is whether there are subgroups of interest from those trials to justify further trial prosecution. This has to do with the future of ET and the generalizability of the trial results.
The Future of ET
On the basis of recent experience the main issues to be tackled, that will concern the generalizability of the results of the future trials on ET for acute ischemic stroke, should be i) time, ii) patient selection, and iii) the type of endovascular approach.
Time and bridging
To avoid treatment delay, “bridging” has been proposed with the start of i.v. thrombolysis while ET is being organized. However, bridging was not superior to i.v. rt-PA in IMS III in patients who initiated i.v. rt-PA within 3 hours of stroke onset [2••], as primary ET was not superior to i.v. rt-PA in the SYNTHESIS Expansion in patients randomized within 4.5 hours of stroke onset [3••].
Time to recanalization and reperfusion does matter in stroke
This conviction derives from the information we have on systemic thrombolysis where a correlation between outcome and time to treatment has been indicated [41], and from the natural history of clinically-defined transient ischemic attack where the longer the duration of symptoms, the higher the probability of finding an acute diffusion lesion seems [42]. However, a pooled analysis of the MERCI and Multi MERCI trials suggests that time is only one of the many variables that may affect outcome and that stroke patients presenting at later may still benefit [43]. The mean time from onset to endovascular therapy was 4 hours 9 minutes in IMS III [2••] and 3 hours 45 minutes in SYNTHESIS Expansion [3••], whilst the corresponding times for i.v. rt-PA initiation were 2 hours 2 minutes and 2 hours 45 minutes. It is possible that the time lost with the endovascular procedure hampered its clinical efficacy, although a time role in subgroup analysis in the two studies was not demonstrated. The endovascular procedures in IMS III were performed on top of i.v. rt-PA administered very early. Therefore, the hypothesis that the limited efficacy of ET is due to the delay in initiating it may not be as crucial.
SYNTHESIS Expansion [3••] was performed in unselected patients with ischemic stroke, as the ambition of this trial was to test the efficacy of ET on the stroke burden and not in a subgroup of patients. However, ET was not superior to i.v. rt-PA either in patients with large vessel occlusion in MR RESCUE [4••] and IMS III [2••]. In these trials the new generation of stent retrievers was not used (MR RESCUE) or was used in a minority of patients (IMS III) owing to their recent appearance on the market. The technology of devices advances rapidly and it is conceivable that the latest-generation devices—stent retrievers—could produce greater benefit if used widely, as suggested by the results of SWIFT and TREVO 2 trials. The target of these devices, however, cannot be every patient with acute ischemic stroke, like i.v. rt-PA, but just the subgroup of large vessel strokes. It is therefore reasonable that the on-going trials have this target (Table 2).
Other pathophysiological variables, the objects of research, could help to identify subgroups of patients that could benefit most from ET, such as clot composition [44], clot burden [45], and collateral flow [46, 47]. However, the more we restrict the number of patients suitable for ET, the fewer will be the number of patients that could benefit from this treatment. However, like in the PROACT study [16••], small well-defined patient groups may demonstrate benefit. The challenge will be how widely it could be used and the magnitude of its effect, in view of a cost–benefit analysis that will be unavoidable for courtiers with the intention to adopt it.
Conclusion
Implications for Practice
The available evidence does not show that endovascular therapy achieves superior outcomes in comparison to intravenous thrombolysis for the acute treatment of ischemic stroke patients, and does not provide support for the use of the more invasive and expensive ET over accepted use thrombolysis.
Implications for Research
The acute use of ET for ischemic stroke should be considered experimental as its role in clinical practice must be tested with RCTs. The future challenge will be testing new-generation devices in selected patients with acute ischemic stroke in the structured setting of proper RCTs that will expose its efficacy and safety. The evolving role of ET has to go through the difficult process of validation in order to demonstrate its benefit for the patients.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Wardlaw JM, Murray V, Berge E, et al. Recombinant tissue plasminogen activator for acute ischaemic stroke: an updated systematic review and meta-analysis. Lancet. 2012;379:2364–72.
•• Broderick JP, Palesch YY, Demchuk AM, et al. Endovascular therapy after intravenous rt-PA versus rt-PA alone for stroke. N Engl J Med. 2013;368:893–903. Randomized trial comparing ET in patients pre-treated with i.v. rt-PA within 3 hours of symptom onset, with standard i.v. rt-PA; endovascular approach chosen by the site neurointerventionalist (i.e., thrombectomy with the Merci retriever, Penumbra System, or Solitaire, or endovascular delivery of rt-PA by means of the Micro-Sonic SV infusion system or a standard microcatheter) in 656 patients with acute ischemic stroke (NIHSS score, ≥ 10). The trial showed similar safety outcomes and no significant difference in functional independence with ET after intravenous rt-PA compared with i.v. rt-PA alone.
•• Ciccone A, Valvassori L, Nichelatti M, et al. Endovascular treatment for acute ischemic stroke. N Engl J Med. 2013;368:904–13. Randomized trial comparing ET with standard i.v. rt-PA alone in 362 patients with acute ischemic stroke. Patients had to be eligible for i.v. rt-PA; ET approach was chosen by site neurointerventionalist and the use of any device available on the market at the time of the study was allowed. The trial showed that ET is not superior to standard treatment with i.v. rt-PA alone.
•• Kidwell CS, Jahan R, Gornbein J, et al. A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med. 2013;368:914–23. Randomized trial comparing mechanical embolectomy (Merci Retriever or Penumbra System) with standard care in 127 patients with large vessel, anterior-circulation strokes, within 8 hours of onset; randomization was stratified according to whether the patient had a favorable penumbral pattern (substantial salvageable tissue and small infarct core) or a non-penumbral pattern (large core or small or absent penumbra) at pre-treatment multimodal CT or MRI of the brain. The trial showed that a favorable penumbral pattern on neuroimaging did not identify patients who would differentially benefit from ET for acute ischemic stroke, nor was embolectomy shown to be superior to standard care.
del Zoppo GJ, Zeumer H, Harker LA. Thrombolytic therapy in acute stroke: Possibilities and hazards. Stroke. 1986;17:595–607.
Fletcher AP, Alkjaersig N, Lewis M, et al. A pilot study of urokinase therapy in cerebral infarction. Stroke. 1976;7:135–42.
Hanaway J, Torack R, Fletcher AP, et al. Intracranial bleeding associated with urokinase therapy for acute ischemic hemispheral stroke. Stroke. 1976;7:143–6.
Caplan L. "Top of the basilar" syndrome: selected clinical aspects. Neurology. 1980;30:72–9.
Archer CT, Horenstein S. Basilar artery occlusion. Clinical and radiological correlation. Stroke. 1977;8:383–7.
Nenci GG, Gresele P, Taramelli M, et al. Thrombolytic therapy for thromboembolism of vertebrobasilar artery. Angiology. 1983;34:561–71.
Hacke W, Zeumer H, Ferbert A, et al. Intra-arterial thrombolytic therapy improves outcome in patients with acute vertebrobasilar occlusive disease. Stroke. 1988;19:1216–22.
•• del Zoppo GJ, Ferbert A, Otis S, et al. Local intra-arterial fibrinolytic therapy in acute carotid territory stroke: a pilot study. Stroke. 1988;19:307–13. First evidence of the feasibility of recanalization and safety with direct infusion of PAs in thrombotic/thromboembolic stroke in the carotid artery territory within 6–8 hours of symptom onset in a two-center collaborative effort..
•• Mori E, Tabuchi M, Yoshida T, et al. Intracarotid urokinase with thromboembolic occlusion of the middle cerebral artery. Stroke. 1988;19:802–12. First evidence of the feasibility of recanalization and safety with direct infusion of a PA in thrombotic/thromboembolic stroke in the carotid artery territory within 6–12 hours of symptom onset..
Zeumer H, Freitag HJ, Grzyka U, et al. Local intra-arterial fibrinolysis in acute vertebrobasilar occlusion. Technical developments and recent results. Neuroradiology. 1989;31:336–40.
Krause KH, Jackenkroll R, Betz H, et al. Recanalization of the internal carotid artery in a case of prolonged reversible ischemic neurological deficit. Nervenarzt. 1981;52:197–201.
•• del Zoppo GJ, Higashida RT, Furlan AJ, et al. PROACT: a phase II randomized trial of recombinant pro-urokinase by direct arterial delivery in acute middle cerebral artery stroke. Stroke. 1998;29:4–11. The only closed double-blinded prospective placebo controlled trial of a PA by direct i.a. delivery at an acute thrombotic occlusion in patients presenting with ischemic stroke. The agent, recombinant single chain urokinae (pro-urokinase), produced a significant increase in early recanalization. The heparin infusion used for maintaining sheath patency contributed to both recanalization efficacy and to the appearance of hemorrhagic transformation..
Furlan A, Higashida R, Wechsler L, et al. Intra-arterial prourokinase for acute ischemic stroke. The PROACT II study: a randomized controlled trial. Prolyse in Acute Cerebral Thromboembolism. JAMA. 1999;282:2003–11.
Ogawa A, Mori E, Minematsu K, et al. Randomized trial of intra-arterial infusion of urokinase within 6 hours of middle cerebral artery stroke. The Middle Cerebral Artery Embolism Local Fibrinolygic Intervention Trial (MELT) Japan. Stroke. 2007;38:2633–9.
Macleod MR, Davis SM, Mitchell JP, et al. Results of a multicentre, randomised controlled trial of intra-arterial urokinase in the treatment of acute posterior circulation ischaemic stroke. Cerebrovascular Dis. 2005;20:12–7.
Nogueira RG, Schwamm LH, Hirsch JA. Endovascular approaches to acute stroke, Part 1: Drugs, devices, and data. Am J Neurorad. 2009;30:649–61.
Smith WS, Sung G, Starkman S, et al. Safety and efficacy of mechanical embolectomy in acute ischemic stroke: results of the MERCI trial. Stroke. 2005;36:1432–8.
• Smith WS, Sung G, Saver J, et al. Mechanical thrombectomy for acute ischemic stroke: final results of the Multi MERCI trial. Stroke. 2008;39:1205–12. Multi MERCI was an international, multicenter, prospective, single-arm trial of thrombectomy in patients with large vessel stroke treated within 8 hours of symptom onset. Patients with persistent large vessel occlusion after i.v. tissue PA treatment were included. One hundred and sixty-four patients received thrombectomy and 131 were initially treated with the L5 Retriever. Overall, favorable clinical outcomes (modified Rankin Scale 0–2) occurred in 36% and mortality was 34%; both outcomes were significantly related to vascular recanalization. Symptomatic intracerebral hemorrhage occurred in 16 patients (9.8%). Clinically significant procedural complications occurred in nine (5.5%) patients..
• Penumbra Pivotal Stroke Trial Investigators. The Penumbra Pivotal Stroke Trial: safety and effectiveness of a new generation of mechanical devices for clot removal in intracranial large vessel occlusive disease. Stroke. 2009;40:2761–8. Prospective, multicenter, single-arm study to assess the safety and effectiveness of the Penumbra System in the revascularization of patients with acute ischemic stroke presented within 8 hours of symptom onset and with an angiographic occlusion of a treatable large intracranial vessel. Patients who presented within 3 hours of symptom onset had to be ineligible or refractory to rt-PA therapy. A total of 125 target vessels in 125 patients was treated by the Penumbra System. After the procedure, 81.6% of the treated vessels were successfully revascularized to TIMI 2 to 3. There were 18 procedural events reported in 16 patients (12.8%); three patients (2.4%) had events that were considered serious. A total of 14 (11.2%) suffered from a symptomatic intracranial hemorrhage. All-cause mortality was 32.8% at 90 days with 25% of the patients achieving a modified Rankin Scale score ≤ 2. The authors concluded that the Penumbra System allows safe and effective revascularization..
• Nogueira RG, Lutsep HL, Gupta R, et al. Trevo versus Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2): a randomised trial. Lancet. 2012;380:1231–40. Randomized comparison of efficacy, in terms of recanalization rate, and safety of the Trevo Retriever with the Merci Retriever in 178 patients with angiographically-confirmed large cerebral artery occlusion strokes ineligible for or failure to respond to i.v. rt-PA. The endovascular procedure started within 8 hours of the time last assessed at baseline were eligible for the study. This trial demonstrated the superiority of Trevo over Merci Retriever..
• Saver JL, Jahan R, Levy EI, et al. Solitaire flow restoration device versus the Merci retriever in patients with acute ischaemic stroke (SWIFT): a randomised, parallel-group, non-inferiority trial. Lancet. 2012;380:1241–9. Randomized comparison of efficacy, in terms of recanalization rate, and safety of the Solitaire Retriever with the Merci Retriever in 113 patients with angiographically-confirmed large cerebral artery occlusion strokes ineligible for or failure to respond to i.v. rt-PA. The endovascular procedure started within 8 hours of the time last assessed at baseline were eligible for the study. The trial demonstrated the superiority of Solitaire over the Merci retriever..
Mikulik R, Dusek L, Hill MD, et al. Pattern of response of National Institutes of Health Stroke Scale components to early recanalization in the CLOTBUST trial. Stroke. 2010;41:466–70.
Balucani C, Alexandrov AV. Ultrasound- and microspheres-enhanced thrombolysis for stroke treatment: state of the art. Curr Cardiol Rep. 2010;12:34–41.
• Mullen MT, Pisapia JM, Tilwa S, et al. Systematic review of outcome after ischemic stroke due to anterior circulation occlusion treated with intravenous, intra-arterial, or combined intravenous+intra-arterial thrombolysis. Stroke. 2012;43:2350–5. The authors performed a literature review and meta-analysis comparing the relative efficacy of six reperfusion strategies: i) 0.9 mg/kg i.v. tissue-type PA; ii) i.a. chemical thrombolysis; iii) i.a. mechanical thrombolysis; iv) i.a. combined chemical/mechanical thrombolysis; v) 0.6 mg/kg i.v. tissue-type PA and i.a. thrombolysis; and vi) 0.9 mg/kg i.v. tissue-type PA and i.a. thrombolysis. This study found no evidence that one reperfusion strategy is superior with respect to efficacy or safety, supporting clinical equipoise between reperfusion strategies..
Kaptchuk TJ. Powerful placebo: the dark side of the randomised controlled trial. Lancet. 1998;351:1722–5.
Bailar 3rd JC. The powerful placebo and the Wizard of Oz. N Engl J Med. 2001;344:1630–2.
Hussein HM, Georgiadis AL, Vazquez G, et al. Occurrence and predictors of futile recanalization following endovascular treatment among patients with acute ischemic stroke: a multicenter study. AJNR Am J Neuroradiol. 2010;31:454–8.
Sorimachi T, Fujii Y, Tsuchiya N, et al. Recanalization by mechanical embolus disruption during intra-arterial thrombolysis in the carotid territory. AJNR Am J Neuroradiol. 2004;25:1391–402.
Ringer AJ, Qureshi AI, Fessler RD, et al. Angioplasty of intracranial occlusion resistant to thrombolysis in acute ischemic stroke. Neurosurgery. 2001;48:1282–8.
Qureshi AI, Siddiqui AM, Suri MF, et al. Aggressive mechanical clot disruption and low-dose intra-arterial third-generation thrombolytic agent for ischemic stroke: a prospective study. Neurosurgery. 2002;51:1319–27.
Bergui M, Stura G, Daniele D, et al. Mechanical thrombolysis in ischemic stroke attributable to basilar artery occlusion as first-line treatment. Stroke. 2006;37:145–50.
Leys D, Ringelstein EB, Kaste M, Hacke W. The main components of stroke unit care: Results of a European expert survey. Cerebrovasc Dis. 2007;23:344–52.
Consoli D, de Falco FA, Lenzi GL, Miceli G, Palombo F, Rosati G, Simonetti G, Stanzione P, Ugenti R, Zangrillo A. Cap 4. Le Stroke Unit: definizioni, criteri di accreditamento, indicatori e verifiche di qualità. Pp 13–19. In: Organizzazione dell’assistenza all’ictus: le Stroke Unit. Ministero della Salute Editor. Quaderni del Ministero della Salute, n.2, marzo-aprile 2010. Available at: http://www.quadernidellasalute.it/archivio-quaderni/2-marzo-aprile-2010.php. Accessed 20 Oct 2013.
Ciccone A, Valvassori L, Gasparotti R, et al. Debunking 7 myths that hamper the realization of randomized controlled trials on intra-arterial thrombolysis for acute ischemic stroke. Stroke. 2007;38:2191–5.
Johnston SC, Hauser SL. The dangers of clinical conviction: an “M&M” of endovascular therapies for stroke. Ann Neurol. 2013;73:A5–6.
Goyal M, Swartz RH. Epistemology, parachutes, and "yeah, but" interventional stroke trials. Stroke. 2013;44:2036–8.
Hacke W, Donnan G, Fieschi C, et al. Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet. 2004;363:768–74.
Easton JD, Saver JL, Albers GW, et al. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke. 2009;40:2276–93.
Nogueira RG, Smith WS, Sung G, et al. Effect of time to reperfusion on clinical outcome of anterior circulation strokes treated with thrombectomy: pooled analysis of the MERCI and Multi MERCI trials. Stroke. 2011;42:3144–9.
Liebeskind DS, Sanossian N, Yong WH, et al. CT and MRI early vessel signs reflect clot composition in acute stroke. Stroke. 2011;42:1237–43.
Legrand L, Naggara O, Turc G, et al. Clot burden score on admission T2*-MRI predicts recanalization in acute stroke. Stroke. 2013;44:1878–84.
Bang OY, Saver JL, Kim SJ, et al. Collateral flow predicts response to endovascular therapy for acute ischemic stroke. Stroke. 2011;42:693–9.
McVerry F, Liebeskind DS, Muir KW. Systematic review of methods for assessing leptomeningeal collateral flow. AJNR Am J Neuroradiol. 2012;33:576–82.
Compliance with Ethics Guidelines
Conflict of Interest
Alfonso Ciccone serves on the Clinical Events Committee of the TREVO (Thrombectomy REvascularization of large Vessel Occlusion in acute ischemic stroke) study for Concentric Medical Inc. Preparation of didactic material for the Stroke Day organized by the Italian Stroke Forum for Pierrel Research Italy SPA.
Gregory J. del Zoppo declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Stroke
Rights and permissions
About this article
Cite this article
Ciccone, A., del Zoppo, G.J. Evolving Role of Endovascular Treatment of Acute Ischemic Stroke. Curr Neurol Neurosci Rep 14, 416 (2014). https://doi.org/10.1007/s11910-013-0416-6
Published:
DOI: https://doi.org/10.1007/s11910-013-0416-6