Abstract
Purpose of Review
In the last 50 years, vancomycin has been the agent of choice to treat infections due to methicillin-resistant Staphylococcus aureus (MRSA). However, vancomycin treatment failure is not uncommon, even when MRSA strains are fully susceptible to vancomycin. Treatment with vancomycin requires careful monitoring of drug levels as there is a potential for nephrotoxicity. Resistance to clindamycin is not infrequent, which also limits therapeutic options for treating infections due to MRSA in children. This paper reviews the current data on pharmacokinetics and pharmacodynamics and clinical efficacy of vancomycin in children.
Recent Findings
Resistance to vancomycin in MRSA (MIC >2 mg/L) is infrequent; there is increasing evidence in the literature that vancomycin maybe ineffective against increasing proportion of isolates with MICs between 1 and 2 mg/L. Recent studies and meta-analyses have demonstrated that strains with high vancomycin MICs are associated with poor outcomes especially in patients with bacteremia and deep tissue infections due to MRSA. This gradual increase in vancomycin MIC has been reported as MIC creep or vancomycin heteroresistance. Patients infected with MRSA isolates that exhibit MIC creep experience poorer clinical outcomes, including delayed treatment response, increased mortality, increase rate of relapse, and extended hospitalization. There are limited data to guide vancomycin dosing in children with MRSA. Although the vancomycin area under the curve AUC24/MIC ratio > 400 has been shown to predict clinical efficacy in adults, this relationship has not been documented very well for treatment outcomes in MRSA infections in children. Use of higher vancomycin dosages in attempts to achieve higher trough concentrations has been associated with increased nephrotoxicity.
Summary
New recently approved antibiotics including ceftaroline, dalbavancin, and tedizolid offer a number of advantages over vancomycin to treat staphylococcal infections: improved antimicrobial activity, superior pharmacokinetics, pharmacodynamics, tolerability, and dosing, including once-daily and weekly regimens, and less need for monitoring drug levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Staphylococcus aureus was first identified as a bacterial pathogen in the nineteenth century. Penicillin was considered the drug of choice until S. aureus developed penicillin resistance by production of beta-lactamase. This led to discovery of semisynthetic penicillins such as dicloxacillin and nafcillin, but quickly methicillin-resistant S. aureus (MRSA) emerged due to the acquisition of genes that have decreased affinity for beta-lactams, including antistaphylococcal penicillins, cephalosporins, and carbapenems [1]. In the last 50 years, vancomycin has been the agent of choice to treat MRSA infections, although other agents such as clindamycin, tetracyclines, and co-trimoxazole have also been utilized. However, vancomycin treatment failure is not uncommon, even when MRSA strains are fully susceptible to vancomycin (MIC ≤ 2 mg/mL) [2]. Treatment with vancomycin requires careful monitoring of drug levels as there is a potential for nephrotoxicity. In addition, resistance to clindamycin is not infrequent, which also limits therapeutic options for treating infections due to MRSA in children.
In the last few years, tedizolid, daptomycin, telavancin, dalbavancin, and ceftaroline have been approved for treatment for staphylococcal infections in adults, including MRSA. Ceftaroline and daptomycin have been approved by the Food and Drug Administration (FDA) for use in children. Ceftaroline, daptomycin, dalbavancin, telavancin, and tedizolid offer a number of advantages over currently available drugs to treat staphylococcal and other Gram-positive infections, especially vancomycin: improved antimicrobial activity, superior pharmacokinetics, pharmacodynamics, tolerability, and dosing, including once-daily and weekly regimens, and less need for monitoring drug levels. However, vancomycin remains the mainstay for treatment of infections due to MRSA in children, despite issues with what appears to be decreasing susceptibility and toxicity. In this paper we will review current data on pharmacokinetics and pharmacodynamics and clinical efficacy of vancomycin in children.
Staphylococcus aureus and Resistance to β-Lactam Agents
β-lactams have been the drug of choice for treating infections caused by S. aureus. However, due to the development of resistance, their usefulness has been compromised. β-Lactamase production was noted soon after penicillin was introduced, which led to the development of isoxazoyl penicillin (e.g., oxacillin) and the β-lactamase-insensitive penicillin derivative methicillin. Following the development of oxacillin and other antistaphylococcal penicillins, methicillin-resistant S. aureus emerged that encoded a penicillin-binding protein (PBP) that could not be inactivated by β-lactam antibiotics. Hospital MRSA strains are type I, II, or III staphylococcal cassette chromosome mec (SCCmec) cassettes and express high levels of resistance to oxacillin and cause invasive infection mainly in the hospital setting leading to high morbidity and mortality [3]. In the last decade, a type IV SCCmec cassette has originated in the community, known as community-associated MRSA (CA-MRSA), which contains genes encoding the Panton–Valentine leukocidin (PVL) and clone (USA300) is widespread in the North America and among other developed nations, while CA-MRSA type V SCCmec cassette has emerged in Asia. USA300 and related PVL-containing clones, such as USA400, USA500, USA1000, and USA1110, are capable of causing a variety of very serious infections, including necrotizing fasciitis, pyomyositis, septic thrombophlebitis of the extremities, the “pelvic syndrome” (septic arthritis of the hips, pelvic osteomyelitis, pelvic abscesses), and septic thrombophlebitis in children, Waterhouse–Friderichsen syndrome, rapidly progressive pneumonia, and ocular infections. However, CA-MRSA mainly cause purulent and/or pustular skin and soft tissue infections in healthy individuals [2, 4]. CA-MRSA express a low-level resistance to oxacillin and are usually resistant to all β-lactams, including cephalosporins. Treatment of CA-MRSA usually includes the use of agents like clindamycin, tetracyclines, and trimethoprim–sulfamethoxazole (TMP–SMX) which are utilized in patients treated on an outpatient basis. Severe infections with CA-MRSA that require hospitalization, intravenous antibiotics like vancomycin, linezolid and daptomycin are usually utilized for treatment. [4]. Although clindamycin can be used for CA-MRSA, resistance has been increasing in patients treated with it [5, 6]. Thus, patients treated with clindamycin must be monitored more closely for the development of self-induced resistance.
Staphylococcus aureus and Vancomycin
In the mid-1950s, vancomycin was first utilized for the treatment of Gram-positive infections in adults and in children but with the advent of extended spectrum PCNs and cephalosporins, vancomycin was not used widely until 1980s for the treatment for MRSA strains [3]. In the 2000s, vancomycin has come to the forefront of concern. Recent publications have documented decreased susceptibility to vancomycin in MRSA [7, 8], decreased efficacy [9, 10], and increased toxicity with higher doses and in combination therapy with piperacillin–tazobactam [11,12,13,14,15,16,17].
Vancomycin, a glycopeptide, inhibits cell wall synthesis by binding to the d-alanyl-d-alanine moieties and prevents cross-linking of the peptidoglycan layer. It is administered intravenously and has poor gastrointestinal absorption. Over 90% of the drug is removed by renal excretion, and in patients with reduced creatinine clearance, there is marked accumulation of vancomycin. It is imperative to conduct therapeutic drug monitoring of vancomycin for efficacy and toxicity. Common adverse reaction to vancomycin is “red-man syndrome,” which is mainly infusion related, and nephrotoxicity. Ototoxicity and thrombocytopenia are seen rarely.
Staphylococcus aureus and Reduced Susceptibility to Vancomycin
Resistance to vancomycin in MRSA (MIC of > 2 mg/L) is infrequent, but there is increasing evidence in the literature that vancomycin maybe ineffective against increasing proportion of isolates with MICs between 1 and 2 mg/L. Recently, several studies and meta-analyses have demonstrated that strains with high vancomycin MICs are associated with poor outcomes especially in patients with bacteremia and deep tissue infections (osteomyelitis, necrotizing pneumonia) due to MRSA [9, 18, 19]. This gradual increase in the value of vancomycin MIC for S. aureus has been reported as MIC creep or vancomycin heteroresistance (subpopulations of resistant S. aureus within a larger population of vancomycin susceptible bacteria), and patients infected with MRSA isolates that exhibit MIC creep might experience poorer clinical outcomes, including delayed treatment response, increased mortality, increase rate of relapse, extended hospitalization, or overall increased cost of hospitalization. Soriano et al. [20] showed that mortality associated with MRSA bacteremia was significantly higher when the empirical antibiotic was inappropriate and when vancomycin was empirically used for the treatment of infection with strains with high vancomycin MIC (> 1 mg/L). This phenomenon of MIC creep and vancomycin therapy failure with S. aureus infections with a MIC ≥ 4 mg/L led the Clinical and Laboratory Standards Institute (CLSI) in 2016 to reduce vancomycin breakpoints for susceptible S. aureus from ≤ 4 to ≤ 2 mg/L, and from ≥ 32 to ≥ 16 mg/L for resistant S. aureus [21]. These changes aimed to increase the sensitivity of the detection of non-susceptible isolates. It has been debated that the MIC creep phenomenon may not be real as it has been reported inconsistently and it maybe be influenced by the type of microbiological susceptibility test used (Etest, broth microdilution (BMD), or automated systems) or type of S. aureus strain or storage of the isolates or type of patient population evaluated. The reference standard for measuring MIC remains BMD. Studies have documented vancomycin MIC creep with using BMD and Etest methods, and other studies have documented no vancomycin MIC creep when using the same methods [22,23,24,25]. Furthermore, results from primary studies and meta-analysis have been inconsistent; some have shown higher rates of mortality and treatment failure, whereas others have indicated no association between high vancomycin MICs and mortality. A recent meta-analysis that included 55 studies and mean values of vancomycin MICs, of 29,340 S. aureus isolates documented no evidence of MIC creep [26]. Goldman and colleagues evaluated vancomycin MIC creep or heteroresistance in 208 pediatric S. aureus blood isolates by three methods (BMD, Etest, Vitek2). They reported that vancomycin MICs did not increase nor was heteroresistance identified. Vancomycin MIC results did vary across testing methods, with the standard Etest resulting in a higher value 94% of the time when compared with BMD. No MIC was > 2 mg/L by any testing method [27]. This can be problematic as a falsely elevated vancomycin MIC may lead the clinician to utilize another agent besides vancomycin. It is important for clinicians to be aware of the testing method utilized for susceptibility testing and consider MIC results based on the method utilized and not deter the utilization of vancomycin. This suggest that vancomycin continues to be the standard option in treatment of MRSA infections when MIC is determined with Etest or BMD methods. Current guidelines from the Infectious Diseases Society of America (IDSA) for the treatment of MRSA infections recommend that for isolates susceptible to vancomycin (MIC, 2 mg/L), “the patient’s clinical response should determine the continued use of vancomycin, independent of the MIC” [28]. Despite these recommendations, the literature describing the association between high vancomycin MICs and worsened outcomes may likely influence changes in clinical practice for some practitioners solely on the basis of vancomycin MIC results, independently of the patient’s clinical status. Perhaps, based on these conflicting results and inconsistency, CLSI categorical breakpoint interpretations (S, I, R) should be reported and MIC values should be suppressed in order to prevent misinterpretation and bias from MIC values.
Vancomycin Pharmacokinetics/Dynamics in Children, Dosing, and Toxicity
Vancomycin is a time-dependent antibiotic and is administered intravenously. It is 25 to 50% protein bound, mainly to albumin, and is almost exclusively eliminated by the renal route. The pharmacokinetics of vancomycin has shown large inter-individual variability, primarily linked to a patient’s age, clinical condition, and disease. To reduce nephrotoxicity and optimize efficacy, serum trough concentrations are monitored. Due to the lack of data for vancomycin dosing and monitoring in pediatric patients, guidelines developed for adults are utilized as a reference. Historically, vancomycin in pediatric patients has been dosed at 40 mg/kg/day for empiric treatment. Previously, serum trough concentrations were targeted to 5–10 mg/L in most situations or 10–15 mg/L for treatment of central nervous system infections [29]. Because of an increase in MRSA infections in pediatric patients, increased inhibitory MIC, antibiotic penetration issues, and unique metabolic differences between children and adults, it has been shown that higher doses of vancomycin may be required in some pediatric patients. The maximum recommended dose for adult or pediatric patients is 100 mg/kg/day or 6 g/day [30]. To minimize the development of resistant strains, improve tissue penetration, and optimize vancomycin pharmacodynamics, the 2011 IDSA guidelines suggested targeting these higher trough concentrations and its effectiveness is more correlated with area under the curve (AUC) to MIC ratio (AUC:MIC). The guideline suggests that trough concentrations of 15–20 mg/L should achieve an area under the curve/24 h/MIC (AUC24/MIC) > 400 in adults if the vancomycin MIC is ≤ 1 mg/L [28]. Additionally, the guidelines state that there are limited data to guide vancomycin dosing in children with MRSA. Although the vancomycin area under the curve AUC24/MIC ratio > 400 has been shown to predict clinical efficacy in adults, this relationship has not been documented very well between vancomycin AUC24/MIC and treatment outcomes in MRSA infections in children. Most of the pediatric studies conducted to date have evaluated dosing that would achieve similar AUC:MIC goals. No pediatric outcome data have supported specific AUC:MIC concentrations; a recent study demonstrates a correlation between troughs in pediatric patients and outcomes [31]. In a multicenter retrospective study, the optimal vancomycin trough concentration was determined that would impact the duration of methicillin-resistant Staphylococcus aureus bacteremia in children. It was reported that a median vancomycin trough concentration of < 10 mg/L within the first 72 h may be associated with a longer duration of bacteremia compared with a median trough concentration of ≥ 10 mg/L [31]. It remains unclear if vancomycin trough concentrations of ≥ 15 mg/L are needed in children with MRSA bacteremia. This question is important because children have enhanced renal elimination, which makes it challenging for them to obtain a trough concentration of ≥ 15 mg/L and attempts to reach this goal often require higher doses and an increased frequency of administration. Pediatric patients often clear vancomycin much faster than adults. Analysis of vancomycin clearance has demonstrated a median clearance of 0.12–0.04 L/kg/h in patients 2.2–13.4 years of age, 2.5 times higher than the reported average renal clearance in adults of 0.048 L/kg/h [32]. Due to increased clearance in pediatric patients, much higher and more frequent mg/kg dosing is needed to achieve similar trough concentrations as adults. Pharmacodynamic data suggests that higher dosages (60 mg/kg/day) are required to achieve AUC24/MIC > 400 for isolates with a vancomycin MIC < 1 g/mL, and guidelines suggest considering targeting trough concentrations of 15–20 μg/mL in children with serious infections [33]. Following adoption of the new target trough levels for vancomycin, typical pediatric starting doses of 40–60 mg/kg daily (usually divided for administration q6-8h) have remained the same at many institutions. Several studies have shown that such doses are frequently insufficient to achieve the new target trough levels, and recent studies have shown that significantly higher doses than those in current use are required to achieve these higher trough levels; however, more data are needed to support starting doses above 60 mg/kg daily in pediatrics [32, 34,35,36,37,38]. Several studies have shown low rates of achieving therapeutic vancomycin trough levels in pediatric patients with current starting doses [34,35,36,37,38]. The delay in achieving the target trough level not only impedes early treatment of the infection but also promotes the development of resistant strains. A recent pharmacokinetic evaluation modeled a dose of 15 mg/kg every 6 h (q6h) and showed that estimated troughs of 7–10 mg/L were predicted to correlate to achieving an AUC:MIC goal of more than 400 mg h/L for more than 90%, and 1–17%, at MICs of 1 and 2 mg/L, respectively [39]. Similarly, another published model on pediatric patients 3 months and older showed troughs of 8–9 mg/L corresponded to AUC:MIC goals, but even with doses of 60–70 mg/kg/day, trough goals were only obtained in 45% of children [32]. Hwang et al. studied vancomycin dosing and target attainment in 218 Taiwanese children. The mean age was 6.0 ± 5.1 years, and the mean body weight was 20 ± 11.7 kg. Vancomycin trough concentrations were moderately correlated with AUC values (p < 0.01). Dosing of 15 mg/kg/dose q6h produced significantly higher AUC values (p < 0.001) and vancomycin trough concentrations (p < 0.001) compared with dosing of 10 mg/kg/dose q6h. In children receiving a 10-mg/kg/dose q6h, 5.6% (5/90) achieved the target trough concentrations of 15–20 mg/mL and 9.5% (5/90) achieved the goal AUC/MIC ≥ 400. In children receiving a 15-mg/kg/dose q6h, 13% (6/46) achieved the target trough concentrations of 15–20 mg/mL, whereas 54.3% (25/46) achieved the goal AUC/MIC ≥ 400 [40]. Chhim and colleagues evaluated vancomycin dosing practices for suspected invasive staphylococcal infections and found that 40 mg/kg per day did not result in therapeutic trough concentrations or predicted AUC24 > 400 in the majority of patients. Even 60 mg/kg per day did not routinely achieve these target ranges in children [41]. Additionally, a meta-analysis of 20 studies revealed that doses lower than 60 mg/kg/day were not enough to achieve desirable vancomycin plasma concentrations “area under the curve in 24 h/minimum inhibitory concentration >400 (AUC0-24/MIC>400) or trough 10-20 mg/L” to control bacterial infections in pediatrics [42••]. Further, some data suggest that young patients between 1 and 6 years of age are more likely to require 80–85 mg/kg/day divided q6h to achieve troughs of 15–20 mg/L [38].
Eighty to 90% of vancomycin is cleared through the kidneys; the half-life of the drug in a patient’s body depends heavily on renal function. Given age-related differences in renal function and vancomycin clearance, it seems that vancomycin dosing strategies should be adjusted according to age in pediatric patients and a few have suggested alternative starting doses for example starting dose of 60 mg/kg daily for patients 1 to 5 months of age and those 13 to 18 years of age and a starting dose of 70 mg/kg daily for patients 6 months to 12 years of age [2]. Although targeting troughs of 15 to 20 mg/L may provide a simplistic means of assurance of pharmacodynamic target attainment in complicated infections, concern has arisen that it may also unnecessarily increase nephrotoxicity risk in some patients. The results of a study showed that although adult patients with trough levels > 10 mg/L were more likely to achieve the pharmacodynamic AUC24:MIC target than those with trough levels < 10 mg/L, pushing trough levels > 15 mg/L was not associated with a statistically significant increase in AUC24:MIC target attainment. Additionally, the study results showed that the mean trough in those patients who developed vancomycin-induced nephrotoxicity (VIN) was 19.5 mg/L versus 14.5 mg/L in those who did not develop VIN [43]. Thus, targeting a higher trough goal increased the risk for the development of VIN but did not increase the proportion of patients achieving the pharmacodynamic target. Kishk et al. [44] looked at vancomycin AUC/MIC and corresponding troughs in pediatrics. Their retrospective study concluded that the probability of achieving an AUC/MIC > 400 using only a trough serum concentration and an MIC with patients receiving 15 mg/kg every 6 h is variable based on the method used to calculate the AUC. An AUC/MIC of 400 in children may be correlated to a trough concentration of 11 mg/L using a trapezoidal method to calculate AUC [44]. Recently, a meta-analysis published by Fiorito and colleagues reported that the rate of VIN is increased in pediatric patients with higher vancomycin troughs along with contributing factors such as intensive care unit admission, hypovolemia, and concurrent use of nephrotoxic agents [45••].
Overall, it is hard to draw any specific conclusions on predictors of vancomycin-associated nephrotoxicity in pediatric patients as majority of the studies have much variability in inclusion and exclusion criteria and make interpretation a challenge. Pharmacodynamic studies to assess area under the curve to minimum inhibitory concentration (AUC/MIC) ratios in pediatrics may help clarify monitoring recommendations and requirements. It is suggested that Bayesian pharmacokinetic dosing approach based on a single vancomycin level to determine vancomycin exposure may provide a clearer indication of vancomycin efficacy and toxicity and the risk of nephrotoxicity may be increased by additional risk factors besides vancomycin trough levels [46]. Bayesian method is limited by that it utilizes a software which can be expensive, a trapezoidal model, requires manual calculation by obtaining 2 steady-state levels, with 1 level drawn following administration/distribution and another just prior to the next scheduled dose. These levels are used to calculate a patient’s pharmacokinetic parameters and various formulas to calculate the AUC for a single dose. To calculate the AUC24, the single-dose AUCs are then multiplied by the daily doses administered. Limitations of the trapezoidal models are its inability to account for acute physiologic changes, underestimating true AUC values, and its requirement of at least 2 vancomycin levels [47].
Clinical Effectiveness of Vancomycin for Treatment of Invasive MRSA Infections in Children
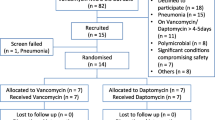
Recent studies have suggested that vancomycin may not be as effective as alternate therapies for treatment of MRSA coinfection in children with influenza-related respiratory infection and osteoarticular infections due to MSSA and MRSA. Coinfection with influenza virus and MRSA can cause life-threatening pneumonia in children. The Pediatric Intensive Care Influenza (PICFLU) Study enrolled children < 18 years of age with confirmed influenza and respiratory failure on ventilatory support admitted to 34 participating PICUs in the USA from December 2008 through May 2016 [48••]. Viral testing was performed using RT-PCR. The diagnosis of bacterial infection by culture was done at each clinical site within 72 h of admission. Specimens obtained included blood, endotracheal, bronchoalveolar lavage (BAL), and pleural fluid. One hundred seventy children with documented influenza infection were enrolled; 30 (17.6%) were diagnosed with MRSA co-infection. Other bacteria were identified in 61 (25.9%) children including 31 with MSSA, and 10 with S. pneumoniae. Majority of the children with MRSA co-infection had acute lung injury or vasopressor use compared with 50%, of children with other bacterial co-infections, p ≤ 0.001 and > 70% of patients with MRSA co-infection received ECMO compared with < 9% of children in the other bacterial co-infections (p ≤ 0.001). Most striking was the mortality rate among the children with MRSA co-infection (40% v. 4.3% RR 9.3; 95% CI, 3.8–22.9). When the outcomes were analyzed relative to which antibiotics were used, those children who received early vancomycin alone had a mortality rate of 69.2% compared with 12.5% of children who received vancomycin and another anti-MRSA antibiotic (RR 5.5; 95% CI, 1.2. 21.3; p = 0.003). Early vancomycin was given to 96.7% of the children, of which 51.7% received additional anti-MRSA antibiotics. Other anti-MRSA antibiotics used were clindamycin, ceftaroline, and linezolid. There was difficulty in reaching therapeutic vancomycin levels; dosing did not influence initial trough levels; 78% were < 10 μg/mL. All the MRSA isolates that were tested were susceptible to clindamycin. However, one child who was treated early with clindamycin alone died, even though the isolate was susceptible. All the tested MRSA isolates (28/30) were susceptible to vancomycin; however, 13.3% had MICs of 1–2 μg/mL; the number of isolates with MICs of 2 μg/mL and relationship to patient outcome were not given.
The reasons for vancomycin failure were not clear. Vancomycin poorly penetrates lung tissue. An extensive literature review conducted by Stein and Wells [49] in 2010 found that vancomycin concentrations in the epithelial lining fluid (ELF) ranged from 5 to 25% of levels in plasma obtained at the same time. In contrast, overall mean concentrations of linezolid in the ELF were general similar or higher than those in plasma. These data suggest that higher doses of vancomycin may need to be used in treating MRSA pneumonia. Other factors may also be responsible for the poor response to vancomycin in these patients. Clindamycin and linezolid, in addition to superior tissue penetration, inhibit bacterial protein synthesis and thus may reduce production of endotoxin. Similar data were recently reported in adults with methicillin-resistant S. aureus bacteremia by Geriak et al. [50]. These patients were in a clinical trial comparing monotherapy with vancomycin or daptomycin to a combination of daptomycin and ceftaroline. The study was terminated early as the results of a preliminary data analysis revealed the mortality in the monotherapy group to be 26% compared with 0% in the combination therapy group. Mortality in the monotherapy group was associated with IL-10 concentrations > 5 pg/mL.
Choice of second anti-MRSA agent depends on local susceptibility patterns. Clindamycin, if susceptible, is a logical choice; however, S. aureus and MRSA resistance to clindamycin currently ranges from 10 to 20% [51•]. Clindamycin susceptibility declined from 90 to 83% in S. aureus isolates from pediatric patients in the USA during the period of 2005–2014 [52]. There was also a great degree of geographical variability in the resistance rates. Ceftaroline, an expanded spectrum cephalosporin with MRSA activity, was used as adjunct therapy in four children who survived. Ceftaroline has been approved for treatment of community-acquired pneumonia in adults and children, specifically infections due to S. pneumoniae [52]. Data on efficacy for treatment of pneumonia due to S. aureus, including MRSA, are limited [53]. Cies et al. [54] described the ceftaroline pharmacokinetics in seven children (mean age 7, range 1–12 years) with suspected or confirmed MRSA infections in the PICU. These patients had a larger volume of distribution and faster clearance than healthy children, suggesting that higher doses and a more frequent dosing interval may be needed. However, six of the seven had documented MRSA infection; all six responded clinically and microbiologically with any dosing adjustments.
S. aureus is also the most frequent cause of acute hematogenous osteomyelitis and septic arthritis in children in the USA. Vancomycin is frequently used for initial presumptive therapy in these children. McNeil et al. [55] performed a retrospective review of children with acute hematogenous osteomyelitis or septic arthritis who had positive blood cultures for S. aureus, seen at Texas Children’s Hospital from 2011 to 2014. A total 102 cases were identified; 35 (34.3%) were MRSA. Early transition to oral antibiotics was associated with a better outcome. There was no difference in rates of complications between children who received ≥ 7 days compared with those who < 7 days of vancomycin therapy. Prolonged courses of vancomycin and/or vancomycin serum troughs > 15μg/mL were not associated with decreased duration of fever, bacteremia, hospitalization, need for repeat operation, and orthopedic complications but were associated with acute kidney injury.
A second analysis of the same database examined the association of the vancomycin MIC, and if the isolates were positive for Panton–Valentine leucocidin (PVL) with clinical outcomes in children with acute hematogenous osteomyelitis and septic arthritis due to methicillin-susceptible S. aureus (MSSA) [57]. There were 183 cases of MSSA: 26.2% were USA300, 23.5% PVL positive. Although MRSA isolates were more likely to have a vancomycin MIC ≥ 1.5 μg/mL (done by Etest) than MSSA isolates (43.4 to 61.7%, P = 0.02), the proportion of MSSA isolates with vancomycin MICs ≥ 1.5 μg/mL significantly increased in the second half of the study period (from 51.7 to 71.8%, P = 0.004). Children with MSSA isolates that had an elevated vancomycin MIC were more likely to undergo multiple surgical procedures and have venous thromboses even when adjusting for presumptive therapy with a β-lactam antibiotic. There was no association of vancomycin MICs with patient’s age, underlying condition, or the proportion of isolates that were PVL positive or USA300. Vancomycin MICs ≥ 2 μg/mL were associated with adverse clinical outcomes in MSSA irrespective of antibiotic choice. The presence of an elevated vancomycin MIC in a MSSA isolate may be a surrogate marker for organism virulence.
Conclusions
As of this writing there are several new antibiotics for the treatment of S. aureus infections in children that have been approved by the FDA or nearing approval. Ceftaroline and daptomycin are currently approved for use in children [53]. It is expected that the approved indications will continue to expand beyond skin and soft tissue infections and community-acquired pneumonia to include osteoarticular infections and others. Dalbavancin, telavancin, and tedizolid are currently in phase III trials in children in the USA. FDA approval is anticipated within 2 to 3 years. These drugs offer significant advantages over vancomycin for the treatment of MRSA infections in children. Ceftaroline has an excellent safety profile and does not require monitoring of serum levels. Daptomycin has once-daily dosing, making it suitable for outpatient IV therapy against a wide range of potentially resistant Gram-positive infections. One major drawback is that it cannot be used for pulmonary infections. Prolonged therapy with daptomycin has also been associated with the emergence of resistance, especially if the patient has received prior vancomycin. The emergence of daptomycin resistance may be avoided by using combination therapy with a β-lactam antibiotic, which seems to also be synergistic. Although dalbavancin and telavancin are not yet approved, they offer superior antimicrobial activity, safety, and ease of dosing to vancomycin. Tedizolid is the only new antistaphylococcal agent that is also available in an oral formulation. This strength, plus once-a-day, dosing offers major advantages over linezolid, although cost will be an issue, especially because linezolid will shortly be available generically. The use of these drugs has the potential to shorten hospitalization and significantly reduce costs for pediatric care.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Klein EY, Sun L, Smith DL, Laxminarayan R. The changing epidemiology of methicillin-resistant Staphylococcus aureus in the United States: a national observational study. Am J Epidemiol. 2013;177(7):666–74.
David MZ, Daum RS. Community-associated methicillin-resistant Staphylococcus aureus: epidemiology and clinical consequences of an emerging epidemic. Clin Microbiol Rev. 2010;23(3):616–87.
Spagnolo AM, Panatto OD, Amicizia D. Staphylococcus aureus with reduced susceptibility to vancomycin in healthcare settings. J Prev Med Hyg. 2014;55:137–44.
Rybak MJ, LaPlante KL. Community-associated methicillin-resistant Staphylococcus aureus; a review. Pharmacotherapy. 2005;25:74–85.
Patel M, Waites KB, Moser SA. Prevalence of inducible clindamycin resistance among community- and hospital-associated Staphylococcus aureus isolates. J Clin Microbiol. 2006;44(7):2481–4.
Chavez-Bueno S, Bozdogan B, Katz K. Inducible clindamycin resistance and molecular epidemiologic trends of pediatric community-acquired methicillin-resistant Staphylococcus aureus in Dallas, Texas. Antimicrob Agents Chemother. 2005;49(6):2283–8.
Howden BP, Davies JK, Johnson PD. Reduced vancomycin susceptibility in Staphylococcus aureus, including vancomycin-intermediate and heterogeneous vancomycin-intermediate strains: resistance mechanisms, laboratory detection, and clinical implications. Clin Microbiol Rev. 2010;23(1):99–139.
Cosgrove SE, Carroll KC, Perl TM. Staphylococcus aureus with reduced susceptibility to vancomycin. Clin Infect Dis. 2004;39(4):539–45.
Kalil AC, Van Schooneveld TC, Fey PD, Rupp ME. Association between vancomycin minimum inhibitory concentration and mortality among patients with Staphylococcus aureus bloodstream infections: a systematic review and meta-analysis. JAMA. 2014;312:1552–64.
Murray KP, Zhao JJ, Davis SL, Kullar R, Kaye KS, Lephart P, et al. Early use of daptomycin versus vancomycin for methicillin-resistant Staphylococcus aureus bacteremia with vancomycin minimum inhibitory concentration >1 mg/L: a matched cohort study. Clin Infect Dis. 2013;56:1562–9.
Wong-Beringer A, Joo J, Tse E, Beringer P. Vancomycin-associated nephrotoxicity: a critical appraisal of risk with high-dose therapy. Int J Antimicrob Agents. 2011;37:95–101.
Van Hal SJ, Paterson DL, Lodise TP. Systematic review and meta-analysis of vancomycin-induced nephrotoxicity associated with dosing schedules that maintain troughs between 15 and 20 milligrams per liter. Antimicrob Agents Chemother. 2013;57:734–44.
Filippone EJ, Kraft WK, Farber JL. The nephrotoxicity of vancomycin. Clin Pharmacol Ther. 2017;102(3):459–69.
Gomes DM, Smotherman C, Birch A, Dpree L, Della Vecchia BJ, Kraemer DE, et al. Comparison of acute kidney injury during treatment with vancomycin in combination with piperacillin-tazobactam or cefepime. Pharmacotherapy. 2014;4:662–9.
Moenster RP, Linneman TW, Finnegan PM, Hand S, Thomas Z, McDonald. Acute renal failure associated with vancomycin and β-lactams for the treatment of osteomyelitis in diabetics: piperacillin-tazobactam as compared with cefepime. Clin Microbiol Infect. 2014;20:O384–O38.
Hammond DA, Smith MN, Painter JT, Meena NK. Comparative incidence of acute kidney injury in critically ill patients receiving vancomycin with concomitant piperacillin-tazobactam or cefepime: a retrospective cohort study. Pharmacotherapy. 2016;36:463–71.
Giuliano C, Patel CR, Kale-Pradhan PB. Is the combination of piperacillin-tazobactam and vancomycin associated with development of acute kidney injury? A meta-analysis. Pharmacotherapy. 2017. https://doi.org/10.1002/phar.185.
van Hal SJ, Lodise TP, Paterson DL. The clinical significance of vancomycin minimum inhibitory concentration in Staphylococcus aureus infections: a systematic review and meta-analysis. Clin Infect Dis. 2012;54:755–71.
Song KH, Kim M, Kim JC. Impact of vancomycin MIC on treatment outcomes in invasive Staphylococcus aureus infections. Antimicrob Agents Chemother. 2017;61(3):e01845–16.
Soriano A, Marco F, Martinez JA, Pisos E, Almela M, Dimova VP, et al. Influence of vancomycin minimum inhibitory concentration on the treatment of methicillin-resistant Staphylococcus aureus bacteremia. Clin Infect Dis. 2008;46:193–200.
Clinical and Laboratory Standards Institute (CLSI). Performance standards for antimicrobial susceptibility testing. 26th ed. CLSI supplement M100S. CLSI: Wayne, PA; 2016.
Kehrmann J, Kaase M, Szabados F, Gaterman SG, Buer J, Rath PM, et al. Vancomycin MIC creep in MRSA blood culture isolates from Germany: a regional problem? Eur J Clin Microbiol Infect Dis. 2011;30:677–83.
Jones RN. Microbiological features of vancomycin in the 21st century: minimum inhibitory concentration creep, bactericidal/static activity, and applied breakpoints to predict clinical outcomes or detect resistant strains. Clin Infect Dis. 2006;42(Suppl 1):S13–24.
Hawser SP, Bouchillon SK, Hoban DJ. Rising incidence of Staphylococcus aureus with reduced susceptibility to vancomycin and susceptibility to antibiotics: a global analysis 2004–2009. Int J Antimicrob Agents. 2011;37:219–24.
Edwards B, Milne K, Lawes T. Is vancomycin MIC “creep” method dependent? Analysis of methicillin-resistant Staphylococcus aureus susceptibility trends in blood isolates from North East Scotland from 2006 to 2010. J Clin Microbiol. 2012;50(2):318–25.
Diaz R, Afreixo A, Ramalheira E. Evaluation of vancomycin MIC creep in methicillin-resistant Staphylococcus aureus infections-a systematic review and meta-analysis. Clin Microbiol Infect. 2018;24(2):97–104.
Goldman JL, Harrison CJ, Al M. No evidence of vancomycin minimal inhibitory concentration creep or heteroresistance identified in pediatric Staphylococcus aureus blood isolates. Pediatr Infect Dis J. 2014;33(2):216–8.
Liu C, Bayer A, Cosgrove SE, Daum RS, Fridkin SK, Gorwitz RJ, et al. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis. 2011;52:e18–55.
Rybak M, Lomaestro B, Rotschafer JC, Moellering R Jr, Craig W, Billeter M, et al. Therapeutic monitoring of vancomycin in adult patients: a consensus review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, and the Society of Infectious Diseases Pharmacists. Am J Health Syst Pharm. 2009;66:82–98.
Frymoyer A, Hersh AL, Benet LZ, Guglielmo BJ. Current recommended dosing of vancomycin for children with invasive methicillin-resistant Staphylococcus aureus infections is inadequate. Pediatr Infect Dis J. 2009;28(5):398–402.
Hsu AJ, Hamdy RF, Huang Y, Olson JA, Ghobrial S, Gerber JS, et al. Vancomycin trough concentrations and duration of methicillin- resistant Staphylococcus aureus bacteremia in children. J Pediatric Infect Dis Soc. 2018 Dec 3;7(4):338–41. https://doi.org/10.1093/jpids/pix068.
Le J, Bradley JS, Murray W. Improved vancomycin dosing in children using area-cnder-the-curve exposure. Pediatr Infect Dis J. 2013;32(4):e155–63.
Hoang J, Dersch-Mills D, Bresee L. Achieving therapeutic vancomycin levels in pediatric patients. Can J Hosp Pharm. 2014;67(6):416–22.
Benner KW, Worthington MA, Kimberlin DW, Hill K, Buckley K, Tofil NM. Correlation of vancomycin dosing to serum concentrations in pediatric patients: a retrospective database review. J Pediatr Pharmacol Ther. 2009;14(2):86–93.
Glover ML, Cole E, Wolfsdorf J. Vancomycin dosage requirements among pediatric intensive care unit patients with normal renal function. J Crit Care. 2000;15(1):1–4.
Frymoyer A, Hersh AL, Coralic Z, Benet LZ, Guglielmo BJ. Prediction of vancomycin pharmacodynamics in children with invasive methicillin- resistant Staphylococcus aureus infections: a Monte Carlo simulation. Clin Ther. 2010;32(3):534–42.
Geerlof LM, Boucher J. Evaluation of vancomycin dosing and corresponding drug concentrations in pediatric patients. Hospital Pediatrics. 2014;4:342–7. https://doi.org/10.1542/hpeds.2014-0019.
Durham SH, Simmons ML, Mulherin DW, Foland JA. An evaluation of vancomycin dosing for complicated infections in pediatric patients. Hospital Pediatrics. 2015;5:276–81. https://doi.org/10.1542/hpeds.2014-0081.
Frymoyer A, Guglielmo BJ, Hersh AL. Desired vancomycin trough serum concentration for treating invasive methicillin-resistant staphylococcal infections. Pediatr Infect Dis J. 2013;32(10):1077–9.
Hwang D, Chang-Nan C, Chang L, Peng CC. Vancomycin dosing and target attainment in children. J Microbiol Immunol Infect. 2017;50(4):494–9.
Chhim RF, Arnold SR, Lee KR. Vancomycin dosing practices, trough concentrations, and predicted area under the curve in children with suspected invasive staphylococcal nfections. J Pediatr Infect Dis Soc. 2013;2(3):259–62.
•• Silva Alves GC, Dutra da Silva S, Ftade VP, Rorigues D, Baldoni AO, de Castro WV, et al. Determining the optimal vancomycin daily dose for pediatrics: a meta-analysis. Eur J Clin Pharmacol. 2017;73(11):1341–53. Important meta-analysis summarizing vancomycin daily dose in pediatric patients.
Hale CM, Seabury RW, Steele JM, Darko W, Miller CD. Are vancomycin trough concentrations of 15 to 20 mg/L associated with increased attainment of an AUC/MIC ≥ 400 in patients with presumed MRSA infection? J Pharm Pract. 2017;30(3):329–35. https://doi.org/10.1177/0897190016642692.
Kishk OA, Lardieri AB, Heil EL, Morgan JA. Vancomycin AUC/MIC and corresponding troughs in a pediatric population. J Pediatr Pharmacol Ther. 2017;22(1):41–7.
•• Fiorito TM, Luther MK, Dennehy PH, LaPlante KL, Matson KL. Nephrotoxicity with vancomycin in the pediatric population: a systematic review and meta-analysis. Pediatr Infect Dis J. 2018;37(7):654–61. Important meta-analysis summarizing nephrotoxicity in pediatric patients.
Turner RB, Kojiro K, Shephard EA, Won R, Chang E, Chan D, et al. Review and validation of Bayesian dose-optimizing software and equations for calculation of vancomycin area under the curve in critically ill patients. Pharmacotherapy. 2018;38(12):1174–83.
Neely MN, Kato L, Youn G, Kraler L, Bayard D, van Guilder M, et al. Prospective trial on the use of trough concentration versus area under the curve to determine therapeutic vancomycin dosing. Antimicrob Agents Chemother. 2018;62(2):e02042–17. https://doi.org/10.1128/AAC.02042-17.
•• Randolph AG, Xu R, Novak T, Newhams MM, Wardenburg JB, Weiss SL, et al. Vancomycin monotherapy may be insufficient to treat methicillin-resistant Staphylococcus aureus coinfection in children with influenza-related illness. Clin Infect Dis. 2019;68(3):365–72. https://doi.org/10.1093/cid/ciy495. Important clinical study demonstrating poor outcome in children who were treated with vancomycin alone.
Stein GE, Wells EM. The importance of tissue penetration in achieving successful antimicrobial treatment of nosocomial pneumoniae and complicated skin and soft-tissue infections caused by methicillin-resistant Staphylococcus aureus: vancomycin and linezolid. Curr Med Res Opin. 2010;25:571–88.
Geriak M, Haddad F, Rizvi K, Rose W, Kullar R, LaPlante K, et al. Clinical data on daptomycin plus ceftaroline versus standard of care monotherapy in the treatment of methicillin-resistant Staphylococcus aureus bacteremia. Antimicrob Agents Chemother. 2019;63:e02483–18.
• Sutter DE, Milburn F, Chukwuma U, Dzialowy N, Maranich AM, Hospenthal DR. Changing susceptibility of Staphylococcus aureus in a US pediatric population. Pediatrics. 2016;137:e20153099. Survey demonstrating increasing significant levels of clindamycin resistance among S. aureus isolates from children in the USA.
Cies JJ, Moore WS 2nd, Enache A, Chopra A. Ceftaroline for suspected confirmed invasive methicillin-resistant Staphylococcus aureus: a pharmacokinetic case series. Pediatr Crit Care Med. 2018;19:e292–9.
Sharma R, Francois D, Hammerschlag MR. New antimicrobial agents for the treatment of staphylococcal infections in children. Pediatr Clin N Am. 2017;64:1369–87.
McNeil JC, Kaplan SL, Vallejo JG. The influence of the route of antibiotic administration, methicillin susceptibility, vancomycin duration and serum trough concentration on outcomes of pediatric Staphylococcus aureus bacteremic osteoarticular infection. Pediatr Infect Dis. 2017;36:572–7.
Krok EY, Vallejo J, Sommer LM, Rosas L, Kaplan SL, Hulten KG, et al. Association of vancomycin MIC and molecular characteristics with clinical outcomes in methicillin-susceptible Staphylococcus aureus acute hematogenous osteoarticular infections in children. Antimicrob Agents Chemother. 2018;62:1–10.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pediatric Infectious Diseases
Rights and permissions
About this article
Cite this article
Sharma, R., Hammerschlag, M.R. Treatment of Methicillin-Resistant Staphylococcus aureus (MRSA) Infections in Children: a Reappraisal of Vancomycin. Curr Infect Dis Rep 21, 37 (2019). https://doi.org/10.1007/s11908-019-0695-4
Published:
DOI: https://doi.org/10.1007/s11908-019-0695-4