Abstract
Cryptococcus neoformans is an encapsulated fungal pathogen that is remarkable for its tendency to cause meningoencephalitis, especially in patients with AIDS. While disease is less common in children than adults, it remains an important cause of morbidity and mortality among HIV-infected children without access to anti-retroviral therapy. This review highlights recent insights into both the biology and treatment of cryptococcosis with a special emphasis on the pediatric literature.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cryptococcosis is fungal disease that most commonly manifests as meningoencephalitis (CME), disseminated disease and pneumonia. Disease occurs globally though for unknown reasons; children are much less commonly affected than adults. Cryptococcosis is caused primarily by two distinct species, Cryptococcus neoformans (CN) and Cryptococcus gattii. Disease caused by these two species is similar in many ways, though important epidemiologic and clinical differences exist, highlighting the genetic divergence of these species an estimated 49 million years ago [1].
C. gattii was first recognized for its tendency to cause disease in the native peoples of tropical and sub-tropical areas of the world, especially Australasia. More recently, this organism has been increasingly recognized to cause disease outside these regions, including an outbreak in the Pacific Northwest. Disease often occurs in individuals without known immunodeficiency, though subtle defects in immunity (e.g., anti-granulocyte-macrophage colony stimulating factor (GMCSF) antibodies) have been recognized [2••].
CN disease occurs globally with an estimated burden of 1 million cases resulting in 625,000 deaths annually [3]. This condition is primarily an opportunistic infection especially among individuals (including children) with defects in T cell immunity, though cases of CN disease in individuals without recognized immunodeficiency are regularly reported. The history and prevalence of CN disease is especially remarkable for its association with the AIDS epidemic. Accordingly, the highest rates of cryptococcosis are seen in sub-Saharan African where anti-retroviral therapy (ART) is unavailable to many. This report focuses of recent advance in CN disease, especially as it relates to children with HIV disease.
The Organism
In the environment, CN is a typical saprophyte, deriving nourishment from dead and dying organic material. Organisms can be readily isolated from the environment, including bird (especially pigeon) droppings and decaying trees. Interestingly, CN is not thought to be a pathogen or colonizer of birds. The emergence of CN as a human pathogen has been hypothesized to correlate with selective advantages provided by specific traits that promote survival advantages in interactions with natural predators such as soil ameba (reviewed in [4]). Within in the host, this pathogen is a facultative intracellular pathogen that is well suited for intracellular survival. The interaction between CN and macrophages plays a central role in cryptococcal pathogenesis [5, 6].
A number of virulence factors have been identified and well characterized, including encapsulation, melanin production, and the ability to grow at 37 °C. Modulation of the immune response through the elicitation of non-protective and/or protective immunity is central to cryptococcal pathogenesis. In this regard, the polysaccharide capsular material is remarkable for its ability to interfere with opsonization [7], impair chemotaxis [8, 9] and actively promote non-protective TH2 inflammation [10]. The capsular material is actively shed into tissue during infection [11] and has been hypothesized to play a role in promoting increased intracranial pressure (ICP) [12–14]. Besides the polysaccharide capsule, increasing attention has focused cell wall-associated polysaccharides, including chitin in cryptococcal pathogenesis. Strains deficient in chitosan (the deacetylated form of chitin) show decreased virulence in animal models [15]. Chitin associates with polysaccharide capsule, provides structural integrity to the cell, and modifies the immune response [16, 17•]. Specifically, chitin recognition via chitotriosidase promotes non-protective TH2 inflammation [18••]. Consistent with the saprophytic nature of this pathogen, a variety of enzymes (both secreted and non-secreted) have also been linked to virulence, including glucosylceramide synthase, phospholipase, urease, and metalloprotease (reviewed in [19].
Several unique processes that contribute to cryptococcal virulence have recently been identified. This includes the formation of giant or titan cells, which can reach up to 100 μm in cell body diameter compared to the typical cell size of 5–7 μm. Titan cells display cross-linked capsules, thickened cell walls, and increased ploidy [20]. Titan cells are more resistant to phagocytosis. They are also more virulent and exhibit enhanced dissemination in experimental cryptococcosis [21].
Additionally, CN can induce its own extrusion from phagocytic cells through a process known as non-lytic exocytosis [22–24]. Non-lytic exocytosis, which is appears to be regulated by the local pH, allows organisms can escape the phagosomal component of infected host cells without rupturing the host cell. It also enables the transfer of organisms from one cell to another. Presumably, this process plays an important role in promoting dissemination within the host.
CN is capable of undergoing significant phenotypic variation through different mechanisms that can subvert the host immune response. This includes phenotypic switching [25] and replicative aging [26••]. Phenotypic switching is a high frequency reversible process that produces strains with specific phenotypic differences. These changes affect important physical characteristics of the organism including the capsule resulting in significant changes in virulence and the ability to induce ICP [13]. In replicative aging, founder cells develop a thickened cell wall, which inhibits phagocytosis and killing by antifungals in vitro. It has been hypothesize that the accumulation of old cells in vivo can lead to persistence and resistance to antifungal therapy [27•]. The ability of the CN to respond to changes in the local environment has also been increasing realized. For example, quorum sensing and the local release of metabolites (e.g., pantothenic acid) that alter the expression of virulence factors has been described [28, 29••].
Pathogenesis
Infection is thought to be acquired through inhalation of aerosolized and possibly desiccated organisms. A central but poorly understood issue of cryptococcal pathogenesis relates to whether diseases result from the reactivation of a latent focus of infection in the setting of immunosuppression versus progression of a primary infection. Several lines of evidence (including pathology, molecular typing, animal models, and serologic studies) indicate that reactivation type disease (similar to tuberculosis) can occur [30–33]. According to this model, infection is acquired early in life, but remains latent only to be re-activated in the context of immunosuppression. Primary progressive infection also appears to occur as indicated by outbreaks reports and the demonstration of recent acquisition of infection from the local environment [34].
As a pathogen, CN is somewhat unique in its avidity to the CNS. Three mechanisms have been proposed to explain how CN enters the CNS, though relative contribution of each to the disease state is unknown. According to the Trojan horse theory, CN enters the CNS via infected macrophages or monocytes. In support of this theory, depletion of macrophages has been shown to reduce CNS fungal burden in a murine model of cryptococcosis [35]. Likewise, infection of animals using macrophages containing CN enhances dissemination into the CNS. Alternatively, CN can enter the CNS through endothelial cell uptake via a process known as transcytosis, which can be demonstrated both in vitro and in vivo [36]. This appears to be an active process and likely involves the secretion of enzymes (e.g., metalloproteases [37••], urease [38]) in conjunction with the binding of pathogen-associated ligands like hyaluronic acid to host receptors (CDD44) on endothelial cells [39]. Finally, CN may enter the CNS by damaging the intercellular connections between endothelial cells. This process has been hypothesized to involve capsular-induced damage to endothelial cells [40] and be associated with changes in intracellular actin arrangement [41].
Pediatric Cryptococcosis
Due to the rarity of pediatric cryptococcosis, the precise prevalence is difficult to define and may vary by region. Studies of US children with AIDS in the 1990s estimated an incidence of cryptococcosis to be about 1 % [42]. The basis for this lower incidence of cryptococcosis among children when compared with adults remains poorly understood, but could be related to differences in exposure and/or immune response that allows for progression of disease. Serologic studies suggest that in certain urban areas, sub-clinical cryptococcal infection is common among children older than 2 years of age [43, 44]. Furthermore, these studies suggest ongoing exposure throughout childhood. Nonetheless, it is possible that the type of exposure in children is qualitatively (e.g., different strains) or quantitatively different when compared with adults [45]. Besides AIDS, cryptococcosis has been described in the context of primary and acquired immunodeficiencies as well as in apparently healthy children. This includes hyper IgM syndrome [46], hyper IgE syndrome [47], Bruton’s agammaglobulinemia [48], SLE [49], leukemia [50], and sarcoma [51]. Organ transplantation and the use of biologic agents (e.g., anti-TNF antibodies [52]) are also recognized as important risk factors for cryptococcosis. Recent studies in adults suggest that subtle differences in the immune system including polymorphism in Fc receptors [53, 54••] and antibodies to GMCSF [2••] may play an unrecognized role in susceptibility to cryptococcal infection in both apparently healthy individuals and those that are immunocompromised.
Because of the relatively small number of cases of pediatric cases of cryptococcosis, much of our understanding and recommendations regarding this disease represent extrapolations from adult data. Since 2009, there have been four series from different parts of the world (USA, Brazil, South Africa, and Colombia) describing the pediatric experience with cryptococcosis in HIV-infected children [55–57, 58••]. The number of children in these studies ranges from 41 to 361. The percent of HIV infection children in these studies varies from 16 % in a US study to 91 % in a South African study. Series of pediatric cryptococcosis have also been recently reported from China and Taiwan. These studies are remarkable for the percent of children without underlying immunodeficiency and the absence of HIV infection [59, 60]. The reported mortality of pediatric cryptococcosis in these series ranges from 9.5 to 43 % [55, 56, 61].
The largest description of pediatric (age <15 years) cryptococcosis (n = 361, 91 % HIV infected) comes from South Africa [57]. In this series, pediatric cryptococcosis represented 2 % of all cryptococcal cases over a 2-year period with an annual incidence of 47 cases per 100,000 persons for HIV-infected children when compared with 120 cases per 100,000 in HIV-infected adults. A bimodal peak in the incidence was found with the greatest incidence in children <1 year of age and a second peak among children 5–10 years of age. Among children <1 year of age, this incidence was comparable to that of Haemophilus influenzae meningitis among children less than 1 year. Among children undergoing testing, the majority of HIV infected had CD4+ T cell counts less than 50 cells/uL and CD4+ T cell percentages less than 15 %. When compared with adults with cryptococcosis, affected children were less likely to have HIV and more likely to be infected with C. gattii (7 % of pediatric cohort). This peak in incidence in children <1 year has not been described in other pediatric series with most reports describing a peak incidence in older children (age 8–12 years), including reports from Botswana and Ghana [62, 63]. The authors suggest that rapid HIV progression in some infants associated with congenital HIV infection may be responsible for this peak [57]. Interestingly, while cryptococcosis during pregnancy is well described, congenital cryptococcosis is thought to be rare. Infection may occur via swallowing or inhalation of infected materials. Placental transmission may also occur though in general the placenta appears to be a very effective barrier in preventing fetal infection [64].
The most recent pediatric series of cryptococcosis comes from a national survey of Colombian children (<16 years) over an 18-year period in 2014 [58••]. This series highlights important trends in pediatric cryptococcosis including the emergence of non-AIDS cases of cryptococcosis in regions where ART is available. In this series, the annual incidence of pediatrics cryptococcosis was 0.017 to 0.12 cases per 100,000 children depending on the region of the country. Overall, 41 children were identified 10 (24.4 %) were HIV positive, 3 (7.3 %) had reporter either corticosteroid use, malignancy or autoimmune disease, and 19 (46.3 %) had no known risk factors. The mean age of affected children in this series was 8.4 years with a slight male predominance, which is similar to what has been described in previous pediatric series [42, 65, 66]. The most common form of disease was neurocyptococcosis (87.8 %), which was followed by the disseminated disease (12.2 %). Among the five patients with disseminated disease, two had skin involvement. The most common symptoms were headache (78.1 %), fever (68.8 %), nausea and vomiting (65.6 %), confusion (50 %), and meningeal signs (37.5 %).
Recent Advances in Diagnosis
Traditionally, cryptococcosis has been diagnosed by a variety of techniques, including India ink staining, latex agglutination, enzyme immunoassays (EIAs), and culture. More recently, a rapid diagnostic lateral flow assay (LFA) (IMMY, Norman, OK, USA) has been developed. This inexpensive assay can be performed in less than 10 min and remains stable at room temperature, making it ideal as a point of care test for resource-limited settings. The LFA detects glucuronoxylomannan, the primary capsular polysaccharide antigens and distinguishes between the four major cryptococcal serotypes (A and D for C neoformans and B and C for C. gattii) [67•]. The LFA is currently FDA approved for use on cerebrospinal fluid (CSF) samples only; however, it is also highly sensitive and specific for serum testing [67•, 68•].
LFA testing of the CSF also appears to correlate with fungal burden and may be useful in prognosis. A prospective study conducted in Uganda examined the accuracy of the LFA compared to standard diagnostic tests and also sought to correlate the LFA titer with mortality at 2 and 10 weeks. Higher LFA titers prior to antifungal treatment correlated with increased mortality and each twofold increase in titer led to incremental increases in both 2 and 10-week mortality [69•].
The LFA has limited utility in measuring response to therapy. Another limitation of this assay (as observed with the latex agglutination test) is the presence of false negatives due to the prozone phenomenon, which occurs in the context of antigen excess. This phenomenon can be eliminated by including a specimen dilution step in testing [70•].
Given high incidence and mortality of cryptococcosis in areas of the world with limited access to ART, the World Health Organization currently recommends routine screening using the LFA on blood or serum samples for HIV-infected adults with CD 4+ T cell counts ≤100 cell/uL (who.int/hiv/pub/cryptococcal_disease2011/en/). Individuals with a positive LFA assay should undergo CSF testing including measurement of opening pressure with prompt institution of therapy. A prospective study evaluating preemptive fluconazole treatment of LFA positive high-risk individuals did indeed find a decrease in development of cryptococcal meningitis [70•]. Current guidelines, however, do not call for routine screening of children because of the relatively lower incidence of pediatric cryptococcosis.
Therapy
There are currently only three classes of antifungals used to treat cryptococcosis: polyenes (amphotericin B), azoles, and a pyrimidine analog flucytosine (5-FC). Of note, CN is inherently resistant to echinocandins. The treatment regimen for cryptococcosis depends on the type of disease and the underlying immune status of the host. For CME and disseminated disease in HIV-infected children, the Infectious Disease Society of America guidelines recommend the combination amphotericin B deoxycholate and 5-FC for initial induction phase of therapy (minimal of 2 weeks) [71]. This is followed by a consolidation phase with 8 weeks of fluconazole. Once this has been completed maintenance (suppressive therapy) should be instituted. Discontinuation of maintenance therapy in children receiving ART and CD4 T cell >100/μl and sustained (>3 months) virologic response are poorly studied but should be considered. These guidelines are based on extrapolation of adult studies, as pediatric studies are not available given the relatively small number of cases. Despite standard therapy, the mortality and morbidity of CME remains high. Furthermore, treatment of CME is significantly limited in areas of the world (e.g., Africa and Asia) where CME incidence is highest due to limitations in drug availability (amphotericin and 5-FC).
The most common side effect of amphotericin B deoxycholate is nephrotoxicity, including urinary potassium and magnesium wasting, renal tubular acidosis, and nephrogenic diabetes insidipus. The risk of nephrotoxicity can be lowered with the use of lipid formulations of amphotericin B and the avoidance of other nephrotoxic drugs. Pre-hydration with normal saline also reduces the renal toxicity associated with amphotericin B. Furthermore, lipid preparation of amphotericin (liposomal amphotericin B (3–4 mg/kg) and amphotericin B lipid complex (5 mg/kg)) may be used as alternatives for the treatment of CME in individuals with underlying renal dysfunction. Other adverse events include infusion-related reaction and a reversible normocytic anemia. The most prominent side effect of 5-FC is hematologic toxicity including leukopenia and thrombocytopenia, which tends to occur within the first 2 weeks of use. 5-FC toxicity is associated with elevated aminotransferases, hepatic necrosis, and gastrointestinal upset, and thus, periodic monitoring of serum concentrations is recommended.
Several studies highlight the importance of combination amphotericin/5-FC in the initial treatment of CNS cryptococcosis [72–74]. The most recent is a prospective, randomized trial conducted in Vietnam [75••]. Specifically, this trial compared the efficacy of combination therapy with amphotericin B and 5-FC versus amphotericin B and fluconazole, or amphotericin B alone in the initial treatment of CME in HIV-infected individuals. Individuals receiving combination therapy with 5-FC had improved survival at both 10 weeks and 6 months after diagnosis when compared with either group. Enhanced CSF fungal clearance was also observed with amphotericin 5-FC combination therapy. In contrast, combination therapy with amphotericin B and fluconazole did not offer survival benefit when compared with amphotericin monotherapy. This study was open to individuals over 14 years age though the median age was 28 years, and the number of children was not documented.
Despite the demonstrated utility of amphotericin and 5-FC in the initial treatment of CME, these drugs are not routinely available in most parts of Asia and Africa where CME burden is greatest [76•]. In response, a variety of trials have been devised to develop new treatment strategies that provide optimal outcome with limited drug requirement. In a study conducted in Malawi, 5-FC was studied in combination with fluconazole for the initial induction therapy in adults with CME. This study demonstrated that the combination of 5-FC with high doses of fluconazole (1200 mg/day) enhanced clearance of CN from the CSF at 2 weeks when compared with fluconazole monotherapy. Improved survival at 2 and 10 weeks was also noted [77]. A follow-up study evaluated the effects of the addition of short-term amphotericin (7 days) to either fluconazole alone or fluconazole plus 5-FC in initial induction therapy [78]. Early fungal clearance was highest for patients receiving triple therapy, though the study was not powered to discern differences in survival. A multi-center phase II/III non-inferiority trial is underway to test the therapeutic utility of short courses of high-dose liposomal amphotericin B (AmBisome) combined with high-dose fluconazole in HIV-positive adults with CME [79•].
The potential utility of adjuvant γ-interferon therapy in cryptococcosis has been studied in animal models [80, 81] and limited human studies [82, 83]. γ-Interferon plays an important role in activation macrophages an inhibiting intracellular growth of CN [84]. In a randomized controlled study, HIV-infected adult patients with CME were initially treated with the combination amphotericin B and 5-FC alone or together with γ-interferon [82]. Though the study was not powered to detect differences in mortality, even a short course (two doses) of adjuvant γ-interferon was associated with enhances CSF fungal clearance. Importantly, fungal clearance has been previously established as a surrogate for outcome in CME treatment studies [85]. Of note, no increase in IRIS was noted.
Fluconazole Resistance
The potential for the emergence fluconazole resistance among CN strains has gained increasing attention especially in areas where anti-retroviral therapy (ART) is not available, and there is widespread use of fluconazole. A surveillance study of cryptococcal isolates from across the globe (Asia-Pacific region, Latin America, Africa/Middle East, and North America) over a 10.5-year (1997–2007) period revealed an overall increase in resistance in fluconazole (as determined by CLSI standardized disk diffusion testing) from 7.3 to 11 % though susceptibility to voriconazole was preserved (with resistant rates of 1.7 to 1.8 %) [64]. The increase in fluconazole resistance was most prominent in certain regions (e.g., Africa/Middle East, Asia Pacific Region) where resistance rose to as high as 33 %. In contrast, resistance among North American isolates initially rose, but then decreased to 0 % in the 2005–2007 period. Nonetheless, high rates of fluconazole resistance have not been reported in other studies including one performed on African isolates [65]. Furthermore, the clinical significance reported fluconazole resistance is complicated by issues surrounding optimal testing methodologies and correlations between in vitro susceptibility and clinical response. In a review of the literature, Cheong and McCormack reported on 20 cases of fluconazole resistance in patients with CME over a 20-year period (from 1991 to 2011) [66]. Interestingly, 30 % of patient in these studies had no prior fluconazole exposure consistent with the notion that these strains may be inherently resistant to fluconazole. Inherent fluconazole resistance in CN that may not be readily detected initially, but result in clinical failure may occur through a phenomenon known as heteroresistance. In heteroresistance sub-populations of organisms are able to adapt to increasing concentrations of fluconazole. This correlates with the development of disomy in certain chromosomes, which include genes that code for the target enzyme, alpha demethylase, and azole efflux pumps [67•, 68•]. Current recommendations suggest testing for fluconazole susceptibility in the context of treatment failure [71].
Increased Intracranial Pressure
Elevated intracranial pressure (ICP) has been reported to occur in up to 60 % of adults with CME and is an important determinant of morbidity and mortality in this disease [14, 86•]. The incidence of increased ICP in children with CME is poorly defined. In two pediatric series, where the CSF opening pressure was measured, the percentage of patients with intracranial hypertension was very high ranging between 73.9 and 83 % [65, 87]. The reasons why CME is so commonly associated with increased ICP is poorly understood, though there has been significant speculation concerning the role of the capsular polysaccharide in this process. Capsular material is actively shed within the CSF and brain during infection. The large molecular size and viscous nature of this polysaccharide has been hypothesized to interfere with CSF reabsorption at the level of the arachnoid grannulations [13, 88, 89]. Accumulation of polysaccharide within the brain tissue intercellular spaces has also been suggested to result in an osmotic edema [12]. Edema may additionally exacerbate the problem of impaired CSF reabsorption by producing a stiff brain that is unable to accommodate the increased volume of CSF within the ventricular space.
Current guidelines emphasize the importance of alleviating increased intracranial pressure in the treatment of CME. For patients with pressure greater than 25 cm of H2O and symptoms of increased intracranial pressure, CSF should be removed to reduce to a normal pressure ≤20 cm of CSF or by 50 % if ICP is extremely high [71]. Despite current recommendations, lack of awareness or access to manometers in resource-limited countries hinders the utility of therapeutic lumbar punctures despite evidence that patients receiving at least one therapeutic LP after diagnosis have decreased mortality perhaps even in patients with a normal initial opening pressure [90••].
Overall, corticosteroids should not be used as adjunctive therapy for increased ICP associated with CME. In an initial study of HIV-infected patients with CME, corticosteroid use was associated with lower rates of clinical response and higher mortality, though the sample size in this group was small [14]. More recently, a double-blinded randomized trial examining the effects of adjunctive dexamethasone in CME among 451 patients in Asia and Africa confirmed these findings. In this study, corticosteroids did not reduce mortality and was associated with more adverse events and disability than was placebo [91••]. Findings from these studies are consistent with the hypothesis that corticosteroids can weaken an already impaired immune response. In contrast, corticosteroids have been used to treat severe recalcitrant, increased ICP associated with C. gattii infection in immunocompetent individuals, although additional study is needed before this practice become routine [92••, 93]. It seems likely that the utility of corticosteroid in CME is dependent on several variables including local host inflammatory response, infecting strain, and stage of infection.
IRIS
As seen with other opportunistic infections, AIDS patients with CME can experience a paradoxical worsening of symptoms due to immune reconstitution inflammatory syndrome (IRIS) in association with improved immune function secondary to ART. This can present as relapsing aseptic meningitis, increased intracranial pressure, new focal neurologic signs, intracranial cryptococcomas, lymphadenopathy, or development of abscesses [94••]. Alternatively, IRIS may unmask previously unrecognized cryptococcosis. The occurrence of IRIS in CME varies widely with a median of 1–10 months but may occur as late as 41 months [95•]. There is minimal data on IRIS in pediatric CME. In a recent report of seven HIV-infected children with CME from South Africa, IRIS was felt to contribute significantly to the morbidity and mortality of this disease. Potential manifestations of IRIS in this cohort included increase ICP, nodal airway compression, and skin nodules [96•]. Corticosteroids are typically used in conjunction with ongoing antifungal therapy to treat CME-associated IRIS especially in those associated with increasing CNS inflammation and increased ICP.
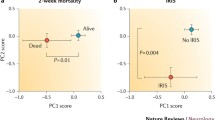
There is conflicting data on the effects of early ART for HIV-infected patients with CME. An initial study involving 41 patients with CME found that early ART produced non-significant decreases in mortality [97]. In contrast, recent studies suggest improved outcomes in CME with delayed ART therapy. In this regard, early AZT therapy in HIV-positive was associated with an increased incidence of CME IRIS with no improvement in CSF fungal clearance [98••]. Furthermore, a randomized controlled trial of HIV-positive adults from South Africa and Uganda with CME found that patients who received earlier ART (1 to 2 weeks after CME diagnosis) had a 15 % higher mortality rate at 26 weeks compared with patients for whom ART was deferred for 5 weeks after diagnosis (45 vs. 30 %, p = 0.03) [99••]. The highest mortality rate was observed for patients with low initial white cell count (<5 WBC/μL) in the early\ ART group consistent with the notion that increased inflammatory response in the CNS due to ART-associated immune reconstitution was associated with damage to the host.
Subsequent immunologic analysis revealed that early ART initiation was associated with an elevated CSF WBC >5/μL at day 14 of amphotericin treatment and median of 6 days of ART treatment. This in turn correlated with elevated CSF macrophage markers (sCD14, sCD163). Interestingly, IL-13, a prototypical TH2 cytokine, was elevated in a sub-cohort of patients receiving early ART on day 14 of amphotericin treatment [100•]. In another study of CME-associated IRIS, lower numbers of antigen specific interferon gamma (a TH1 cytokine) producing T cells prior to ART were associated with increase mortality [101•]. Taken together, these findings highlight the potential contribution of enhanced TH2 inflammation in the morbidity and mortality of CME-associated IRIS. Clinically, these findings have translated into the practice of delayed (4–10 weeks) initiation of ART following a diagnosis of CME.
Conclusions
C. neoformans is a unique encapsulated fungal pathogen that is remarkable for its proclivity to cause meningoencephalitis with increased intracranial pressure among AIDS patients. Fortunately, with the advent of effective anti-retroviral therapy, the population of HIV-infected individuals at risk for CME has been significantly reduced. Nonetheless, current CME therapies are inadequate resulting in significant disease-associated morbidity and mortality among affected individuals. In areas of the world with limited resources, the number of cases of CME remains high and our ability to effectively treat disease is extremely limited. Significant gains have been made in our understanding of the host and pathogen features that contribute to disease pathogenesis. The development of new therapies based on these insights is urgently needed.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Ngamskulrungroj P, Gilgado F, Faganello J, Litvintseva AP, Leal AL, Tsui KM, et al. Genetic diversity of the Cryptococcus species complex suggests that Cryptococcus gattii deserves to have varieties. PLoS One. 2009;4(6):e5862.
Rosen LB, Freeman AF, Yang LM, Jutivorakool K, Olivier KN, Angkasekwinai N, et al. Anti-GM-CSF autoantibodies in patients with cryptococcal meningitis. J Immunol. 2013;190(8):3959–66. Identifies autoreactive antibodies to GM-CSF as a potential risk factor for cryptococcosis in otherwise healthy individuals.
Park BJ, Wannemuehler KA, Marston BJ, Govender N, Pappas PG, Chiller TM. Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDS. AIDS. 2009;23(4):525–30.
Casadevall A. Amoeba provide insight into the origin of virulence in pathogenic fungi. Adv Exp Med Biol. 2012;710:1–10.
Shao X, Mednick A, Alvarez M, van Rooijen N, Casadevall A, Goldman DL. An innate immune system cell is a major determinant of species-related susceptibility differences to fungal pneumonia. J Immunol. 2005;175(5):3244–51.
Feldmesser M, Tucker S, Casadevall A. Intracellular parasitism of macrophages by Cryptococcus neoformans. Trends Microbiol. 2001;9(6):273–8.
Kozel TR, Gotschlich EC. The capsule of cryptococcus neoformans passively inhibits phagocytosis of the yeast by macrophages. J Immunol. 1982;129(4):1675–80.
Ellerbroek PM, Ulfman LH, Hoepelman AI, Coenjaerts FE. Cryptococcal glucuronoxylomannan interferes with neutrophil rolling on the endothelium. Cell Microbiol. 2004;6(6):581–92.
Lipovsky MM, Gekker G, Hu S, Ehrlich LC, Hoepelman AI, Peterson PK. Cryptococcal glucuronoxylomannan induces interleukin (IL)-8 production by human microglia but inhibits neutrophil migration toward IL-8. J Infect Dis. 1998;177(1):260–3.
Almeida GM, Andrade RM, Bento CA. The capsular polysaccharides of Cryptococcus neoformans activate normal CD4(+) T cells in a dominant Th2 pattern. J Immunol. 2001;167(10):5845–51.
Lee SC, Casadevall A. Polysaccharide antigen in brain tissue of AIDS patients with cryptococcal meningitis. Clin Infect Dis. 1996;23(1):194–5.
Hirano A, Zimmerman HM, Levine S. The fine structure of cerebral fluid accumulation. Iii. Extracellular spread of cryptococcal polysaccharides in the acute stage. Am J Pathol. 1964;45:1–19.
Fries BC, Lee SC, Kennan R, Zhao W, Casadevall A, Goldman DL. Phenotypic switching of Cryptococcus neoformans can produce variants that elicit increased intracranial pressure in a rat model of cryptococcal meningoencephalitis. Infect Immun. 2005;73(3):1779–87.
Graybill JR, Sobel J, Saag M, van Der Horst C, Powderly W, Cloud G, et al. Diagnosis and management of increased intracranial pressure in patients with AIDS and cryptococcal meningitis. The NIAID Mycoses Study Group and AIDS Cooperative Treatment Groups. Clin Infect Dis. 2000;30(1):47–54.
Baker LG, Specht CA, Lodge JK. Cell wall chitosan is necessary for virulence in the opportunistic pathogen Cryptococcus neoformans. Eukaryot Cell. 2011;10(9):1264–8.
Fonseca FL, Nimrichter L, Cordero RJ, Frases S, Rodrigues J, Goldman DL, et al. Role for chitin and chitooligomers in the capsular architecture of Cryptococcus neoformans. Eukaryot Cell. 2009;8(10):1543–53.
Fonseca FL, Guimaraes AJ, Kmetzsch L, Dutra FF, Silva FD, Taborda CP, et al. Binding of the wheat germ lectin to Cryptococcus neoformans chitooligomers affects multiple mechanisms required for fungal pathogenesis. Fungal Genet Biol. 2013;60:64–73. This study implicates chitin as a virulence factor in CME.
Wiesner DL, Specht CA, Lee CK, Smith KD, Mukaremera L, Lee ST, et al. Chitin recognition via chitotriosidase promotes pathologic type-2 helper T cell responses to cryptococcal infection. PLoS Pathog. 2015;11(3):e1004701. Important study that implicates chitin-induced immune dysregulation in the pathogenesis of CME.
Almeida F, Wolf JM, Casadevall A. Virulence-associated enzymes of Cryptococcus neoformans. Eukaryotic Cell. 2015.
Zaragoza O, Nielsen K. Titan cells in Cryptococcus neoformans: cells with a giant impact. Curr Opin Microbiol. 2013;16(4):409–13.
Crabtree JN, Okagaki LH, Wiesner DL, Strain AK, Nielsen JN, Nielsen K. Titan cell production enhances the virulence of Cryptococcus neoformans. Infect Immun. 2012;80(11):3776–85.
Nicola AM, Robertson EJ, Albuquerque P, Derengowski Lda S, Casadevall A. Nonlytic exocytosis of Cryptococcus neoformans from macrophages occurs in vivo and is influenced by phagosomal pH. mBio. 2011; 2(4).
Alvarez M, Casadevall A. Phagosome extrusion and host-cell survival after Cryptococcus neoformans phagocytosis by macrophages. Curr Biol. 2006;16(21):2161–5.
Johnston SA, May RC. The human fungal pathogen Cryptococcus neoformans escapes macrophages by a phagosome emptying mechanism that is inhibited by Arp2/3 complex-mediated actin polymerisation. PLoS Pathog. 2010;6(8):e1001041.
Goldman DL, Fries BC, Franzot SP, Montella L, Casadevall A. Phenotypic switching in the human pathogenic fungus Cryptococcus neoformans is associated with changes in virulence and pulmonary inflammatory response in rodents. Proc Natl Acad Sci USA. 1998;95(25):14967–72.
Bouklas T, Pechuan X, Goldman DL, Edelman B, Bergman A, Fries BC. Old Cryptococcus neoformans cells contribute to virulence in chronic cryptococcosis. mBio. 2013; 4(4). Initial description of ageing in C. neoformans and its potential contribution to CME pathogenesis.
Bouklas T, Fries BC. Aging: an emergent phenotypic trait that contributes to the virulence of Cryptococcus neoformans. Future Microbiol. 2015;10(2):191–7. Reviews the contribution of ageing to CME.
Lee H, Chang YC, Nardone G, Kwon-Chung KJ. TUP1 disruption in Cryptococcus neoformans uncovers a peptide-mediated density-dependent growth phenomenon that mimics quorum sensing. Mol Microbiol. 2007;64(3):591–601.
Albuquerque P, Nicola AM, Nieves E, Paes HC, Williamson PR, Silva-Pereira I, et al. Quorum sensing-mediated, cell density-dependent regulation of growth and virulence in Cryptococcus neoformans. mBio. 2014;5(1):e00986–00913. Describes pantothenic acid-mediated quorum sensing in C. neformans and its potential role in disease.
Garcia-Hermoso D, Janbon G, Dromer F. Epidemiological evidence for dormant Cryptococcus neoformans infection. J Clin Microbiol. 1999;37(10):3204–9.
Haugen RK, Baker RD. The pulmonary lesions in cryptococcosis with special reference to subpleural nodules. Am J Clin Pathol. 1954;24(12):1381–90.
Saha DC, Goldman DL, Shao X, Casadevall A, Husain S, Limaye AP, et al. Serologic evidence for reactivation of cryptococcosis in solid-organ transplant recipients. Clin Vaccine Immunol. 2007;14(12):1550–4.
Goldman DL, Lee SC, Mednick AJ, Montella L, Casadevall A. Persistent Cryptococcus neoformans pulmonary infection in the rat is associated with intracellular parasitism, decreased inducible nitric oxide synthase expression, and altered antibody responsiveness to cryptococcal polysaccharide. Infect Immun. 2000;68(2):832–8.
Nosanchuk JD, Shoham S, Fries BC, Shapiro DS, Levitz SM, Casadevall A. Evidence of zoonotic transmission of Cryptococcus neoformans from a pet cockatoo to an immunocompromised patient. Ann Intern Med. 2000;132(3):205–8.
Charlier C, Nielsen K, Daou S, Brigitte M, Chretien F, Dromer F. Evidence of a role for monocytes in dissemination and brain invasion by Cryptococcus neoformans. Infect Immun. 2009;77(1):120–7.
Chang YC, Stins MF, McCaffery MJ, Miller GF, Pare DR, Dam T, et al. Cryptococcal yeast cells invade the central nervous system via transcellular penetration of the blood–brain barrier. Infect Immun. 2004;72(9):4985–95.
Vu K, Tham R, Uhrig JP, Thompson 3rd GR, Na Pombejra S, Jamklang M, et al. Invasion of the central nervous system by Cryptococcus neoformans requires a secreted fungal metalloprotease. mBio. 2014;5(3):e01101–14. Reports the discovey of a metalloprotease involved in the translocation of C. neoformans into the CNS.
Shi M, Li SS, Zheng C, Jones GJ, Kim KS, Zhou H, et al. Real-time imaging of trapping and urease-dependent transmigration of Cryptococcus neoformans in mouse brain. J Clin Invest. 2010;120(5):1683–93.
Jong A, Wu CH, Shackleford GM, Kwon-Chung KJ, Chang YC, Chen HM, et al. Involvement of human CD44 during Cryptococcus neoformans infection of brain microvascular endothelial cells. Cell Microbiol. 2008;10(6):1313–26.
Ibrahim AS, Filler SG, Alcouloumre MS, Kozel TR, Edwards Jr JE, Ghannoum MA. Adherence to and damage of endothelial cells by Cryptococcus neoformans in vitro: role of the capsule. Infect Immun. 1995;63(11):4368–74.
Chen SH, Stins MF, Huang SH, Chen YH, Kwon-Chung KJ, Chang Y, et al. Cryptococcus neoformans induces alterations in the cytoskeleton of human brain microvascular endothelial cells. J Med Microbiol. 2003;52(Pt 11):961–70.
Abadi J, Nachman S, Kressel AB, Pirofski L. Cryptococcosis in children with AIDS. Clin Infect Dis. 1999;28(2):309–13.
Goldman DL, Khine H, Abadi J, Lindenberg DJ, Pirofski L, Niang R, et al. Serologic evidence for Cryptococcus neoformans infection in early childhood. Pediatrics. 2001;107(5):E66.
Abadi J, Pirofski L. Antibodies reactive with the cryptococcal capsular polysaccharide glucuronoxylomannan are present in sera from children with and without human immunodeficiency virus infection. J Infect Dis. 1999;180(3):915–9.
Miglia KJ, Govender NP, Rossouw J, Meiring S, Mitchell TG. Analyses of pediatric isolates of Cryptococcus neoformans from South Africa. J Clin Microbiol. 2011;49(1):307–14.
Iseki M, Anzo M, Yamashita N, Matsuo N. Hyper-IgM immunodeficiency with disseminated cryptococcosis. Acta Paediatr. 1994;83(7):780–2.
Jacobs DH, Macher AM, Handler R, Bennett JE, Collen MJ, Gallin JI. Esophageal cryptococcosis in a patient with the hyperimmunoglobulin E-recurrent infection (Job’s) syndrome. Gastroenterology. 1984;87(1):201–3.
Wahab JA, Hanifah MJ, Choo KE. Bruton’s agammaglobulinaemia in a child presenting with cryptococcal empyema thoracis and periauricular pyogenic abscess. Singap Med J. 1995;36(6):686–9.
Liou J, Chiu C, Tseng C, Chi C, Fu L. Cryptococcal meningitis in pediatric systemic lupus erythematosus. Mycoses. 2003;46(3–4):153–6.
Leggiadro RJ, Barrett FF, Hughes WT. Extrapulmonary cryptococcosis in immunocompromised infants and children. Pediatr Infect Dis J. 1992;11(1):43–7.
Sweeney DA, Caserta MT, Korones DN, Casadevall A, Goldman DL. A ten-year-old boy with a pulmonary nodule secondary to Cryptococcus neoformans: case report and review of the literature. Pediatr Infect Dis J. 2003;22(12):1089–93.
Hage CA, Wood KL, Winer-Muram HT, Wilson SJ, Sarosi G, Knox KS. Pulmonary cryptococcosis after initiation of anti-tumor necrosis factor-alpha therapy. Chest. 2003;124(6):2395–7.
Meletiadis J, Walsh TJ, Choi EH, Pappas PG, Ennis D, Douglas J, et al. Study of common functional genetic polymorphisms of FCGR2A, 3A and 3B genes and the risk for cryptococcosis in HIV-uninfected patients. Med Mycol. 2007;45(6):513–8.
Rohatgi S, Gohil S, Kuniholm MH, Schultz H, Dufaud C, Armour KL, et al. Fc gamma receptor 3A polymorphism and risk for HIV-associated cryptococcal disease. mBio. 2013;4(5):e00573–00513. Study that implicates Fc polymorphisms as a contributing risk factor for CME in HIV-infected patients.
Joshi NS, Fisher BT, Prasad PA, Zaoutis TE. Epidemiology of cryptococcal infection in hospitalized children. Pediatr Infect Dis J. 2010;29(12):e91–5.
Severo CB, Xavier MO, Gazzoni AF, Severo LC. Cryptococcosis in children. Paediatr Respir Rev. 2009;10(4):166–71.
Meiring ST, Quan VC, Cohen C, Dawood H, Karstaedt AS, McCarthy KM, et al. A comparison of paediatric- and adult-onset cryptococcosis detected through population-based surveillance in South Africa, 2005–2007. AIDS 2012.
Lizarazo J, Escandon P, Agudelo CI, Castaneda E. Cryptococcosis in Colombian children and literature review. Mem Inst Oswaldo Cruz. 2014;109(6):797–804. Most recent description of pediatric cryptoccosis. Compares the Colombian experience with earlier pediatric reports.
Huang KY, Huang YC, Hung IJ, Lin TY. Cryptococcosis in nonhuman immunodeficiency virus-infected children. Pediatr Neurol. 2010;42(4):267–70.
Yuanjie Z, Jianghan C, Nan X, Xiaojun W, Hai W, Wanqing L, et al. Cryptococcal meningitis in immunocompetent children. Mycoses. 2012;55(2):168–71.
Gumbo T, Kadzirange G, Mielke J, Gangaidzo IT, Hakim JG. Cryptococcus neoformans meningoencephalitis in African children with acquired immunodeficiency syndrome. Pediatr Infect Dis J. 2002;21(1):54–6.
Mullan PC, Steenhoff AP, Draper H, Wedin T, Bafana M, Anabwani G, et al. Etiology of meningitis among patients admitted to a tertiary referral hospital in Botswana. Pediatr Infect Dis J. 2011;30(7):620–2.
Owusu M, Nguah SB, Boaitey YA, Badu-Boateng E, Abubakr AR, Lartey RA, et al. Aetiological agents of cerebrospinal meningitis: a retrospective study from a teaching hospital in Ghana. Ann Clin Microbiol Antimicrob. 2012;11:28.
Patel M, Beckerman KP, Reznik S, Madan RP, Goldman DL. Transplacental transmission of Cryptococcus neoformans to an HIV-exposed premature neonate. J Perinatol. 2012;32(3):235–7.
Likasitwattanakul S, Poneprasert B, Sirisanthana V. Cryptococcosis in HIV-infected children. Southeast Asian J Trop Med Public Health. 2004;35(4):935–9.
Gonzalez CE, Shetty D, Lewis LL, Mueller BU, Pizzo PA, Walsh TJ. Cryptococcosis in human immunodeficiency virus-infected children. Pediatr Infect Dis J. 1996;15(9):796–800.
Hansen J, Slechta ES, Gates-Hollingsworth MA, Neary B, Barker AP, Bauman S, et al. Large-scale evaluation of the immuno-mycologics lateral flow and enzyme-linked immunoassays for detection of cryptococcal antigen in serum and cerebrospinal fluid. Clin Vaccine Immunol. 2013;20(1):52–5. Large study that confirms the high sensitivity and specificity of LFA testing on serum and CSF in the diagnosis of CME.
Huang HR, Fan LC, Rajbanshi B, Xu JF. Evaluation of a new cryptococcal antigen lateral flow immunoassay in serum, cerebrospinal fluid and urine for the diagnosis of cryptococcosis: a meta-analysis and systematic review. PLoS One. 2015;10(5):e0127117. A meta-analysis that indicates high accuracy of serum and CSF LFA testing in CME diagnosis. Also reviews data on urine testing.
Kabanda T, Siedner MJ, Klausner JD, Muzoora C, Boulware DR. Point-of-care diagnosis and prognostication of cryptococcal meningitis with the cryptococcal antigen lateral flow assay on cerebrospinal fluid. Clin Infect Dis. 2014;58(1):113–6. Reports a correlation between high CSF LFA titers with both CSF fungal burden and mortality.
Lourens A, Jarvis JN, Meintjes G, Samuel CM. Rapid diagnosis of cryptococcal meningitis by use of lateral flow assay on cerebrospinal fluid samples: influence of the high-dose “hook” effect. J Clin Microbiol. 2014;52(12):4172–5. Details the importance of specimen dilution in LFA testing to avoid false negatives associated with antigen excess.
Perfect JR, Dismukes WE, Dromer F, Goldman DL, Graybill JR, Hamill RJ, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the infectious diseases society of america. Clin Infect Dis. 2010;50(3):291–322.
van der Horst CM, Saag MS, Cloud GA, Hamill RJ, Graybill JR, Sobel JD, et al. Treatment of cryptococcal meningitis associated with the acquired immunodeficiency syndrome. National Institute of Allergy and Infectious Diseases Mycoses Study Group and AIDS Clinical Trials Group. N Engl J Med. 1997;337(1):15–21.
Dromer F, Bernede-Bauduin C, Guillemot D, Lortholary O. Major role for amphotericin B-flucytosine combination in severe cryptococcosis. PLoS ONE. 2008;3(8):e2870.
Bennett JE, Dismukes WE, Duma RJ, Medoff G, Sande MA, Gallis H, et al. A comparison of amphotericin B alone and combined with flucytosine in the treatment of cryptoccal meningitis. N Engl J Med. 1979;301(3):126–31.
Day JN, Chau TT, Lalloo DG. Combination antifungal therapy for cryptococcal meningitis. N Engl J Med. 2013;368(26):2522–3. A recent randomized control study that highligts the importances of combined amphotericin-5FC therapy in the initial treatement of CME.
Loyse A, Dromer F, Day J, Lortholary O, Harrison TS. Flucytosine and cryptococcosis: time to urgently address the worldwide accessibility of a 50-year-old antifungal. J Antimicrob Chemother. 2013;68(11):2435–44. A review of importance of 5-FC in the treatment of CME.
Nussbaum JC, Jackson A, Namarika D, Phulusa J, Kenala J, Kanyemba C, et al. Combination flucytosine and high-dose fluconazole compared with fluconazole monotherapy for the treatment of cryptococcal meningitis: a randomized trial in Malawi. Clin Infect Dis. 2010;50(3):338–44.
Jackson AT, Nussbaum JC, Phulusa J, Namarika D, Chikasema M, Kanyemba C, et al. A phase II randomized controlled trial adding oral flucytosine to high-dose fluconazole, with short-course amphotericin B, for cryptococcal meningitis. AIDS. 2012;26(11):1363–70.
Molefi M, Chofle AA, Molloy SF, Kalluvya S, Changalucha JM, Cainelli F, et al. AMBITION-cm: intermittent high dose Am Bisome on a high dose fluconazole backbone for cryptococcal meningitis induction therapy in sub-Saharan Africa: study protocol for a randomized controlled trial. Trials. 2015;16:276. A description of the pending tiral to examine the utility of short course of ambisome in conjuction with high dose fluconazole in the intial treatment of CME.
Bava AJ, Afeltra J, Negroni R, Diez RA. Interferon gamma increases survival in murine experimental cryptococcosis. Rev Inst Med Trop Sao Paulo. 1995;37(5):391–6.
Joly V, Saint-Julien L, Carbon C, Yeni P. In vivo activity of interferon-gamma in combination with amphotericin B in the treatment of experimental cryptococcosis. J Infect Dis. 1994;170(5):1331–4.
Jarvis JN, Meintjes G, Rebe K, Williams GN, Bicanic T, Williams A, et al. Adjunctive interferon-gamma immunotherapy for the treatment of HIV-associated cryptococcal meningitis: a randomized controlled trial. AIDS. 2012;26(9):1105–13.
Pappas PG, Bustamante B, Ticona E, Hamill RJ, Johnson PC, Reboli A, et al. Recombinant interferon- gamma 1b as adjunctive therapy for AIDS-related acute cryptococcal meningitis. J Infect Dis. 2004;189(12):2185–91.
Perfect JR, Granger DL, Durack DT. Effects of antifungal agents and gamma interferon on macrophage cytotoxicity for fungi and tumor cells. J Infect Dis. 1987;156(2):316–23.
Bicanic T, Meintjes G, Wood R, Hayes M, Rebe K, Bekker LG, et al. Fungal burden, early fungicidal activity, and outcome in cryptococcal meningitis in antiretroviral-naive or antiretroviral-experienced patients treated with amphotericin B or fluconazole. Clin Infect Dis. 2007;45(1):76–80.
Brizendine KD, Baddley JW, Pappas PG. Predictors of mortality and differences in clinical features among patients with Cryptococcosis according to immune status. PLoS One. 2013;8(3):e60431. A study that identifies cryptococcemia and increased ICP as risk factors for death in CME.
Guo J, Zhou J, Zhang S, Zhang X, Li J, Sun Y, et al. A case–control study of risk factors for HIV-negative children with cryptococcal meningitis in Shi Jiazhuang, China. BMC Infect Dis. 2012;12:376.
Denning DW, Armstrong RW, Lewis BH, Stevens DA. Elevated cerebrospinal fluid pressures in patients with cryptococcal meningitis and acquired immunodeficiency syndrome. Am J Med. 1991;91(3):267–72.
Hussey F, Schanzer B, Katzman R. A simple constant-infusion manometric test for measurement of CSF absorption. II. Clinical studies. Neurology. 1970;20(7):665–80.
Rolfes MA, Hullsiek KH, Rhein J, Nabeta HW, Taseera K, Schutz C, et al. The effect of therapeutic lumbar punctures on acute mortality from cryptococcal meningitis. Clin Infect Dis. 2014;59(11):1607–14. A study that highlights the importance of therapeutic lumbar puncture in reducing the mortality of CME.
Beardsley J, Wolbers M, Kibengo FM, Ggayi AB, Kamali A, Cuc NT, et al. Adjunctive dexamethasone in HIV-associated cryptococcal meningitis. N Engl J Med. 2016;374(6):542–54. Large, double blinded, controlled study documenting increased adverse effects associated with corticosteroid use in CME among HIV-infected indviduals.
Franco-Paredes C, Womack T, Bohlmeyer T, Sellers B, Hays A, Patel K, et al. Management of Cryptococcus gattii meningoencephalitis. Lancet Infect Dis. 2015;15(3):348–55. A review that includes a discussion on the management of increased ICP (including the use of corticosteroids) in patients with CME secondary to C. gattii.
Seaton RA, Verma N, Naraqi S, Wembri JP, Warrell DA. The effect of corticosteroids on visual loss in Cryptococcus neoformans var. gattii meningitis. Trans R Soc Trop Med Hyg. 1997;91(1):50–2.
Meya DB, Okurut S, Zziwa G, Rolfes MA, Kelsey M, Cose S, et al. Cellular immune activation in cerebrospinal fluid from ugandans with cryptococcal meningitis and immune reconstitution inflammatory syndrome. J Infect Dis. 2015;211(10):1597–606. Identifies the presence of CD4+ T cells and monocytes in the CSF as a risk factor for CME- associated IRIS.
Hashimoto H, Hatakeyama S, Yotsuyanagi H. Development of cryptococcal immune reconstitution inflammatory syndrome 41 months after the initiation of antiretroviral therapy in an AIDS patient. AIDS Res Ther. 2015;12:33. A report describing a delayed presentatiion of IRIS-associated CME.
Hassan H, Cotton MF, Rabie H. Complicated and protracted cryptococcal disease in HIV-infected children. Pediatr Infect Dis J. 2015;34(1):62–5. A small series of pediatric CME cases that highlights the potential contribution of IRIS to protracted cryptococcal disease.
Zolopa A, Andersen J, Powderly W, Sanchez A, Sanne I, Suckow C, et al. Early antiretroviral therapy reduces AIDS progression/death in individuals with acute opportunistic infections: a multicenter randomized strategy trial. PLoS One. 2009;4(5):e5575.
Bisson GP, Molefi M, Bellamy S, Thakur R, Steenhoff A, Tamuhla N, et al. Early versus delayed antiretroviral therapy and cerebrospinal fluid fungal clearance in adults with HIV and cryptococcal meningitis. Clin Infect Dis. 2013;56(8):1165–73. Study that suggest that early ART does not result in early CSF clearance but may increase the risk of IRIS.
Boulware DR, Meya DB, Muzoora C, Rolfes MA, Huppler Hullsiek K, Musubire A, et al. Timing of antiretroviral therapy after diagnosis of cryptococcal meningitis. N Engl J Med. 2014;370(26):2487–98. A recent report that describes significant increase in mortality associated with early ART in CME, espcially for those with low initial CSF white blood cell counts.
Scriven JE, Rhein J, Hullsiek KH, von Hohenberg M, Linder G, Rolfes MA, et al. Early ART after cryptococcal meningitis is associated with cerebrospinal fluid pleocytosis and macrophage activation in a multisite randomized trial. J Infect Dis. 2015;212(5):769–78. A characterization of the cellular response of the CSF in patients with CME that finds evidence for inappropriate macrophage activation in pateints with IRIS.
Chang CC, Lim A, Omarjee S, Levitz SM, Gosnell BI, Spelman T, et al. Cryptococcosis-IRIS is associated with lower cryptococcus-specific IFN-gamma responses before antiretroviral therapy but not higher T-cell responses during therapy. J Infect Dis. 2013;208(6):898–906. A study that reports low cryptococal specfic T-cells prior to ART therapy as a risk factor for the development of IRIS.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Drs Kao and Goldman declare no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain studies with human or animal subjects performed by the author.
Additional information
This article is part of the Topical Collection on Pediatric Infectious Diseases
Rights and permissions
About this article
Cite this article
Kao, C., Goldman, D.L. Cryptococcal Disease in HIV-Infected Children. Curr Infect Dis Rep 18, 27 (2016). https://doi.org/10.1007/s11908-016-0534-9
Published:
DOI: https://doi.org/10.1007/s11908-016-0534-9