Abstract
Purpose of Review
Atherosclerosis is a chronic disease characterized by lipid retention and inflammation in the artery wall. The retention and oxidation of low-density lipoprotein (LDL) in sub-endothelial space play a critical role in atherosclerotic plaque formation and destabilization. Oxidized LDL (ox-LDL) and other modified LDL particles are avidly taken up by endothelial cells, smooth muscle cells, and macrophages mainly through several scavenger receptors, including CD36 which is a class B scavenger receptor and membrane glycoprotein.
Recent Findings
Animal studies performed on CD36-deficient mice suggest that deficiency of CD36 prevents the development of atherosclerosis, though with some debate. CD36 serves as a signaling hub protein at the crossroad of inflammation, lipid metabolism, and fatty acid metabolism. In addition, the level of soluble CD36 (unattached to cells) in the circulating blood was elevated in patients with atherosclerosis and other metabolic disorders.
Summary
We performed a state-of-the-art review on the structure, ligands, functions, and regulation of CD36 in the context of atherosclerosis by focusing on the pathological role of CD36 in the dysfunction of endothelial cells, smooth muscle cells, monocytes/macrophages, and platelets. Finally, we highlight therapeutic possibilities to target CD36 expression/activity in atherosclerosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular diseases (CVD) represent the main cause of death worldwide and are often caused by atherosclerosis [1]. Atherosclerosis is a progressive inflammatory and lipid disorder, which commences with proteoglycan-mediated uptake of low-density lipoprotein (LDL) that progress with endothelial dysfunction and subsequent activation of a cascade of cellular events that result in high inflammation [2]. Circulating monocytes adhere and transmigrate through injured endothelium and eventually differentiate into macrophages [3•, 4••]. The differentiated macrophages generate reactive oxygen species (ROS) acting on vascular smooth muscle cells (VSMCs) to induce proliferation, migration, and production of extracellular matrix (ECM) proteins [3•]. Macrophages and VSMCs express multiple scavenger receptors ingesting ox-LDL, originating from oxidative modification LDL in the subendothelial space of vessel wall, and become foam cells, which contribute to the formation of atherosclerotic plaques [3•, 4••]. With the silent progression and destabilization of atherosclerotic plaques, the clinical symptoms and acute cardiovascular events are likely to occur.
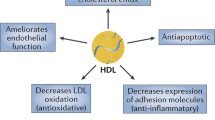
It has been well established that ox-LDL uptake by scavenger receptors could lead to macrophage-derived foam cell formation and atherosclerosis [5, 6]. CD36, a major class B scavenger receptor, exerts substantial effects on ox-LDL uptake by macrophages [7]. Cumulative data have indicated the important role of CD36 in regulating key physiological processes and cellular events in the initial and progression phases of atherosclerosis, such as inflammation, lipid metabolism, endothelial dysfunction, smooth muscle cell dysfunction, and foam cell formation [8]. In the present review, we elaborate on the current knowledge as to the structure, ligands, biological functions, and modulators of CD36. Moreover, we highlight targeted anti-atherosclerotic therapies directed against CD36.
The Structure and Ligands of CD36
The Structure of CD36
CD36 is an 88-kDa transmembrane glycoprotein receptor that belongs to the class B scavenger receptor family [9]. CD36 gene is located on chromosome 7 (7q11.2) and encompasses 17 exons and 18 introns. CD36 is comprised of 472 amino acids and folded into a single peptide chain, with two transmembrane domains, two very short cytoplasmic domains, and a large glycosylated extracellular domain with hairpin-like membrane topology [10]. Further research is needed to be done to confirm the association of structural alternations of CD36, plasma membrane trafficking, and ligand binding capacity, with the occurrence of cardiometabolic diseases [11].
The Ligands of CD36
The extracellular domain of CD36 has several binding sites that confer the ability to recognize a variety of endogenous and exogenous ligands, which can be mainly classified into four categories: (1) long-chain FAs, (2) pathogen-associated molecules, (3) endogenous danger molecules, and (4) molecules that contain the thrombospondin-1 (TSP-1) structural homology region [12]. Upon binding to ligands, CD36 can be involved in a variety of biological processes such as innate immunity regulation, angiogenesis, thrombosis, inflammation, and atherosclerosis, but the detailed mechanisms are incompletely established. TSP-1 binds to the CLESH-1 domain that is located at amino acids 93 ~ 155 of CD36. Additionally, the binding site of oxPL and ox-LDL resides in regions of amino acids (157–171) and (155–183), respectively [13]. Moreover, many structurally distinct FAs (saturated, monounsaturated (cis and trans), polyunsaturated, and oxidized) can bind to the ectodomain Lys-164 of CD36, promoting the uptake of ox-LDL [14, 15]. Intriguingly, the binding sites for different ligands were not specific, as evidenced by different ligands sharing the same binding sites. For instance, the FA-binding site (amino 127–279) on CD36 overlaps that of ox-LDL and oxidized phosphatidylcholine (amino 157–171) [16] (Fig. 1).
Regulation of CD36 Expression
Transcription Factors
Many transcription factors are implicated in the regulation of CD36, which mediates excessive ox-LDL uptake, thus promoting the initiation and progression of atherosclerosis. Peroxisome proliferator-activated receptor γ (PPARγ) represents a primary transcription factor that binds to the promoter region of CD36 and modulates CD36 in a positive feedback manner [17]. Activation of PPARγ by its agonist, 1-O-alkyl glycerophosphate (AGP), promotes the expression of CD36 and CD36-mediated ox-LDL uptake in microglial cells [18]. Additionally, protein kinase Cθ-dependent ATF2 activation was required for thrombin-elicited CD36-dependent ox-LDL uptake [19]. Recent data showed that STAT5 activated PPARγ through inhibition of the 3′-untranslated region of CD36 [20]. In addition, pregnane X receptor (PXR) increased CD36 expression concomitant with lipid accumulation in macrophages. However, depletion of myeloid PXR diminished the risk of atherosclerosis, most likely by suppressing CD-36-mediated ox-LDL uptake [21]. Other transcription factors such as RCAN1 [22], AdipoR2 [23], and IRGM/IRMG1 [24] are also involved in the regulation of CD36 function and suppression of ox-LDL uptake, which can eventually contribute to reduced risk and severity of atherosclerosis. A more recent study has shown that inhibitors of the janus tyrosine kinase (JAK)-STAT pathway (ruxolitinib and tofacitinib) suppressed the uptake of Ac-LDL and the expression of both CD36 and CD204 in LPS-activated macrophages [25]. Hence, modulation of these transcription factors might serve as a potential therapeutic target for atherosclerosis.
miRNA
In addition to transcription factors, post-transcriptional regulation by miRNAs is also involved in the modulation of CD36 expression and function. Ample evidence indicates that CD36 can be post-transcriptionally regulated by different miRNAs in a tissue-specific manner. During bone marrow cell differentiation, CD36 expression is associated with changes in miRNA expression profile [26], suggesting that miRNAs might be linked to CD36 function with respect to the macrophage activation. In fact, the interaction between miRNA and CD36 is closely associated with lipid metabolic disorders. In the diabetes populations and experimental diabetic models, miR-320 translocates into the nucleus, subsequently activating CD36, which contributes to increased uptake of FA that can lead to myocardial lipotoxicity [27]. Furthermore, obese individuals also exhibited an altered miRNA expression profile, which might be related to CD36-dependent macrophage cholesterol efflux [28]. Further direct evidence confirmed miRNA directly impacts CD36 function. miR-181a overexpression can reverse the ox-LDL-induced upregulation of CD36 in THP-1 macrophage and the formation of foam cells [29]. In line with the above results, miR-758-5p overexpression also diminished CD36 expression by targeting the CD36 3′-UTR concomitant with the improved lipid metabolism in macrophages [30]. Although the current results indicated that miRNAs can influence the expression of CD36, precision role of CD36 in miRNA-regulated atherosclerosis needs further investigation.
LncRNA
CD36 can also be regulated by long noncoding RNAs (LncRNA), which serve as important regulators in the pathological processes of cardiovascular disease. LncRNA MALAT1, an abundantly expressed lncRNA in THP-1 cells, was correlated with β-catenin-dependent CD36 expression and CD36-mediated lipid uptake by macrophages, partially though suppressing β-catenin binding to the CD36 promoter [31]. It remains to be investigated whether MALAT1 regulated CD36 through changing the nucleosome organization of CD36. Silencing the lncRNA NEAT1 also inhibited CD36 expression and lipid uptake. However, overexpression of NEAT1 showed opposite effects in RAW264.7 cells [32]. Moreover, overexpression of lncRNA E330013P06 induced CD36 upregulation, contributing to atherogenic phenotype in macrophages isolated from diabetic mice [33]. Co-expression network analysis showed co-expressed lncRNAs n382000 and n341587 had a high correlation coefficient with CD36 mRNA expression in patients with type II diabetes [34]. Notably, ultraconserved RNAs, a novel conserved class of lncRNAs, were identified to regulate CD36-related lipogenesis genes through interaction with pri-miR-195/pri-miR-4668 in macrophages [35]. A more recent study has shown that PELATON, a novel lncRNA enriched in unstable atherosclerotic plaques, was also involved in the regulation of CD36 expression. Silencing of PELATON markedly diminished phagocytosis, lipid uptake, and the expression of CD36 in macrophages. Considering CD36 is a key mediator of phagocytosis of lipoproteins, it is plausible that PELATON may regulate the progression of atherosclerotic plaques though the modulation of CD36-mediated ox-LDL phagocytosis [36].
DNA Methylation
DNA methylation can epigenetically regulate gene expression via hypermethylation of CpG islands in promoter regions. Several promoter sequences and distal cis-regulatory elements of the human CD36 gene contain a number of CpG methylation sites. Currently, genome-wide or epigenome-wide studies in metabolic disorders indicated that CD36 DNA was less methylated in obesity population compared with the normal BMI subjects [37]. Furthermore, the CD36 SNPs variants were associated with CD36 expression due to the methylation of CD36, indicating that SNPs and methylation appear to regulate CD36 mRNA expression [38].
In obese patients, significant downregulation of CD36 methylation level was observed, especially the triglyceride-associated CpG in a regulatory region of CD36, therefore impacts the CD36 level and expression of CD36 variants [39]. Identifying the active regulatory regions for atherosclerosis-associated DNA methylation sites could be an effective method to identify traits-associated methylation changes in the research field of atherosclerosis.
Histone Modification
Cumulative evidence has indicated that histone modification affects CD36 expression in various cell types under distinct pathological conditions. Long-term exposure to ox-LDL induced histone trimethylation at CD36 promoters and induced CD36 expression and proinflammatory phenotype in monocytes, while the phenotype was abolished by histone methyltransferase inhibitor [40]. In addition, H3K4me3 modification at the CD36 promoter affected hematopoietic stem cell differentiation [41].
It has been reported that HDAC inhibitor, trichostatin A, promotes the acetylation status of H4 at the CD36 promoter and increased CD36 expression, followed by excessive uptake of ox-LDL into the macrophages, and exacerbated atherosclerosis [42]. In contrast, CD36 expression also was decreased by HDAC inhibitor, MPT0E014 [43]. Additionally, transcriptional repression of CD36 was induced by lysophosphatidic acid though inhibition of HDAC7 translocation to nucleus in microvascular endothelial cells [44]. It warrants further evaluation whether individual HDAC isoform elicits a differential effect on CD36 expression and downstream atherosclerotic events.
Autophagy-Lysosome-Dependent and Ubiquitin-Proteasome Degradation
Autophagy, a biological process that degrades and recycles organelles, exerts a key role in maintaining the balanced energy in response to nutrient stress. Autophagy modulates cholesterol mobilization from macrophage to reverse cholesterol transport, which is deregulated in advanced atherosclerosis. Previous studies have shown that macrophage-specific deletion of ATG5 leads to proatherogenic inflammasome activation in macrophages, thus contributing to the consecutive infiltration of macrophages and destabilization of atherosclerotic plaques [45]. Therefore, maintaining the appropriate activation of autophagy might be a beneficial strategy for the treatment of atherosclerosis. It has been recently shown that SGLT2 inhibitor empagliflozin administration ameliorated cardiac lipotoxicity, activated energy sensor AMPK, and induced autophagy in experimental diabetic models. Importantly, CD36 expression was also decreased due to the activation of autophagy upon empagliflozin treatment [46]. Recent results demonstrated the existence of crosstalk between autophagy and CD36 [47]. It remains to be evaluated how the crosstalk operates and whether the correlation between autophagy and CD36 is linked to the pathogenesis of atherosclerosis. Moreover, exogenous addition of CTRP13 activated autophagy-lysosomal system and inhibited CD36 expression, and foam cell formation. Importantly, the authors found that autophagy-lysosomal system mediated CD36 degradation, suppressed macrophage lipid uptake and retention; this mechanism was implicated in the beneficial effects of CTRP13 in atherosclerosis [48]. Notably, ubiquitin-proteasome system, another protein degradation system, was also implicated in the regulation of CD36 and generated beneficial effects under atherosclerotic condition. The ingestion of ox-LDL was inhibited by ubiquitin-proteasome system via promoting CD36 degradation [49]. In conclusion, manipulation of intracellular protein degradation though pharmacological and genetic approaches might present a valuable therapeutic strategy for atherosclerosis treatment.
CD36-Mediated Signal Transduction
Although CD36 lacks well-characterized intracellular signaling domains such as kinase, phosphatase, or G protein binding domains, it can function as a signaling hub molecule through interacting with many membrane-localized receptors. For example, CD36 can transduce src family non-receptor tyrosine kinases, JNK, ERK 1/2, IRGM1 and TLR2/6-dependent signaling [8]. Upon CD36 binding to various types of ligands, the Src family kinase initiates the CD36-mediated intracellular signaling, which is implicated in angiogenesis, inflammation, and atherosclerosis [16]. The binding of CD36 to TSP-1 promotes the Src homology 2 domain–containing protein tyrosine phosphatase-1 (SHP-1) to form a complex with vascular endothelial growth factor receptor 2 (VEGFR2). Then, the formation of SHP-1/VEGFR2 complex dephosphorylates VEGFR2, leading to anti-angiogenesis effects in microvascular endothelial cells [50]. In addition, lysophosphatidic acid interacts with protein kinase D1 and leads to HDAC7/FoxO1 interaction that inhibits CD36 transcription in microvascular endothelial cells, thereby contributing to proangiogenic and proarteriogenic reprogramming [44].
The hyperlipidemic environment in the plasma and atherosclerotic plaques also fosters clinically manifested thrombotic events. In the platelets, the binding of ox-LDL to CD36 initiated protein kinase C-dependent NOX-2 activation and excessive ROS generation in blood platelets through inhibition of cGMP signaling [51]. In addition, damaged mitochondria could generate ROS due to the impaired ROS clearing mechanisms. Interestingly, increased CD36 expression leads to mitochondrial ROS overproduction in aortic lesion macrophages upon stimulation of pro-atherogenic ox-LDL, which could switch the mitochondrial metabolism to superoxide production. However, inhibition of mitochondria-derived superoxide generation suppresses ox-LDL induced NF-kB activation and pro-inflammatory cytokine production [52••]. These findings suggest the therapeutic possibility to treat chronic inflammation and atherosclerosis by targeting oxidized LDL/CD36 signaling in macrophages via modulating dysregulated fatty acid metabolism and mitochondria ROS production [52••]. Foam cell formation is the hallmark in atherosclerotic plaque formation and progression, which is also mediated by CD36-related signaling. Wnt5a enhanced CD36 expression and lipid deposition, eventually leading to increased foam cell formation [53]. SNX10 deficiency reduced the interactions between CD36 and Lyn, thus inhibiting CD36-mediated lipoprotein uptake and foam cell formation [54]. Therefore, uncovering CD36-related signaling pathways and elucidating their specific mechanisms would help identify potential targets for therapeutic intervention in atherosclerosis.
Molecular Mechanisms of CD36 in Atherosclerosis
CD36 and Endothelial Dysfunction
The trans-endothelial transport of LDL to the subendothelial space, where LDL is oxidized, is an initiating event in atherosclerosis. Recent single-cell transcriptome analyses have revealed that endothelial cells are one main cell population of the aorta. CD36 is extensively expressed on the surface of endothelial cells throughout the aorta [55]. Notably, CD36 expression was increased upon simulation with ox-LDL or high-fat diet feeding, which promoted aortic uptake of ox-LDL or other modified lipids. In contrast, CD36-mediated ox-LDL uptake was attenuated in CD36−/− mice. Consistently, there was a decreased lipid and arterial stiffness in CD36−/− mice compared with wild-type mice fed with high-fat diet [56, 57]. Importantly, CD36-mediated endocytosis of LDL into rat aorta or coronary artery is a crucial mechanism in atherogenesis [58]. Moreover, endothelial cell specific CD36 knockout mice showed diminished long-chain FA transfer across endothelial cells, improved glucose tolerance, and decreased lipid deposition in the heart [59]. This phenomenon is most likely due to the fact that CD36-mediated uptake of ox-LDL is FA-dependent. Importantly, CD36 can take up FAs through enhancing the rate of intracellular esterification [60••]. Therefore, FAs bind to CD36 and enhance CD36-mediated ox-LDL uptake, and finally contribute to atherosclerosis.
CD36 and Vascular Smooth Muscle Cell (VSMC) Dysfunction
VSMCs, another major cell population in the arterial wall, are essential for maintaining vascular tone. Aberrant changes in VSMC behavior, function and antioxidant status contribute to atherosclerotic plaque progression. CD36 is expressed on VSMCs and is associated with disturbed lipid metabolism and deregulated immune response of the arterial wall in response to ox-LDL [60••]. CD36 functions as a pattern recognition receptor in innate immunity. Ox-LDL-induced G-CSF and GM-CSF expression and increased migration capacity of VSMCs were reversed by CD36 siRNA in primarily cultured VSMCs [61]. Previous studies have revealed that obstructive vessels highly expressed CD36. VMSCs proliferate and migrate from media to intima and cause the thickening of the arterial wall (neointima formation), which is a strong risk factor for thrombogenesis. Both global or VSMC-specific CD36−/− mice had significantly reduced neointimal thickening [62]. In agreement with the in vivo results, cultured VSMCs isolated from thoracic aorta of CD36−/− mice failed to proliferate, and this phenotype might be mediated by inhibited cyclin A expression [62]. Collectively, targeting CD36 in vasculature represents a potentially promising therapeutic target for vascular damage and other vascular disorders.
The Role of CD36 in Macrophage Dysfunction
Under dyslipidemia scenario, LDL particles accumulation in the subendothelial space is subject to oxidative modification, which then triggers the transmigration and differentiation of monocytes. Ox-LDL can induce CD36 expression though PPARγ, which in turn promotes ox-LDL uptake by the macrophages and entrapment of macrophages within the plaques, allowing for macrophages to become lipid-laden foam cells [9]. Intracellular ROS is a main contributor to the pro-atherogenic effect of CD36. Unexpectedly, inhibition of NADPH oxidase failed to completely block the pro-atherogenic effects of CD36 [63], which implies that there are other key modulators associated with the pro-atherogenic effect of CD36. Interestingly, mitochondria, the main source of ROS, could serve as the downstream effector of the ox-LDL/CD36 axis. CD36 also regulated ROS generation and impacted inflammatory status though mitochondria pathway. Mechanistically, macrophages from CD36−/− mice exhibited increased oxidative phosphorylation upon ox-LDL treatment, displaying a probable M1 macrophage phenotype, while wild-type macrophages switched to glycolysis [52••]. The above results indicated that mitochondrial metabolic reprogramming was closely associated with the CD36-mediated effects.
Impaired migration of macrophages fosters macrophage trapping in the subendothelial space. Ox-LDL inhibited the mobile capacity and actin polymerization, which was blocked in CD36-deficient cells. Further data revealed that CD36 regulated the migration of macrophages via NADPH oxidase-dependent ROS generation, resulting in inactivation of SHP-2 and FAK activation [63]. This research provided insight into ox-LDL-induced macrophage trapping under athero-inflammatory lesions. Intriguingly, treatment with a CD36 ligand EP80317 (300 μg/kg) leads to reduced recruitment of macrophages to atherosclerotic lesions in ApoE−/− mice, which was prevented in CD36−/− mice, suggesting that this ligand may decrease oxLDL binding to CD36 in a competitive manner [64]. Additionally, CD36 could regulate the cell polarization that commonly termed M1 macrophages to M2 macrophages. This process is a prerequisite step that empowers the migrative capacity of macrophages. Ox-LDL incubation resulted in the retraction of macrophage front end lamellipodia concomitant with impaired cell polarity [65]. Of note, the M2 macrophage activation requires FA oxidation to support the loss of macrophage polarization. Interestingly, CD36 takes up the triacylglycerol substrates, producing enough FA to fuel the polarity loss [66]. Importantly, testicular orphan nuclear receptor 4 (TR4) can sensor the increased generation of FA and promote the expression of CD36, which forms a vicious cycle that finally contributes to the formation of form cells [67]. CD36 is recently shown to be involved in oxLDL-induced secretion of vimentin and the release of pro-inflammatory cytokines (such as TNF-α and IL-6) in activated macrophages [68]. The finding provides a novel mechanistic explanation for trapping macrophages within atherosclerotic plaque. Taken together, these studies support the notion that inhibition of CD36 prevents macrophage polarization, migration and contributes to atherosclerosis prevention.
CD36 and Platelet Activation
Chronic vascular injury occurs throughout the lifetime of a human but remains silent until a plaque develops high inflammation in the endothelium and fibrous cap with ensuing rupture. When this acute injury occurs, platelets are recruited and attached to the endothelial surface of injury sites. Then, coordinated molecules mobilize, resulting in platelets aggregation and finally formation of fibrin clot and thrombi. Delineation of the mechanisms that contribute to pro-thrombotic phenotype of platelets could provide novel therapeutic targets for thrombi-related diseases. Various endogenous or exogenous molecules, such as ox-LDL, can bind CD36 and drive the platelets to become hyperactivated via Src family kinases, Vav-guanine nucleotide exchange factors, cGMP, and NADPH oxidase [69]. Moreover, advanced glycation end product directly and specifically interact with platelet-derived CD36, promoting rapid thrombosis, while CD36−/− mice had a delayed time to form the occlusive thrombi [70]. TSP-1, another CD36 ligand, was abundantly present in the α-granules of platelets. Importantly, both CD36−/− and TSP-1−/− mice showed apparently enhanced dissolution of thrombi formed on collagen [71]. These data imply that TSP1/CD36 (ligand/receptor axis) was involved in the maintenance of a stable thrombus.
Recent data have also indicated that platelet CD36 enhanced caspase-dependent procoagulant activity in vivo via ERK5 [72]. Furthermore, when subjected to ox-LDL stimulation, platelets form aggregates with monocytes, which in turn promotes ox-LDL uptake by monocytes in a CD36-dependent manner [8]. Interestingly, the platelets from patients with coronary artery disease expressed higher levels of CD36 than disease-free population. More importantly, the co-culture of platelets derived from patients with coronary artery disease with monocytes induced polarization and foam cell formation [73]. These findings suggest complex interactions between various CD36-expressing cell types drive the onset and progression of atherosclerosis. The role of CD36 in atherosclerosis is summarized in Fig. 2.
Pharmacological Modifiers of CD36
CD36 represents a promising therapeutic target for atherosclerosis. Statins, the most widely used lipid-lowering drugs, can inhibit CD36 expression/activity via a PPARγ-dependent pathway in macrophages [74]. Statins (fluvastatin and pitavastatin) also decreased CD36 expression in aortic VSMCs [75]. The inhibitory action of statins against CD36 was further validated by the observation that monocytes from statin-treated patients with acute coronary syndromes exhibited lower expression of CD36 [76]. Moreover, statin-treated subjects diminished the proportion of macrophage with low-CD36 in adipose tissue [77]. Another commonly-used anti-hypertensive drug, nifedipine, also suppressed CD36 expression and lipid uptake and deposition in macrophages [78]. Consistent with the previous studies, ezetimibe, a selective inhibitor of intestinal cholesterol absorption, decreased CD36 expression and foam cell formation [79]. Interestingly, apart from the traditional cardioprotective drugs, tamoxifen, an anti-breast cancer medicine also decreased CD36-dependent foam cell formation [80].
Besides the above synthetic modulators of CD36, increasing evidence has shown that bioactive compounds from herbal products also exert anti-atherosclerotic actions though inhibiting CD36 expression and CD36-mediated key cellular events in atherosclerosis. For example, andrographolide inhibited CD36 level by promoting the degradation of CD36 and blunting ox-LDL-induced foam cell formation in mouse macrophages [81]. In addition, pomegranate peel polyphenols, spiromastixones, and puerarin could suppress CD36 expression, thereby decreasing CD36-mediated lipid uptake, promoting cholesterol efflux, and reducing foam cell formation [82,83,84]. Tanshinone IIA, a multi-target compound from traditional Chinese herb-Danshen [85, 86], prevented atherothrombosis by targeting platelet CD36 and MKK4/JNK2-mediated platelet activation [87]. More recently, Orientin, a flavonoid from plants, inhibited ox-LDL induced inflammatory response and lipid droplet formation [88]. Furthermore, quercetin also generated the anti-atherosclerotic effect in ApoE−/− mice [89]. Similar CD36-inhibitory and anti-atherosclerotic effects has been observed in other bioactive compounds, such as quercetin [90] and curcumin [91].
In summary, these synthetic and herbal compounds are promising agents to halt CD36-dependent atherogenic events.
Conclusion and Perspectives
CD36 coding mutations have been shown to be associated with altered lipid/fatty acid metabolism, glucose intolerance, type 2 diabetes, and cardiovascular diseases in mice and humans [11]. CD36 acts a multi-functional inflammatory-metabolic receptor by physiologically regulating lipid homeostasis and immune homeostasis. Imbalanced expression of CD36 is associated with the occurrence and development of atherosclerosis. Thus, it is particularly important to find the “prime protection window” to early block the progression of atherosclerosis. Future studies are encouraged to focus on the following: (1) post-transcriptional regulation of CD36 by novel long non-coding RNAs and the impact on vascular dysfunction, (2) focus on the impact of histone modifications (such as acetylation and methylation) on CD36, (3) characterization of the pathogenic role of single nucleotide polymorphisms of CD36 in atherosclerosis, and (4) the potential role of the soluble form of CD36 (sCD36) as a reliable biomarker for atherosclerosis diagnosis in patients.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2020 update: a report from the American Heart Association. Circulation. 2020;141(9):E139–596.
Afroz R, Cao Y, Rostam MA, Ta H, Xu S, Zheng W, et al. Signalling pathways regulating galactosaminoglycan synthesis and structure in vascular smooth muscle: implications for lipoprotein binding and atherosclerosis. Pharmacol Ther. 2018;187:88–97.
• Wang DD, Yang Y, Lei YN, et al. Targeting foam cell formation in atherosclerosis: therapeutic potential of natural products. Pharmacol Rev. 2019;71(4):596–670 This is a comprehensive review of the role of all scavenger receptors (incluidng CD36) in atherosclerosis.
•• Libby P, Buring JE, Badimon L, et al. Atherosclerosis. Nat Rev Dis Primers. 2019;5(1):56. https://doi.org/10.1038/s41572-019-0106-zThis is a detailed review of the epidemiology, mechanisms, and therapies of atherosclerosis.
Tian KM, Ogura S, Little PJ, Xu SW, Sawamura T. Targeting LOX-1 in atherosclerosis and vasculopathy: current knowledge and future perspectives. Ann N Y Acad Sci. 2019;1443(1):34–53.
Xu SW, Ogura S, Chen JW, Little PJ, Moss J, Liu PQ. LOX-1 in atherosclerosis: biological functions and pharmacological modifiers. Cell Mol Life Sci. 2013;70(16):2859–72.
Jay AG, Hamilton JA. The enigmatic membrane fatty acid transporter CD36: new insights into fatty acid binding and their effects on uptake of oxidized LDL. Prostag Leukotr Ess. 2018;138:64–70.
Park YM. CD36, a scavenger receptor implicated in atherosclerosis. Exp Mol Med. 2014;46:e99.
Nozaki S, Kashiwagi H, Yamashita S, Nakagawa T, Kostner B, Tomiyama Y, et al. Reduced uptake of oxidized low density lipoproteins in monocyte-derived macrophages from CD36-deficient subjects. J Clin Invest. 1995;96(4):1859–65.
Hoosdally SJ, Andress EJ, Wooding C, Martin CA, Linton KJ. The human scavenger receptor CD36: glycosylation status and its role in trafficking and function. J Biol Chem. 2009;284(24):16277–88.
Meyre D, Andress EJ, Sharma T, Snippe M, Asif H, Maharaj A, et al. Contribution of rare coding mutations in CD36 to type 2 diabetes and cardio-metabolic complications. Sci Rep. 2019;9(1):17123.
Zhao L, Varghese Z, Moorhead JF, Chen Y, Ruan XZ. CD36 and lipid metabolism in the evolution of atherosclerosis. Br Med Bull. 2018;126(1):101–12.
Puente Navazo MD, Daviet L, Ninio E, McGregor JL. Identification on human CD36 of a domain (155-183) implicated in binding oxidized low-density lipoproteins (Ox-LDL). Arterioscler Thromb Vasc Biol. 1996;16(8):1033–9.
Pepino MY, Kuda O, Samovski D, Abumrad NA. Structure-function of CD36 and importance of fatty acid signal transduction in fat metabolism. Annu Rev Nutr. 2014;34:281–303.
Jay AG, Chen AN, Paz MA, Hung JP, Hamilton JA. CD36 binds oxidized low density lipoprotein (LDL) in a mechanism dependent upon fatty acid binding. J Biol Chem. 2015;290(8):4590–603.
Silverstein RL, Li W, Park YM, Rahaman SO. Mechanisms of cell signaling by the scavenger receptor CD36: implications in atherosclerosis and thrombosis. Trans Am Clin Climatol Assoc. 2010;121:206–20.
Han S, Sidell N. Peroxisome-proliferator-activated-receptor gamma (PPARgamma) independent induction of CD36 in THP-1 monocytes by retinoic acid. Immunology. 2002;106(1):53–9.
Tsukahara T. 1-O-alkyl glycerophosphate-induced CD36 expression drives oxidative stress in microglial cells. Cell Signal. 2020;65:109459.
Raghavan S, Singh NK, Gali S, Mani AM, Rao GN. Protein kinase Ctheta via activating transcription factor 2-mediated CD36 expression and foam cell formation of Ly6C(hi) cells contributes to atherosclerosis. Circulation. 2018;138(21):2395–412.
Hosui A, Tatsumi T, Hikita H, Saito Y, Hiramatsu N, Tsujii M, et al. Signal transducer and activator of transcription 5 plays a crucial role in hepatic lipid metabolism through regulation of CD36 expression. Hepatol Res. 2017;47(8):813–25.
Sui Y, Xu J, Rios-Pilier J, Zhou C. Deficiency of PXR decreases atherosclerosis in apoE-deficient mice. J Lipid Res. 2011;52(9):1652–9.
Mendez-Barbero N, Esteban V, Villahoz S, et al. A major role for RCAN1 in atherosclerosis progression. EMBO Mol Med. 2013;5(12):1901–17.
Lindgren A, Levin M, Rodrigo Blomqvist S, Wikström J, Ahnmark A, Mogensen C, et al. Adiponectin receptor 2 deficiency results in reduced atherosclerosis in the brachiocephalic artery in apolipoprotein E deficient mice. PLoS One. 2013;8(11):e80330.
Xia F, Li R, Wang C, Yang S, Tian L, Dong H, et al. IRGM1 regulates oxidized LDL uptake by macrophage via actin-dependent receptor internalization during atherosclerosis. Sci Rep. 2013;3:1867.
Hashimoto R, Kakigi R, Miyamoto Y, Nakamura K, Itoh S, Daida H, et al. JAK-STAT-dependent regulation of scavenger receptors in LPS-activated murine macrophages. Eur J Pharmacol. 2020;871:172940.
Zhou H, Zhang J, Eyers F, Xiang Y, Herbert C, Tay HL, et al. Identification of the microRNA networks contributing to macrophage differentiation and function. Oncotarget. 2016;7(20):28806–20.
Li H, Fan J, Zhao Y, Zhang X, Dai B, Zhan J, et al. Nuclear miR-320 mediates diabetes-induced cardiac dysfunction by activating transcription of fatty acid metabolic genes to cause lipotoxicity in the heart. Circ Res. 2019;125(12):1106–20.
Barberio MD, Kasselman LJ, Playford MP, Epstein SB, Renna HA, Goldberg M, et al. Cholesterol efflux alterations in adolescent obesity: role of adipose-derived extracellular vesical microRNAs. J Transl Med. 2019;17(1):232.
Du XJ, Lu JM, Sha Y. MiR-181a inhibits vascular inflammation induced by ox-LDL via targeting TLR4 in human macrophages. J Cell Physiol. 2018;233(10):6996–7003.
Li BR, Xia LQ. Liu J, et al: miR-758-5p regulates cholesterol uptake via targeting the CD36 3′UTR. Biochem Biophys Res Commun. 2017;494(1–2):384–9.
Huangfu N, Xu Z, Zheng W, Wang Y, Cheng J, Chen X. LncRNA MALAT1 regulates oxLDL-induced CD36 expression via activating beta-catenin. Biochem Biophys Res Commun. 2018;495(3):2111–7.
Chen DD, Hui LL, Zhang XC, Chang Q. NEAT1 contributes to ox-LDL-induced inflammation and oxidative stress in macrophages through inhibiting miR-128. J Cell Biochem. 2018.
Reddy MA, Chen Z, Park JT, Wang M, Lanting L, Zhang Q, et al. Regulation of inflammatory phenotype in macrophages by a diabetes-induced long noncoding RNA. Diabetes. 2014;63(12):4249–61.
Wang X, Chang X, Zhang P, Fan L, Zhou T, Sun K. Aberrant expression of long non-coding RNAs in newly diagnosed type 2 diabetes indicates potential roles in chronic inflammation and insulin resistance. Cell Physiol Biochem. 2017;43(6):2367–78.
Guo J, Fang W, Sun L, et al. Ultraconserved element uc.372 drives hepatic lipid accumulation by suppressing miR-195/miR4668 maturation. Nat Commun. 2018;9(1):612.
Hung J, Scanlon JP, Mahmoud AD, Rodor J, Ballantyne M, Fontaine MAC, et al. Novel plaque enriched long noncoding RNA in atherosclerotic macrophage regulation (PELATON). Arterioscl Throm Vas. 2020;40(3):697–713.
Keller M, Hopp L, Liu X, Wohland T, Rohde K, Cancello R, et al. Genome-wide DNA promoter methylation and transcriptome analysis in human adipose tissue unravels novel candidate genes for obesity. Mol Metab. 2017;6(1):86–100.
Love-Gregory L, Kraja AT, Allum F, Aslibekyan S, Hedman ÅK, Duan Y, et al. Higher chylomicron remnants and LDL particle numbers associate with CD36 SNPs and DNA methylation sites that reduce CD36. J Lipid Res. 2016;57(12):2176–84.
Allum F, Shao X, Guenard F, et al. Characterization of functional methylomes by next-generation capture sequencing identifies novel disease-associated variants. Nat Commun. 2015;6:7211.
Bekkering S, Quintin J, Joosten LA, van der Meer JW, Netea MG, Riksen NP. Oxidized low-density lipoprotein induces long-term proinflammatory cytokine production and foam cell formation via epigenetic reprogramming of monocytes. Arterioscler Thromb Vasc Biol. 2014;34(8):1731–8.
Cui K, Zang C, Roh TY, Schones DE, Childs RW, Peng W, et al. Chromatin signatures in multipotent human hematopoietic stem cells indicate the fate of bivalent genes during differentiation. Cell Stem Cell. 2009;4(1):80–93.
Choi JH, Nam KH, Kim J, Baek MW, Park JE, Park HY, et al. Trichostatin A exacerbates atherosclerosis in low density lipoprotein receptor-deficient mice. Arterioscler Thromb Vasc Biol. 2005;25(11):2404–9.
Lee TI, Kao YH, Tsai WC, Chung CC, Chen YC, Chen YJ. HDAC inhibition modulates cardiac PPARs and fatty acid metabolism in diabetic cardiomyopathy. PPAR Res. 2016;2016:1–10.
Ren B, Best B, Ramakrishnan DP, Walcott BP, Storz P, Silverstein RL. LPA/PKD-1-FoxO1 signaling axis mediates endothelial cell CD36 transcriptional repression and proangiogenic and proarteriogenic reprogramming. Arterioscler Thromb Vasc Biol. 2016;36(6):1197–208.
Razani B, Feng C, Coleman T, Emanuel R, Wen H, Hwang S, et al. Autophagy links inflammasomes to atherosclerotic progression. Cell Metab. 2012;15(4):534–44.
Aragon-Herrera A, Feijoo-Bandin S, Otero Santiago M, et al. Empagliflozin reduces the levels of CD36 and cardiotoxic lipids while improving autophagy in the hearts of Zucker diabetic fatty rats. Biochem Pharmacol. 2019;170:113677.
Li Y, Yang P, Zhao L, Chen Y, Zhang X, Zeng S, et al. CD36 plays a negative role in the regulation of lipophagy in hepatocytes through an AMPK-dependent pathway. J Lipid Res. 2019;60(4):844–55.
Wang C, Xu W, Liang M, Huang D, Huang K. CTRP13 inhibits atherosclerosis via autophagy-lysosome-dependent degradation of CD36. FASEB J. 2019;33(2):2290–300.
Zhang F, Xia X, Chai R, et al. Inhibition of USP14 suppresses the formation of foam cell by promoting CD36 degradation. J Cell Mol Med. 2020.
Chu LY, Ramakrishnan DP, Silverstein RL. Thrombospondin-1 modulates VEGF signaling via CD36 by recruiting SHP-1 to VEGFR2 complex in microvascular endothelial cells. Blood. 2013;122(10):1822–32.
Magwenzi S, Woodward C, Wraith KS, Aburima A, Raslan Z, Jones H, et al. Oxidized LDL activates blood platelets through CD36/NOX2-mediated inhibition of the cGMP/protein kinase G signaling cascade. Blood. 2015;125(17):2693–703.
•• Chen Y, Yang M, Huang W, et al. Mitochondrial metabolic reprogramming by CD36 signaling drives macrophage inflammatory responses. Circ Res. 2019;125(12):1087–102. https://doi.org/10.1038/s41572-019-0106-z. This study likns oxidized LDL/CD36 signaling in macrophages with altered fatty acid metabolism and inflammation response.
Ackers I, Szymanski C, Duckett KJ, Consitt LA, Silver MJ, Malgor R. Blocking Wnt5a signaling decreases CD36 expression and foam cell formation in atherosclerosis. Cardiovasc Pathol. 2018;34:1–8.
Fan Y, Yang J, Li H, Li HD, Zhang S, Li X, et al. SNX10 deficiency restricts foam cell formation and protects against atherosclerosis by suppressing CD36-Lyn axis. Can J Cardiol. 2020.
Kalluri AS, Vellarikkal SK, Edelman ER, Nguyen L, Subramanian A, Ellinor PT, et al. Single-cell analysis of the normal mouse aorta reveals functionally distinct endothelial cell populations. Circulation. 2019;140(2):147–63.
Silverstein RL. Oxidized lipid uptake by scavenger receptor CD36 (cluster of differentiation 36) modulates endothelial surface properties and may contribute to atherogenesis. Arterioscler Thromb Vasc Biol. 2018;38(1):4–5.
Le Master E, Huang RT, Zhang CX, et al. Proatherogenic flow increases endothelial stiffness via enhanced CD36-mediated uptake of oxidized low-density lipoproteins. Arterioscl Throm Vas. 2018;38(1):64–75.
Gerbod-Giannone MC, Dallet L, Naudin G, Sahin A, Decossas M, Poussard S, et al. Involvement of caveolin-1 and CD36 in native LDL endocytosis by endothelial cells. Biochim Biophys Acta Gen Subj. 2019;1863(5):830–8.
Son NH, Basu D, Samovski D, Pietka TA, Peche VS, Willecke F, et al. Endothelial cell CD36 optimizes tissue fatty acid uptake. J Clin Invest. 2018;128(10):4329–42.
•• Xu S, Jay A, Brunaldi K, Huang N, Hamilton JA. CD36 enhances fatty acid uptake by increasing the rate of intracellular esterification but not transport across the plasma membrane. Biochemistry. 2013;52(41):7254–61 This is an important study of the role of CD36 in fatty acid uptake.
Kiyan Y, Tkachuk S, Hilfiker-Kleiner D, Haller H, Fuhrman B. Dumler I: oxLDL induces inflammatory responses in vascular smooth muscle cells via urokinase receptor association with CD36 and TLR4. J Mol Cell Cardiol. 2014;66:72–82.
Yue H, Febbraio M, Klenotic PA, Kennedy DJ, Wu Y, Chen S, et al. CD36 enhances vascular smooth muscle cell proliferation and development of neointimal hyperplasia. Arterioscler Thromb Vasc Biol. 2019;39(2):263–75.
Park YM, Febbraio M, Silverstein RL. CD36 modulates migration of mouse and human macrophages in response to oxidized LDL and may contribute to macrophage trapping in the arterial intima. J Clin Invest. 2009;119(1):136–45.
Harb D, Bujold K, Febbraio M, Sirois MG, Ong H, Marleau S. The role of the scavenger receptor CD36 in regulating mononuclear phagocyte trafficking to atherosclerotic lesions and vascular inflammation. Cardiovasc Res. 2009;83(1):42–51.
Park YM, Drazba JA, Vasanji A, Egelhoff T, Febbraio M, Silverstein RL. Oxidized LDL/CD36 interaction induces loss of cell polarity and inhibits macrophage locomotion. Mol Biol Cell. 2012;23(16):3057–68.
Huang SCC, Everts B, Ivanova Y, O’Sullivan D, Nascimento M, Smith AM, et al. Cell-intrinsic lysosomal lipolysis is essential for alternative activation of macrophages. Nat Immunol. 2014;15(9):846–55.
Xie S, Lee YF, Kim E, Chen LM, Ni J, Fang LY, et al. TR4 nuclear receptor functions as a fatty acid sensor to modulate CD36 expression and foam cell formation. P Natl Acad Sci USA. 2009;106(32):13353–8.
Kim S, Cho W, Kim I, Lee SH, Oh GT, Park YM. Oxidized LDL induces vimentin secretion by macrophages and contributes to atherosclerotic inflammation. J Mol Med. 2020.
Yang M, Silverstein RL. CD36 and ERK5 link dyslipidemia to apoptotic-like platelet procoagulant function. Curr Opin Hematol. 2019;26(5):357–65.
Zhu W, Li W, Silverstein RL. Advanced glycation end products induce a prothrombotic phenotype in mice via interaction with platelet CD36. Blood. 2012;119(25):6136–44.
Kuijpers MJ, de Witt S, Nergiz-Unal R, et al. Supporting roles of platelet thrombospondin-1 and CD36 in thrombus formation on collagen. Arterioscler Thromb Vasc Biol. 2014;34(6):1187–92.
Yang M, Kholmukhamedov A, Schulte ML, Cooley BC, Scoggins N’O, Wood JP, et al. Platelet CD36 signaling through ERK5 promotes caspase-dependent procoagulant activity and fibrin deposition in vivo. Blood Adv. 2018;2(21):2848–61.
Mehrpouri M, Bashash D, Mohammadi MH, Gheydari ME, Satlsar ES, Hamidpour M. Co-culture of platelets with monocytes induced M2 macrophage polarization and formation of foam cells: shedding light on the crucial role of platelets in monocyte differentiation. Turk J Haematol. 2019;36(2):97–105.
Han J, Zhou X, Yokoyama T, Hajjar DP, Gotto AM Jr, Nicholson AC. Pitavastatin downregulates expression of the macrophage type B scavenger receptor, CD36. Circulation. 2004;109(6):790–6.
Fukuda K, Matsumura T, Senokuchi T, Ishii N, Kinoshita H, Yamada S, et al. Statins meditate anti-atherosclerotic action in smooth muscle cells by peroxisome proliferator-activated receptor-gamma activation. Biochem Biophys Res Commun. 2015;457(1):23–30.
Piechota M, Banaszewska A, Dudziak J, Slomczynski M, Plewa R. Highly upregulated expression of CD36 and MSR1 in circulating monocytes of patients with acute coronary syndromes. Protein J. 2012;31(6):511–8.
Lesna IK, Petras M, Cejkova S, et al. Cardiovascular disease predictors and adipose tissue macrophage polarization: is there a link? Eur J Prev Cardiol. 2018;25(3):328–34.
Zhang Q, Sha Ma AZ, Wang C, Tang WQ, Song ZY. Nifedipine inhibits ox-LDL-induced lipid accumulation in human blood-derived macrophages. Biochem Biophys Res Commun. 2015;457(3):440–4.
Qin L, Yang YB, Yang YX, Zhu N, Liu Z, Ni YG, et al. Inhibition of macrophage-derived foam cell formation by ezetimibe via the caveolin-1/MAPK pathway. Clin Exp Pharmacol Physiol. 2016;43(2):182–92.
Yu M, Jiang M, Chen Y, Zhang S, Zhang W, Yang X, et al. Inhibition of macrophage CD36 expression and cellular oxidized low density lipoprotein (oxLDL) accumulation by tamoxifen: a peroxisome proliferator-activated receptor (PPAR)gamma-dependent mechanism. J Biol Chem. 2016;291(33):16977–89.
Lin HC, Lii CK, Chen HC, Lin AH, Yang YC, Chen HW. Andrographolide inhibits oxidized LDL-induced cholesterol accumulation and foam cell formation in macrophages. Am J Chin Med. 2018;46(1):87–106.
Wu C, Chen R, Liu M, Liu D, Li X, Wang S, et al. Spiromastixones inhibit foam cell formation via regulation of cholesterol efflux and uptake in RAW264.7 macrophages. Mar Drugs. 2015;13(10):6352–65.
Zhang H, Zhai Z, Zhou H, et al. Puerarin inhibits oxLDL-induced macrophage activation and foam cell formation in human THP1 macrophage. Biomed Res Int. 2015;2015:403616.
Zhao S, Li J, Wang L, Wu X. Pomegranate peel polyphenols inhibit lipid accumulation and enhance cholesterol efflux in raw264.7 macrophages. Food Funct. 2016;7(7):3201–10.
Fang J, Little PJ, Xu SW. Atheroprotective effects and molecular targets of tanshinones derived from herbal medicine danshen. Med Res Rev. 2018;38(1):201–28.
Li ZM, Xu SW, Liu PQ. Salvia miltiorrhizaBurge (Danshen): a golden herbal medicine in cardiovascular therapeutics. Acta Pharmacol Sin. 2018;39(5):802–24.
Wang H, Zhong L, Mi S, Song N, Zhang W, Zhong M. Tanshinone IIA prevents platelet activation and down-regulates CD36 and MKK4/JNK2 signaling pathway. BMC Cardiovasc Disord. 2020;20(1):81.
Li CM, Cai CC, Zheng XJ, Sun J, Ye L. Orientin suppresses oxidized low-density lipoproteins induced inflammation and oxidative stress of macrophages in atherosclerosis. Biosci Biotechnol Biochem. 2020;84(4):774–9.
Jia Q, Cao H, Shen D, Li S, Yan L, Chen C, et al. Quercetin protects against atherosclerosis by regulating the expression of PCSK9, CD36, PPARgamma, LXRalpha and ABCA1. Int J Mol Med. 2019;44(3):893–902.
Jia Q, Cao H, Shen D, Li S, Yan L, Chen C, et al. Quercetin protects against atherosclerosis by regulating the expression of PCSK9, CD36, PPARγ, LXRα and ABCA1. Int J Mol Med. 2019;44(3):893–902.
Zingg JM, Hasan ST, Nakagawa K, et al. Modulation of cAMP levels by high-fat diet and curcumin and regulatory effects on CD36/FAT scavenger receptor/fatty acids transporter gene expression. BioFactors (Oxford, England). 2017;43(1):42–53.
Acknowledgments
The authors were grateful to Prof. Roy Silverstein (Medical College of Wisconsin) for his insightful comments on and proof-reading of this manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Topical Collection on Vascular Biology
Rights and permissions
About this article
Cite this article
Tian, K., Xu, Y., Sahebkar, A. et al. CD36 in Atherosclerosis: Pathophysiological Mechanisms and Therapeutic Implications. Curr Atheroscler Rep 22, 59 (2020). https://doi.org/10.1007/s11883-020-00870-8
Published:
DOI: https://doi.org/10.1007/s11883-020-00870-8