Abstract
Purpose of Review
Work-related asthma is a common disorder among adult asthma patients, and in the case of occupational asthma, it is induced by workplace exposures.
Recent Findings
Occupational asthma provides an excellent model and benchmark for identifying and testing different allergy or inflammatory biomarkers associated with its inception or progression. Moreover, specific inhalation challenge with the incriminated agent represents an experimental setting to identify and validate potential systemic or local biomarkers. Some biomarkers are mainly blood-borne, while local airway biomarkers are derived from inflammatory or resident cells. Genetic and gene–environment interaction studies also provide an excellent framework to identify relevant profiles associated with the risk of developing these work-related conditions.
Summary
Despite significant efforts to identify clinically relevant inflammatory and genomic markers for occupational asthma, apart from the documented utility of airway inflammatory biomarkers, it remains elusive to define specific markers or signatures clearly associated with different endpoints or outcomes in occupational asthma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Occupational asthma (OA) is defined as a type of asthma caused by the workplace [1]. Two types of OA are distinguished: allergic OA, which is induced by sensitizers and appears after a latency period of sensitization to the causal agent, and irritant-induced OA, which is due to acute high-level exposure to respiratory irritants or to persistent exposure to moderate–high-level exposure to respiratory irritants [2, 3].
Substances causing allergic OA are classified into low-molecular-weight (LMW) compounds (often chemicals) or high-molecular-weight (HMW) agents (primarily proteins or glycoproteins). HMW agents usually induce an immediate or a dual asthmatic response, similar to the airway inflammation found after inhalation challenges with common aeroallergens, through an immunoglobulin (Ig) E-mediated mechanism. LMW agents often induced late asthmatic responses, and the underlying pathologic mechanism is still being debated, with the exception of some few demonstrated IgE-mediated mechanisms, such as some cases of OA induced by isocyanates or red cedar dust [4].
Since OA has been defined as an inflammatory disease, progress has been made in the search for biological and genetic markers that might serve as complementary tools: to facilitate the diagnosis of OA; to identify reliable predictors of the disease or its prognosis in groups of workers; and for a better characterization of personal susceptibility to develop OA before exposure to one particular agent. Early detection might allow for improved treatment outcomes and even be useful in the primary prevention of OA. Biological and genomic markers would help identify susceptible workers.
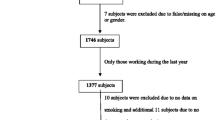
This review focuses on recent research in this field and provides an update on current knowledge in the role of biological and genetic biomarkers in OA. An English literature search using electronic engines (PubMed and EMBASE) was conducted in peer review journals using OVID and the SOD (Documents Obtaining Service from the Health Public Service Libraries in Madrid, Spain) in order to perform the most suitable and representative articles in this genetic and biomarkers in OA review. The search was limited to published studies and review articles from 2010 to June 2016 but some previous referential articles in this field have been expressly included.
Airway Inflammatory Markers Following Specific Inhalation Challenge
Specific inhalation challenge (SIC) constitutes the reference standard for the diagnosis of OA [5••]. A positive response is defined by a fall in forced expiratory volume in 1 s (FEV1) ≥15 % from baseline [5••]. If airflow obstruction is not induced by inhalation of the specific agent, an increase in nonspecific bronchial responsiveness, sputum eosinophils, or exhaled nitric oxide after specific antigen challenge supports the likelihood that the patient has OA or non-asthmatic eosinophilic bronchitis due to that allergen [6].
Over the past two decades, there has been growing interest in the noninvasive assessment of eosinophilic airway inflammation through sputum cell analysis and the measurement of fractional concentrations of exhaled nitric oxide (FeNO) as complementary tools to conventional lung function tests in the diagnosis and management of asthma. The analysis of induced sputum cell counts is regarded as a useful and additional tool in the investigation of OA [5••]. However, sputum induction and processing are time-consuming, and it is usually restricted to tertiary centers. In contrast, FeNO is easy to measure and is feasible in almost all patients, providing immediate results. However, it is more sensitive to confounding factors, such as smoking, atopy, and treatment with inhaled corticosteroids, as compared with sputum eosinophil counts [7]. Although FeNO could be considered as an induced sputum surrogate to measure eosinophilic airway inflammation, its real value in the investigation of OA remains, at least, controversial.
Induced Sputum Associated with the SIC
The use of differential cell counts in induced sputum (IS) during the investigation of OA can improve its utility by bringing an additional objective measure to this investigation. Although inadequate maneuvers during the performance of the spirometry could affect the reliability of FEV1 and PC20, these airway inflammation parameters are not affected by improper maneuvers during sputum induction [7]. The best timing for the collection of sputum with respect to the exposure to occupational agents is likely to be 7–24 h after exposure [8].
Eosinophil counts and eosinophilic cationic protein (ECP) concentration rapidly increased, observing higher levels in less than 24 h after specific challenge in IS samples of responder workers compared with the non-responders or controls [9]. The magnitude of increase in sputum eosinophil counts occurring after exposure to occupational agents that should be regarded as clinically significant is not clearly established. A combination of a greater than 0.26 × 106/ml increase in sputum eosinophil numbers and a decrease in the concentration of methacholine inducing a 20 % fall in FEV1 of at least 1.8-fold compared with baseline values predicted a 20 % fall in FEV1 in 96 % (95%CI = 70–99 %) of patients [10]. Vandenplas et al. concluded that a >3 % increase in sputum eosinophils at the end of the first challenge day was the most accurate parameter for predicting the development of an asthmatic response on subsequent challenges. With a sensitivity of 67 % and a specificity of 97 %, an increase of sputum eosinophils could help identify a subject who would develop an asthmatic reaction only after repeated exposure [11]. Malo et al. performed a retrospective study confirming that elevated sputum eosinophils (≥3 %), in combination with a normal nonspecific bronchial provocation test, exhibited the highest predictive value for the diagnosis of OA caused by HMW and LMW agents [12]. Coupling information on the level of eosinophils to responsiveness to methacholine increased positive predictive values for OA from 39 to 69 %. The current study shows that sputum eosinophilia is common after exposure to both types of sensitizers, HMW and LMW, and following all types of asthmatic responses [10, 13•].
A post-challenge increase in sputum neutrophil count has also been documented [11, 14, 15], especially after exposure to LMW agents with and without asthma [13•, 16]. Nevertheless, the interpretation of changes in sputum neutrophil counts requires further validation.
In a retrospective study of 82 subjects with OA confirmed with a positive SIC (41 sensitized to LMW and 41 to HMW agents), Prince et al. assessed changes in airway inflammatory cells following SIC in sensitized workers [14]. They also looked for possible influencing factors on the pattern of inflammatory responses to SIC. In the LMW group, eosinophil counts increased following late asthmatic responses, as well as neutrophil numbers. In the HMW group, eosinophil percentages increased, both after early and dual asthmatic responses. Interestingly, the increased neutrophil count was higher in current smokers than in ex-smokers or non-smokers. The length of exposure to the agent, tobacco use, and baseline percentage of eosinophils were independent predictors of the change in eosinophils, whereas age and baseline neutrophil percentage were predictors of the change in neutrophils.
Sanchez-Vidaurre et al. compared the inflammation cell percentages and inflammatory markers in sputum samples of subjects with and without OA [13•]. Thirty-four subjects tested positive to SIC and were diagnosed with OA, 10 due to HMW agents and 24 to LMW agents. Seventeen subjects presented a negative SIC. Increases in sputum eosinophils, neutrophils, and interleukin (IL)-10 concentration and decrease in leukotriene B4 levels were observed in patients with HMW-induced OA, but not in those exposed to LMW agents. Increased sputum neutrophils and increased IL-8 levels were observed in subjects exposed to LMW agents who were diagnosed as having other respiratory diseases [13•].
However, some interfering factors might modify the sputum cell response and the interpretation of sputum results. Treatment with corticosteroids might blunt eosinophil influx, endotoxin contamination might favor sputum neutrophilia, and relatively high levels of exposure to chemicals might produce irritant effects [7].
Fractional Exhaled Nitric Oxide Associated with SIC
Nitric oxide (NO), produced in the respiratory tract by the activation of NO synthase in various cell types, is detectable in exhaled air. This noninvasive biomarker has been used in asthma as an indicator of the presence of mainly eosinophilic inflammation and response to treatment with corticosteroids [17]. FeNO can be measured online with fixed or portable instruments, or exhaled air can be collected for offline FeNO measurements [7].
Assessment of changes in FeNO levels during SIC may be useful in subjects who fail to provide suitable sputum samples [7, 16], but the role of FeNO in occupational challenge testing remains unproven. Several prospective studies have investigated FeNO changes after SIC in this setting [8, 18, 19••]. A significant increase in FeNO level was observed only 24 h after positive challenges, while there was a significant increase in sputum eosinophil at 7 h [8, 20]. Pedrosa et al. showed a significant 14 ppb FeNO change 24 h after positive SIC (n = 21) compared with negative tests (n = 13) with HMW agents, and retrospective receiver–operator curve analysis achieved a sensitivity of 81 % and a specificity of 92 % in identifying a positive result from a 12 % increase in FeNO [21].
However, Sastre et al. found that only LMW agents induced a significant increase in FeNO after a positive SIC [22]. Sixty-eight subjects studied with suspect of OA were enrolled, 45 with a positive SIC (27.9 % to HMW and 72.1 % to LMW agents) and 23 with a negative SIC. In subjects with a negative SIC, they found a significant increase in FeNO levels only in smokers. Moreover, there was no FeNO increase depending on the type of asthmatic reaction in the SIC, in contrast to Ferazzoni et al. [20] who reported that the magnitude of FeNO increase was greater in subjects who experienced an immediate asthmatic reaction induced by isocyanates.
Walters et al. included 16 workers undertaking SICs to predominantly LMW agents [23]. Negative control challenges were associated with mean changes in FeNO of 9 % or 1.1 ppb. Subsequent positive SICs were associated with mean changes in FeNO of 7 % or 2.1 ppb, with no significantly different levels to controls. Only 2 from 16 (13 % from the included workers) experienced clinically relevant FeNO changes after the SIC. Three other studies have demonstrated an increase in FeNO levels 24 h after exposure to HMW and LMW agents, with a good correlation with sputum eosinophil measurements [8, 20, 24].
However, the measure of changes in FeNO levels seems to be a less reliable tool than changes in sputum eosinophils to discriminate between a positive or a negative SIC [8]. One of the reasons for the discrepancies among the studies might pertain to the different phenotypes of patients. Lemiere et al. [19••] wondered whether the increase of FeNO levels following a positive SIC was restricted to the phenotypes of subjects sharing common clinical characteristics. They analyzed, in a prospective observational study, consecutive subjects who had been investigated for possible OA, through the performance of a SIC from 2006 to 2012, by using a statistical cluster analysis. One hundred and seventy-eight subjects underwent SIC, and 98 had a positive cluster analysis result. The cluster analysis performed in the OA subgroup identified three distinct phenotypes. Cluster 1 included milder asthmatic subjects than clusters 2 and 3. Cluster 3 contrasted greatly with clusters 1 and 2 with lower number of atopic subjects, no exposure to HMW agents, and greater number of late reactions. Furthermore, FeNO changes during SIC were restricted to clusters 1 and 2, in which the subjects were mainly exposed to HMW agents. The molecular weight of the agent (HMW vs. LMW) was the only factor associated with an increase in FeNO (OR = 4.2, 95%CI = 1.1–16.8) in subjects with a positive SIC, concluding that an increase in FeNO was strongly associated with asthmatic reactions induced by HMW agents. In conclusion, measurement of changes in FeNO levels after the SIC in OA appears more effective for ruling in asthma than for ruling it out.
Biological Markers in the Diagnosis of OA
Sputum Biomarkers
Sputum studies have shown that exposure to occupational agents at work and in the laboratory can induce an eosinophilic [7, 11] and, less consistently, a neutrophilic inflammation of the airways in sensitized subjects [25]. According to this, an increase in sputum eosinophils might precede functional changes after repeated exposures to low doses of occupational agents in sensitized subjects who develop asthmatic reactions induced by common inhalant allergens, as well as HMW and LMW occupational agents [11]. Moreover, sputum eosinophilia could play a role as a possible determinant of the decline in FEV1 in patients with OA. Talini et al. published in 2015 the results of a cohort of 39 patients with OA, routinely followed up between 1990 and 2009, while they were still exposed at work [26•]. Twenty-three participants were sensitized to LMW agents and 16 to HMW compounds, according to a positive SIC. In a multivariate analysis, only persistent exposure to the implicated agent and higher baseline sputum eosinophil levels significantly (≥3 %) correlated with a greater decline in FEV1.
The differential diagnosis between asthma and chronic obstructive pulmonary disease (COPD) associated with work could offer another specific role for induced sputum. Exposure to vapors, gases, dusts, and fumes could induce COPD, even in never-smoker workers. In some problematic cases, particularly in patients who have contraindications against a SIC, induced sputum might allow the assessment of biomarker profiles, helping the distinction between both diseases. Kleniewska et al. demonstrated in a cohort of 20 patients with COPD and 24 with OA that asthmatics had significantly higher sputum eosinophils percentages in comparison to COPD patients (p = 0.004), although COPD patients had higher eosinophil percentages than healthy controls (p = 0.009) [27]. Additionally, increased concentrations of matrix metalloproteinase (MMP)-9 and IL-1β in IS were detected in COPD patients compared to OA workers. MMP-9 levels in IS also increase in allergic OA patients who underwent SIC on two consecutive days with flour, but no changes in the levels of other MMPs have been reported [28].
Fractional Exhaled Nitric Oxide
An accurate and reproducible diagnostic role has been postulated for determining FeNO in cases of OA in which the presence of airway inflammation is observed [7]. Elevated levels of FeNO were found mainly in cases of OA induced by substances of HMW in which the existence of an IgE-mediated mechanism was demonstrated, such as baker’s asthma. Baatjies et al. studied the usefulness of FeNO in 424 supermarket bakery workers in a cross-sectional study using a questionnaire and determining the presence of specific IgE to wheat, rye, and alpha-amylase [29]. The median FeNO level during the work shift was 15 ppb, decreasing among smokers (12 ppb) and raised in atopic subjects, up to 21 ppb. Furthermore, increased FeNO levels were associated with IgE to cereals independently of current smoking or presence of atopy. Moreover, in a stratified analysis in a subgroup of atopic and non-smoker workers, FeNO showed the strongest relationship with the detection of specific IgE to wheat or rye (OR = 9.43, 95%CI = 4.44–20.04), work-related allergic rhinitis (OR = 8.13, 95%CI = 3.72–17.76), and probable baker’s asthma (OR = 6.72, 95%CI = 2.5–18.06). Tafuro et al. obtained similar results in warehouse workers with mite-induced allergy [30]. More recently, Van der Walt et al. evaluated 150 spice mill workers in a cross-sectional study using European Community Respiratory Health Survey questionnaires, spirometry, FeNO, and serum-specific IgE to garlic, chili pepper, and wheat [31]. They showed that FeNO levels >50 ppb were significantly associated with asthma-like symptoms due to spice dust, particularly in individuals sensitized to garlic and chili pepper (OR = 17.04, 95%CI = 2.30–126.03). Some LMW allergens, such as isocyanates, increase FeNO levels in OA. Jonaid et al. investigated the association between FeNO, using a handheld device, and occupational isocyanate exposure [32]. In a sample of 229 workers recruited from several spray-painting companies located in the Netherlands, and classified depending on their involvement in spray painting or in other tasks, isocyanate exposure above the median level was not associated with FeNO levels, but in atopic and non-smokers workers, a marginally significant association between FeNO and exposure to isocyanates was observed. As expected, FeNO was negatively associated with current smoking and positively with atopy, separately. Moreover, a borderline significant association was found between FeNO and work-related conjunctivitis, rhinitis, and asthma-like symptoms after adjustment for confounders such as age, gender, or atopy. This result suggests that increased FeNO levels might indicate increased airway inflammation in atopic and non-smoker workers exposed to isocyanates, and especially at higher levels of exposure. Concordantly, Shiryaeva et al. compared FeNO levels in two seafood worker populations involved in the processing and not in fishing (Norwegian salmon workers vs. Russian trawler workers), but with different workplace conditions [33]. Russian trawler workers are often located on the lower desks of the ships in confined and narrow spaces, natural ventilation, and manual or semiautomatic process lines. In contrast, Norwegian salmon workers do their job in factories, highly automatized and mechanical ventilation systems. They found substantially higher FeNO levels among asthmatic trawler workers compared to asthmatic salmon workers, while this last group of asthmatics did not have significantly higher levels compared to non-asthmatic salmon workers. Again, smoking, presence of specific IgE, exposure conditions at the workplace, or even population/genetic-based differences might have influenced the FeNO levels.
Conversely, it has not been shown that the determination of FeNO can be discriminative in non-eosinophilic OA, such as asthma suffered by janitorial workers. Vizcaya et al. studied 42 cleaners with asthma and/or recent respiratory symptoms in comparison to 53 healthy cleaners [34]. They found no significant differences in the levels of FeNO. Cases and controls did not differ in the percentages of detectable levels of interleukins and growth factors. Cases had significant levels of total IgE, but atopy was clearly higher among the asthmatics [34].
According to these reported data, measuring FeNO could be helpful as a marker of persistent allergen exposure in sensitized patients with OA, particularly induced by HMW agents, and also for some, but not for all, LMW agents. However, many different factors influence the FeNO levels, so its role as a complementary tool in the clinical management of OA patients remains unclear.
Serum Markers in OA
Because blood eosinophilia has been associated with eosinophilic airway inflammation, serum ECP has also been proposed as a candidate marker for OA [35]. In 12 bakery plant workers diagnosed with baker’s asthma who clinically improved with a job relocation at the workplace, while the sputum ECP levels did not show a significant difference at 6 months, there was a remarkable difference in serum ECP levels after the intervention (12.2 ± 3.0 vs. 2.8 ± 3.1 μg/l, p = 0.004) [36]. In 43 patients with allergic OA, serum ECP was significantly increased compared to the controls (p = 0.009), and shorter time interval since the removal from exposure to the implicated agent correlated with higher ECP levels (rS = 0.375) [37]. The ECP levels in nasal lavage significantly increased in patients with glutaraldehyde [38], and the reproducibility of ECP concentrations in nasal lavage has been validated in the setting of SIC in OA [39].
Classically, specific IgE tests for HMW agents exhibited the highest overall specificity relative to SIC for the diagnosis of OA (79 %, 95%CI = 50.5–93.3 %) [40]. This specificity could be increased by considering a single nonspecific challenge test. Apart from specific IgE, there is much less evidence for other molecules. Combined, the serum levels of ferritin and transferrin showed a specificity of 85.7 % for the diagnosis of methylene diisocyanate (MDI)-OA [35], but these results were neither confirmed in toluene diisocyanate (TDI)-exposed workers by Sastre et al. [41]. Serum IgG to tissue transglutaminase and serum cytokine MMP-9 levels have been proposed as useful biomarkers for identifying cases of TDI-OA among exposed workers [42]. However, serum MMP-9, IL-1β, or IL-6 seem to be less useful than the analogous assay in IS in order to establish a work-induced COPD [27]. In addition, expression of vitamin D binding protein (VDBP) was upregulated in patients with isocyanate-OA, and the sensitivity and specificity for predicting the phenotype of isocyanate-OA with VDBP were 69 and 81 %, respectively [43]. Higher levels of urine isoprostanes, prostaglandin isomers produced from polyunsaturated fatty acids, have been found in patients with non-atopic moderate persistent asthma, but also in workers exposed to formaldehyde, suggesting a possible role for these molecules in primary prevention [44]. Urine cysteinyl-leukotriene (LT) and 8-iso-prostaglandin in the exhaled breath condensate, a stable oxidative stress marker that is increased in asthmatics reflecting also non-eosinophilic inflammation, have also been measured for the follow-up of patients with OA [37].
In conclusion, an integrative approach that combines clinical parameters with biomarkers is being investigated for OA. However, potential biomarkers remain currently to be validated.
Genetic Markers in Occupational Asthma
The genetic mechanisms behind complex diseases, such as OA, are derived from multiple genes with minor effects. This means that candidate gene approaches are not sufficient to understand the pathogenesis of these kinds of diseases. Other hypothesis-free approaches like genome-wide association studies could help clarify these genetic mechanisms as they screen hundreds of thousands of single nucleotide polymorphisms (SNPs) simultaneously using microarray systems [45, 46]. To facilitate the understanding of the described genetic markers, we are addressing LMW- and HMW-induced OA separately. They are all summarized in Table 1.
OA Caused by LMW Agents
The best-studied model is the occupational exposure to isocyanates, mainly TDI, and only a small proportion of subjects exposed to isocyanates develop OA, suggesting the presence of some susceptibility factors.
Human Leukocyte Antigen Allele Studies
Human leukocyte antigen (HLA) is a genomic region located at chromosome 6p21, which encodes for six HLA “classical” genes as well as other “non-classical” HLA genes [69]. HLA class II genes, whose molecules (HLA-DR, HLA-DQ, and HLA-DP) are involved in binding antigen-derived peptides and their presentation to T lymphocytes, have been involved in TDI-induced OA [47]. Bignon et al. reported that European workers harboring HLA-DQB1*0503 and the allelic combination DQB1*0201/0301 were at increased risk of TDI-OA [48]. Balboni et al. obtained similar results among unrelated Italian Caucasian workers with TDI-OA, TDI-exposed subjects without OA, and unexposed normal subjects [49]. There was a significant positive association between the disease and HLA-DQB1*0503 and a protective association between the disease and HLA-DQB1*0501, which differed in just one single position. These findings were later confirmed in a similar population [47], although not by Rihs et al. [70]. However, in this last study, subjects were exposed to different types of isocyanates, not only TDI, confirmed diagnosis mainly through symptoms, and used airway resistance instead of spirometry to determine airway responsiveness. Furthermore, there are important differences in HLA associations, according to geographical influence. Those associations described in European populations differ from those published in Asians. The HLA haplotype associated with TDI-OA in Korean populations is DRB1*1501-DQB1*0602-DPB1*0501 [51]. Yucesoy et al. investigated the association between SNPs located across the major histocompatibility complex and susceptibility to diisocyanate (DI)-induced OA [52]. There were associations between an increased risk of DI-OA HLA-E rs1573294, HLA-DPB1 rs928976, HLA-B rs1811197, HLA-DOA rs3128935, and HLA-DQA2 rs7773955 SNPs.
For other LMW agents, a higher frequency of HLA DQB1*0603 and DQB1*0302 alleles and a reduced frequency of the DQB1*0501 allele have been reported in western red cedar sawmill workers with OA when compared with healthy workers [50]. Among chemical workers exposed to organic anhydrides, HLA class II allele DQB1*0501 was associated with increased IgE sensitization [71].
CTNNA3 (Alpha-T Catenin)
Currently, the strongest genetic marker of TDI-OA is α-catenin. Two different studies, conducted on populations of different genetic backgrounds, Koreans and Caucasians [45, 53••], have replicated results. CTNNA3 is the gene coding for α-catenin, located on chromosome 10q21.3. α-Catenin is a key protein of the adherence junctional complex in epithelial cells and plays an important role in cellular adherence. This protein is primarily expressed in the testes and heart, with low-level expression in several other tissues, including the brain [72, 73].
Two SNPs of the CTNNA3 gene (rs10762058 and rs7088181) showed significant associations with TDI-OA in two independent studies performed with 84 patients and 263 unexposed healthy controls from Korea [47] and 130 patients vs. 131 unexposed healthy controls of Caucasian origin [53••]. These two SNPs are in strong linkage disequilibrium, and the minor haplotype HT2 /GG/ carriers had significantly lower PC20 methacholine levels than in non-carrier subjects, suggesting that genetic polymorphisms of CTNNA3 confer a risk of TDI-OA through increased airway hyper-responsiveness to methacholine due to airway inflammation. Likewise, Kim et al. found significantly lower CTNNA3 mRNA expression in carriers with the minor haplotype HT2 compared with non-carriers. This led the authors to speculate that downregulation of CTNNA3 in genetic polymorphisms might disturb the defense systems of the airway epithelium in stressful environments, such as exposure to TDI [45]. Another SNP located in the 3′ downstream region (rs1786929) has been significantly associated with the development of TDI-induced OA. Those subjects with /TC/ or /CC/ genotypes showed significantly higher IgG against cytokeratin 19 than those having a /TT/ genotype [45]. However, this last result was not replicated in a Caucasian population [53••].
Antioxidant Gene Polymorphisms
A number of enzymatic antioxidants, including glutathione S-transferases (GSTs), manganese superoxide dismutase (SOD2), and microsomal epoxide hydrolase (EPHX1), play a major protective role in redox imbalance in the lung as well as help regulate inflammatory responses [74, 75]. Because oxidative stress is an important early event in the pathway for DI-induced respiratory damage, genetic variability within genes coding for antioxidant defense systems might directly influence the ultimate expression of OA.
Glutathione S-Transferases
It is a group of three enzymes: GSTM1 (chromosome 1p13.3), GSTP1 (chromosome 11q13), and GSTT1 (chromosome 22q11.2). There is a good rationale to explore GST genotypes as GSTs modify the biotransformation of isocyanates and excretion of metabolic products [76], and reduced glutathione directly inhibits in vitro binding of DI with albumin [77]. GSTP1 is the most highly expressed GST in the respiratory epithelium. The Ile105Val substitution in GSTP1 (rs1695) has been reported to alter the kinetics of the enzyme, and minor allele homozygosity (Val105/Val105) was shown to confer a protective effect on asthma [78, 79]. However, reports on the role of this variant in OA are inconsistent. Mapp et al. reported a protective effect of the Val105 allele against TDI-OA [54]. Consistently, Yucesory et al. found a reduced risk for DI-OA in workers with the Val105 allele in comparison with asymptomatic exposed workers. This author also found that GSTP1 rs762803 was a risk factor of DI-OA, when comparing subjects with a positive SIC vs. a negative one [55], whereas Piirilä et al. did not find such effect in workers exposed to TDI, hexamethylene diisocyanate (HDI), and MDI [56]. Nevertheless, the functional consequence of this last SNP is unknown.
Regarding GSTM1 and GSTT1 enzymes, both are expressed weakly in the lungs [80, 81]. Null alleles of GSTM1 and GSTT1 genes in homozygosis result in the complete absence of enzyme activity and confer susceptibility to atopic bronchial and childhood asthma [82–84]. Moreover, GSTM1 null genotype was associated with increased risk of TDI-OA [56]. On the contrary, Yucesoy et al. found that the null allele of GSTM1 was associated with a reduced risk of DI-OA, according to the result in the SIC [55]. Data regarding GST enzymes are still controversial and inconsistent.
Manganese Superoxide Dismutase
SOD2 enzyme (chromosome 6q25.3) is an essential first line of defense against superoxide formed by the tetravalent reduction of oxygen during mitochondrial electron transport and catalyzes the dismutation of superoxide radicals into hydrogen peroxide. SOD2, one of the three known isoforms of SOD, is unique in that it is inducible by stimuli that cause oxidative stress [85]. The SOD2 gene contains a single nucleotide polymorphism (rs4880 SNP) that results in an Ala → Val substitution, which decreases the activity of SOD2. The rs4880 SNP has been widely studied and found to be associated with several respiratory diseases, including childhood asthma [86] and bronchial hyperresponsiveness [87]. The homozygous minor allele of SOD2 rs4880 has been associated with a higher risk of DI-OA, although only when comparing positive and negative SICs, but not when comparing subjects with positive SIC vs. asymptomatic exposed workers [55].
Microsomal Epoxide Hydrolase
EPHX1 (chromosome 1q42.1) is involved in the detoxification of epoxides and expressed in most tissues, including the airway epithelium. Two common variations located in exon 3 (Tyr113His, rs1051740) and exon 4 (His139Arg, rs2234922) have been reported to reduce and increase in vitro enzyme activity, respectively [88]. More recently, these variants have been associated with asthma, among other respiratory diseases [89]. Moreover, Yucesoy et al. analyzed eight SNPs in the EPHX1 gene and found that the minor allele of EPHX1 rs28544502 SNP conferred protection against DI-OA when compared with patients SIC+ and SIC− [55]. On the other hand, the carrier of the minor alleles for EPHX1 rs1051741 and for EPHX1 rs2740171 conferred an increased risk of DI-OA, comparing DI-OA confirmed by SIC vs. asymptomatic exposed workers.
N-Acetyltransferases
N-acetyltransferase (NAT) enzymes are involved in the activation/inactivation of numerous xenobiotics. The NAT1 and NAT2 genes are both located on chromosome 8 (8p21.3–23.1 and 8p21.3–23.1 and 8p22, respectively) and catalyze the N-acetylation and O-acetylation of aromatic and heterocyclic amines [90]. They are also involved in the deactivation of pro-inflammatory cysteinyl-LT, which are potent mediators of airway narrowing [91]. Both NAT1 and NAT2 are expressed in the airway epithelium and show wide inter-individual variation [92]. NATs are also known to be involved in the deactivation of aromatic amines that can be formed from DI in aqueous environments [93]. Because oxidative stress is an important early event in DI-induced respiratory damage, genetic modification of the enzymatic activity of NATs could directly influence the expression of the disease.
Yucesoy et al. studied 18 SNPs within the NAT1 and NAT2 genes on 132 DI-OA French Caucasian patients and 148 HDI-exposed asymptomatic workers [57]. NAT2 rs2410556 and rs4271002 were individually significantly associated with the DI-OA diagnosis in the univariate analysis. In the logistic regression model comparing asthmatics and asymptomatic worker groups, rs2410556 (p = 0.004) and rs4271002 (p < 0.001) single nucleotide polymorphisms and the genotype combination, NAT2 rs4271002*NAT1rs11777998, showed associations with DI-OA risk (p = 0.014). In a second model, comparing only confirmed DI-OA, the NAT2 rs4271002 variant and the combined genotype, NAT1 rs8190845*NAT2 rs13277605, were significantly associated with DI-OA risk (p = 0.022 and p = 0.036, respectively) [57].
Th2 Gene Markers
A candidate gene study was performed in 103 isocyanate-exposed workers with DA confirmed by a positive SIC test, 115 symptomatic workers with negative SIC tests, and 150 asymptomatic spray painters exposed to HDI [94]. As Th2 cytokine gene polymorphisms of IL-4 receptor alpha (IL-4RA) and IL-13 have been associated with allergic asthma and/or allergic sensitization, workers were genotyped for IL-4RA (I50V), IL-4RA (Q551R), IL-4RA (E375A), IL-13 (R110Q), and CD14 (C159T) SNPs. Specific genotype combinations (i.e., IL-4RA II + IL-13 RR, IL-4RA II + CD14 CT, and IL-4RA II + IL-13 RR + CD14 CT) were associated with DI-OA compared with SIC-negative workers, but only among HDI-exposed workers. When comparing HDI-exposed workers with DI-OA (n = 50) and a group of asymptomatic HDI-exposed workers (n = 150), the association between DI-OA and the IL-4RA II + CD14 CT and IL-4RA II + IL-13 RR + CD14 CT genotype combinations trended toward statistical significance (p < 0.10) after adjustment for relevant confounding variables [95, 96].
Inflammatory Response Genes
A recent study analyzed SNPs on genes selected based on their role in asthmatic inflammatory processes and previously reported associations with asthma phenotypes [58]. These genes were TNF-α, IL-1α, IL-1β, IL-1RN, IL-10, TGF-β1, ADAM33, ALOX-5, PTGS1, PTGS2, and NAG-1/GDF15. Most of the SNPs analyzed were not significantly associated with DA. However, TNFα rs1800629 and PTGS2 rs20417 SNPs conferred an increased risk of DA in a group of Caucasian French Canadians, whereas TGFB1 rs1800469 and PTGS1 rs5788 showed a protective effect [58].
Epigenetic Marker: Interferon-γ Promoter Methylation
Promoter methylation is an epigenetic modification of gene expression. Environmental exposures may influence disease expression through modification of promoter regions, downregulating gene transcription by this novel mechanism. A statistically significant increase in the methylation of the IFN-γ promoter in DI-OA has been described compared with both exposed workers with lower respiratory symptoms and negative specific inhalation test and asymptomatic exposed workers [59•]. Subset analysis showed that IFN-γ methylation was significantly associated with the DA status in subgroups such as non-smokers, workers with absence of airway hyper-responsiveness (defined as PC20 = 32 mg/ml), male gender, or workers with MDI exposure only. According to the ROC analysis, the sensitivity was 77.5 % and the specificity was 80 % for identifying DA workers in a multivariate predictive model after adjusting for type of DI exposure, smoking status, methacholine PC20, and gender. However, this finding has to be replicated in patients with different ethnic backgrounds and longitudinal studies to test its capacity in predicting the risk of DI-OA.
OA Caused by HMW Agents
Toll-Like Receptors and CD14 Polymorphisms in Animal Workers Exposed to Indoor Dust and Endotoxin
Occupational exposure to organic dust has been shown to be associated with chronic airways disease, and endotoxin, present in organic dust, appears to be a major causative agent contributing to airway inflammation and obstruction [97]. Gao et al. investigated the association between Toll-like receptors TLR2 and TLR4 polymorphisms and OA in 374 Canadian swine operators [60]. TLR2 recognizes ligands from Gram-positive bacteria, whereas TLR4 responds to endotoxin from Gram-negative bacteria. Workers with genotype /AA/ in TLR2-16933 T/A polymorphism had significantly greater mean values of lung function tests than workers with wild-type genotypes (/AT/ or /TT/). This result was also observed for TLR2− Arg677Trp polymorphism among the workers. No such significant differences were observed for Asp299Gly and Thr399Ile polymorphisms in the TLR4 gene. The authors suggested that TLR2 polymorphisms might be protective of airway disease in individuals exposed to Gram-positive organisms in the inhaled airborne dust. However, Pacheco et al. found that the TLR4-8551 G variant, which is less responsive to endotoxin, was significantly associated with a higher risk of atopy and laboratory animal sensitization in a group of 335 workers [98]. Nevertheless, these TLR4 variants were not predictors of laboratory animal-induced symptoms.
CD14 is a co-receptor, in association with TLR4 and MD-2, for the detection of bacterial lipopolysaccharides (endotoxin). In a study including Caucasian laboratory animal workers, more highly endotoxin-exposed workers with CD14-1619 G alleles had significantly lower FEV1 and FEF25–75 percentages predicted than those with CD14-1619AA [61]. Atopic workers were particularly affected by cumulative endotoxin exposures.
Microsomal Epoxide Hydrolase Polymorphisms in Cotton Textile Workers (Endotoxin-Exposed)
Microsomal epoxide hydrolase (mEH) is an enzyme which catalyzes the hydrolysis of reactive oxidative species generated by endotoxin exposure into less reactive and more hydrosoluble compounds. In the coding region of the mEH gene, two relatively common genetic polymorphisms are characterized. In exon 3, the Tyr113His (C113T) polymorphism results in a 40–50 % decrease in enzyme activity, and thus, the His allele has been called the “slow allele.” In exon 4, the His139Arg (G139A) polymorphism is associated with a 25 % increase of enzyme activity, with the Arg allele termed the “fast allele” [88]. Hang et al. investigated whether polymorphisms in mEH modify the association between endotoxin exposure and faster decline in lung function in a 20-year prospective cohort study of 265 cotton textile mill workers (endotoxin-exposed) and 234 silk workers (non-endotoxin-exposed) in Shanghai, China [62]. Endotoxin exposure was associated with a faster decline in lung function among subjects with “slow” mEH genotypes (His/His) over 20 years compared to non-endotoxin-exposed workers. An annual difference of −6.7 ml/year was observed.
ADRβ2, TLR4, IL-18, IL-4Rα, IL-13, and CD14 in Baker’s Asthma
Israel et al. studied a Korean cohort of bakery workers to identify genetic loci associated with susceptibility to baker’s asthma [63]. Several candidate SNPs in β2-adrenergic receptor (ADRβ2), TLR4, IL-18, and IL-4Rα were analyzed based upon known pathogenic mechanisms. A haplotype of three ADRB2 SNPs (GAA composed of 46 A/G, 252 A/G, and 523 A/C) was found to be significantly associated with work-related respiratory symptoms in bakery workers. Among the IL-18 SNPs, genotypes of −137 G/C promoter (GC or CC) and its haplotype ht3 /ACC/ were significantly associated with the rate of sensitization to wheat flour [99]. A subsequent study focused primarily on TLR4 genetic polymorphisms (homozygotes for the −2027 G and −1608 C and haplotype 2 /GC/) revealed a significant protective association between genetic polymorphisms and risk of work-related respiratory symptoms [64]. A mutant allele of IL-4Rα Ile75Val A/G was associated with a higher prevalence of work-related respiratory symptoms, whereas the wild-type IL-4Rα allele Gln576Arg A/G was associated with higher sensitization to wheat flour [65].
Acouetey et al. examined genetic susceptibility loci in 351 bakery apprentices in France [100]. IL-13 R130Q/IL-4Rα S478P or IL-13 R130Q/IL-4Rα Q551R were significant predictors of decreased lung functions in bakery workers. These findings suggest that genetic polymorphisms in innate immune response genes, such as TLR4, were potential markers for work-related respiratory symptoms in bakery workers, whereas genetic polymorphisms of IL-4Rα/IL-13 might be genetic markers for increased sensitization to wheat flour and development of work-related respiratory symptoms. Recently, Marraccini et al. identified a polymorphism in CD14 (rs2569190) that might be differentially expressed in Italian bakery workers (p = 0.06) [66]. The /TT/ genotype was more frequent among occupational asthma or rhinitis group than healthy controls or an atopic group.
HLA in Animal Workers
Jeal et al. performed HLA typing for the DRB1 and DQB1 loci in 109 laboratory workers sensitized to rat proteins and 397 referents [67]. HLA-DR7 was significantly associated with sensitization (OR = 1.82), respiratory symptoms at work (OR = 2.96), and sensitization combined with symptoms (OR = 3.8), whereas workers with HLA-DR3 were less likely to be sensitized. In Finish asthmatic farmers allergic to cow dander and sensitized to Bos d 2, the HLA-DR/DQ genotypes were determined and compared with the genotypes of 151 unrelated controls. The frequencies of HLA class II alleles DRB1*0101, DRB1*0404, DQB1*0302, and DQB1*0501 were significantly higher among Bos d 2-sensitized than among controls. In addition, the allergic subjects expressed significantly lower frequencies of HLA-DRB1*0301 and DQB1*0201 alleles than did the control subjects [68].
Conclusions
Currently, the best-known biomarkers in OA are those associated with lower airway inflammation, particularly of the eosinophilic type (cell counts in induced sputum and FeNO levels). FeNO can be helpful in the diagnosis of OA, particularly to rule in asthma, and it might play a role in the management of OA patients, but its real value in the assessment of OA remains controversial. Induced sputum could be considered as a consolidated and helpful tool in the diagnosis and follow-up of OA patients. Unfortunately, it is not easily accessible in many centers.
Candidate gene association studies have failed to identify reliable predictors of OA, probably due to the low case frequencies of OA syndromes and the intrinsic limitations of candidate gene methodological approaches. Future investigations including genome-wide association studies might be able to identify high-risk genotypes. Furthermore, gene expression profiling in human cells or with biologic specimens obtained from exposed workers with OA might assist in the identification of biologically relevant genes.
There is a clear need to identify potential biomarkers related with work-related respiratory disorders. Further research is needed, including longitudinal studies, to find reliable biological and genetic markers for OA.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Tarlo SM, Lemiere C. Occupational asthma. N Engl J Med. 2014;370:640–9.
Moscato G, Pala G, Barnig C, De Blay F, Del Giacco SR, Folletti I, et al. EAACI Consensus statement for investigation of work-related asthma in non-specialized centres. Allergy. 2012;67:491–501.
Vandenplas O, Wiszniewska M, Raulf M, de Blay F, Gerth van Wijk R, Moscato G, et al. EAACI position paper: irritant-induced asthma. Allergy. 2014;69:1141–53.
Dufour MH, Lemiere C, Prince P, Boulet LP. Comparative airway response to high versus low-molecular weight agents in occupational asthma. Eur Respir J. 2009;33:734–9.
Vandenplas O, Suojalehto H, Aasen TB, Baur X, Burge PS, de Blay F, et al. ERS Task Force Report on Occupational Asthma. Specific inhalation challenge in the diagnosis of occupational asthma: consensus statement. Eur Respir J. 2014;43:1573–87. This consensus statement provides practical recommendations for specific inhalation challenge in the diagnosis of occupational asthma derived from a systematic literature search, a census of active European centres, a Delphi conference, and expert consensus.
Quirce S. Eosinophilic bronchitis in the workplace. Curr Opin Allergy Clin Immunol. 2004;4:87–91.
Quirce S, Lemière C, De Blay F, Del Pozo V, Gerth van Wijk R, Maestrelli P, et al. EAACI Task Force Consensus Report. Non-invasive methods for assessment of airway inflammation in occupational settings. Allergy. 2010;65:445–58.
Lemière C, D’Alpaos V, Chaboillez S, César M, Wattiez M, Chiry S, et al. Investigation of occupational asthma sputum cell counts or exhaled nitric oxide? Chest. 2010;137:617–22.
Raulf-Heimsoth M, Liebig R, Marczynsky B, Borowitzki G, Bernard S, Freundt S, et al. Implementation of non-invasive methods in the diagnosis of diisocyanate-induced asthma. Adv Exp Med Biol. 2013;788:293–300.
Lemière C, Chaboillez S, Malo JC, Cartier A. Changes in sputum cell counts alters exposure to occupational agents: what do they mean? J Allergy Clin Immunol. 2001;107:1063–8.
Vandenplas O, D’Alpaos HJ, Jamart J, Thimpont J, Huaux F, et al. Sputum eosinophilia: an early marker of bronchial response to occupational agents. Allergy. 2009;64:754–61.
Malo JL, Cardinal S, Ghezzo H, L’Archeveche J, Castellanos L, Maghni K. Association of bronchial reactivity to occupational agents with methacholine reactivity, sputum cells and immunoglobulin E-mediated reactivity. Clin Exp Allergy. 2011;41:497–504.
Sánchez-Vidaurre S, Cruz MJ, Gómez-Ollés S, Morel F, Muñoz X. Sputum inflammatory profile before and after specific inhalation challenge in individuals with suspected occupational asthma. PLoS One. 2013;8:e78304. This is the first study comparing inflammatory cell percentages and inflammatory markers in sputum samples of subjects with and without occupational asthma and between HMW- and LMW-induced asthma.
Prince P, Lemière C, Dufour MH, Chaboillez S, Boulet LP. Airway inflammatory responses following exposure to occupational agents. Chest. 2012;141:1522–7.
Leigh R, Hargreave FE. Occupational neutrophilic asthma. Can Respir J. 1999;6:194–6.
Pala G, Pignatti P, Moscato G. Occupational exposure to toluene diisocyanate and neutrophilic bronchitis without asthma. Clin Toxicol. 2011;49:506–7.
Essat M, Harnan S, Gomersall T, Tappenden P, Wong R, Pavord I, et al. Fractional exhaled nitric oxide for the management of asthma in adults: a systematic review. Eur Respir J. 2016;47:751–68.
Piipari R, Piirila P, Keskinen H, Tuppurainen M, Sovijarvi A, Nordmana H. Exhaled nitric oxide in specific challenge tests to assess occupational asthma. Eur Respir J. 2002;20:1532–7.
Lemiere C, Nguyen S, Sava F, D’Alpaos V, Huaux F, Vandenplas O. Occupational asthma phenotypes identified by increased fractional exhaled nitric oxide after exposure to causal agents. J Allergy Clin Immunol. 2014;134:1063–7. Statistical cluster analysis was realized in a prospective observational study that included subjects who had been investigated for possible occupational asthma.
Ferrazoni S, Scarpa MC, Guarnieri G, Corraldi M, Mutti A, Maestrelli P. Exhaled nitric oxide and breath condensate pH in asthmatic reactions induced by isocyanates. Chest. 2009;136:155–62.
Pedrosa M, Barranco P, Lopez-Carrasco V, Quirce S. Changes in exhaled nitric oxide levels after bronchial allergen challenge. Lung. 2012;190:209–14.
Sastre J, Costa C, Garcia del Potro M, Aguado E, Mahillo I, Férnandez-Nieto M. Changes in exhaled nitric oxide after inhalation challenge with occupational agents. J Investig Allergol Clin Immunol. 2013;23:421–7.
Walters GI, Moore VC, McGrath EE, Burge S. Fractional exhaled nitric oxide in the interpretation of specific inhalational challenge tests for occupational asthma. Lung. 2014;192:119–24.
Swierczynska-Machura D, Krakowiak A, Wiszniewska M, Dudek W, Walusiak J, Palczynski C. Exhaled nitric oxide levels after specific inhalatory challenge test in subjects with diagnosed occupational asthma. Int J Occup Med Environ Health. 2008;21:219–25.
Vandenplas O, D’Alpaos V, Evrard G, Jamart J, Thimpont J, Huaux F, et al. Asthma related to cleaning agents: a clinical insight. BMJ Open. 2013;3:e003568.
Talini D, Novelli F, Bacci E, Bartoli M, Cianchetti S, Costa F, et al. Sputum eosinophilia is a determinant of FEV1 decline in occupational asthma: results of an observational study. BMJ Open. 2015;5:e005748. In this study, higher baseline sputum levels could appear as a possible determinant of the decline in FEV1 in patients with OA who continued at work. Although the number of patients examined is relatively small, the study suggests that higher levels of inflammation may cause an accelerated decline in FEV1.
Kleniewska A, Walusiak-Skorupa J, Piotrowski W, Nowakowska-Swirta E, Wiszniewska M. Comparison of biomarkers in serum and induced sputum of patients with occupational asthma and chronic obstructive pulmonary disease. J Occup Health 2016;58:333–9.
Castano R, Miedinger D, Maghni K, Ghezzo H, Trudeau C, Castellanos L, et al. Matrix metalloproteinase-9 increases in the sputum from allergic occupational asthma patients after specific inhalation challenge. Int Arch Allergy Immunol. 2013;160:161–4.
Baatjies R, Jeebhay MF. Sensitization to cereal flour allergens is a major determinant of elevated exhaled nitric oxide in bakers. Occup Environ Med. 2013;70:310–6.
Tafuro F, Ridolo E, Goldoni M, Montagni M, Mutti A, Corradi M. Work-related allergies to storage mites in Parma (Italy) ham workers. BMJ Open. 2015;5:e007502.
Van der Walt A, Baatjies, Singh T, Jeebhay MF. Environmental factors associated with baseline and serial changes in fractional exhaled nitric oxide (FeNO) in spice mill workers. Occup Environ Med. 2016. doi:10.1136/oemed-2015-103005.
Jonaid BS, Pronk A, Doekes G, Heederik D. Exhaled nitric oxide in spray painters exposed to isocyanates: effect modification by atopy and smoking. Occup Environ Med. 2014;71:415–22.
Shiryaeva O, Aasmoe L, Straume B, Bang BE. Respiratory symptoms, lung functions and exhaled nitric oxide (FeNO) in two types of fish processing workers: Russian trawler fishermen and Norwegian salmon industry workers. Int J Occup Environ Health. 2015;21:53–60.
Vizcaya D, Mirabelli MC, Orriols R, Antó JM, Barreiro E, Burgos F, et al. Functional and biological characteristics of asthma in cleaning workers. Respir Med. 2013;107:673–83.
Hur GY, Park HS. Biological and genetic markers in occupational asthma. Curr Allergy Asthma Rep. 2015;15:488.
Kim MH, Jung JW, Kang HR. The usefulness of job relocation and serum eosinophil cationic protein in baker’s asthma. Int Arch Allergy Immunol. 2013;161:252–7.
Pelclová D, Fenclová Z, Vlcková S, Klusachová P, Levedová P, Syslová K, et al. Occupational asthma follow-up: which markers are elevated in exhaled breath condensate and plasma? Int J Occup Med Environ Health. 2014;27:205–15.
Palczynski C, Walusiak J, Ruta U, Górski P. Occupational asthma and rhinitis due to glutaraldehyde: changes in nasal lavage fluid after specific inhalatory challenge test. Allergy. 2001;56:1186–91.
Castano R, Thériault G, Maghni K, Ghezzo H, Malo JL, Gautrin D. Reproducibility of nasal lavage in the context of the inhalation challenge investigation of occupational rhinitis. Am J Rhinol. 2008;22:271–5.
Beach J, Russell K, Blitz S, Hooton N, Spooner C, Lemiere C, et al. A systematic review of the diagnosis of occupational asthma. Chest. 2007;131:569–78.
Sastre J, Sastre B, Fernández-Nieto M, et al. Serum ferritin and transferrin levels are not serologic markers of toluene diisocyanate-induced occupational asthma. J Allergy Clin Immunol. 2010;125:762–4.
Palikhe NS, Kim JH, Park HS. Biomarkers predicting isocyanate-induced asthma. Allergy, Asthma Immunol Res. 2011;3:21–6.
Kim SH, Choi GS, Nam YH, et al. Role of vitamin D-binding protein in isocyanate-induced occupational asthma. Exp Mol Med. 2012;44:319–29.
Czerska M, Zielinski M, Gromadzinska J. Isoprostanes—a novel major group of oxidative stress markers. Int J Occup Med Environ Health. 2016;29:179–90.
Kim SH, Cho BY, Park CS, Shin ES, Cho EY, Yang EM, et al. Alpha-T-catenin (CTNNA3) gene was identified as a risk variant for toluene diisocyanate-induced asthma by genome-wide association analysis. Clin Exp Allergy. 2009;39:203–12.
Yucesoy B, Kaufman KM, Lummus ZL, Weirauch MT, Zhang G, Cartier A, et al. Genome-wide association study identifies novel loci associated with diisocyanate-induced occupational asthma. Toxicol Sci. 2015;146:192–201.
Mapp CE, Beghe B, Balboni A, Zamorani G, Padoan M, Jovine L, et al. Association between HLA genes and susceptibility to toluene diisocyanate-induced asthma. Clin Exp Allergy. 2000;30:651–6.
Bignon JS, Aron Y, Ju LY, Kopferschmitt MC, Garnier R, Mapp C, et al. HLA class II alleles in isocyanate-induced asthma. Am J Respir Crit Care Med. 1994;149:71–5.
Balboni A, Baricordi OR, Fabbri LM, Gandini E, Ciaccia A, Mapp CE. Association between toluene diisocyanate-induced asthma and DQB1 markers: a possible role for aspartic acid at position 57. Eur Respir J. 1996;9:207–10.
Horne C, Quintana PJ, Keown PA, Dimich-Ward H, Chan-Yeung M. Distribution of DRB1 and DQB1 HLA class II alleles in occupational asthma due to western red cedar. Eur Respir J. 2000;15:911–4.
Choi JH, Lee KW, Kim CW, Park CS, Lee HY, Hur GY, et al. The HLA DRB1*1501-DQB1*0602-DPB1*0501 haplotype is a risk factor for toluene diisocyanate-induced occupational asthma. Int Arch Allergy Immunol. 2009;150:156–63.
Yucesoy B, Johnson VJ, Lummus ZL, Kashon ML, Rao M, Bannerman-Thompson H, et al. Genetic variants in the major histocompatibility complex class I and class II genes are associated with diisocyanate-induced asthma. J Occup Environ Med. 2014;56:382–7.
Bernstein DI, Kashon M, Lummus ZL, Johnson VJ, Fluharty K, Gautrin D, et al. CTNNA3 (α-catenin) gene variants are associated with diisocyanate asthma: a replication study in a Caucasian worker population. Toxicol Sci. 2013;131:242–6. First genetic marker consistently replicated in two populations from different genetic background.
Mapp CE, Fryer AA, De Marzo N, Pozzato V, Padoan M, Boschetto P, et al. Glutathione S-transferase GSTP1 is a susceptibility gene for occupational asthma induced by isocyanates. J Allergy Clin Immunol. 2002;109:867–72.
Yucesoy B, Johnson VJ, Lummus ZL, Kissling GE, Fluharty K, Gautrin D, et al. Genetic variants in antioxidant genes are associated with diisocyanate-induced asthma. Toxicol Sci. 2012;129:166–73.
Piirilä P, Wikman H, Luukkonen R, Kääriä K, Rosenberg C, Nordman H, et al. Glutathione S-transferase genotypes and allergic responses to diisocyanate exposure. Pharmacogenetics. 2001;11:437–45.
Yucesoy B, Kissling GE, Johnson VJ, Lummus ZL, Gautrin D, Cartier A, et al. N-acetyltransferase 2 genotypes are associated with diisocyanate-induced asthma. J Occup Environ Med. 2015;57:1331–6.
Yucesoy B, Kashon ML, Johnson VJ, Lummus ZL, Fluharty K, Gautrin D, et al. Genetic variants in TNFα, TGFβ1, PTGS1 and PTGS2 genes are associated with diisocyanate-induced asthma. J Immunotoxicol. 2016;13:119–26.
Ouyang B, Bernstein DI, Lummus ZL, Ying J, Boulet LP, Cartier A, et al. Interferon-γ promoter is hypermethylated in blood DNA from workers with confirmed diisocyanate asthma. Toxicol Sci. 2013;133:218–24. First epigenetic modification suggested as possible diagnostic marker.
Gao Z, Dosman JA, Rennie DC, Schwartz DA, Yang IV, Beach J, et al. Association of Toll-like receptor 2 gene polymorphisms with lung function in workers in swine operations. Ann Allergy Asthma Immunol. 2013;110:44–50.
Pacheco K, Rose C, Silveira LJ, van Dyke M, Goelz K, Macphail K, et al. Gene–environment interactions influence airways function in laboratory animal workers. J Allergy Clin Immunol. 2010;126:232–40.
Hang J, Zhou W, Wang X, Zhang H, Sun B, Dai H, et al. Microsomal epoxide hydrolase, endotoxin, and lung function decline in cotton textile workers. Am J Respir Crit Care Med. 2005;171:165–70.
Israel E, Chinchilli VM, Ford JG, Boushey HA, Cherniack R, Craig TJ, et al. Use of regularly scheduled albuterol treatment in asthma: genotype-stratified, randomised, placebo-controlled cross-over trial. Lancet. 2004;364:1505–12.
Cho HJ, Kim SH, Kim JH, Choi H, Son JK, Hur GY, et al. Effect of Toll-like receptor 4 gene polymorphisms on work-related respiratory symptoms and sensitization to wheat flour in bakery workers. Ann Allergy Asthma Immunol. 2011;107:57–64.
Hur GY, Ye YM, Koh DH, Kim SH, Park HS. IL-4 receptor α polymorphisms may be a susceptible factor for work-related respiratory symptoms in bakery workers. Allergy, Asthma Immunol Res. 2013;5:371–6.
Marraccini P, Cantone L, Barretta F, Marsili C, Leghissa P, Santini M, et al. Inflammatory markers and genetic polymorphisms in workers exposed to flour dust. J Occup Environ Med. 2016;58:e166–70.
Jeal H, Draper A, Jones M, Harris J, Welsh K, Taylor AN, et al. HLA associations with occupational sensitization to rat lipocalin allergens: a model for other animal allergies? J Allergy Clin Immunol. 2003;111:795–9.
Kauppinen A, Peräsaari J, Taivainen A, Kinnunen T, Saarelainen S, Rytkönen-Nissinen M, et al. Association of HLA class II alleles with sensitization to cow dander Bos d 2, an important occupational allergen. Immunobiology. 2012;217:8–12.
Shiina T, Inoko H, Kulski JK. An update of the HLA genomic region, locus information and disease associations. Tissue Antigens. 2004;64:631–49.
Rihs HP, Barbalho-Krölls T, Huber H, Bau X. No evidence for the influence of HLA class II in alleles in isocyanate-induced asthma. Am J Ind Med. 1997;32:522–7.
Jones MG, Nielsen J, Welch J, Harris J, Welinder H, Bensryd I, et al. Association of HLA-DQ5 and HLA-DR1 with sensitization to organic acid anhydrides. Clin Exp Allergy. 2004;34:812–6.
Janssens B, Mohapatra B, Vatta M, Goossens S, Vanpoucke G, Kools P, et al. Assessment of the CTNNA3 gene encoding human alpha T-catenin regarding its involvement in dilated cardiomyopathy. Hum Genet. 2003;112:227–36.
Janssens B, Goossens S, Staes K, Gilbert B, van Hengel J, Colpaert C, et al. AlphaT-catenin: a novel tissue-specific beta-catenin-binding protein mediating strong cell–cell adhesion. J Cell Sci. 2001;114:3177–88.
Bowler RP. Oxidative stress in the pathogenesis of asthma. Curr Allergy Asthma Rep. 2004;4:116–22.
Rahman I, Biswas SK, Kode A. Oxidant and antioxidant balance in the airways and airway diseases. Eur J Pharmacol. 2006;533:222–39.
Littorin M, Hou S, Broberg K, Bjork J, Falt S, Abdoulaye G, et al. Influence of polymorphic metabolic enzymes on biotransformation and effects of diphenylmethane diisocyanate. Int Arch Occup Environ Health. 2008;81:429–4.
Wisnewski AV, Liu Q, Liu J, Redlich CA. Glutathione protects human airway proteins and epithelial cells from isocyanates. Clin Exp Allergy. 2005;35:352–7.
Fryer AA, Bianco A, Hepple M, Jones PW, Strange RC, Spiteri MA. Polymorphism at the glutathione S-transferase GSTP1 locus. A new marker for bronchial hyperresponsiveness and asthma. Am J Respir Crit Care Med. 2000;161:1437–42.
Aynacioglu AS, Nacak M, Filiz A, Ekinci E, Roots I. Protective role of glutathione S-transferase P1 (GSTP1) Val105Val genotype in patients with bronchial asthma. Br J Clin Pharmacol. 2004;57:213–7.
Anttila S, Hirvonen A, Vainio H, Husgafvel-Pursiainen K, Hayes JD, Ketterer B. Immunohistochemical localization of glutathione S-transferases in human lung. Cancer Res. 1993;53:5643–8.
Cantlay AM, Smith CA, Wallace WA, Yap PL, Lamb D, Harrison DJ. Heterogeneous expression and polymorphic genotype of glutathione S-transferases in human lung. Thorax. 1994;49:1010–4.
Ivaschenko TE, Sideleva OG, Baranov VS. Glutathione-S-transferase micro and theta gene polymorphisms as new risk factors of atopic bronchial asthma. J Mol Med. 2002;80:39–43.
Kabesch M, Hoefler C, Carr D, Leupold W, Weiland SK, von Mutius E. Glutathione S transferase deficiency and passive smoking increase childhood asthma. Thorax. 2004;59:569–73.
Karam RA, Pasha HF, El-Shal AS, Rahman HM, Gad DM. Impact of glutathione-S-transferase gene polymorphisms on enzyme activity, lung function and bronchial asthma susceptibility in Egyptian children. Gene. 2012;497:314–9.
Hassan HM. Biosynthesis and regulation of superoxide dismutases. Free Radic Biol Med. 1988;5:377–85.
Kuo Chou TN, Li YS, Lue KH, Liao CF, Lin Y, Tzeng PR, et al. Genetic polymorphism of manganese superoxide dismutase is associated with childhood asthma. J Asthma. 2010;47:532–8.
Siedlinski M, van Diemen CC, Postma DS, Vonk JM, Boezen HM. Superoxide dismutases, lung function and bronchial responsiveness in a general population. Eur Respir J. 2009;33:986–92.
Hassett C, Aicher L, Sidhu JS, Omiecinski CJ. Human microsomal epoxide hydrolase: genetic polymorphism and functional expression in vitro of amino acid variants. Hum Mol Genet. 1994;3:421–8.
Tung KY, Tsai CH, Lee YL. Microsomal epoxide hydroxylase genotypes/diplotypes, traffic air pollution, and childhood asthma. Chest. 2011;139:839–84.
Hein DW. Molecular genetics and function of NAT1 and NAT2: role in aromatic amine metabolism and carcinogenesis. Mutat Res. 2002;506–507:65–77.
Bateman ED, Hurd SS, Barnes PJ, Bousquet J, Drazen JM, FitzGerald M, et al. Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J. 2008;31:143–78.
Windmill KF, Gaedigk A, Hall PM, Samaratunga H, Grant DM, McManus ME. Localization of N-acetyltransferases NAT1 and NAT2 in human tissues. Toxicol Sci. 2000;54:19–29.
Bolognesi C, Baur X, Marczynski B, Norppa H, Sepai O, Sabbioni G. Carcinogenic risk of toluene diisocyanate and 4,4′-methylenediphenyl diisocyanate: epidemiological and experimental evidence. Crit Rev Toxicol. 2001;31:737–72.
Bernstein DI, Wang N, Campo P, Chakraborty R, Smith A, Cartier A, et al. Diisocyanate asthma and gene-environment interactions with IL4RA, CD-14, and IL-13 genes. Ann Allergy Asthma Immunol. 2006;97:800–6.
Bernstein DI, Kissling GE, Khurana-Hershey G, Yucesoy B, Johnson VJ, Cartier A, et al. Hexamethylene diisocyanate asthma is associated with genetic polymorphisms of CD14, IL-13, and IL-4 receptor alpha. J Allergy Clin Immunol. 2011;128:418–20.
Bernstein DI. Genetics of occupational asthma. Curr Opin Allergy Clin Immunol. 2011;11:86–9.
Gautrin D, Malo JL. Risk factors, predictors and markers for work-related asthma and rhinitis. Curr Allergy Asthma Rep. 2010;10:365–72.
Pacheco K, Maier L, Silveira L, Goelz K, Noteware K, Luna B, et al. Association of Toll-like receptor 4 alleles with symptoms and sensitization to laboratory animals. J Allergy Clin Immunol. 2008;122:896–902.
Kim SH, Hur GY, Jin HJ, Choi H, Park HS. Effect of interleukin-18 gene polymorphisms on sensitization to wheat flour in bakery workers. J Korean Med Sci. 2012;27:382–7.
Acouetey DS, Zmirou-Navier D, Avogbe PH, Tossa P, Rémen T, Barbaud A, et al. Genetic predictors of inflammation in the risk of occupational asthma in young apprentices. Ann Allergy Asthma Immunol. 2013;110:423–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Drs. Dominguez-Ortega, Barranco, Rodríguez-Pérez, and Quirce declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Occupational Allergies
Rights and permissions
About this article
Cite this article
Dominguez-Ortega, J., Barranco, P., Rodríguez-Pérez, R. et al. Biomarkers in Occupational Asthma. Curr Allergy Asthma Rep 16, 63 (2016). https://doi.org/10.1007/s11882-016-0644-3
Published:
DOI: https://doi.org/10.1007/s11882-016-0644-3