Abstract
Purpose
Functional dependency is a known determinant of surgical risk. To enhance our understanding of the relationship between dependency and adverse surgical outcomes, we studied how postoperative mortality following a surgical complication was impacted by preoperative functional dependency.
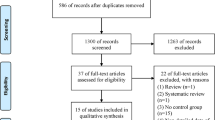
Methods
We explored a historical cohort of 6,483,387 surgical patients within the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP). All patients ≥ 18 years old within the ACS-NSQIP from 2007 to 2017 were included.
Results
There were 6,222,611 (96.5%) functionally independent, 176,308 (2.7%) partially dependent, and 47,428 (0.7%) totally dependent patients. Within 30 days postoperatively, 57,652 (0.9%) independent, 15,075 (8.6%) partially dependent, and 10,168 (21.4%) totally dependent patients died. After adjusting for confounders, increasing functional dependency was associated with increased odds of mortality (Partially Dependent OR: 1.72, 99% CI: 1.66 to 1.77; Totally Dependent OR: 2.26, 99% CI: 2.15 to 2.37). Dependency also significantly impacted mortality following a complication; however, independent patients usually experienced much stronger increases in the odds of mortality. There were six complications not associated with increased odds of mortality. Model diagnostics show our model was able to distinguish between patients who did and did not suffer 30-day postoperative mortality nearly 96.7% of the time.
Conclusions
Within our cohort, dependent surgical patients had higher rates of comorbidities, complications, and odds of 30-day mortality. Preoperative functional status significantly impacted the level of postoperative mortality following a complication, but independent patients were most affected.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Frailty is a multidimensional construct of physiologic reserve characterized by deterioration in mobility, nutrition, cognition, and the general ability to accomplish activities of daily living (ADL). The definition of frailty has been debated, but it is a known factor of adverse postoperative outcomes [1,2,3,4,5,6,7,8,9,10,11,12,13,14]. The American College of Surgeons (ACS) recommends that geriatric patients be assigned a baseline frailty score prior to surgery [15]. They offer various operationalized definitions, such as those proposed by Fried et al. [9] and Robinson et al. [13] Moreover, several validated tools for estimating frailty exist today [6, 16,17,18], but they often require many variables and are not always applicable to an entire population of patients in a quick, easy, and cost-efficient manner [3, 14, 16, 17, 19, 20]. In fact, the ACS fails to include many of the necessary components of these indices within their National Surgical Quality Improvement Program (ACS-NSQIP) database [21].
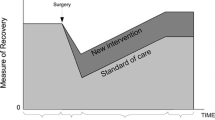
Functional dependency, based on ability to perform activities of daily living, is a reliable alternative measure to assess surgical risk and is easy to determine when obtaining a patient history. While not a replacement for frailty, preoperative assessment of functional status may be more practical due to its relative ease to define, measure, and predict adverse surgical outcomes associated with frailty, including postoperative mortality [2]. In fact, functional dependency is often thought to be an advanced symptom of frailty [2, 3, 22]. The NSQIP preoperative risk variable Functional Health Status is included in many risk models as a significant contributor to postoperative outcomes.
While the correlation between postoperative complications and subsequent mortality is well established, it remains unclear to what extent preoperative functional status is an important contributor to this relationship. [2, 23,24,25,26,27,28,29]. An improved understanding of this relationship may be used to better risk stratify patients at varying degrees of preoperative functional status. The purpose of this study is to explore how the odds of postoperative mortality following a surgical complication was influenced by preoperative functional dependency, within a historical cohort.
Materials and Methods
The Human Subjects Research Protections Program at Vanderbilt University approved this study with a waiver for written, informed consent. It adheres to the applicable EQUATOR guidelines [30].
Data Source
We reviewed a historical cohort of deidentified patient data from the ACS-NSQIP. The dataset includes baseline risk factors, intraoperative exposures, and 30-day postoperative outcomes for patients undergoing major surgical procedures. The ACS-NSQIP data collection methodology has been extensively described elsewhere [21].
Patient Population
All encounters for adult (≥ 18 years old) patients spanning from January 1, 2007 to December 31, 2017 contained within the NSQIP database were included. Despite physical decline being predominantly prevalent in geriatric patients, we chose to control for age within our regression (Sect. 2.5.3) rather than exclude younger patients. There were no other exclusion criteria.
Variable Definitions
All variables were obtained using the NSQIP database definitions, including 30-day mortality and functional dependency [21]. During the ACS-NSQIP data collection process, patients are preoperatively classified based on their ability to do daily living activities on their own or with assistance in the 30 days prior to surgery. A patient is “independent” if they do not need assistance for any activity of daily living (ADL), “partially dependent” if they require some assistance, or “totally dependent” if total assistance is required. Patients are then followed for up to 30 days after surgery. Complications or death occurring outside of this period are not included. In the absence of an explicit metric, we used this information to construct our outcome variable, 30-day postoperative mortality, if the patient had a known value for “Year of death”. Otherwise, they were assumed to have lived through the 30-day period. As extremes of age are considered protected health information, the NSQIP groups patients older than 89 into a “90 + ” category. However, we elected to treat age continuously and did not further stratify.
Missing Data
Five rounds of multiple imputation using chained equations (MICE) was performed for most missing data, including functional dependency status. Rubin’s rules were used to pool results across the five imputations [31,32,33,34]. Laboratory values were believed to be missing-not-at-random (MNAR). As such, proportions of missingness were considerably higher. Thus, we instead employed the missing-indicator method for laboratory variables [35, 36].
Statistical Analysis
This study is strictly considered to be hypothesis generating and intended to highlight relationships for future, focused study. Given this, coupled with the size of the dataset, we elected not to perform ad hoc power analysis. Demographic and procedural variables were summarized with medians and interquartile range (IQR) for continuous variables and with counts and percentages for categorical variables. Significance level (α) for calculated p-values was set to 0.01 (1%) [37]. All statistical analyses were performed using R version 3.6 [R Foundation for Statistical Computing, Vienna, Austria].
Unadjusted Analysis
Using the chi-squared test of significance, we evaluated the composite null hypothesis that the level of dependency significantly effects the odds of mortality. Univariate rates of death for individual complications, stratified by functional status, were also reported.
Variable Selection
We performed a two-stage least absolute shrinkage and selection operator (LASSO) logistic regression procedure [38, 39]. First, potential confounding variables were selected by the LASSO in each imputed dataset. All demographic, procedural, comorbidity, and surgical outcome data, reviewed first by coauthors for availability and biological plausibility, were screened by LASSO as candidates for inclusion. Those selected in all imputations were used in the second stage [40].
Partly due to their extensive data quality improvement efforts over the years, the ACS-NSQIP does not have an exhaustive list of all frailty factors. As mentioned, the ACS recommends defining frailty using the Fried Frailty Phenotype (FFP) [9], but only supplied 1 of the 5 required data elements (weight loss) within all of our study years. Similarly, the Risk Analysis Index (RAI) [15] has been validated as a quick and easy manner of estimating frailty but contains components of eating, toilet use, personal hygiene, and cognitive decline that are also unavailable within the ACS-NSQIP. However, the modified frailty index-5 (mFI-5) has been validated against its parent index, the modified frailty index-11 (mFI-11), to have strong predictive ability for mortality and postoperative complications [16]. The 5 factors included in mFI-5: functional status, diabetes, hypertension requiring medication, history of congestive heart failure, and history of COPD, were all accounted for within our adjusted analysis.
Selected demographic variables include year of surgery, race, gender, age, height, and weight. Comorbidities and procedural variables include surgical specialty, wound classification, ASA class, dyspnea, preoperative sepsis, preoperative renal failure, preoperative transfusion, inpatient/outpatient status, transfer status, emergency surgery, smoking history, ventilator dependency, dialysis, disseminated cancer, wound infection, steroid use, weight loss, bleeding disorder, and days from admission to operation. Laboratory values chosen were blood urea nitrogen level, serum albumin, bilirubin, serum glutamic oxaloacetic transaminase, alkaline phosphatase, white blood cell count, hematocrit volume, platelet count, and international ratio of prothrombin time. Complications selected were acute renal failure, urinary tract infection, stroke/cerebrovascular accident, cardiac arrest, myocardial infarction, transfusions, deep vein thrombosis requiring therapy, occurrences of sepsis and septic shock, return to the OR, surgical site infections, wound disruption, pneumonia, unplanned intubation, pulmonary embolism, and progressive renal insufficiency.
Adjusted Analysis
Using the selected covariates, including functional status, we fit a “base” logistic model without interactions. Surgical complications were then sequentially interacted with functional dependency and individually added to the base model. This process was repeated iteratively for every complication, yielding an individual model for each one.
Odds ratios (OR) representing the effect on mortality, stratified by functional status, with 99% confidence intervals were reported. The analysis of variance (ANOVA) tested the statistical significance of interactions. The receiver operating characteristic (ROC) curve and concordance statistic assessed discriminative ability of the model, while a calibration plot measured the predictive accuracy [41, 42]. Variance inflation factors (VIF) assessed for multicollinearity. Numeric variables were centered to reduce structural multicollinearity.
Post Hoc Analysis
First, we summarized the distribution of demographic and procedural variables within a cohort of patients who did and did receive unplanned intubation to illuminate the key differences between the two group of patients. We also performed a post hoc power analysis.
Results
Patient Demographics
We analyzed 6,483,387 surgical patients. 2,548 patients younger than 18 were excluded. Proportions of functional status decreased from 96.6% functionally independent (n = 6,222,611), to 2.7% (n = 176,308) partially dependent, to 0.7% (n = 47,428) totally dependent patients (Appendix 1).
Missing Data
Besides laboratory values, rates of missingness were mostly low (< 2%). Functional dependency had a missingness rate of 0.5% (37,040). There were no missing mortality data (Appendix 2).
Unadjusted Analysis
Within 30-day postoperative period, 1.3% (n = 82,895) of patients died. Average mortality rate progressively increased from 0.9% (n = 57,652) in functionally independent patients, to 8.6% (n = 15,075) in partially dependent patients, and 21.4%, (n = 10,168) in totally dependent patients. The chi-squared test reported a significant univariate association between dependency and mortality (P < 0.001). Most surgical complications, such as stroke, cardiac arrest, and myocardial infarction were univariately associated with increased mortality rates. However, several complications were not associated with increased mortality in dependent patients. For instance, the occurrence of a superficial surgical site infection was associated with increased mortality in independent patients (0.9% to 1.1%) but lower mortality in partially dependent patients and totally dependent patients (8.7% to 6.2% and 21.9% to 11.3%, respectively). Univariate mortality rates following a complication, stratified by dependency, are shown in Table 1.
Adjusted Analysis
Controlling for confounding, partial and total dependency were associated with 1.7 times (OR: 1.72, 99% CI: 1.66 to 1.77) and 2.3 times (OR: 2.26, 99% CI: 2.15 to 2.37) higher odds of mortality than independent patients, respectively. Table 2 shows the odds ratios (OR) and 99% confidence intervals of all base variables selected by the LASSO.
The odds of mortality significantly varied by preoperative functional status following all complications (P < 0.001). After controlling for demographics, comorbidities, and other complications, 12 of 18 surgical complications were significantly associated with increased odds of mortality (OR > 1) in independent patients. In contrast, only 9 and 4 complications had significant, positive associations in partially and totally dependent patients, respectively. Table 3 details the OR for each complication, and its relationship with preoperative dependency. Our base model had excellent discrimination: the area under the ROC (AUROC) curve was 0.967. Overall, the model was well calibrated. Variance inflation factors (VIF) were mostly low (< 2).
Post HocAnalysis
In our primary analysis, unplanned intubation was significantly associated with increased the odds of mortality in both independent and partially dependent patients but decreased odds of mortality in totally dependent patients. Despite this, the univariate rate of death for totally dependent patients following unplanned intubation increased (Table 1–20.3% without unplanned intubation, 38.7% with). To further examine this discrepancy, we summarized the distribution of demographics for totally dependent intubated patients (Appendix 3). Among intubated patients, the rate of total dependency was much higher (5.9% of intubated patients were totally dependent vs. 0.73% of all patients). There was a slightly higher rate of total dependency among intubated patients who died than intubated patients who lived, although the two were similar (5.4% of patients with unplanned intubation who lived were totally dependent vs. 7.2% of intubated patients who died). Approximately 40% (1,326 of 3,438) of totally dependent patients who received unplanned intubation died—almost twice the rate of non-intubated functionally dependent patients. However, to compensate for this increased rate of death, totally dependent patients who received intubation and died were on average older, weighed less, and had increased rates of most comorbidities and serious complications (e.g., renal failure, stroke, cardiac arrest, septic shock)—with nearly 4 times more instances of cardiac arrest.
A post hoc power analysis was also performed. This revealed that we would need approximately 464 patients per functional capacity group to detect a significant association at our level of significance, 80% power and a “small” effect size.
Discussion
We studied how preoperative functional dependency influenced postoperative mortality following a complication within a historical cohort. While our model analyzed dependence and not frailty, our results are adjusted for the components of frailty included in the mFI-5. Functional dependence is an easily determined measure, that is patient-centered and relevant, can the patient perform his or her daily activities. Our data suggests that dependent patients have more comorbidities, suffer more complications, and have higher rates of postoperative mortality. Second, the impact of a postoperative complication on the odds of mortality varied by preoperative functional ability. Relative to dependent patients, surgical complications in independent patients were associated with stronger increases in the odds of mortality.
Understanding the association between functional health and adverse postoperative outcomes is a strategic imperative for hospitals, considering that nearly 20% of all 30-day mortality is attributable to a postoperative complication [43]. Moreover, accurate estimates of surgical risk might convince patients to opt for less invasive or non-surgical care, further diminishing potential mortality rates [1]. Current emphasis has been on defining and identifying functional dependence. For example, dependent patients are older, more likely to be female, and have more comorbidities, including malnutrition [2, 44,45,46]. In that regard, our work agrees with previous literature. Functionally dependent patients had more comorbidities and complications, weighed less, and were older and more often female.
We found that the association between complication and mortality can be divided into 3 groups: Group 1 – surgical site infections and disruptions, pulmonary emboli, deep venous thrombosis, urinary tract infections, and sepsis are associated with increased mortality in independent patients but not in dependent patients. This was present in both the unadjusted and adjusted analyses. Group 2 – acute renal failure, stroke, myocardial infarction, and cardiac arrest are associated with increased mortality in both functionally independent and dependent patients. Again, this was present in both the unadjusted and adjusted analyses. Group 3 – pneumonia, unplanned intubation, progressive renal insufficiency, and septic shock are associated with increased mortality in all 3 functional levels by univariate analysis and in independent patients in the adjusted analysis, but associated with decreased mortality, after adjustment, in the totally dependent patients.
Importantly, Group 1 complications are associated with increased death in the independent patients, but in the dependent patients, they appear to be merely epiphenomena and carry different prognostic weights in the different functional patients. In Group 2 patients, these complications are associated with increased mortality at all levels of dependence, but the odds ratios are smaller in magnitude for dependent patients than for independent patients. This probably relates to the higher baseline level of mortality risk in the dependent patients or the performed procedure itself, where a similar absolute increase in mortality produces a smaller odds ratio of increased mortality. Group 3 results seem counterintuitive, as one might expect the burden of surgical complications to become heavier on those functionally dependent patients who are not as physically equipped to cope. But within our cohort this was not always the case. As interpreting negative odds ratios (B < 0 or OR < 1) for these comorbidities as “protective” of death is anecdotally implausible, these negative odds ratios must be interpreted based on their conditions.
First, the simultaneous occurrence of multiple complications could explain an OR < 1 in at least one of them. Surgical complications could be seen as competing risks. Several infection and sepsis complications may compete. E.g., by database definitions, the patient cannot have both sepsis and septic shock complications. There could be “survival” or “opportunity” bias due to differences in the distribution of postoperative timing of surgical outcomes. Death, of course, is the ultimate competing risk. Patients cannot get more complications after dying. Although outside the scope of this study, cursory analysis reveals that independent, partially dependent, and totally dependent patients had a median time to death of 10, 11, and 8 days, respectively. However, most of the less serious complications (surgical site infection, wound disruption, etc.) have median time to manifestation that are greater than or approximately equal the median time to death. Conversely, more serious surgical complications (cardiac arrest, stroke, renal failure, etc.) on average manifested earlier, before death. Thus, it could be the case that dependent patients often do not survive long enough for less serious complications to manifest themselves and impact the odds of mortality. What is more, dependent patients who live long enough to have a complication such as a surgical site infection might have a less likelihood of developing a more serious complication at that point in their recovery.
Another possible explanation, which is common to all observational studies regardless of sample size, is endogeneity. The presence of unmeasured and uncontrolled confounding variables, such as lifestyle, regional, or hospital-specific factors that are correlated with 30-day mortality and either dependency or the interacting surgical complication, could introduce bias. For instance, palliation is an aspect that confounds surgical outcomes in dependent patients. Currently, the ACS-NSQIP lacks a manner of identifying those with palliative intent. Importantly, the move to withdraw care may occur more frequently in these patients than a fully independent one–skewing the outcome data.
There are several strengths of the analysis which should be illuminated, of which the size and quality of the dataset is a significant one. Using a large, national database containing data originating from a wide variety of demographic populations and procedural settings leads to improved generalizability, increased statistical power, and more precise results. Consistent methodology and data definitions incorporated by the ACS-NSQIP further reinforce these advantages. Moreover, we used a robust and replicable statistical methodology to isolate the effect of the interaction between functional dependency and mortality after a surgical complication while taking care not to overfit our model to the data or introduce bias. Due to this, the discriminative (i.e., the ability to distinguish between patients who did and did not die) and predictive ability of our model is extremely high–as emphasized by the ROC curve and model calibration, respectively. Setting the significance level below the arbitrary standard of 5% affords us even further confidence in the precision of our results and diminishes doubt that the impact of surgical complications remains consistent across patients of different dependency levels. However, despite our sample size, we may have type II errors and missed rarely occurring interacting complications that were truly associated with increased mortality.
The ACS-NSQIP data collection process is meticulous despite its scale, but it is important to note potential sources of bias which can be magnified by large datasets [47]. First, if the underlying sampling procedure is non-representative of the overall population, bias is introduced. Although precautions are taken to limit oversampling within the ACS-NSQIP, there are several surgical procedures, such as general or vascular procedures, which are overrepresented by the sampling methodologies available to participating sites. Measurement error is another prevalent source of bias in large datasets. While small control studies can devote great time and effort to precision, this is more difficult to achieve by large scale databases which are aggregating data from a multitude of sources across the country. Our analysis also lacks accounting for hospital-specific factors or baseline procedural risk. There are many hospital factors that have been associated with mortality following a complication, including hospital size, occupancy, teaching status, intensive care unit staffing, nurse-to-patient ratio, etc. [1] Although extensive, the ACS-NSQIP database does not contain an exhaustive list of these factors, as well as other surgical outcomes, limiting the potential scope of this analysis.
Frailty and functional dependency are two distinct, yet interrelated concepts that are known determinants of mortality and other adverse postoperative outcomes [8, 12, 13]. While we found evidence that dependent patients were still more likely to experience postoperative mortality than their independent counterparts, functionally independent patients saw stronger increases in the odds of death following a complication. That said, it is important to note that the associations seen in this exploratory analysis are not statements of causation. As such, they are not yet fit to inform clinical practice. Despite this, we believe functional dependency status to have a clear association with postoperative mortality, deserving more in-depth investigation using more granular datasets. Given the relatively low risk and ease of doing so in routine clinical practice, we would recommend preoperative assessment of functional dependency, if unable to perform validated assessment of frailty.
Funding Disclosure
Dr. Robert Freundlich receives funding from K23HL148640 (NIH-NHLBI). Other authors–departmental funding.
References
Shah, R., et al., Association of Frailty with Failure to Rescue After Low-Risk and High-Risk Inpatient Surgery. JAMA Surg, 2018. 153(5): p. e180214.
Scarborough, J.E., et al., The impact of functional dependency on outcomes after complex general and vascular surgery. Ann Surg, 2015. 261(3): p. 432-7.
Pel-Littel, R.E., et al., Frailty: defining and measuring of a concept. J Nutr Health Aging, 2009. 13(4): p. 390-4.
Akyar, S., et al., The Impact of Frailty on Postoperative Cardiopulmonary Complications in the Emergency General Surgery Population. Surg J (N Y), 2018. 4(2): p. e66-e77.
Puts, M.T., P. Lips, and D.J. Deeg, Static and dynamic measures of frailty predicted decline in performance-based and self-reported physical functioning. J Clin Epidemiol, 2005. 58(11): p. 1188-98.
Rockwood, K., et al., A global clinical measure of fitness and frailty in elderly people. Cmaj, 2005. 173(5): p. 489-95.
Theou, O., et al., Operationalization of frailty using eight commonly used scales and comparison of their ability to predict all-cause mortality. J Am Geriatr Soc, 2013. 61(9): p. 1537-51.
Lally F, Crome P. Understanding frailty. Postgrad Med J. 2007;83(975):16-20. https://doi.org/10.1136/pgmj.2006.048587A
Linda P. Fried, Catherine M. Tangen, Jeremy Walston, Anne B. Newman, Calvin Hirsch, John Gottdiener, Teresa Seeman, Russell Tracy, Willem J. Kop, Gregory Burke, Mary Ann McBurnie, Frailty in Older Adults: Evidence for a Phenotype, The Journals of Gerontology: Series A, Volume 56, Issue 3, 1 March 2001, Pages M146–M157. https://doi.org/10.1093/gerona/56.3.M146A
Makary MA, Segev DL, Pronovost PJ Syin D, Bandeen-Roche K, Patel P, Takenaga R, Devgan L, Holzmueller CG, Tian J, Fried LP. Frailty as a predictor of surgical outcomes in older patients J Am Coll Surg. 2010 Jun;210(6):901–8. https://doi.org/10.1016/j.jamcollsurg.2010.01.028. Epub 2010 Apr 28 PMID: 20510798.
Bergman H, Ferrucci L, Guralnik J, et al. Frailty: an emerging research and clinical paradigm--issues and controversies. J Gerontol A Biol Sci Med Sci. 2007;62(7):731-737. https://doi.org/10.1093/gerona/62.7.731A
Linda P. Fried, Luigi Ferrucci, Jonathan Darer, Jeff D. Williamson, Gerard Anderson, Untangling the Concepts of Disability, Frailty, and Comorbidity: Implications for Improved Targeting and Care, The Journals of Gerontology: Series A, Volume 59, Issue 3, March 2004, Pages M255–M263. https://doi.org/10.1093/gerona/59.3.M255A
Thomas N. Robinson, Ben Eiseman, Jeffrey I. Wallace, Skotti D. Church, Kim K. McFann, Shirley M. Pfister, Terra J. Sharp, Marc Moss, Redefining Geriatric Preoperative Assessment Using Frailty, Disability and Co-Morbidity, Annals of Surgery: September 2009 - Volume 250 - Issue 3 - p 449–455. https://doi.org/10.1097/SLA.0b013e3181b45598
Cheung A, Haas B, Ringer TJ, McFarlan A, Wong CL. Canadian Study of Health and Aging Clinical Frailty Scale: Does It Predict Adverse Outcomes among Geriatric Trauma Patients?. J Am Coll Surg. 2017 Nov;225(5):658–665.e3. https://doi.org/10.1016/j.jamcollsurg.2017.08.008. Epub 2017 Sep 6. PMID: 28888692.
Chow, W.B., et al., Optimal preoperative assessment of the geriatric surgical patient: a best practices guideline from the American College of Surgeons National Surgical Quality Improvement Program and the American Geriatrics Society. J Am Coll Surg, 2012. 215(4): p. 453-66.
Hall DE, Arya S, Schmid KK, Blaser C, Carlson MA, Bailey TL, Purviance G, Bockman T, Lynch TG, Johanning J. Development and Initial Validation of the Risk Analysis Index for Measuring Frailty in Surgical Populations. JAMA Surg. 2017 Feb 1;152(2)175–182. https://doi.org/10.1001/jamasurg.2016.4202. PMID: 27893030; PMCID: PMC7140150.
Subramaniam S, Aalberg JJ, Soriano RP, Divino CM. New 5-Factor Modified Frailty Index Using American College of Surgeons NSQIP Data. J Am Coll Surg. 2018 Feb;226(2)173–181.e8. https://doi.org/10.1016/j.jamcollsurg.2017.11.005. Epub 2017 Nov 16. PMID: 29155268.
E Dent P Kowal EO Hoogendijk 2016 Jun Frailty measurement in research and clinical practice: A review Eur J Intern Med. 31 3 10 https://doi.org/10.1016/j.ejim.2016.03.007. Epub 2016 Mar 31 PMID: 27039014
McDonald VS, Thompson KA, Lewis PR, Sise CB, Sise MJ, Shackford SR. Frailty in trauma: A systematic review of the surgical literature for clinical assessment tools. J Trauma Acute Care Surg. 2016 May;80(5)824–834. https://doi.org/10.1097/TA.0000000000000981. PMID: 26881488.
Joseph B, Pandit V, Zangbar B, Kulvatunyou N, Tang A, O'Keeffe T, Green DJ, Vercruysse G, Fain MJ, Friese RS, Rhee P. Validating trauma-specific frailty index for geriatric trauma patients: a prospective analysis. J Am Coll Surg. 2014 Jul;219(1):10–17.e1. https://doi.org/10.1016/j.jamcollsurg.2014.03.020. Epub 2014 Mar 19. Erratum in: J Am Coll Surg. 2016 Mar;222(3):336. PMID: 24952434.
Program, A.C.o.S.N.S.Q.I. User Guide for the 2017 ACS NSQIP Participant Use Data File. 12/16/2020]; Available from: https://www.facs.org/~/media/files/quality%20programs/nsqip/nsqip_puf_userguide_2017.ashx.
Fried, L.P., et al., Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci, 2004;59(3): p. 255–263.
Khan, M.A., et al., Perioperative risk factors for 30-day mortality after bariatric surgery: is functional status important? Surg Endosc, 2013. 27(5): p. 1772-7.
Ponzetto, M., et al., Risk factors for early and late mortality in hospitalized older patients: the continuing importance of functional status. J Gerontol A Biol Sci Med Sci, 2003. 58(11): p. 1049-54.
Cohen, M.E., et al., Effect of subjective preoperative variables on risk-adjusted assessment of hospital morbidity and mortality. Ann Surg, 2009. 249(4): p. 682-9.
Kilic, A., et al., Functional status is highly predictive of outcomes after redo lung transplantation: an analysis of 390 cases in the modern era. Ann Thorac Surg, 2013. 96(5): p. 1804–11; discussion 1811.
de la Fuente, S.G., K.M. Bennett, and J.E. Scarborough, Functional status determines postoperative outcomes in elderly patients undergoing hepatic resections. J Surg Oncol, 2013;107(8):865–70.
Lentine, K.L., et al., Impact of Functional Status on Outcomes of Simultaneous Pancreas-kidney Transplantation: Risks and Opportunities for Patient Benefit. Transplant Direct, 2020. 6(9): p. e599.
Stienen, M.N. et al., The influence of preoperative dependency on mortality, functional recovery and complications after microsurgical resection of intracranial tumors. J Neurooncol, 2018;139(2):441–448.
Network, E. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. 12/16/20]; Available from: https://www.equator-network.org/reporting-guidelines/strobe/.
White, I.R., P. Royston, and A.M. Wood, Multiple imputation using chained equations: Issues and guidance for practice. Stat Med, 2011;30(4): p. 377–99.
Buuren, S. and C. Groothuis-Oudshoorn, MICE: Multivariate Imputation by Chained Equations in R. Journal of Statistical Software, 2011. 45.
Jakobsen, J.C., et al., When and how should multiple imputation be used for handling missing data in randomised clinical trials - a practical guide with flowcharts. BMC Med Res Methodol, 2017. 17(1): p. 162.
Little, R.J., et al., The prevention and treatment of missing data in clinical trials. The New England journal of medicine, 2012;367(14): p. 1355–1360.
Groenwold, R.H., et al., Missing covariate data in clinical research: when and when not to use the missing-indicator method for analysis. Cmaj, 2012. 184(11): p. 1265-9.
Jones, M.P., Indicator and Stratification Methods for Missing Explanatory Variables in Multiple Linear Regression. Journal of the American Statistical Association, 1996. 91(433): p. 222-230.
Wasserstein, R.L. and N.A. Lazar, The ASA Statement on p-Values: Context, Process, and Purpose. The American Statistician, 2016. 70(2): p. 129-133.
Tibshirani, R., Regression Shrinkage and Selection Via the Lasso. Journal of the Royal Statistical Society: Series B (Methodological), 1996. 58(1): p. 267-288.
Bien, J., J. Taylor, and R. Tibshirani, A LASSO FOR HIERARCHICAL INTERACTIONS. Ann Stat, 2013. 41(3): p. 1111-1141.
Zhao, Y. and Q. Long, Variable Selection in the Presence of Missing Data: Imputation-based Methods. Wiley Interdiscip Rev Comput Stat, 2017. 9(5).
Steyerberg, E.W., et al., Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology, 2010. 21(1): p. 128-38.
Cook, N.R., Statistical evaluation of prognostic versus diagnostic models: beyond the ROC curve. Clin Chem, 2008. 54(1): p. 17-23.
Freundlich, R.E., et al., Complications Associated With Mortality in the National Surgical Quality Improvement Program Database. Anesth Analg, 2018. 127(1): p. 55-62.
Naseer, M., H. Forssell, and C. Fagerström, Malnutrition, functional ability and mortality among older people aged ⩾ 60 years: a 7-year longitudinal study. Eur J Clin Nutr, 2016. 70(3): p. 399-404.
Curtis, G.L., et al., Dependent Functional Status is a Risk Factor for Perioperative and Postoperative Complications After Total Hip Arthroplasty. J Arthroplasty, 2019. 34(7s): p. S348-s351.
Minhas, S.V., A.S. Mazmudar, and A.A. Patel, Pre-operative functional status as a predictor of morbidity and mortality after elective cervical spine surgery. Bone Joint J, 2017. 99-b(6): p. 824–828.
Kaplan, R.M., D.A. Chambers, and R.E. Glasgow, Big data and large sample size: a cautionary note on the potential for bias. Clin Transl Sci, 2014. 7(4): p. 342-6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Robert Freundlich has stock in Pfizer, 3 M, Johnson and Johnson, and Gilead Pharmaceuticals.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1: Patient Demographics
Summary Statistics | ||||||
|---|---|---|---|---|---|---|
Whole dataset | Totally Independent | Partially Dependent | Totally Dependent | |||
Total Number of Patients | 6,483,387 | 6,222,611 | 176,308 | 47,428 | ||
Death (%) | 84,170 (1.3) | 57,652 (0.9) | 15,075 (8.6) | 10,168 (21.4) | ||
Demographics | Year (%) | 2007 | 210,405 (3.2) | 195,729 (3.1) | 10,236 (5.8) | 4440 (9.4) |
2008 | 269,847 (4.2) | 251,709 (4.0) | 12,963 (7.4) | 5175 (10.9) | ||
2009 | 336,185 (5.2) | 313,595 (5.0) | 16,503 (9.4) | 6087 (12.8) | ||
2010 | 363,431 (5.6) | 343,089 (5.5) | 14,923 (8.5) | 5210 (11.0) | ||
2011 | 442,149 (6.8) | 420,960 (6.8) | 14,120 (8.0) | 3878 (8.2) | ||
2012 | 543,885 (8.4) | 525,316 (8.4) | 13,542 (7.7) | 2903 (6.1) | ||
2013 | 651,940 (10.1) | 628,574 (10.1) | 14,715 (8.3) | 3145 (6.6) | ||
2014 | 750,937 (11.6) | 726,360 (11.7) | 16,006 (9.1) | 3184 (6.7) | ||
2015 | 885,502 (13.7) | 855,685 (13.8) | 20,042 (11.4) | 4178 (8.8) | ||
2016 | 1,000,393 (15.4) | 966,924 (15.5) | 21,245 (12.0) | 4549 (9.6) | ||
2017 | 1,028,713 (15.9) | 994,670 (16.0) | 22,013 (12.5) | 4679 (9.9) | ||
Race (%) | White | 4,747,446 (73.4) | 4,561,675 (73.5) | 126,902 (72.2) | 32,109 (68.0) | |
Black | 643,386 (9.9) | 608,546 (9.8) | 23,364 (13.3) | 8426 (17.9) | ||
Asian | 172,860 (2.7) | 166,434 (2.7) | 3801 (2.2) | 1015 (2.2) | ||
Other | 903,309 (14.0) | 870,373 (14.0) | 21,695 (12.3) | 5644 (12.0) | ||
Sex = Female (%) | 3,691,976 (57.0) | 3,549,090 (57.1) | 98,076 (55.7) | 24,242 (51.2) | ||
Age (years)—median (IQR) | 58 [45, 69] | 57 [44, 68] | 72 [60, 82] | 69 [56, 80] | ||
Height (cm)—median (IQR) | 168 [160, 175] | 168 [160, 175] | 165 [157, 175] | 168 [157, 175] | ||
Weight (kg)—median (IQR) | 81.6 [68.0, 97.5] | 81.6 [68.0, 97.5] | 74.4 [61.2, 90.7] | 72.6 [59.0, 88.9] | ||
Preoperative Comorbidities and Procedural Variables | Surgical Specialty (%) | General Surgery | 3,325,982 (51.3) | 3,211,754 (51.6) | 71,363 (40.5) | 26,090 (55.0) |
Vascular | 484,793 (7.5) | 437,155 (7.0) | 36,437 (20.7) | 8857 (18.7) | ||
Orthopedics | 1,189,299 (18.3) | 1,129,604 (18.2) | 44,290 (25.1) | 6708 (14.1) | ||
Urology | 321,597 (5.0) | 312,158 (5.0) | 5857 (3.3) | 1365 (2.9) | ||
Neurosurgery | 286,015 (4.4) | 273,362 (4.4) | 9168 (5.2) | 1799 (3.8) | ||
Other | 875,700 (13.5) | 858,577 (13.8) | 9193 (5.2) | 2609 (5.5) | ||
Wound Classification (%) | 1 – Clean | 3,575,426 (55.1) | 3,439,672 (55.3) | 96,463 (54.7) | 17,940 (37.8) | |
2 – Clean/ Contaminated | 2,140,662 (33.0) | 2,081,106 (33.4) | 38,687 (21.9) | 10,981 (23.2) | ||
3 – Contaminated | 423,012 (6.5) | 399,617 (6.4) | 14,776 (8.4) | 5693 (12.0) | ||
4 – Dirty/Infected | 344,282 (5.3) | 302,214 (4.9) | 26,382 (15.0) | 12,814 (27.0) | ||
ASA Class (%) | 1 | 583,875 (9.0) | 579,093 (9.3) | 1235 (0.7) | 87 (0.2) | |
2 | 2,912,622 (45.1) | 2,876,798 (46.4) | 18,893 (10.7) | 1886 (4.0) | ||
3 | 2,556,923 (39.6) | 2,417,971 (39.0) | 104,291 (59.3) | 20,239 (42.8) | ||
4/5 | 410,794 (6.4) | 330,433 (5.3) | 51,355 (29.2) | 25,078 (53.0) | ||
Diabetes (%) | 0 – No | 5,486,362 (84.6) | 5,302,856 (85.2) | 120,327 (68.2) | 32,787 (69.1) | |
1 – Insulin | 377,319 (5.8) | 330,895 (5.3) | 33,704 (19.1) | 9797 (20.7) | ||
2 – Non-Insulin | 619,698 (9.6) | 588,860 (9.5) | 22,277 (12.6) | 4844 (10.2) | ||
Dyspnea (%) | 0 – No | 6,044,616 (93.2) | 5,826,783 (93.6) | 145,917 (82.8) | 37,516 (79.1) | |
1 – At Rest | 42,863 (0.7) | 29,051 (0.5) | 7206 (4.1) | 6149 (13.0) | ||
2 – Moderate Exertion | 395,878 (6.1) | 366,762 (5.9) | 23,182 (13.1) | 3761 (7.9) | ||
Sepsis (%) | 0 – None | 6,084,721 (94.0) | 5,884,964 (94.8) | 140,007 (79.6) | 26,515 (56.0) | |
1 – Systemic Inflammatory Response Syndrome (SIRS) | 219,814 (3.4) | 192,436 (3.1) | 18,442 (10.5) | 6972 (14.7) | ||
2 – Sepsis | 135,212 (2.1) | 114,743 (1.8) | 13,177 (7.5) | 6082 (12.8) | ||
3 – Septic Shock | 31,359 (0.5) | 18,641 (0.3) | 4320 (2.5) | 7790 (16.4) | ||
Functional Status (%) | 0 – Totally Independent | 6,222,611 (96.5) | 6,222,611 (100.0) | 0 (0.0) | 0 (0.0) | |
1 – Partially Dependent | 176,308 (2.7) | 0 (0.0) | 176,308 (100.0) | 0 (0.0) | ||
2 – Totally Dependent | 47,428 (0.7) | 0 (0.0) | 0 (0.0) | 47,428 (100.0) | ||
Outpatient (%) | 2,550,335 (39.3) | 2,511,457 (40.4) | 17,433 (9.9) | 2786 (5.9) | ||
Transfer Status = Admitted from other (%) | 274,086 (4.2) | 202,184 (3.3) | 47,389 (26.9) | 21,499 (45.4) | ||
Emergency (%) | 636,169 (9.8) | 575,060 (9.2) | 37,692 (21.4) | 18,058 (38.1) | ||
Smoker (%) | 1,189,267 (18.3) | 1,142,322 (18.4) | 32,105 (18.2) | 7512 (15.8) | ||
Ventilator Dependent (%) | 29,861 (0.5) | 15,185 (0.2) | 2453 (1.4) | 11,582 (24.4) | ||
History of Severe Chronic Obstructive Pulmonary Disease (%) | 296,716 (4.6) | 263,668 (4.2) | 24,312 (13.8) | 6339 (13.4) | ||
Ascites (%) | 30,524 (0.5) | 24,623 (0.4) | 3268 (1.9) | 2401 (5.1) | ||
History of Congestive Heart Failure (%) | 56,817 (0.9) | 41,922 (0.7) | 10,120 (5.7) | 4161 (8.8) | ||
Hypertension Requiring Medication (%) | 2,943,652 (45.4) | 2,771,762 (44.5) | 123,744 (70.2) | 30,723 (64.8) | ||
Acute Renal Failure (%) | 25,937 (0.4) | 19,058 (0.3) | 3786 (2.1) | 2738 (5.8) | ||
Dialysis (%) | 94,879 (1.5) | 75,327 (1.2) | 13,473 (7.6) | 5052 (10.7) | ||
Disseminated Cancer (%) | 142,302 (2.2) | 132,313 (2.1) | 7499 (4.3) | 1738 (3.7) | ||
Open Wound/Wound Infection (%) | 216,208 (3.3) | 157,509 (2.5) | 39,712 (22.5) | 16,980 (35.8) | ||
Steroid Use for Chronic Condition (%) | 226,678 (3.5) | 207,868 (3.3) | 13,610 (7.7) | 3680 (7.8) | ||
Weight Loss (%) | 92,197 (1.4) | 80,291 (1.3) | 8687 (4.9) | 2723 (5.7) | ||
Bleeding Disorder (%) | 294,254 (4.5) | 250,997 (4.0) | 30,855 (17.5) | 9800 (20.7) | ||
Transfusion (%) | 58,983 (0.9) | 45,321 (0.7) | 8075 (4.6) | 4904 (10.3) | ||
Intraoperative/ Postoperative Complications | Return to Operating Room = Yes (%) | 214,429 (3.3) | 189,899 (3.1) | 16,015 (9.1) | 7192 (15.2) | |
Superficial Incisional Surgical Site Infection (%) | 114,112 (1.8) | 106,398 (1.7) | 5692 (3.2) | 1397 (2.9) | ||
Deep Incisional Surgical Site Infection (%) | 36,876 (0.6) | 33,148 (0.5) | 2670 (1.5) | 834 (1.8) | ||
Organ Space Surgical Site Infection (%) | 81,794 (1.3) | 76,040 (1.2) | 3792 (2.2) | 1507 (3.2) | ||
Wound Disruption (%) | 27,445 (0.4) | 24,442 (0.4) | 2058 (1.2) | 785 (1.7) | ||
Pneumonia (%) | 82,053 (1.3) | 66,004 (1.1) | 9817 (5.6) | 5376 (11.3) | ||
Unplanned Intubation (%) | 58,243 (0.9) | 47,258 (0.8) | 6996 (4.0) | 3437 (7.2) | ||
Pulmonary Embolism (%) | 21,471 (0.3) | 19,776 (0.3) | 1172 (0.7) | 418 (0.9) | ||
Progressive Renal Insufficiency (%) | 17,862 (0.3) | 15,411 (0.2) | 1618 (0.9) | 690 (1.5) | ||
Acute Renal Failure (%) | 20,581 (0.3) | 16,516 (0.3) | 2226 (1.3) | 1621 (3.4) | ||
Urinary Tract Infection (%) | 90,406 (1.4) | 78,808 (1.3) | 7861 (4.5) | 3135 (6.6) | ||
Stroke/Cerebrovascular Accident (%) | 13,548 (0.2) | 11,419 (0.2) | 1454 (0.8) | 576 (1.2) | ||
Cardiac Arrest (%) | 21,281 (0.3) | 16,569 (0.3) | 2743 (1.6) | 1703 (3.6) | ||
Myocardial Infarction (%) | 23,347 (0.4) | 19,872 (0.3) | 2545 (1.4) | 705 (1.5) | ||
Transfusions (%) | 329,261 (5.1) | 288,116 (4.6) | 29,329 (16.6) | 9115 (19.2) | ||
Deep Vein Thrombosis Requiring Therapy (%) | 38,829 (0.6) | 34,039 (0.5) | 3085 (1.7) | 1433 (3.0) | ||
Sepsis (%) | 107,620 (1.7) | 93,228 (1.5) | 9392 (5.3) | 4127 (8.7) | ||
Septic Shock (%) | 54,799 (0.8) | 42,644 (0.7) | 7368 (4.2) | 3980 (8.4) | ||
Lab Values | Blood Urea Nitrogen (mg/dL)—median (IQR) | 15.0 [11.0, 19.0] | 15.00 [11.0, 19.0] | 18.5 [13.0, 27.0] | 21.0 [13.0, 33.6] | |
Serum Albumin (g/dL)—median (IQR) | 4.0 [3.6, 4.3] | 4.0 [3.6, 4.3] | 3.3 [2.7, 3.8] | 2.8 [2.2, 3.4] | ||
Total Bilirubin (mg/dL)—median (IQR) | 0.5 [0.4, 0.8] | 0.5 [0.4, 0.8] | 0.5 [0.36, 0.8] | 0.6 [0.4, 0.9] | ||
Serum Glutamic Oxaloacetic Transaminase (units/L)—median (IQR) | 22 [17,29] | 22 [17,29] | 22 [17,31] | 25 [18,41] | ||
Alkaline Phosphatase (units/L)—median (IQR) | 77 [62, 97] | 76 [61, 96] | 87 [68, 118] | 90 [68, 127] | ||
White Blood Cell Count (K/uL)—median (IQR) | 7.40 [5.90, 9.40] | 7.30 [5.90, 9.30] | 8.50 [6.51, 11.40] | 10.0 [7.30, 14.14] | ||
Hematocrit (volume %)—median (IQR) | 40.0 [36.5, 42.9] | 40.0 [36.8, 43.0] | 35.0 [30.5, 39.2] | 32.3 [28.2, 37.1] | ||
Platelet Count (K/uL)—median (IQR) | 241 [198, 291] | 241 [198, 290] | 236 [182, 306] | 234 [167, 319] | ||
International Normalized Ratio of Prothrombin Time values—median (IQR) | 1.0 [1.0, 1.1] | 1.0 [1.0, 1.1] | 1.1 [1.0, 1.2] | 1.2 [1.1, 1.4] | ||
Appendix 2: Missingness Rates
Count | Proportion | |
|---|---|---|
Age | 24,622 | 0.38% |
Sex | 4014 | 0.06% |
Race | 16,386 | 0.25% |
Height | 130,609 | 2.01% |
Weight | 69,082 | 1.07% |
Work Relative Value Unit | 5742 | 0.09% |
In/outpatient | 4 | < 0.00% |
Transfer Status | 5711 | 0.09% |
Anesthesia | 1545 | 0.02% |
Surgical Service | 1 | < 0.00% |
Emergency | 32 | < 0.00% |
Wound Classification | 5 | < 0.00% |
ASA Classification | 19,173 | 0.30% |
Diabetes | 8 | < 0.00% |
Smoke | 25 | < 0.00% |
Dyspnea | 30 | < 0.00% |
Functional Status | 37,040 | 0.57% |
Ventilator | 11 | < 0.00% |
History of Chronic Obstructive Pulmonary Disease | 13 | < 0.00% |
Ascites | 20 | < 0.00% |
History of Congestive Heart Failure | 13 | < 0.00% |
Hypertension | 16 | < 0.00% |
Preoperative Acute Renal Failure | 19 | < 0.00% |
Dialysis | 24 | < 0.00% |
Disseminated Cancer | 17 | < 0.00% |
Open Wound/Wound Infection | 17 | < 0.00% |
Steroid | 17 | < 0.00% |
Weight Loss | 18 | < 0.00% |
Bleeding Disorder | 15 | < 0.00% |
Preop Transfusion | 20 | < 0.00% |
Systemic Sepsis | 12,281 | 0.19% |
Operation Time | 945 | 0.01% |
Hospital Length of Stay | 5683 | 0.09% |
Days from Admission to Surgery | 239 | < 0.00% |
Return to Operating Room | 55 | < 0.00% |
Serum Sodium | 1,232,739 | 19.01% |
Blood Urea Nitrogen | 1,416,070 | 21.84% |
Serum Creatinine | 1,186,261 | 18.30% |
Serum Albumin | 3,150,009 | 48.59% |
Total Bilirubin | 3,151,874 | 48.61% |
Serum Glutamic Oxaloacetic Transaminase | 3,145,901 | 48.52% |
Alkaline Phosphatase | 3,131,423 | 48.30% |
White Blood Cell Count | 1,033,486 | 15.94% |
Hematocrit | 942,893 | 14.54% |
Platelet Count | 1,037,770 | 16.01% |
Partial Thromboplastin Time | 4,278,329 | 65.99% |
International Normalized Ratio (INR) of Prothrombin Time values | 3,732,736 | 57.57% |
Prothrombin Time | 5,809,086 | 89.60% |
Appendix 3: Totally Dependent Patients with Unplanned Intubation Cohort Summary
Lived | Died | ||
|---|---|---|---|
Count (%) | 2112 (5.4) | 1326 (7.2) | |
Sex = Female (%) | 945 (44.8) | 618 (46.6) | |
Age (years)—median (IQR) | 65 [54, 75] | 72 [61, 81] | |
Weight (kg)—median (IQR) | 76 [63, 94] | 71 [59, 87] | |
Wound Classification (%) | 1 – Clean | 560 (26.5) | 372 (28.1) |
2 – Clean/ Contaminated | 510 (24.1) | 299 (22.5) | |
3 – Contaminated | 328 (15.5) | 210 (15.8) | |
4 – Dirty/Infected | 714 (33.8) | 445 (33.6) | |
ASA Class (%) | 1 | 1 (0.0) | 1 (0.1) |
2 | 38 (1.8) | 13 (1.0) | |
3 | 677 (32.1) | 379 (28.6) | |
4/5 | 1391 (66.0) | 933 (70.4) | |
Diabetes (%) | 0 – No | 1492 (70.6) | 896 (67.6) |
1 – Insulin | 398 (18.8) | 286 (21.6) | |
2 – Non-Insulin | 222 (10.5) | 144 (10.9) | |
Dyspnea (%) | 0 – No | 1420 (67.2) | 872 (65.8) |
1 – At Rest | 462 (21.9) | 297 (22.4) | |
2 – Moderate Exertion | 230 (10.9) | 157 (11.8) | |
Sepsis (%) | 0 – None | 750 (35.5) | 478 (36.1) |
1 – Systemic Inflammatory Response Syndrome (SIRS) | 403 (19.1) | 270 (20.4) | |
2 – Sepsis | 312 (14.8) | 269 (20.3) | |
3 – Septic Shock | 646 (30.6) | 307 (23.2) | |
Outpatient (%) | 14 (0.7) | 14 (1.1) | |
Transfer Status = Admitted from other (%) | 927 (43.9) | 624 (47.1) | |
Emergency (%) | 1144 (54.2) | 662 (49.9) | |
Smoker (%) | 474 (22.4) | 250 (18.9) | |
Ventilator Dependent (%) | 863 (40.9) | 352 (26.5) | |
History of Severe Chronic Obstructive Pulmonary Disease (%) | 373 (17.7) | 251 (18.9) | |
Ascites (%) | 174 (8.2) | 138 (10.4) | |
History of Congestive Heart Failure (%) | 282 (13.4) | 205 (15.5) | |
Hypertension Requiring Medication (%) | 1384 (65.5) | 936 (70.6) | |
Acute Renal Failure (%) | 182 (8.6) | 109 (8.2) | |
Dialysis (%) | 225 (10.7) | 241 (18.2) | |
Disseminated Cancer (%) | 62 (2.9) | 85 (6.4) | |
Open Wound/Wound Infection (%) | 678 (32.1) | 526 (39.7) | |
Steroid Use for Chronic Condition (%) | 200 (9.5) | 176 (13.3) | |
Weight Loss (%) | 141 (6.7) | 136 (10.3) | |
Bleeding Disorder (%) | 497 (23.5) | 352 (26.5) | |
Transfusion (%) | 268 (12.7) | 180 (13.6) | |
Return to Operating Room = Yes (%) | 743 (35.2) | 315 (23.8) | |
Superficial Incisional Surgical Site Infection (%) | 112 (5.3) | 33 (2.5) | |
Deep Incisional Surgical Site Infection (%) | 70 (3.3) | 33 (2.5) | |
Organ Space Surgical Site Infection (%) | 168 (8.0) | 76 (5.7) | |
Wound Disruption (%) | 95 (4.5) | 53 (4.0) | |
Pneumonia (%) | 959 (45.4) | 494 (37.3) | |
Unplanned Intubation (%) | 2112 (100.0) | 1326 (100.0) | |
Pulmonary Embolism (%) | 59 (2.8) | 30 (2.3) | |
Progressive Renal Insufficiency (%) | 85 (4.0) | 53 (4.0) | |
Acute Renal Failure (%) | 168 (8.0) | 137 (10.3) | |
Urinary Tract Infection (%) | 264 (12.5) | 115 (8.7) | |
Stroke/Cerebrovascular Accident (%) | 62 (2.9) | 49 (3.7) | |
Cardiac Arrest (%) | 174 (8.2) | 472 (35.6) | |
Myocardial Infarction (%) | 71 (3.4) | 87 (6.6) | |
Transfusions (%) | 472 (22.3) | 349 (26.3) | |
Deep Vein Thrombosis Requiring Therapy (%) | 186 (8.8) | 69 (5.2) | |
Sepsis (%) | 393 (18.6) | 156 (11.8) | |
Septic Shock (%) | 614 (29.1) | 527 (39.7) | |
Rights and permissions
About this article
Cite this article
Clifton, J.C., Engoren, M., Shotwell, M.S. et al. The Impact of Functional Dependence and Related Surgical Complications on Postoperative Mortality. J Med Syst 46, 6 (2022). https://doi.org/10.1007/s10916-021-01779-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-021-01779-8