Abstract
Purpose
The use of open intra-peritoneal onlay mesh repairs (O-IPOMs) for treating medium/large incisional ventral hernias has come into question due to the development of minimally invasive and sublay procedures. This study aimed to identify factors that are associated with the use of O-IPOMs in France.
Methods
We analysed prospectively collected data from the French Hernia Registry on incisional ventral hernia repairs (IVHR) for hernias ≥ 4 cm in width.
Results
We obtained data for 2261 IVHR (from 11/09/2011 to 30/03/2020): 733 O-IPOMs and 1,528 other techniques. We found that the O-IPOMs were performed on patients with more patient-related risk factors compared with the other techniques. Specifically, there was a higher proportion of patients with ASA III/IV (40.47% vs. 28.02%; p < 0.00001) and at least one patient-related risk factor (66.17% vs. 58.51%; p = 0.0005). Of the 733 O-IPOMs, 195 used Ventrio ST™ (VST), the most commonly used mesh for such IPOMs in our database; the other 538 O-IPOMs used other meshes (OM). The VST subgroup had a higher proportion of patients with ASA III/IV (52.58% vs. 36.07%; p < 0.0001) and on anticoagulants (26.04% vs. 18.41%; p = 0.0229) compared with the OM subgroup; they also had a lower recurrence rate after 2 years (5.83% vs. 15.41%; p = 0.008). However, large (≥ 10 cm) or lateral defects were more common in the OM subgroup, and their mesh/defect area ratio was lower.
Conclusion
O-IPOMs were performed on patients with more comorbidities and/or complex incisional hernias compared with other techniques.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intraperitoneal onlay mesh repair (IPOM) [1] is widely used to treat incisional ventral hernias. It can be carried out using minimally invasive techniques, either laparoscopy [2], including with robots [3], or open surgery with small hernia patches [4, 5] for very small defects. The use of IPOMs increased following the development of bilayer (or covered) meshes, which are designed to minimise the risk of adhesions and complications related to contact with the viscera. However, there has been recent concern about late complications related to the intraperitoneal meshes [6], increased morbidity during repeat operations (e.g., related to inadvertent enterotomy [7, 8]) and higher rates of recurrence for larger defects [9] than when using preperitoneal (underlay) and/or retro-rectus (sublay) (1) mesh placement. As a result, the use of preperitoneal sublay repairs is currently increasing, as in previous years, boosted by advances in minimally invasive surgery (MIS), robotic [10], open and combined surgical techniques [11].
At present, the place of Open-IPOMs (O-IPOMs) in the surgical armamentarium appears questionable, given the advantages of minimally invasive IPOMs and sublay techniques. However, in a recent Expert Consensus, it was stated that ‘for open elective incisional hernia repair, sublay mesh location is preferred, but open intraperitoneal onlay mesh may be useful in certain settings’ [12]. As there is little research on this topic [13], we aimed to identify the ‘settings’ in which O-IPOM is performed. We hypothesised that surgeons favour quick and safe procedures when there are hernia-related or patient-related risk factors, such as patients on anticoagulants. We also aimed to determine whether the Ventrio ST™ (VST) mesh, the most frequently used mesh for medium/large O-IPOMs in our database, presents advantages compared with other O-IPOM meshes.
Materials and methods
Study design
We conducted a descriptive study based on prospectively collected data from the French Hernia Registry [14]. We included data for incisional ventral hernia repairs (IVHR) that were carried out to treat midline or lateral incisional ventral hernias that were ≥ 4 cm in width and classified as W2/W3 according to the European Hernia Society (EHS) classification [15]. Data were included that were collected from 11/09/2011 to 30/03/2020. Data were excluded for repairs that were carried out to treat smaller (W1) incisional hernias, primary ventral hernias, lumbar hernias or parastomal hernias. Data were also excluded for repairs that used biological or slowly absorbable meshes.
The first aim of the study was to determine the prevalence of patient-related and hernia-related risk factors for patients who were treated using O-IPOM compared with other techniques. The second aim was to compare the early/2-year outcomes and risk factors for patients treated using the Ventrio ST mesh (the most commonly used O-IPOM mesh in our database for treating incisional hernias ≥ 4 cm in width) versus other O-IPOM meshes (OM).
French Hernia Registry
The French Hernia Registry is a secure online national database (Club-Hernie.com) for members of the French Hernia Club, which has been running since 11/09/2011. Details concerning the registry have been previously described [16]. The French Hernia Registry platform also hosts a number of prospective cohort studies, including a study run by the French Society of Surgery (AFC) [17], which involved 61 hospitals in several French-speaking countries. Data from this AFC cohort were also included in the present study.
Follow-up
The follow-up of patients in the database is carried out by a self-employed clinical research assistant. This involves structured telephone interviews that are conducted after 1, 2 and 5 years (± 3 months). The interviews are based on a questionnaire that has been administered since 1999 [18]. A patient is considered to be lost to follow-up (LTFU) if they cannot be contacted after five attempts on different days and at different times. If the patients report any symptoms, they are strongly advised to make an appointment to see their surgeon. Data are entered into the Registry concerning the results of physical examination, CT scans, recurrence, reoperation, adverse events and medication changes.
Ethics
This retrospective study used data that was prospectively collected in the French Hernia Registry. The study complies with the General Data Protection Regulation (GDPR), French legal requirements (CNIL MR4: 2,212,908) and local ethical standards (institutional review board approval: IRB00010835).
Data
The data included demographics, patient-related risk factors, hernia-related risk factors (including the Altemeier classification [19]), operative data and postoperative complications, including surgical site occurrences (SSO), surgical site infections (SSI), organ space complications [20] and the Clavien-Dindo classification [21]. The data also included postoperative pain, as assessed using a visual analogic scale (VAS; 1–10) at days 0, 1 and 8 as well as 1-month post-surgery. Data concerning hernia recurrence and late adverse events were collected during the follow-up interviews (at 1 and 2 years). Recurrence was classified as either reoperated or not reoperated but confirmed by CT scan, ultrasound and/or medical examination by a surgeon. Chronic pain was assessed using the VRS-4 (verbal rating scale: no pain, mild pain or discomfort, moderate pain, severe pain)[22].
O-IPOM: surgical techniques
After adhesiolysis, and replacing the hernia contents in the abdominal cavity, the non-absorbable mesh is placed intraperitoneally, secured with sutures and/or tacks, and the wound (midline or lateral defect) is closed (bridging repairs were excluded) with slowly absorbable sutures. The technical details are displayed on tables and in the result section.
Ventrio ST™ mesh
The Ventrio™ ST mesh (VST; Davol Inc., Subsidiary of C.R. Bard, Inc, Warwick, R.I. 02886, US) is a self-expanding (absorbable memory ring), uncoated, monofilament polypropylene patch. On its visceral side, it is covered with an absorbable hydrogel barrier, based on Sepra™ Technology, and it has a pocket designed to facilitate fixation.
Primary measures of interest Patient- and hernia-related risk factors.
Secondary measures of interest Operation duration and early/late outcomes, including the recurrence rate, late adverse events and chronic pain.
Statistical analysis
Categorical variables were presented using numbers and percentages; comparisons were carried out using Chi2 tests (or Fisher’s exact tests, when necessary). Continuous data were presented as the mean with the standard deviation (SD) or the median with the interquartile range (IQR); comparisons were carried out using Student t-tests. Statistical significance was inferred for p < 0.05.
Results
Flow chart (Fig. 1)
Data were obtained for 2,261 IVHR that were carried out between 11/09/2011 and 30/03/2020. The incisional hernias were ≥ 4 cm in width and classified as W2/W3 according to the EHS classification [15]. The IVHR included 482 operations from the AFC study (from 01/10/2015 to 31/03/2016) [17].
There were 733 (32.42%) operations that used O-IPOM; other techniques were used for the remaining 1,528 operations. The latter included 502 (22.20%) laparoscopic IPOM (L-IPOM), 790 (34.94%) open-sublay repairs, 51 (2.26%) robotic-sublay repairs, 51 (2.26%) open-onlay repairs, 102 (4.51%) open-suture repairs, and 32 (1.42%) non-specified procedures.
The O-IPOM used VST meshes for 195 operations and OM for the remaining 538 operations. The patients who received these different meshes (VST or OM) were compared in terms of their risk factors, postoperative outcomes, postoperative pain and follow-up results. The proportion of patients in these two groups remained relatively stable throughout the follow-up period.
Trends in surgical procedures for IVHR (Figs. 2 and 3)
Trends in the proportion of W2/W3 incisional ventral hernia repairs that use IPOM vs. sublay mesh placement. NB. 2011 and 2020 are not full years (4 months and 3 months, respectively); the W2/W3 classification is according to the European Hernia Society [15]; IPOM: intraperitoneal onlay mesh; sublay: sublay mesh placement
Trends in the proportion of open vs. laparoscopic IPOM for treating W2/W3 incisional ventral hernias. NB. 2011 and 2020 are not full years (4 months and 3 months, respectively); the W2/W3 classification is according to the European Hernia Society [15]; IPOM intraperitoneal onlay mesh, O-IPOM open IPOM, L-IPOM laparoscopic IPOM
The surgical procedures that are used for IVHR have evolved over the years. Figure 2 shows that the proportion of IPOMs (both open and laparoscopic) in our database steadily decreased over the study period, while the proportion of extraperitoneal (sublay) procedures increased and eventually exceeded the IPOMs. As these were the two main techniques that were used, the two curves can be seen to mirror each other. In Fig. 3, it can be seen that the proportion of O-IPOMs steadily decreased while the proportion of L-IPOMs increased, with a 50:50 ratio by the end of the study period. Marked changes can be seen in the central sections of the curves for both Figs. 2 and 3, which correspond to the inclusion of data from the AFC study from 01/10/2015 to 31/03/2016 [17]. During this period, the proportion of IPOMs decreased (Fig. 2) and the ratio of O-IPOMs/L-IPOMs increased (Fig. 3).
Comparison of O-IPOMs and other techniques
Patient-related risk factors (Table 1)
The patients who had O-IPOMs had significantly more comorbidities than those who had IVHR using other techniques (control group). Specifically, 40.47% of the patients in the O-IPOM group had an American Society of Anaesthesiologists (ASA) physical status classification of III/IV compared with 28.02% in the control group (p < 0.00001). In addition, the proportion of patients with at least one risk factor (e.g., current smoker, diabetic) was significantly higher in the O-IPOM group than in the control group (66.17% vs 58.51%; p = 0.0005).
Hernia-related risk factors (Table 2)
There were no statistically significant differences between the O-IPOM and control groups apart from the number of concurrent small bowel resections (0.55% vs. 1.57%; p = 0.0416).
Comparison of O-IPOMs using VST vs. other meshes
Analyses were run to compare the 195 patients who had O-IPOMs using VST with the 538 patients who had O-IPOMs using OM (37 different types). All of the meshes were designed for intraperitoneal placement.
Patient-related risk factors (Table 3)
A higher proportion of patients in the VST subgroup had an ASA classification of III/IV compared with the OM subgroup (52.58% vs. 36.07%; p < 0.0001); there were also more patients on anticoagulants (26.04% vs. 18.41%; p = 0.0229). Of note, the different subcategories of anticoagulants or antiplatelet drugs were not specified in the database and so could not be analysed further. We also found that the proportion of patients with a history of chemotherapy and/or radiotherapy was significantly higher in the OM subgroup (4.17% vs. 12.90%; p = 0.0008). There were no statistically significant differences between the subgroups in terms of the demographic characteristics or other risk factors, including those related to abdominal pressure.
Hernia-related risk factors (Table 4)
There were no statistically significant differences between the VST and OM subgroups in terms of the hernia-related risk factors. However, the proportion of patients with at least one of these risk factors was significantly higher in the OM subgroup (47.03% vs. 34.87%; p = 0.0034). It was also found that there was less antibiotic prophylaxis in the OM subgroup.
Intra-operative data (Table 5)
The proportion of patients with midline defects was significantly higher in the VST subgroup compared with the OM subgroup (90.59% vs. 82.07%; p = 0.0078), while the proportion of patients with lateral defects was significantly lower (VST: 9.41% vs. OM: 17.93%; p = 0.0078). There was also a higher median mesh/defect surface area ratio (11.01 cm2 vs. 5.06 cm2; p < 0.0001) and larger overlap in the VST subgroup (p = 0.0005), which can be attributed to this subgroup having smaller defects and larger meshes (Table 5). The mean defect area was larger than the median area in both subgroups (VST: 56.61 cm2 vs. 36 cm2; OM: 89.52 cm2 vs. 42 cm2), particularly in the OM subgroup, as this group had some particularly large defects.
The method of mesh fixation differed significantly between the subgroups (p < 0.0001) and was mainly performed using absorbable tacks in the VST subgroup (57.0%) and sutures in the OM subgroup (64.4%).
Operation duration
The median operative time was significantly shorter in the VST subgroup compared with the OM subgroup (50 min vs. 65 min; p < 0.0001), with a difference of around 15 min.
30-day postoperative outcomes (Table 6)
The 30-day postoperative complications were not found to differ significantly between the VST and OM subgroups, neither in terms of their incidence nor their severity. We found that there were 33 patients (16.92%) in the VST subgroup and 98 (18.21%) in the OM subgroup (p = 0.7724) who had at least one complication. For patients with more than one complication, the most severe was used for the Clavien-Dindo grading.
In terms of the specific complications that occurred, there was bowel obstruction (or postoperative ileus) in 20 of the 733 patients (2.73%) who had O-IPOM; all of these resolved without reoperation after a median (IQR) hospital stay of 7 (4–11) days. Intraperitoneal bleeding was found to occur in three patients (VST subgroup: one patient; OM subgroup: two patients), all of whom were reoperated. A mesh infection occurred in eight patients (VST subgroup: three patients; OM subgroup: five patients), all of whom required reoperation. The median (IQR) hospital stay for these eight patients was 10 (5–33) days. Of note, three of these patients were on anticoagulants, one had a history of chemotherapy, and all had been given antibiotic prophylaxis.
Other complications that occurred included periprosthetic fluid collection. This was found in one patient (0.5%) in the VST subgroup (which resolved spontaneously) and in seven patients (1.3%) in the OM subgroup, three of whom required treatment (including CT-guided percutaneous drainage). General complications also occurred, which accounted for almost half of all the complications. These affected 17 patients (8.72%) in the VST subgroup and 49 (9.11%) in the OM subgroup (p = 0.8706). However, it is relevant to note that 82% of the postoperative complications were benign (Clavien-Dindo I/II), and more than 80% of the patients did not have any postoperative complications (uneventful postoperative course).
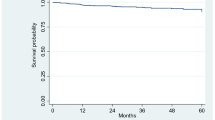
Recurrence and late adverse events (Table 8)
The median (IQR) follow-up duration was 26 (6–61) months for the VST subgroup and 24 (17–29) months for the OM subgroup. For the first follow-up, there were a total of 537 patients: 137 (70.25%) in the VST subgroup and 400 (74.35%) in OM subgroup. For the second follow-up, there were 399 patients: 120 (61.54%) in the VST subgroup and 279 (51.86%) in the OM subgroup (Fig. 1). Over this follow-up period of around 2 years, the recurrence rate was significantly lower in the VST subgroup (5.83% vs. 15.41%; p = 0.008). Two cases of bowel obstruction were noted in the OM subgroup (one operated, one not operated), while there were none in the VST subgroup. There were also two cases of late SSO in the VST subgroup (both reoperated) compared with three cases in the OM subgroup (none reoperated; p = 0.6058).
The PROM included a VRS pain assessment, which was completed by 462 patients: 122 in the VST subgroup and 340 in the OM subgroup. The proportion of patients who reported moderate or severe pain did not differ significantly between the two subgroups (14.75% vs. 14.71%; p = 0.9897).
Discussion
Key results
This multi-centre study on W2/W3 incisional hernia repairs showed that, compared to other techniques, O-IPOMs were carried out more frequently when there were patient-related risk factors. Specifically, we found that patients who had IPOMs were more likely to have an ASA classification of III/IV (40.47% vs. 28.02%; p < 0.00001); they were also more likely to have at least one patient-related risk factor (66.17% vs 58.51%; p = 0.0005). In terms of the meshes, it was found that patients who had VST were more likely to have an ASA classification of III/IV (52.58% vs. 36.07%; p < 0.0001) and to use anticoagulants (26.04% vs. 18.41%; p = 0.0229) than those who had OM. The 2-year recurrence rate was also found to be significantly lower for the patients who had VST compared with those who had OM (5.83% vs. 15.41%; p = 0.008). However, this result should be interpreted with caution because the OM subgroup had more W3 and lateral defects as well as a lower mesh/defect surface area ratio.
As in the Herniamed registry [23], we found that the proportion of IPOMs steadily decreased over time, while the proportion of sublay procedures increased (Fig. 2). Nevertheless, there was still a large number of IPOMs, with 1,235 (54.62%) operations (733 O-IPOMs and 502 L-IPOMs) out of a total of 2,261 W2/W3 incisional ventral hernia repairs. The proportion of L-IPOMs was fairly similar (22.20% vs. 27.25%) to that found in the German Herniamed registry [24] for W2/W3 IVHR, but we found a higher proportion of O-IPOMs (32.42% vs. 13.84%) and a lower proportion of open-sublay procedures (34.94% vs. 49.82%). These differences may relate to different surgical preferences and guidelines for different countries, but also to different types of hospitals. As can be seen in Figs. 2 and 3, the inclusion of patients from the AFC study [17] had a marked effect: during this period the proportion of IPOMs decreased (Fig. 2), while the ratio of O-IPOMs/L-IPOMs increased (Fig. 3). The participating centres in the AFC study were mostly public hospitals (some academic), while most of the Hernia Club founder-members work in private hospitals, where laparoscopic IPOM is frequently used as a rapid procedure that avoids large retro-muscular dissection. However, the inclusion of the AFC data did not modify the global trend lines for the whole cohort.
We found that the rates of reoperation for bowel obstruction were low following the IPOMs, as assessed at the 2-year follow-up. Specifically, this was found to be 0.4% (2/537; Table 8), which is similar to the 0.3% previously found for primary umbilical hernia (≥ 4 cm) repairs treated using L-IPOMs [25]. In addition, another study from the Danish Hernia Registry [6] found a rate of reoperation for bowel obstruction of 0.8% (9/1119) for open mesh repairs and 1.6% (28/1,757) for laparoscopic repairs.
Although the follow-up of patients in our study was conducted through telephone calls, which are not the best way to detect subclinical recurrence, they are nevertheless effective for detecting adverse events and reoperations. A recent systematic review [26] concluded that the “short-term risks of intraperitoneal placement for incisional hernia repair are not life-threatening and are comparable to other prosthetic surgical techniques”. The most serious complications that can occur following IPOMs include mesh migration, visceral erosion and enterocutaneous fistulas, and they are all generally late complications. However, fortunately, they are rare and have only been described as case reports. It is difficult to investigate the occurrence of these complications in a study such as ours, as the follow-up of patients over long periods of time (10 years or more) is challenging [27], even when nationwide comprehensive administrative records are available. Such records were used in the Danish Hernia Registry and they showed that coated polypropylene meshes were associated with fewer complications than uncoated polypropylene meshes at the 5-year follow-up (hazard ratio = 1.20; 95% CI 0.04–0.90; p = 0.04) [6].
Many previous studies, systematic reviews and meta-analyses have compared the results of O-IPOM, L-IPOM and open-sublay procedures [28,29,30]. Each of these techniques has its own advantages and drawbacks, and they may vary in terms of their clinical usefulness. In a recent Expert Consensus, guided by systematic review [12], it was agreed that “for open elective incisional hernia repair, sublay mesh location is preferred, but open intraperitoneal onlay mesh may be useful in certain settings”.
In our study, we did not primarily aim to compare the results of O-IPOM with other techniques, but rather to identify factors that may have led to O-IPOMs being performed for W2/W3 incisional ventral hernias. We were able to show that open-IPOMs were carried out more often in the presence of patient-related risk factors (Table 1). Specifically, patients who had O-IPOM were more likely to have an ASA classification of III/IV compared with those who were operated using other techniques (40.47% vs. 28.02%; p < 0.00001); in addition, they were more likely to have at least one patient-related risk factor (66.17% vs 58.51%; p = 0.0005). We also analysed hernia-related risks factors (Table 2) and found that there were no statistically significant group differences for the Altemeier classification or the use of antibiotic prophylaxis. Of note, the latter was not recorded for almost 10% of cases; this could have been due to missing data or to misinterpretation of the old French guidelines, which were not as clear as the current version (revised in 2018). We found that concurrent small bowel resection was rarer in patients undergoing O-IPOM compared with other techniques. In general, O-IPOMs are not recommended when there is concurrent enterotomy, although in rare cases an alternative technique may not be possible. For instance, in complex cases, O-IPOMs tend to be used to treat large incisional hernias [31, 32], and they have even been described as “a desperate solution to solve a complex problem when there is no other alternative due to anatomical conditions after previous surgery” [13]. However, such cases were not reported in our cohort, probably because biological and slowly absorbable meshes were not included.
The second aim of our study was to compare patients who were treated using the VST mesh with those treated using other meshes. The VST, which was designed to facilitate and shorten the O-IPOM procedure, is the most-frequently used mesh for medium/large O-IPOMs in our registry. We focused on W2/W3 defects because the treatment of smaller defects (W1) can be very different, especially when using small ventral hernia patches [4, 5, 33]. We found that patients in the VST subgroup were more likely to have an ASA classification of III/IV compared with the OM subgroup (52.58% vs. 36.07%; p < 0.0001); this classification concerned over half of the VST patients (Table 3). We also found that around two-thirds of the patients in the VST subgroup had at least one patient-related risk factor, and that more than a quarter suffered from conditions requiring anticoagulants, which is a well-known risk factor [24, 34]; this latter proportion was significantly higher in the VST than in the OM subgroup (26.04% vs. 18.41%; p = 0.0229). Conversely, a history of chemotherapy and/or radiotherapy was more common in the OM subgroup (4.17% vs. 12.90%; p = 0.0008), as was the presence of at least one hernia-related risk factor (47.03% vs. 34.87%; p = 0.0034). There were also more patients with no antibiotic prophylaxis in the OM subgroup, although the reason for this is unclear. Of note, none of the 61 patients in OM subgroup for whom antibiotic prophylaxis was not recorded developed a mesh infection.
Differences were found between the VST and OM subgroups in terms of the mesh/defect surface area ratio (Table 5; 11.01 vs. 5.06; p < 0.0001). The ratio was twice as large in the VST subgroup, which can be attributed to a smaller defect width (5 cm vs. 6 cm; p = 0.0006) and a larger mesh area (456 cm2 vs. 300 cm2; p < 0.0001) with more overlap ≥ 5 cm (64.42% vs. 60.37%; p = 0.0005). These findings may relate to the higher proportion of midline repairs for the VST subgroup (90% of the VST procedures), as it is easier to insert a large mesh for midline repairs than for some lateral repairs. In addition, the surrounding pocket of the VST facilitates secure far-lateral stapling, which may have encouraged the surgeons to choose a larger mesh. We also found that there was more variation in the size of the defect in the OM subgroup. This could be attributed to some rare, complex cases that required very large meshes. As a result, the difference between the mean and median defect area was larger in the OM subgroup (89.52 cm2 vs. 42 cm2) than in the VST subgroup (56.61 cm2 vs. 36 cm2).
We found that mesh fixation was performed using tacks more frequently in the VST subgroup than in the OM subgroup (Table 5). This may relate to the design of the VST mesh, which is equipped with a surrounding pocket to facilitate secure stapling. As the exposed part of the staple is covered by the pocket tissue, it has no direct contact with the bowels, thus reducing the risk of adhesions. The VST also has an antiadhesive layer, based on Seprafilm™ technology (widely studied and reviewed by the Cochrane collaboration) [35], which is reabsorbed within 30 days after having provided visceral protection during the critical postoperative healing period.
The median operative time for O-IPOMs using VST was 15 min shorter than for those using OM (50 min. vs. 65 min; Table 5). This difference is statistically highly significant (p < 0.0001) and clinically relevant, given the 23% reduction in the operation duration. This finding is likely to relate to the VST mesh design, as described above.
The 30-day postoperative outcomes were analysed for the VST and OM subgroups (Table 6). No statistically significant differences were found between the two groups. The outcomes are in line with the high incidence of patient-related and hernia-related risk factors in both groups (Table 3, Table 4). General complications accounted for almost half of the complications, affecting 17 patients (8.7%) in the VST subgroup and 49 patients (9.11%) in the OM subgroup, including two deaths.
Other complications that occurred within 30 days following surgery included postoperative ileus or early postoperative bowel obstruction, which affected four patients (2.05%) in the VST subgroup and 16 patients (2.97%) in the OM subgroup (p = 0.4980). All of these patients recovered without reoperation after a median (IQR) hospital stay of 7 (4–11) days. These percentages are in line with those found after L-IPOM [36] and are much lower than those reported for colorectal surgery [37]. Early mesh infection was also found to occur, affecting three patients (1.54%) in the VST subgroup and five patients (0.93%) in the OM subgroup (p = 0.4445), all of whom were reoperated. These rates are lower than the 4% reported in a large recent meta-analysis [38]. Four of the eight patients with mesh infection had patient-related risk factors: anticoagulant therapy for three patients and a history of chemotherapy for one patient. Intraperitoneal bleeding and superficial hematomas were found to be rare following surgery, even though there were patient-related risk factors, particularly anticoagulant therapy. This supports the safety of O-IPOMs even when such risk factors are present. The median hospital stay (Table 6) was one day longer for the VST subgroup than for the OM subgroup, which may relate to higher levels of pain at days 0 and 1 (Table 7), possibly resulting from stapling. Although the differences in pain between the subgroups are statistically significant, they are not clinically significant, with a difference of just one VAS point; and by day 30, the median VAS was zero for both subgroups.
The follow-up rate at 1 year (70.25% vs. 74.35%) and 2 years (61.54% vs. 51.86%) was similar for the two subgroups, as was the timing of the 2-year follow-up (26 vs. 24 months). Over the 2 years, it was found that bowel obstruction was very rare, with no cases occurring in the VST subgroup (0.00%) and just three cases (0.75%) occurring in the OM subgroup, with two requiring reoperation. This incidence is lower than that found in a recent review (ranging from 1.1 to 3.7%), which examined complications that occurred following intraperitoneal mesh repairs for incisional hernias [26]. These results indicate that O-IPOMs can be used to treat incisional hernias without increasing of the risk of small bowel obstruction. However, larger studies of a longer duration are required to more reliably determine the incidence of bowel obstruction as well as the incidence of mesh complications, which can occur very late on [39].
Other complications that were identified in our study include surgical site occurrences, which affected two patients in the VST subgroup (both reoperated) and three patients in the OM subgroup (none reoperated; p = 0.6058, Table 8). There was also chronic pain (moderate/severe), which affected a similar proportion of patients in the two subgroups (14.75% vs. 14.71%; p = 0.9897). Such pain is common after incisional ventral hernia repairs [40], especially IPOMs [28]. In the Herniamed study, it was found that this pain did not relate to mesh fixation using tacks [28]. While the possibility of chronic pain must be taken into consideration when decision making with the patient, especially when patients have few symptoms [40], there may be little choice when seeking a solution for frail patients with comorbidities.
The recurrence rate was found to be the only significant difference between the two subgroups in terms of the late outcomes. This was significantly lower for the VST subgroup (5.83% vs. 15.41%; p = 0.008). This result should be interpreted with caution because, as described above, the OM subgroup had a smaller mesh/defect surface area ratio, more W3 hernias and more lateral defects, which are known to relate to poorer outcomes [28].
Limitations
The main limitation of the present study is that this was a descriptive study, based on prospectively collected, non-randomised data. Although propensity score matching was initially considered, this was not carried out because the study aimed to describe the real-life settings in which O-IPOMs were performed; this would have been hindered by a propensity score based on patient-related or hernia-related risk factors.
Conclusion
This observational study included 733 O-IPOMs that were performed to treat W2/W3 incisional ventral hernias. The results showed that, compared with other techniques, O-IPOMs were used more often to treat frail patients with comorbidities, most probably when the priority was to perform a quick and safe procedure. We also found that, in our registry, the VST was mainly used for regular midline, medium/large incisional ventral hernia repairs in frail patients, especially those taking anticoagulants, where a quick and safe repair may be considered the wisest option.
Data availability statement
Data was extracted from Club-Hernie registry (club-hernie.com).
References
Parker SG, Halligan S, Liang MK, Muysoms FE, Adrales GL, Boutall A et al (2020) International classification of abdominal wall planes (ICAP) to describe mesh insertion for ventral hernia repair. Br J Surg 107(3):209–217. https://doi.org/10.1002/bjs.11400
Bittner R, Bain K, Bansal VK, Berrevoet F, Bingener-Casey J, Chen D et al (2019) Update of Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS))—part A. Surg Endosc 33(10):3069–3139. https://doi.org/10.1007/s00464-019-06907-7
Petro CC, Thomas JD, Tu C, Krpata DM, Beffa LR, Rosen MJ et al (2022) Robotic vs laparoscopic ventral hernia repair with intraperitoneal mesh: 1-year exploratory outcomes of the PROVE-IT randomized clinical trial. J Am Coll Surg 234(6):1160–1165. https://doi.org/10.1097/XCS.0000000000000171
Berrevoet F, D’Hont F, Rogiers X, Troisi R, de Hemptinne B (2011) Open intraperitoneal versus retromuscular mesh repair for umbilical hernias less than 3 cm diameter. Am J Surg 201(1):85–90
Berrevoet F, Doerhoff C, Muysoms F, Hopson S, Muzi MG, Nienhuijs S et al (2017) A multicenter prospective study of patients undergoing open ventral hernia repair with intraperitoneal positioning using the monofilament polyester composite ventral patch: interim results of the PANACEA study. Med Devices (Auckl) 10:81–88. https://doi.org/10.1016/j.amjsurg.2010.01.022
Kokotovic D, Bisgaard T, Helgstrand F (2016) Long-term recurrence and complications associated with elective incisional hernia repair. JAMA 316(15):1575–1582. https://doi.org/10.1001/jama.2016.15217
Patel PP, Love MW, Ewing JA, Warren JA, Cobb WS, Carbonell AM (2017) Risks of subsequent abdominal operations after laparoscopic ventral hernia repair. Surg Endosc 31(2):823–828. https://doi.org/10.1007/s00464-016-5038-z
Sharma A, Chowbey P, Kantharia NS, Baijal M, Soni V, Khullar R (2018) Previously implanted intra-peritoneal mesh increases morbidity during re-laparoscopy: a retrospective, case-matched cohort study. Hernia 22(2):343–351. https://doi.org/10.1007/s10029-017-1686-8
Holihan JL, Nguyen DH, Nguyen MT, Mo J, Kao LS, Liang MK (2016) Mesh location in open ventral hernia repair: a systematic review and network meta-analysis. World J Surg 40(1):89–99. https://doi.org/10.1007/s00268-015-3252-9
Belyansky I, Reza Zahiri H, Sanford Z, Weltz AS, Park A (2018) Early operative outcomes of endoscopic (eTEP access) robotic-assisted retromuscular abdominal wall hernia repair. Hernia 22(5):837–847. https://doi.org/10.1007/s10029-018-1795-z
Ngo P, Cossa JP, Largenton C, Pelissier E (2022) Mid-term results of VTEP (Ventral hernia repair by Totally ExtraPeritoneal approach). Surg Endosc 36(7):5313–5318. https://doi.org/10.1007/s00464-021-08911-2
Liang MK, Holihan JL, Itani K, Alawadi ZM, Gonzalez JR, Askenasy EP et al (2017) Ventral hernia management: expert consensus guided by systematic review. Ann Surg 265(1):80–89. https://doi.org/10.1097/SLA.0000000000001701
Kockerling F, Lammers B (2018) Open intraperitoneal onlay mesh (IPOM) technique for incisional hernia repair. Front Surg 5:66. https://doi.org/10.3389/fsurg.2018.00066
Kyle-Leinhase I, Kockerling F, Jorgensen LN, Montgomery A, Gillion JF, Rodriguez JAP et al (2018) Comparison of hernia registries: the CORE project. Hernia 22(4):561–575. https://doi.org/10.1007/s10029-017-1724-6
Muysoms FE, Miserez M, Berrevoet F, Campanelli G, Champault GG, Chelala E et al (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13(4):407–414. https://doi.org/10.1007/s10029-009-0518-x
Gillion JF, Lepere M, Barrat C, Cas O, Dabrowski A, Jurczak F et al (2019) Two-year patient-related outcome measures (PROM) of primary ventral and incisional hernia repair using a novel three-dimensional composite polyester monofilament mesh: the SymCHro registry study. Hernia 23(4):767–781. https://doi.org/10.1007/s10029-019-01924-w
Romain B, Renard Y, Binquet C, Poghosyan T, Moszkowicz D, Gillion JF et al (2020) Recurrence after elective incisional hernia repair is more frequent than you think: An international prospective cohort from the French Society of Surgery. Surgery 168(1):125–134. https://doi.org/10.1016/j.surg.2020.02.016
Gillion JF, Fagniez PL (1999) Chronic pain and cutaneous sensory changes after inguinal hernia repair: comparison between open and laparoscopic techniques. Hernia 3:75–80. https://doi.org/10.1007/BF01194609
Culbertson WR, Altemeier WA, Gonzalez LL, Hill EO (1961) Studies on the epidemiology of postoperative infection of clean operative wounds. Ann Surg 154:599–610. https://doi.org/10.1097/00000658-196110000-00010
DeBord J, Novitsky Y, Fitzgibbons R, Miserez M, Montgomery A (2018) SSI, SSO, SSE, SSOPI: the elusive language of complications in hernia surgery. Hernia 22(5):737–738. https://doi.org/10.1007/s10029-018-1813-1
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Loos MJ, Houterman S, Scheltinga MR, Roumen RM (2008) Evaluating postherniorrhaphy groin pain: visual analogue or verbal rating scale? Hernia 12(2):147–151. https://doi.org/10.1007/s10029-007-0301-9
Kockerling F, Hoffmann H, Mayer F, Zarras K, Reinpold W, Fortelny R et al (2021) What are the trends in incisional hernia repair? Real-world data over 10 years from the Herniamed registry. Hernia 25(2):255–265. https://doi.org/10.1007/s10029-020-02319-y
Kockerling F, Hoffmann H, Adolf D, Reinpold W, Kirchhoff P, Mayer F et al (2021) Potential influencing factors on the outcome in incisional hernia repair: a registry-based multivariable analysis of 22,895 patients. Hernia 25(1):33–49. https://doi.org/10.1007/s10029-020-02184-9
Frey S, Jurczak F, Fromont G, Dabrowski A, Soler M, Cossa JP et al (2021) Are the relative benefits of open versus laparoscopic intraperitoneal mesh repair of umbilical hernias dependent on the diameter of the defect? Surgery 171(2):419–427. https://doi.org/10.1016/j.surg.2021.08.003
Soare AM, Cartu D, Nechita SL, Andronic O, Surlin V (2021) Complications of intraperitoneal mesh techniques for incisional hernia—a systematic review. Chirurgia (Bucharest, Romania) 116(6 Suppl):S36–S42
Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J (2004) Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240(4):578–583. https://doi.org/10.1097/01.sla.0000141193.08524.e7. (discussion 83-5)
Kockerling F, Lammers B, Weyhe D, Reinpold W, Zarras K, Adolf D et al (2021) What is the outcome of the open IPOM versus sublay technique in the treatment of larger incisional hernias?: a propensity score-matched comparison of 9091 patients from the Herniamed Registry. Hernia 25(1):23–31. https://doi.org/10.1007/s10029-020-02143-4
Fafaj A, Petro CC, Tastaldi L, Alkhatib H, AlMarzooqi R, Olson MA et al (2020) Intraperitoneal versus retromuscular mesh placement for open incisional hernias: an analysis of the Americas Hernia Society Quality Collaborative. Br J Surg 107(9):1123–1129. https://doi.org/10.1002/bjs.11560
Yeow M, Wijerathne S, Lomanto D (2022) Intraperitoneal versus extraperitoneal mesh in minimally invasive ventral hernia repair: a systematic review and meta-analysis. Hernia 26(2):533–541. https://doi.org/10.1007/s10029-021-02530-5
Eriksson A, Rosenberg J, Bisgaard T (2014) Surgical treatment for giant incisional hernia: a qualitative systematic review. Hernia 18(1):31–38. https://doi.org/10.1007/s10029-013-1066-y
Deerenberg EB, Timmermans L, Hogerzeil DP, Slieker JC, Eilers PH, Jeekel J et al (2015) A systematic review of the surgical treatment of large incisional hernia. Hernia 19(1):89–101. https://doi.org/10.1007/s10029-014-1321-x
DA Gillion JF, Jurczak F, Dugue T, Bonan A, Chollet JM (2018) Patient Reported Outcomes Measures (PROM) two years after treatment of small ventral hernias using a monofilament polypropylene patch covered with an absorbable hydrogel barrier on its visceral side. Int J Abdom Wall Hernia Surg 1:99–108
Staerkle RF, Hoffmann H, Kockerling F, Adolf D, Bittner R, Kirchhoff P (2018) Does coagulopathy, anticoagulant or antithrombotic therapy matter in incisional hernia repair? Data from the Herniamed Registry. Surg Endosc 32(9):3881–3889. https://doi.org/10.1007/s00464-018-6127-y
Kumar S, Wong PF, Leaper DJ (2009) Intra-peritoneal prophylactic agents for preventing adhesions and adhesive intestinal obstruction after non-gynaecological abdominal surgery. Cochrane Database Syst Rev 1:CD005080. https://doi.org/10.1002/14651858.CD005080.pub2
Domen A, Stabel C, Jawad R, Duchateau N, Fransen E, Vanclooster P et al (2021) Postoperative ileus after laparoscopic primary and incisional abdominal hernia repair with intraperitoneal mesh (DynaMesh(R)-IPOM versus Parietex Composite): a single institution experience. Langenbecks Arch Surg 406(1):209–218. https://doi.org/10.1007/s00423-020-01898-9
Venara A, Alfonsi P, Cotte E, Loriau J, Hamel JF, Slim K et al (2019) Postoperative ileus concealing intra-abdominal complications in enhanced recovery programs-a retrospective analysis of the GRACE database. Int J Colorectal Dis 34(1):71–83. https://doi.org/10.1007/s00384-018-3165-9
Quiroga-Centeno AC, Quiroga-Centeno CA, Guerrero-Macias S, Navas-Quintero O, Gomez-Ochoa SA (2022) Systematic review and meta-analysis of risk factors for Mesh infection following Abdominal Wall Hernia Repair Surgery. Am J Surg 224(1):239–246. https://doi.org/10.1016/j.amjsurg.2021.12.024
Petersen K, Morrison J, Oprea V, Grischkan D, Koch A, Lorenz R et al (2021) Necessary duration of follow-up to assess complications of mesh in hernia surgery: a time-lapse study based on 460 explants. Hernia 25(5):1239–1251. https://doi.org/10.1007/s10029-020-02297-1
de Smet GHJ, Sneiders D, Yurtkap Y, Menon AG, Jeekel J, Kleinrensink GJ et al (2020) Functional outcomes in symptomatic versus asymptomatic patients undergoing incisional hernia repair: replacing one problem with another? A prospective cohort study in 1312 patients. Int J Surg 82:76–84. https://doi.org/10.1016/j.ijsu.2020.07.054
Acknowledgements
We thank those involved in the AFC study (17) for the data acquisition. We also thank the Hernia Club members for data acquisition. L. Arnalsteen (Hôpital Privé La Louvière, Lille, France), J. Atger (Polyclinique des Alpes du Sud, Gap, France), M. Beck (Clinique Ambroise Paré, Thionville, France), A. Belhassen (Clinique Blomet, Paris, France), T. Bensignor (Groupe Hospitalier Paris St Joseph, Paris, France), P. Bernard (Hôpital de Macon, Macon, France), D. Binot (MCO Côte d’Opale, Boulogne sur Mer, France), J. Bousquet (Hôpital Privé de la Chataigneraie, Montpellier, France), D. Blazquez (Clinique Jeanne d’Arc, Paris, France), A. Bonan (Hôpital Privé d’Antony, Antony, France), J. Bousquet (Hôpital Privé de la Chataigneraie, Montpellier, France), J. Cahais (Clinique Saint Hilaire, Rouen, France), O. Cas (Centre Médico Chirurgical–Fondation Wallerstein, Arès, France), A. Champault-Fezais (Groupe Hospitalier Paris St Joseph, Paris, France), P. Chastan (Bordeaux, France), J-M. Chollet (Hôpital Privé d’Antony, Antony, France), N. Christou (CHU, Limoges, France), J-P. Cossa (CMC Bizet, Paris, France), A.C. Couchard (Hôpital Privé d’Antony, Antony, France), T. Crespy (Hôpital Privé de Provence, Aix-en-Provence, France), A. Dabrowski (Clinique de Saint Omer, Saint Omer, France), T. Delaunay (Clinique St Hilaire, Rouen, France), S. Démaret (Clinique Saint Vincent, Besançon, France), S. Derieux (Hôpital de la Croix Saint Simon, Paris, France), F. Drissi (CHU Nantes, Nantes, France), V. Dubuisson (CHU Pellegrin, Bordeaux, France), C. Duchamp (Clinique du Val d’Ouest, Ecully, France), T. Dugué (Clinique Saint-Pierre, Perpignan, France), R. Fara (Hôpital Européen, Marseille, France), S. Frey (CHU, Nantes, France), G. Fromont (Clinique de Bois Bernard, Bois Bernard, France), J-F. Gillion (Hôpital Privé d’Antony, Antony, France), N. Goasguen (Hôpital de la Croix Saint Simon, Paris, France), P. Guéroult (CHU, Angers, France), A. Guillaud (Clinique du Parc, Montpellier, France), C. Jacquin (CH du Prado, Marseille, France), F. Jurczak (Clinique Mutualiste, Saint Nazaire, France), H. Khalil (CHRU Rouen, Rouen, France), G. Hoch (Hôpital UNEOS, Metz, France), C. Kupéras (Clinique Joly, Dijon, France), A. Lamblin (Hôpital Privé La Louvière, Lille, France), P. Ledaguenel (Polyclinique Jean Villar, Av. Maryse Bastié, Bruges, France), M. Lepère (Clinique Saint Charles, La Roche-sur-Yon, France), D. Lépront (Polyclinique de Navarre, Pau, France), J. H. Longeville (Clinique du Val-de-Loire, Nevers, France), N. Le Toux (Clinique Jeanne d’Arc, Paris, France), E. Magne (Clinique Tivoli, Bordeaux, France), N. Maillot (Clinique du Parc, Cholet, France), A. Mensier (Hôpital d’Arras, clinique de Béthune, Béthune, France), D. Moszkowicz (CHU Louis Mourier Colombes, France), P. Ngo (Hôpital Américain, Neuilly, France), O. Oberlin (Croix St Simon Diaconesses, Paris, France), G. Passot (CHU de Lyon Sud, Lyon, France), X. Pavis d’Escurac (Strasbourg, France), J. B. Putinier (CH Mutualiste, Grenoble, France), Y. Renard (CHRU Reims, Reims, France), B. Romain (CHU Strasbourg, Strasbourg, France), D. Sebbar (Hôpital de Saint Brieuc, Saint Brieuc, France), M. Soler (Polyclinique Saint Jean, Cagnes-sur-Mer, France), S. Roos (Clinique Claude Bernard, Albi, France), J-M. Thillois (Hôpital Privé d’Antony, Antony, France), P. Tiry (Clinique de Saint Omer, Saint Omer, France), P. Vu (HPMV, Bry sur Marne, France), R. Verhaeghe (MCO Côte d’Opale, Boulogne sur Mer, France), M. Warlaumont (CHRU Lille, Lille, France), and C. Zaranis (Clinique de La Rochelle, France).
Funding
This study was planned, conducted, and analysed under the auspices of the Hernia Club (https://www.club-hernie.com). The work was supported by an unrestricted educational grant to the Hernia Club CRO from Becton Dickinson Benelux N.V., Erembodegem-Dorp 86, 9320 Erembodegem, Belgium ("BD"). This article contains the personal and professional opinions of the individual authors and does not necessarily reflect the views and opinions of BD or any Business Unit or affiliate of BD. The funder of the present study had no role in the design and conduct of the study (collection, management, analysis, and interpretation of the data).
Author information
Authors and Affiliations
Consortia
Contributions
Concept and design: JFG; Acquisition of data: Co-authors and Hernia-Club members; Data analysis: JFG; Drafting of the manuscript: JFG; Critical revision of the manuscript: All authors; Supervision: JFG (Statistical analysis: SAS HORIANA; Editing: NEWMED Publishing).
Corresponding author
Ethics declarations
Conflict of interest
JFG has received honoraria as a consultant from BD, Cousin-Surgery, Intuitive, Medtronic, Microval, and Swing THT. GF has received honoraria as a consultant from Medtronic. Other co-authors: No competing interests related to this study.
Ethics approval
This retrospective study was approved by the local (IORG0009085) institutional review board (number: IRB00010835).
Human and animal rights
No animals involved in this study.
Informed consent
All participants provided informed consent prior to their participation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of the Hernia Club members are mentioned in Acknowledgements section.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gillion, JF., Fromont, G., Verhaeghe, R. et al. Open IPOMs for medium/large incisional ventral hernia repairs in the French Hernia Registry: factors associated with their use and mesh-related outcomes. Hernia 28, 745–759 (2024). https://doi.org/10.1007/s10029-023-02853-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-023-02853-5