Abstract
Purpose
Persistent postoperative pain (PPP) is a prevalent complication after inguinal hernia repair. The aim of this study was to develop and validate a preoperative risk score for PPP.
Methods
We developed the risk score based on a cohort of 2,508 Danish men, who answered a questionnaire six months after inguinal hernia repair performed 2015–2016. PPP was defined as a numerical rating scale score ≥ 2 during activity six months postoperatively. Logistic regression analyses were undertaken to determine statistically significant predictors of PPP. Univariable analysis selected potential predictors with a p value ≤ 0.20, and a subsequent multivariable model was built using backward elimination with a criterion of p value < 0.10. We created a risk score based on the β coefficients of the multivariable model. The risk score was validated internally using Hosmer–Lemeshow goodness of fit test, calibration belt test, and receiver operating characteristic curve analyses with 95% confidence intervals based on the bootstrap analysis. External validation was performed in a cohort of 293 men recruited preoperatively.
Results
Predictors of PPP were age 18–49 and 50–59 (versus ≥ 60) years (p < 0.001), total load lifted > 1,000 kg/day (p = 0.001), working in a bent-over position > 1 h/day (p < 0.001), leisure-time physical activity < 2 h/week (p = 0.009), increasing body mass index (per unit) (p < 0.003), and repair of recurrent hernia (p = 0.001).The preoperative risk score predicted risks of 6–61% in the development population. The model showed good internal and external validity.
Conclusion
The results suggest that the risk of PPP after inguinal hernia repair can be predicted using a preoperative risk score.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inguinal hernia repair is one of the most common procedures in general surgery with > 20 million procedures performed worldwide each year [1]. Among men, the risk of inguinal hernia repair is around ten times higher than among women [2]. The only cure for symptomatic inguinal hernia is surgical treatment. Men with an asymptomatic or minimally symptomatic inguinal hernia can be considered for watchful waiting [1], but 70% of those men will be referred for surgery within five years because of pain [1].
Persistent postoperative pain (PPP) has been reported to affect 2–30% of patients after inguinal hernia repair six months postoperatively [3, 4], with variations primarily depending on the method of pain evaluation [5], whereas surgical techniques seem less important [6]. PPP 6 months after surgery adversely affects daily life activities for 10–15% of all patients after inguinal hernia repair and 1–3% suffer from severe PPP [1, 6]. Management of PPP after inguinal hernia repair remains difficult with inconclusive results of both pharmacological and surgical treatment [1, 7,8,9]. Since management is difficult, prevention of PPP is of major importance [1]. To this end, a prediction model might be helpful for the surgeon to identify high-risk patients and guide tailoring of their treatment [1]. We have recently found a relationship between lifting > 1,000 kg/day and PPP after inguinal hernia repair, which suggests a previously untapped preventive potential [10].
Risk stratification may be an essential step forward in the prevention of PPP [11, 12]. Using a predictive model in daily practice could lead to personalised patient information, choice of surgical technique, perioperative pain management, and recommendations regarding the duration of postoperative sickness absence or temporary work modifications for high-risk patients. Identification of preoperative risk factors seems most desirable for early prevention [11]. Previous prediction models have been too complex to apply in clinical settings [13, 14], or generic rather than procedure specific (i.e. concerning various kinds of surgery rather than inguinal hernia repair specifically) [15, 16], and none of the models concerning inguinal hernia repair have been validated externally [17]. Thus, prediction models of the risk of PPP after inguinal hernia repair have so far not been translated into clinical practice [12,13,14].
This study aimed to develop and validate a simple and clinically useful risk score to identify patients with an elevated risk of PPP 6 months after inguinal hernia repair.
Methods
Design and study populations
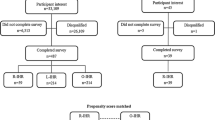
The predictive model was developed based on a 6-month follow-up study of a nationwide cohort of 2,508 Danish men (population I) and validated within a consecutive prospective cohort of 293 Danish men with follow-up at 6 months (population II). We followed the Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis (TRIPOD) statement [18]. The Danish Data Protection Agency approved the study (j.no. 1-16-02-121-15). In Denmark, register and questionnaire studies do not require approval by health research ethics committees and consent is considered given when participants return the questionnaire.
Population I.
The establishment of population I has been described previously [10]. To summarise, the cohort consisted of all men with an inguinal hernia repair according to the Danish Hernia Database in the period January 1 2015 to October 31 2016, who were born between October 1 1949 and October 1 1998 and living in Denmark (excluding Greenland) five months postoperatively. The cohort excluded patients in population II (see below), patients who were < 18 years old at the time of surgery, patients whose data was entered into the database later than five months after their inguinal hernia repair, patients who had no available address or had emigrated or died before follow-up, and patients who were not active in the labour market in the week before their surgery. All members of the cohort received a questionnaire by mail six months after their inguinal hernia repair. Of these, 2,609 (54%) answered the questionnaire and 2,508 contributed to the analyses. The mean time since surgery was 6.5 (SD 1.0) months [10]. Non-response analysis showed minor differences with respect to age (respondents were on average three years older than non-respondents) and no differences concerning the region of residence, socioeconomic status, and surgical characteristics [10].
Population II
Population II consisted of all men scheduled for inguinal hernia repair in three public hospitals in Central and North Denmark Regions, who were 18–65 years old and active in the labour market at the time of surgery, had a cell phone, and were able to understand and read Danish. Eligible patients were included in the study if they returned the preoperative questionnaire before their surgery. At 6-month follow-up, they received a questionnaire by mail. Included patients also received up to 23 short text messages in a period of 6 months postoperatively, where they were asked to report their intensity of pain in the same way as in the questionnaire. If a participant did not respond to the questionnaire at 6 months, the last short text message response was used to determine the outcome. A total of 318 men answered the preoperative questionnaire, and 212 answered the follow-up questionnaire, while short text messages could be used for a further 81 men. Thus, 293 men (92%) contributed to the analyses at follow-up.
Outcome
The outcome was PPP during the last 24 h in terms of inguinal pain on the operated side with an intensity ≥ 2 on a numerical rating scale NRS-11 during activity 6 months postoperatively [3, 18]. The NRS-11 ranged from 0 (no pain) to 10 (worst imaginable pain). The cut-off of ≥ 2 has previously been associated with daily functional impairment [13], also in population I [10].
Demographics
Age at surgery was calculated from the date of birth and the date of surgery. In population I, socioeconomic status was categorised as academics and administrative/office workers, skilled workers, and unskilled workers based on unemployment insurance fund membership [19] in the year of the inguinal hernia repair [10]. In population II, the same socioeconomic status categories were applied, only based on self-reported job titles because information on unemployment insurance fund membership was not available.
Duration of preoperative pain
Information on the duration of preoperative pain was obtained by questionnaire and categorised as ≤ 1, 2–6, and 7–48 months. Of note, the information on preoperative pain was obtained retrospectively in population I.
Occupational mechanical and psychosocial exposures
Questionnaire information on job title at the time of surgery was collected six months postoperatively in population I and preoperatively in population II. After recoding to occupational titles represented in the Danish version of the International Standard Classification of Occupations from 1988, this information was combined with a job-exposure matrix (The Lower Body JEM) [20] to assess occupational mechanical exposures in terms of time spent standing/walking (h/day) and total load lifted (kg/day). The Lower Body JEM cross-tabulates 121 homogeneously exposed job groups with the mean of five experts’ ratings of the just-mentioned exposures [20]. Working in a bent-over position might also be related to PPP through a mechanism of increased intra-abdominal pressure [21], but was not represented in the JEM. Instead, we used the self-reported number of h/day spent working in this position [22]. As described previously, the exposure estimates were adjusted according to self-reported weekly working hours [10].
Information on job demands and job control was collected by questionnaire six months postoperatively in population I and preoperatively in population II. A job strain variable was then constructed as described previously: low strain (low demands, high control), passive (low demands, low control), active (high demands, high control), and high strain (high demands, low control) [10, 23].
Lifestyle factors
Information on present lifestyle factors was collected by questionnaire 6 months postoperatively in population I and preoperatively in population II. Body mass index (BMI) was calculated as weight/(height2) and descriptively categorised as < 25, 25- < 30, and 30–56 kg/m2 – in further analyses (see below), BMI was entered as a continuous variable; leisure-time physical activity was categorised as not active (< 2 h/week) and active (≥ 2 h /week); smoking status was categorised as never, ex-, and current smoker.
Surgical characteristics
For both populations, information on surgical characteristics was obtained from the Danish Hernia Database [24]. Type of hernia repair was categorised as laparoscopic, Lichtenstein, and other (Onstep, other open technique with mesh, open technique without mesh—i.e. types that are not gold standard for inguinal hernia repair in men > 30 years according to international recommendations from 2018 [1, 25]); anatomical hernia type was categorised as lateral, medial, pantaloon, and unspecified, and repair of recurrent hernia was categorised as no and yes.
Statistical analyses
To develop the predictive model, univariable logistic regression analyses were undertaken to assess the strength of the association between each of the potential predictor variables and PPP (population I). All potential predictor variables with p values < 0.2 in these analyses were selected to be simultaneously entered into a multivariable logistic regression model, except the occupational mechanical exposure variables and socioeconomic status. Variable selection was then performed using backward elimination, using a criterion of p value < 0.10 for retention in the model. Due to expected correlations, we a priori decided to attempt to enter each of the occupational mechanical exposure variables assessed with the JEM into our logistic regression model one at a time, and not to include socioeconomic status. Duration of preoperative pain fulfilled the above criteria for inclusion in the model but was only entered in supplementary analyses due to the risk of recall bias [26].
A multivariable logistic regression model was created (model 1) following the steps outlined above. We then created a PPP risk score based on the β coefficients for model 1. Points for this score were assigned by multiplying the respective coefficients by ten times the smallest predictor coefficient in the model and rounding the result to the nearest half-point. The PPP risk score was determined as the sum of the individual point values associated with each predictor. Next, a model with the PPP risk score as the single predictor was created (model 2).
Internal validation
Calibration of models 1 and 2 was assessed by the Hosmer–Lemeshow goodness of fit test [27] and calibration belt test and plot [28, 29]. A p value > 0.05 for these tests indicates that the model is well calibrated, i.e., the model produces probabilities that accurately reflect the actual outcome experience in the data [29, 30]. Calibration belt plots depict this relationship (i.e., the relationship between the probabilities according to the model and the actual outcome experience in the data) along with confidence bands [29]. The discriminatory capability of the models was assessed by receiver operating characteristic (ROC) curve analysis. Bootstrap analysis was performed to obtain 95% confidence intervals (CI) of the area under the curve (AUC) in both models; a total of 500 computer-generated samples from population I were derived by random selection with replacement, and AUC was calculated within each bootstrap sample [31, 32].
External validation
Both models were validated in population II using calibration belt test and plot and ROC curve analysis as described above.
Results
Table 1 presents the prevalence of PPP in population I (19%) and univariable associations of PPP with demographics, duration of preoperative pain, occupational exposures, lifestyle factors, and surgical characteristics. The prevalence of PPP was higher among men aged 18–49 and 50–59 years than among men aged ≥ 60 years. Both socioeconomic status and duration of preoperative pain were related to the outcome. Patients with occupational exposures in the highest categories had an elevated prevalence of PPP. Higher odds ratios (OR) were observed among patients who were not physically active in their leisure-time and patients with a BMI ≥ 30 kg/m2, while smoking was not related to the outcome. The prevalence of PPP did not differ between anatomical hernia types, except for an elevated prevalence in the small unspecified category. No statistically significant difference was found between laparoscopic repair and Lichtenstein repair, but patients with other types of hernia repair had an elevated prevalence of PPP. Patients with the repair of a recurrent hernia had a higher prevalence of PPP than patients with repair of a first-time hernia.
Table 2 presents the multivariable model (model 1) as well as the model including only the PPP risk score (model 2). Model 1 included age, total load lifted per day, working in a bent-over position, leisure-time physical activity, BMI, and repair of recurrent hernia. Other surgical characteristics did not contribute to the model. Thus, the PPP risk score was based entirely on preoperative information. It ranged from 1.8 to 10.1 in population I corresponding to predicted risks of PPP of 6% to 61% according to model 2. The adjusted OR was 1.50 for an increment of 1 PPP risk score point. Figure 1 presents two personalised examples of how to calculate probabilities of PPP based on PPP risk scores, yielding risks of 7% and 41%.
Table 3 presents the PPP risk score performance in population I in terms of probability of PPP, sensitivity, specificity, and positive and negative predictive values at varying cut points of the score. Figure 2 presents observed and expected percentages with PPP according to the PPP risk score (model 2). The Hosmer–Lemeshow goodness of fit test demonstrated close agreement between the observed and expected counts and the p values (p = 0.85 for model 1 and p = 0.52 for model 2) indicated good calibration (cf. calibration belt test and plot in supplemental digital content) and acceptable discriminatory capability with an AUC of 0.64 (95% CI 0.61–0.67) for model 1 and 0.63 (95% CI 0.60–0.65) for model 2. In supplementary analyses, where we included duration of preoperative pain, the discriminative ability of model 1 improved (AUC = 0.69) slightly and the calibration was still excellent (p = 0.91).
The prevalence of PPP was lower in population II (12% versus 19% in population I) and skilled workers constituted 48% of population II against 30% of the population I. The mean time since surgery was similar and population II also resembled population I in other respects (results not shown). External validation (population II) of both models using calibration belt test and plot showed good calibration (supplemental digital content) and the AUCs were similar to the AUCs in the internal validation: in model 1 the AUC was 0.64 (95% CI 0.54–0.76) and in model 2 the AUC was 0.62 (95% CI 0.52–0.72).
Discussion
We created and validated a PPP risk score, which was based entirely on information available preoperatively. The risk score showed good internal validity in the developing population and performed well in a preoperative setting with another population. In particular, the models could estimate probabilities of PPP accurately in both developmental and validation data sets. Predictors of PPP were age at surgery ≤ 59 years, total load lifted > 1,000 kg/day, working in a bent-over position > 1 h/day, leisure-time physical activity < 2 h/week, increasing BMI, and repair of recurrent hernia. The PPP risk score was independent of anatomical hernia type and type of hernia repair.
We defined PPP as an NRS ≥ 2, which reflects daily functional impairment [13, 33]. The outcome was based on NRS-11 [34] 6 months postoperatively as recommended previously [6, 11, 12, 18]. We chose to leave out the duration of preoperative pain due to the retrospective nature of this information in population I. The discriminative capability of model 1 improved slightly when preoperative pain was included, but even without the inclusion of preoperative pain, the calibration was good, and the model performed well in external validation. Preoperative pain has previously been left out of prediction modelling without reducing the predictive power [15].
The main limitation of this study was the relatively small size of population II, leading to wide calibration belts in the external validation of the prediction models. Nevertheless, the observed probabilities of PPP were accurately estimated even in population II. Regarding population I, a further limitation was that the percentage that participated was not optimal (54%), but previous non-response analyses (summarized in the methods section) have not indicated selection bias [10].
Occupational lifting and standing/walking were assessed using a JEM [20]. The validity of the JEM was originally assessed by two external experts, who in general agreed with the ranking of exposures [20]. The JEM has previously shown good predictive validity in studies of total hip replacement [35], surgery for varicose veins [36], inguinal hernia repair [37,38,39], and sickness absence and permanent work disability [40]. The strength of using a JEM is the elimination of recall bias which would be an issue in the case of retrospective exposure assessment based on self-report. Working in a bent-over position was based on self-report with a risk of recall bias in population I, but since model 1 performed well in a preoperative setting (the validation population), recall bias seemed limited. Total load lifted > 1,000 kg/day and standing/walking > 6 h/day have been identified as risk factors for lateral inguinal hernia repair [37, 38, 41], prolonged convalescence after inguinal hernia repair [39], and increased prevalence of PPP [10]. Thus, we expected these exposures and working in a bent-over position to be retained in model 1, whereas we were not surprised that job strain, which was included exploratively [10], did not make it into the final models. Occupational mechanical exposures have not been included in previous models to predict PPP after inguinal hernia repair.
Repair of recurrent hernia was the only surgical characteristic, which was included in our model. In Denmark, the type of repair of a recurrent hernia depends on the initial type of repair; if the initial repair was laparoscopic, the recurrence will typically be treated by a Lichtenstein repair, and vice versa. Future studies focusing on the risk of PPP in relation to the type of repair of recurrent hernias may be warranted. Laparoscopic repair has previously been associated with a lower risk of PPP than Lichtenstein repair [42, 43], which we could not corroborate. We speculate that this may be because laparoscopic repair was previously predominantly performed by highly experienced surgeons, while this difference between the two types of hernia repair no longer pertains. In the past two decades, intensive research in surgical methods and standardisation of inguinal hernia repair have taken place in Denmark [24, 44]. For that reason, the inguinal hernia repairs in our study were to a large extent performed according to the European Hernia Society Guidelines [1], e.g. 97% of the patients had a laparoscopic or a Lichtenstein repair. A high standardisation and volume for each centre must be expected to reduce the risk of PPP in relation to different methods of inguinal hernia repair to a minimum [1]. We did not incorporate surgical experience in our model building, but surgeons’ volumes of inguinal hernia repairs seem to be of minor importance [45] and, in general, inguinal hernia repair is performed in high volume centres in Denmark [46].
The data for the study was collected from 2015 to 2018 and the prevalence of PPP at six months was consistent with the prevalence in Sweden from 2012 to 2015 [42]. It seems likely that our results can be generalised to other countries with working conditions, surgical conditions, and a health care system comparable with the Danish. Our study was restricted to men, and the results may therefore not be generalisable to women.
The prediction models estimated probabilities of PPP accurately in both developmental and validation data sets. This is valuable with a view to personalised guidance to patients and planning of perioperative measures. The PPP risk score may even be useful as a screening tool although the score’s predicted risks did not separate very clearly between those patients who did and did not develop PPP (the AUCs were all around 0.65, which is not excellent). Different trade-offs between sensitivity and specificity (cf. Table 3) may be considered depending on the risks and costs connected with potential interventions to reduce the risk.
Preoperative risk stratification could support clinical decision-making with respect to pre-, peri-, and postoperative management of patients with inguinal hernia. E.g., high-risk patients may be recommended a longer convalescence or a transient reduction of occupational mechanical exposures postoperatively (for highly exposed individuals only). A more strict postoperative follow-up concerning pain and complications may also be considered to treat early postoperative pain more efficiently [1, 8]. We believe that our model has a potential for preoperative risk stratification in clinical settings, and the PPP risk score can easily be translated to an app for use in clinical practice. A logical next step would be an impact study [47] to evaluate if preoperative risk stratification and personalised treatment strategies do indeed improve clinical decision making and lead to a reduced risk of PPP after inguinal hernia repair.
In conclusion, our results suggest that the risk of PPP after inguinal hernia repair can be predicted using a preoperative risk score based on age, occupational mechanical exposures (total load lifted per day and time per day spent working in a bent-over position), BMI, leisure-time physical activity, and repair of recurrent hernia.
Data availability
Data is not available.
Code availability
Code is not available.
References
HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22:1–165. https://doi.org/10.1007/s10029-017-1668-x
Primatesta P, Goldacre MJ (1996) Inguinal hernia repair: incidence of elective and emergency surgery, readmission and mortality. Int J Epidemiol 25:835–839
Bay-Nielsen M, Nilsson E, Nordin P, Kehlet H, for the Swedish Hernia Data Base the Danish Hernia Data Base (2004) Chronic pain after open mesh and sutured repair of indirect inguinal hernia in young males. Br J Surg 91:1372–1376. https://doi.org/10.1002/bjs.4502
Fricano S, Fiorentino E, Cipolla C et al (2010) A minor modification of Lichtenstein repair of primary inguinal hernia: postoperative discomfort evaluation. Am Surg 76:764–769
Molegraaf M, Lange J, Wijsmuller A (2017) Uniformity of chronic pain assessment after inguinal hernia repair: a critical review of the literature. EurSurg Res 58:1–19. https://doi.org/10.1159/000448706
Öberg S, Andresen K, Klausen TW, Rosenberg J (2018) Chronic pain after mesh versus nonmesh repair of inguinal hernias: a systematic review and a network meta-analysis of randomized controlled trials. Surgery 163:1151–1159
Kehlet H (2008) Chronic pain after groin hernia repair. Br J Surg 95:135–136. https://doi.org/10.1002/bjs.6111
Lange JF, Kaufmann R, Wijsmuller AR et al (2015) An international consensus algorithm for management of chronic postoperative inguinal pain. Hernia 19:33–43. https://doi.org/10.1007/s10029-014-1292-y
Andresen K, Rosenberg J (2018) Management of chronic pain after hernia repair. J Pain Res 11:675–681. https://doi.org/10.2147/JPR.S127820
Vad MV, Frost P, Rosenberg J, Svendsen SW (2019) Persistent postoperative pain after inguinal hernia repair in relation to occupational lifting and standing/walking: a 6-month follow-up study. Occup Environ Med 76:712–717. https://doi.org/10.1136/oemed-2019-105919
Schug SA, Bruce J (2017) Risk stratification for the development of chronic postsurgical pain. Pain Rep 2:e627. https://doi.org/10.1097/PR9.0000000000000627
Werner MU, Kongsgaard UE (2014) I. Defining persistent post-surgical pain: is an update required? Br J Anaesth 113:1–4. https://doi.org/10.1093/bja/aeu012
Aasvang EK, Gmaehle E, Hansen JB et al (2010) Predictive risk factors for persistent postherniotomy pain. Anesthesiology 112:957–969. https://doi.org/10.1097/ALN.0b013e3181d31ff8
Montes A, Roca G, Sabate S et al (2015) Genetic and clinical factors associated with chronic postsurgical pain after hernia repair, hysterectomy, and thoracotomy: a two-year multicenter cohort study. Anesthesiology 122:1123–1141. https://doi.org/10.1097/ALN.0000000000000611
Althaus A, Hinrichs-Rocker A, Chapman R et al (2012) Development of a risk index for the prediction of chronic post-surgical pain. Eur J Pain 16:901–910. https://doi.org/10.1002/j.1532-2149.2011.00090.x
Kalkman CJ, Visser K, Moen J, Bonsel GJ, Grobbee DE, Moons KG (2003) Preoperative prediction of severe postoperative pain. Pain 105:415–423 (S0304395903002525)
Altman DG, Vergouwe Y, Royston P, Moons KG (2009) Prognosis and prognostic research: validating a prognostic model. BMJ 338:b605. https://doi.org/10.1136/bmj.b605
Moons KG, Altman DG, Reitsma JB, Collins GS (2015) Transparent reporting of a multivariate prediction model for individual prognosis or development initiative. New guideline for the reporting of studies developing, validating, or updating a multivariable clinical prediction model: the TRIPOD statement. Adv Anat Pathol 22(5):303–305. https://doi.org/10.1097/PAP.0000000000000072
Alfieri S, Amid PK, Campanelli G et al (2011) International guidelines for prevention and management of post-operative chronic pain following inguinal hernia surgery. Hernia 15:239–249. https://doi.org/10.1007/s10029-011-0798-9
Hjøllund NH, Larsen FB, Andersen JH (2007) Register-based follow-up of social benefits and other transfer payments: accuracy and degree of completeness in a Danish interdepartmental administrative database compared with a population-based survey. Scand J Public Health 35:497–502
Rubak TS, Svendsen SW, Andersen JH et al (2014) An expert-based job exposure matrix for large scale epidemiologic studies of primary hip and knee osteoarthritis: the Lower Body JEM. BMC MusculoskeletDisord 15:204
Grillner S, Nilsson J, Thorstensson A (1978) Intra-abdominal pressure changes during natural movements in man. ActaPhysiolScand 103:275–283. https://doi.org/10.1111/j.1748-1716.1978.tb06215.x
Hollmann S, Klimmer F, Schmidt KH, Kylian H (1999) Validation of a questionnaire for assessing physical work load. Scand J Work Environ Health 25:105–114
Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B (1998) The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol 3:322–355
Friis-Andersen H, Bisgaard T (2016) The Danish Inguinal Hernia database. ClinEpidemiol 8:521–524
Köckerling F, Simons MP (2018) Current concepts of inguinal hernia repair. Visc Med 34:145–150. https://doi.org/10.1159/000487278
Tasmuth T, Estlanderb AM, Kalso E (1996) Effect of present pain and mood on the memory of past postoperative pain in women treated surgically for breast cancer. Pain 68:343–347
Hosmer DW, Lemeshow S (1995) Confidence interval estimates of an index of quality performance based on logistic regression models. Stat Med 14:2161–2172
Nattino G, Finazzi S, Bertolini G (2016) A new test and graphical tool to assess the goodness of fit of logistic regression models. Stat Med 35:709–720. https://doi.org/10.1002/sim.6744
Nattino G, Finazzi S, Bertolini G (2014) A new calibration test and a reappraisal of the calibration belt for the assessment of prediction models based on dichotomous outcomes. Stat Med 33:2390–2407. https://doi.org/10.1002/sim.6100
Hosmer DW, Lemeshow S, Sturdivant RX (2013) Applied logistic regression, 3rd edn. Wiley, Hoboken
Harrell FE Jr, Lee KL, Mark DB (1996) Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 15:361–387. https://doi.org/10.1002/(SICI)1097-0258(19960229)15:43.0.CO;2-4
Steyerberg EW, Harrell FE Jr, Borsboom GJ, Eijkemans MJ, Vergouwe Y, Habbema JD (2001) Internal validation of predictive models: efficiency of some procedures for logistic regression analysis. J ClinEpidemiol 54:774–781
Nikkolo C, Lepner U, Murruste M, Vaasna T, Seepter H, Tikk T (2010) Randomised clinical trial comparing lightweight mesh with heavyweight mesh for inguinal hernioplasty. Hernia 14:253–258
VanDenKerkhof EG, Peters ML, Bruce J (2013) Chronic pain after surgery: time for standardization? A framework to establish core risk factor and outcome domains for epidemiological studies. Clin J Pain 29:2–8. https://doi.org/10.1097/AJP.0b013e31824730c2
Rubak TS, Svendsen SW, Søballe K, Frost P (2014) Total hip replacement due to primary osteoarthritis in relation to cumulative occupational exposures and lifestyle factors: a nationwide nested case-control study. Arthritis Care Res (Hoboken ) 66:1496–1505
Tabatabaeifar S, Frost P, Andersen JH, Jensen LD, Thomsen JF, Svendsen SW (2015) Varicose veins in the lower extremities in relation to occupational mechanical exposures: a longitudinal study. Occup Environ Med 72:330–337
Vad MV, Frost P, Rosenberg J, Andersen JH, Svendsen SW (2017) Inguinal hernia repair among men in relation to occupational mechanical exposures and lifestyle factors: a longitudinal study. Occup Environ Med 74:769–775
Vad MV, Frost P, Bay-Nielsen M, Svendsen SW (2012) Impact of occupational mechanical exposures on risk of lateral and medial inguinal hernia requiring surgical repair. Occup Environ Med 69:802–809
Vad MV, Frost P, Svendsen SW (2015) Occupational mechanical exposures and reoperation after first-time inguinal hernia repair: a prognosis study in a male cohort. Hernia 19:893–900
Sommer TG, Svendsen SW, Frost P (2016) Sickness absence and permanent work disability in relation to upper- and lower-body pain and occupational mechanical and psychosocial exposures. Scand J Work Environ Health 42:481–489. https://doi.org/10.5271/sjweh.3600
Svendsen SW, Frost P, Vad MV, Andersen JH (2013) Risk and prognosis of inguinal hernia in relation to occupational mechanical exposures-a systematic review of the epidemiologic evidence. Scand J Work Environ Health 39:5–26
Lundström KJ, Holmberg H, Montgomery A, Nordin P (2018) Patient-reported rates of chronic pain and recurrence after groin hernia repair. Br J Surg 105:106–112. https://doi.org/10.1002/bjs.10652
Niebuhr H, Wegner F, Hukauf M et al (2018) What are the influencing factors for chronic pain following TAPP inguinal hernia repair: an analysis of 20,004 patients from the Herniamed Registry. SurgEndosc 32:1971–1983. https://doi.org/10.1007/s00464-017-5893-2
Kehlet H, Bay-Nielsen M (2008) Nationwide quality improvement of groin hernia repair from the Danish Hernia Database of 87,840 patients from 1998 to 2005. Hernia 12:1–7
Köckerling F, Bittner R, Kraft B, Hukauf M, Kuthe A, Schug-Pass C (2017) Does surgeon volume matter in the outcome of endoscopic inguinal hernia repair? SurgEndosc 31:573–585. https://doi.org/10.1007/s00464-016-5001-z
The Danish Hernia database, annual reports https://www.herniedatabasen.dk/kopi-af-arsrapporter. In: https://www.herniedatabasen.dk/kopi-af-arsrapporter. Accessed 24 Apr 2018
Funding
The study was funded by the Danish Working Environment Research Fund (Grant number 20130023392/5).
Author information
Authors and Affiliations
Contributions
All authors took part in conceiving and designing the work. MV collected the data. MV, GN, and SL conducted the analysis. MV wrote the first draft of the paper in close collaboration with SWS. All authors revised the paper critically for important intellectual content and approved the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
The Danish Data Protection Agency approved the study (j.no.: 1-16-02-121-15).
Human and animals rights
All procedures for the human study were performed according to ethical standards defined by the health research ethics committee. In Denmark, register and questionnaire studies do not require approval by health research ethics committees (request no. 1-10-72-22-15).
Informed consent
Informed consent was obtained for this study according to the Danish health research ethics committees guidelines.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vad, M.V., Svendsen, S.W., Frost, P. et al. Inguinal hernia repair among men: development and validation of a preoperative risk score for persistent postoperative pain. Hernia 26, 177–187 (2022). https://doi.org/10.1007/s10029-021-02376-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-021-02376-x