Abstract
Background
Extramedullary anterior cervical canal tumors can be challenging lesions to reach. The posterolateral trans dentate approach offers an alternative route.
Method
Classic posterior laminoplasty is done to expose the medulla; the dentate ligament is identified as a fibrous structure running from the lateral pial surface of the medulla to the lateral dura between nerve roots spaces. Once the ligament is cut, the medulla can be gently rotated to access the anterior cervical canal. Intraoperative neurophysiological stimulation is mandatory.
Conclusion
This approach allows a safe route, without the need for corpectomies. It should be considered especially in children where multilevel corpectomies could be challenging.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Relevant surgical anatomy
First described by Johann Jacob Huber in 1739, the dentate ligament is a single fibrous strip running bilaterally on the pial surface of the medulla between dorsal and ventral nerve roots, from the craniovertebral junction to T12. Additional triangular extensions attach laterally to the dura mater superiorly to the intervertebral foramen. The ligament divides the spinal canal into an anterior and posterior compartment. At the cervical level, these bands could be single or double, and they are shorter and stronger than those in the thoracic level [5].
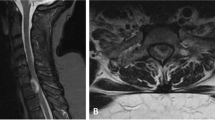
Cervical nerve roots form up of a dorsal and a ventral root, each of them spreading in a fan-like way while entering the medulla. Dorsal and ventral roots converge at the exit of the dural sac, leaving a subarachnoid space between them easily invadable by the tumor [7] (Figs. 1, 2 and 3).
Description of the technique
The patient is placed prone; the head is fixed with a pediatrics skull clamp and over a silicon headrest. Slight neck flexion is used to increase exposure.
Posterior cervical midline approach is done throughout the avascular nuchal ligament until the identification of spinous process, skeletonization of spinous process, laminas, and facet joints is done bilaterally. Laminoplasty, one level above to one level below, is done with a high-speed drill at the vertebral levels involved by the tumor. Midline durotomy with additional lateral cuts at its edges is done for adequate visualization of the lateral part of the medulla, nerve roots, and intracanal lateral dura.
In our case, fluorescein was used to track aberrant patterns of tumoral vessels during the dissection. But no clear aberrant pattern was observed.
The dentate ligament is identified as a whitish longitudinal fiber along the lateral surface of the medulla, between dorsal and ventral nerve roots. Additionally, lateral triangular extensions attach the ligament to the dura mater. These attachments end up in the dura just superiorly to the intervertebral foramina. Section of the longitudinal part at the level of the pial surface and detachment of the transverse part at the dural anchorage is done to release the medulla. Once cut, the medulla can be gently rotated to the contralateral side using a 6.0 polypropylene suture anchorage to the dentate ligament and pia mater. Extreme caution is taken while doing this maneuver under neurophysiological monitoring. Medulla rotation allows further exposure of the anterior canal between the nerve roots. The pial dissection plane is used to achieve complete tumor resection.
Once resected, the pial suture is cut for the medulla to return to its normal position. Dura is closed, and laminoplasty is repositioned with mini plates. If more than 3 level laminoplasty is done, posterior lateral mass screw fixation should be considered.
Indications
Indications for this approach are anterior cervical intradural extramedullary tumors, such as schwannomas, meningiomas, or other dura depending tumors [2, 4], especially in children, where anterior corpectomy can create instability challenging to repair.
This approach can be used in cervical and dorsal anterior locations. On this location, one or more dorsal nerve roots could be cut additionally for better exposure.
Limitations
This approach does not give adequate control of the anterior medullary surface; thus way, it should not be used if anterior medullary pial infiltration is suspected [4].
Very tough tumors, such as calcified meningiomas, should not be tackled through this approach because of the inability for good debulking. Limited between roots space to extract the tumor is another limitation, especially if debulking or fraction of the tumor is not possible.
Exposure is also limited by the degree of medullary rotation tolerable in each patient.
In our practice, the trans dentate approach is done only through one side. Medullary rotation on both sides for bilateral approach is not described in the literature and we do not recommend it.
How to avoid complications
To avoid complications, intraoperative electrophysiological monitoring is mandatory, somatosensory evoked potentials, transcranial motor evoked potentials, and free-running electromyography must be monitored. Especial attention must be given to these parameters when rotating the medulla with the pial suture. Excessive prolonged rotation and traction can lead to permanent medullary damage if not check with the neurophysiology team.
In addition to detaching the dentate ligament from the dura mater, the ligament must be also cut along the lateral edges of the medulla. This maneuver allows a better medullary rotation with less tension.
To create an adequate medullary exposure and minimize complications, laminoplasty must reach the start of the facet joints laterally, and midline durotomy should be expanded with lateral cuts at its edges.
Cerebrospinal fluid (CSF) leak should be bear in mind, especially if long durotomy is needed. To minimize the risk, watertight dural closure must be achieved, if not, lumbar drainage should be considered. Either way, bed rest is mandatory.
Facet joints and nerve roots must be respected in the cervical spine to avoid instability and disabling upper extremity weakness. Cervical lateral mass screw fixation should be considered if 3 or more levels of laminoplasty are planned, to avoid postoperative cervical kyphosis [1, 3].
Microsurgical technique must be mastered not to inadvertently manipulate the spinal cord.
Specific perioperative considerations
Bed rest for at least 5 to 7 days is advisable to avoid postoperative CSF wound leak. Lumbar drainage is usually not needed if adequate dural closure is done. Daily wound observation is needed to spot any CSF leak.
Specific information for the patient
The major issue to discuss with the patient is the possibility of permanent or transitory medullary damage, as well as incomplete resection and CSF leak. Furthermore, the patient must be aware of possible chronic cervical pain. The risk of kyphosis if fixation is not complemented in long laminoplasties should also be mentioned.
A cervical collar is not mandatory [6], but we recommended it in highly active children to avoid excessive mechanical demand during recovery.
References
Deutsch H, Haid RW, Rodts GE, Mummaneni PV (2003) Postlaminectomy cervical deformity. Neurosurg Focus 15(3):E5. https://doi.org/10.3171/foc.2003.15.3.5
Joaquim AF, Almeida JP, Dos Santos MJ, Ghizoni E, de Oliveira E, Tedeschi H (2012) Surgical management of intradural extramedullary tumors located anteriorly to the spinal cord. J Clin Neurosci 19(8):1150–1153. https://doi.org/10.1016/j.jocn.2011.08.044
Kim BS, Dhillon RS (2019) Cervical laminectomy with or without lateral mass instrumentation: a comparison of outcomes. Clin Spine Surg 32(6):226–232. https://doi.org/10.1097/BSD.0000000000000852
Kim CH, Chung CK (2011) Surgical outcome of a posterior approach for large ventral intradural extramedullary spinal cord tumors. Spine (Phila Pa 1976) 36(8):E531-7. https://doi.org/10.1097/BRS.0b013e3181dc8426
Rengachary SS, Pelle D, Guthikonda M (2008) Contributions of Johann jacob Huber to the surface anatomy of the spinal cord and meninges. Neurosurgery 62(6):1370–3. https://doi.org/10.1227/01.neu.0000333310.87554.d5 (discussion 1373-4)
Sakai Y, Ito K, Ito S, Imagama S, Ishiguro N, Harada A (2017) Collar fixation is not mandatory after cervical laminoplasty: a randomized controlled trial. Spine (Phila Pa 1976) 42(5):E253–E259. https://doi.org/10.1097/BRS.0000000000001994
Vital J-M, Cawley DT (2020) Spinal anatomy modern concepts. Springer, Berlin (ISBN 9783030209278)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
For the purpose of this video, no ethics committee approval was needed. Relatives give full consent for any scientific purposes involving the case. The consent includes an image or video recording.
Additional information
Publisher's note
S pringer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
1. Anterior and anterolateral cervical canal extramedullary lesions can be tackled through a posterior trans dentate approach.
2. Intramedullary lesions or tumors invading the anterior medullar pia mater should not be managed throughout this approach.
3. Laminoplasty, one level above and one level below must be done for adequate control and visualization.
4. Midline durotomy needs to be complemented with lateral cuts at its edges.
5. Dentate ligament is easily identified along the side of the medulla as a white cord structure with triangular dural attachments.
6. After the dentate ligament is cut, medullary rotation can be done safely with dentate or pial sutures gently traction.
7. Intraoperative electrophysiological monitoring is mandatory.
8. Meticulous microsurgical technique is needed for inter nerve root dissection.
9. If multilevel laminoplasty is needed, posterior lateral mass screw fixation should be considered to avoid postoperative kyphosis.
10. Close wound follow-up is needed to spot CSF leak or pseudomeningocele.
This article is part of the Topical Collection on Pediatric Spine
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 195483 KB)
Rights and permissions
About this article
Cite this article
Santos, C., Rivero-Garvía, M. & Marquez-Rivas, J. Posterolateral trans dentate approach to anterior extensive extramedullary tumor of the cervical spine in a pediatric case: how I do it. Acta Neurochir 164, 1153–1156 (2022). https://doi.org/10.1007/s00701-021-04988-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-021-04988-9