Abstract
Background
Posterior fossa arteriovenous malformations (pfAVMs) can be challenging lesions to manage. AVMs in this location may have distinct features compared with supratentorial AVMs. Our aim was to systematically review the literature on the presenting characteristics of pfAVMs and compare clinical and angiographic outcomes after the various types of treatment employed.
Methods
The review was conducted according to the Cochrane Collaboration guidelines. Electronic databases from 1900 to March 2018 were searched and complemented by hand-searching and cross-referencing. Articles were categorized into (i) AVM studies that included those in the posterior fossa, (ii) those that focused exclusively on pfAVM, and (iii) those that further specified a cerebellar or brainstem location of the AVM.
Results
Seventy-seven articles with 4512 pfAVM patients were retained for analyses. Compared with historical supratentorial controls, pfAVMs were reported to more frequently present with rupture, to more commonly have associated arterial aneurysms, and to more frequently lead to poor clinical and angiographic outcomes. The quality of the literature and lack of standardization of outcome reporting precluded performing a meta-analysis on the results of the various different treatment modalities.
Conclusions
Posterior fossa AVMs may have some distinct features compared with supratentorial AVMs. The available reports on pfAVMs are not sufficiently standardized to provide reliable guidance for patient management decisions. This goal will require future studies to be multicentric and to focus on standardized, repeatable clinical and angiographic outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Posterior fossa arteriovenous malformations (pfAVMs) are uncommon lesions which remain a challenging clinical problem for treating physicians [2, 5, 12]. Posterior fossa AVMs have been suggested to differ from supratentorial AVMs in more than location: pfAVM patients have been reported to present more frequently with hemorrhage [1, 13, 21], which is poorly tolerated in the smaller confines of the posterior fossa, and can lead to coma or severe neurological compromise. The best way to manage many pfAVM patients remains controversial [7, 16]. Our aim was to systematically review and evaluate the literature on pfAVMs, to focus on the features that are different from supratentorial AVMs, and to summarize the literature to date regarding angiographic and clinical outcomes following management with the various treatment modalities available to clinicians.
Methods
The systematic review was performed according to guidelines on searching strategies published in the Cochrane Handbook for systematic reviews of intervention [4], in the proposal for reporting meta-analysis of observational studies in epidemiology [10], and in the PRISMA statement [20].
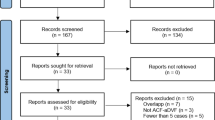
We first identified five prototype pfAVM articles in PubMed (MEDLINE) (EM). We collected the specific medical subject heading (MeSH) and key words linked to these articles to start the search strategy (EM, DZ). The final search strategy was performed in March 2018 on the following databases: PubMed (from 1900 onward), MEDLINE (OVID, from 1946 onward), EMBASE (OVID, from 1974 onward), EMB Reviews (OVID, from 1991 onward), and CINAHL Complete (EBSCO, from 1937 onward). We used terms from controlled vocabularies (MeSH for MEDLINE, EMTREE for EMBASE, and CINAHL Headings for CINAHL) and words and expressions from “all fields” for EMB Reviews and from “title,” “abstract,” and “author’s key words” in MEDLINE, EMBASE, and CINAHL. We used two conceptual groups for the search strategy: (1) posterior cranial fossa and (2) arteriovenous malformation (AVM). The flow chart is presented in Fig. 1, and the detailed search strategy is available in Appendix 1.
A first round of screening (title and abstracts) of all records was performed, and the article excluded if it did not pertain to brain AVMs. Articles were excluded if they dealt exclusively with supratentorial cerebral AVMs without results regarding pfAVMs. Case reports were also excluded. A second round of screening (full text) excluded review articles and basic science report. Articles were retained for analysis if they (1) included 10 or more AVM patients; (2) had a minimum specification of the AVM location as infratentorial; and (3) included explicit angio-architectural, clinical, or angiographic outcome data. Case series with data on both supra- and infratentorial AVMs that did not explicitly detail outcomes for each location independently were excluded. Retained articles were then divided according to the degree of precision regarding the AVM location: (1) pfAVM location only specified as “infratentorial” or (2) pfAVM location specified as “brainstem” or “cerebellar.” All analyses were conducted using R.3.2.2 (R foundations for statistical computing).
Results
The literature search yielded a total of 4643 records (Fig. 1). After eliminating duplicates, 2614 records were screened (title and abstract). The reasons for initial exclusions were the following: article did not include brain AVMs (1728 articles), and article did not include posterior fossa AVMs (287 articles) or case reports (373 articles). This yielded 226 articles for full text analysis. Subsequent exclusions were because article included ≤ 10 patients (48 articles), article without usable outcome data (95 articles), reviews (5 articles), and basic science reports (1 article). The yield for the final analysis was 77 articles.
The 77 retained articles included 4512 pfAVMs. There were 17 reports that combined supratentorial and pfAVMs with data stratified according to location and 60 reports that focused exclusively on pfAVMs. Mode of presentation and angio-architecture of pfAVMs was the subject of 31 articles, while 46 reported the management of patients with pfAVMs (Table 1A and B online). Information regarding the proportion of AVMs located in the posterior fossa was available in 38 articles: 2166/17,115 AVMs or 12.7% (95% CI 12.1–13.2%) (Table 1). More precise information regarding cerebellum versus brainstem location was available in 20 articles with 838/9277 (9%, 95% CI 8.5–9.6%) and 22 articles with 609/14,158 (4.3%, 95% CI 4.0–4.7%), respectively.
Mode of presentation and angio-architecture
Results are summarized in Table 2, with details in Table 1A (online). All 31 articles on presentation and angio-architecture (17 combined supratentorial and pfAVM and 14 focused on pfAVM alone) were retrospective single-center studies. The most commonly reported conclusions were that location in the posterior fossa, compared with supratentorial, was considered to (1) be a risk factor for hemorrhagic presentation (10 articles), (2) more likely harbor associated aneurysms (10 articles), and (3) have a lower likelihood of presenting with seizure (3 articles).
Information regarding the proportion of patients presenting with hemorrhage was available in 45 articles: 1849/2463 pfAVMs (75%, 95% CI 73.3–76.7%) were found after rupture. Information on associated aneurysms was available in 30 articles and were found in 500/1976 (25.3%, 95% CI 23.4–27.2%) cases. There were 31 articles that provided information regarding re-rupture rates of hemorrhagic pfAVMs in 1981 patients, yielding a re-rupture rate of 274/1981 (13.8%, 95% CI 12.4–15.4%).
Patient management and outcome
The 46 reports on patient management included 2 multicenter and 44 single-center studies. All were retrospective. Fourteen studies described the results of surgery, and 5 were on the results of endovascular treatment, 18 on the results of radiosurgery, and 9 detailed outcomes following multimodality treatment (details can be found in Table 2 online).
AVM description
At least one published angiographic grading scale was used to describe the pfAVM in 36/46 (78%) articles (Table 1B online). Multiple (2 or more) grading systems were used in 14/46 (30%) articles. The Spetzler-Martin score [17] was most commonly used (34 articles), followed by the radiosurgery-based AVM score (RBAS) [15] for 11/18 of the radiosurgery reports, with various other grading schemes [9, 19] or 3-tier grading system [18] used in 7 further articles. Only a small proportion of articles 14/46 (30%), 10 of which were radiosurgery reports, used more than one grading scale to score the same pfAVMs to facilitate comparison of outcomes.
Clinical status
Prior to treatment, clinical scores were used to grade patients in 27/46 (59%) articles, most commonly the modified Rankin scale (mRS) (15 articles), followed by the Glasgow coma score (GCS) (7), the Karnofsky score (2), and the World Federation of Neurological Surgeons (WFNS), Hunt-Hess, and Botterell score (1 article each) (Table 1B online).
Clinical outcomes after treatment were provided in 26/46 (57%) reports, most commonly the mRS (19 articles), the Glasgow outcome score (GOS) (6 articles), Karnofsky (3), and Botterell score (1). Three articles used more than one grading scale to score clinical outcomes.
Overall angiographic and clinical outcome
Angiographic and clinical outcomes are presented in Table 3. Overall, the rate of angiographic obliteration for pfAVMs was 1759/2444 (72%, 95% CI 70.2–73.7%), based on the 44/46 articles with data. This rate was based on catheter angiographic results for all of the surgical and endovascular reports, 2/17 radiosurgical articles, and 8/9 multimodality articles. A combination of catheter angiography and MRI was used to determine the AVM obliteration rates in 15/17 radiosurgical reports and 1/9 multimodality articles.
The rate of disability (considered mRS > 2, GOS < 4, Karnofsky < 70, or Botterell scale “severe” (grade IV and V)) after treatment was 189/1062 (17.8%, 95% CI15.6–20.2%), from 24/46 articles with data. The overall rate of mortality for patients with a ruptured pfAVM was 131/1592 (8.2%, 95% CI 7.0–9.7%) from the 35 articles that included this data. From the available reports, it was not possible to distinguish or extract the morbidity and mortality due to treatment from morbidity or mortality due to the disease.
Reported outcomes based on AVM location
“Infratentorial” versus more precisely specified “brainstem” or “cerebellar” location
When AVMs of the posterior fossa were only specified as “infratentorial” (19 articles), the rates of angiographic obliteration ranged from 83 to 100% for surgery (6 articles with usable angiographic outcome data), 47–72% for endovascular management (2 articles with data), 75% for radiosurgery (1 article), and 48–92% obliteration rates for multimodal management (7 articles). The rate of mortality was 58/590 (9.8%, 95% CI 7.7–12.5%) (15/19 articles with data), and the rate of disability was 102/516 (19.9%, 95% CI 16.7–23.6%) (12/19 articles with data).
A more precise location within the posterior fossa was specified in 27 articles (17 brainstem and 10 cerebellar). Angiographic obliteration rates for brainstem AVMs treated with surgery were 90% (3 articles with usable angiographic data), endovascular 46% (1 article), radiosurgery 38–73% (11 articles), and 45–65% for multimodal management (2 articles). The mortality rate for patients with a brainstem AVM was 38/556 (6.8%, 95% CI 5.0–9.2%) (13/17 articles with data), and the incidence of disability was 46/179 (25.7%, 95% CI 19.9–32.6%) (7/17 articles with data).
Angiographic obliteration rates for cerebellar AVMs following surgery were 98–100% (5 articles with usable angiographic data), endovascular 72% (1 article), and radiosurgery 63–77% (4 articles). There were no articles focusing on the multimodal management of cerebellar AVMs. The mortality rate for patients with a cerebellar AVM was 35/446 (7.9%, 95% CI 5.7–10.7%) (7/10 articles with data), and the incidence of disability was 41/367 (11.2%, 95% CI 8.3–14.8%) (5/10 articles with data).
Discussion
There is abundant literature on AVMs of the posterior fossa, but the information that can be extracted to inform clinical decisions remains limited. The proportion of AVMs found in this location (12.9%) is approximately the proportion of brain tissue found in this compartment (~ 1/8 the volume or 12.5%). Posterior fossa AVM patients were reported to less frequently present with seizures, to more frequently present with rupture, to more frequently harbor associated aneurysms, and to more frequently re-rupture. These features have incited some authors to suggest they should be managed more aggressively than supratentorial AVMs. However, the reported increase in rupture rate may well be a presentation bias, cerebellar tissue not being epileptogenic, and pfAVMs mostly remaining undetected until they bleed [16]. Even if it were true that pfAVMs had a more ominous nature than their supratentorial counterpart, this between-patients comparison could not serve to justify preventive interventions. For that purpose, a valid comparison between conservative and interventional management is needed. The preventive treatment of unruptured AVMs remains controversial, even more so since the publication of ARUBA, but that trial included too small a number of pfAVMs to conclude for this location (n = 12).
This review was undertaken to summarize the knowledge available in our literature and gain a broad overview of outcomes following the various ways they can be managed, something that was difficult given the various clinical contexts and quality of reported data. In addition to the well-recognized problems of retrospective observational studies (referral bias, missing data, publication bias), one major problem with the pfAVM dataset was selection bias for each treatment modality and a lack of standardization of how the AVMs were described. The most commonly used description system was the Spetzler-Martin (SM) scale, reported to predict the clinical outcome following surgical management of mostly supratentorial AVMs [17]. Other classifications have been proposed but are less commonly used. The SM scale does not apply to endovascular or radiosurgical treatment approaches in terms of predicting outcome [17]. When different authors use different grading scales to describe AVMs particularly when they are from different specialties with different patient selection criteria, comparison of outcomes becomes difficult or impossible. A small proportion of articles (mostly by radiosurgical authors) used multiple grading scales to facilitate comparisons between studies.
There was also significant variability in how outcomes were defined, when they were recorded and the way they were scored: for example, radiosurgery papers were more likely to use MRI to assess long-term AVM obliteration, even though this modality has a higher false-negative rate than postoperative catheter angiography. Catheter angiography however is less likely to be conducted for long-term follow-up [14]. Scales to describe pre-treatment condition and clinical outcome at follow-up were not uniformly applied; when they were, a variety of scales were used. Some problems are related to the complex, multistage clinical histories of pfAVMs, including multiple clinical episodes and multimodality treatments. It is often unclear which part of the patient history is included in the report and at what stage of the history the data was captured.
Finally, there were problems due to the various ways authors chose to group patients or results. For example, 19 papers specified the numbers of brainstem and cerebellar AVMs, but did not provide stratified clinical or angiographic outcome data, rendering summaries unclear or ambiguous and comparisons difficult or impossible.
When authors chose to present angiographic results for brainstem separate from those for cerebellar locations, surgical management seemed to lead to greater rates of obliteration, but the clinical outcomes scales used in these papers were so variable that it remains difficult to understand the cost of obtaining an occluded AVM in terms of morbidity borne by the patient.
Many of the shortcomings of the current pfAVM literature could be addressed by standardizing definitions, classifications, methods of data collection, and scales. One solution would be to proceed with a large-scale multinational registry, one that would include reproducible clinical and angiographic outcome measures and standardized reporting. However, could such a registry really inform clinical decisions [3, 11]? Patients with pfAVMs that are judged favorable for surgical resection are clearly more likely to undergo surgery, while surgically inaccessible lesions will be managed by endovascular or radiosurgical means. Comparison of outcomes following such patient selection can hardly result in reliable conclusions. The use of propensity scores has been proposed to compensate for selection biases inevitably included in observational studies, but the validity of the method remains controversial [8]. For cases that are judged to potentially be manageable more than one way (including conservative management), a randomized multicenter comparative trial is ongoing [6]. The limitations of this work include those already mentioned regarding the various methods used in the source articles. The heterogeneity of definitions, groupings, scoring scales, selection bias, and the large amount of missing data did not permit a meta-analysis. For similar reasons, the construction of funnel plots to look for publication bias was judged impossible.
Conclusion
AVMs of the posterior fossa represent an appropriate proportion of brain AVMs when the volume of brain tissue in the posterior fossa is taken into account. Posterior fossa AVMs are more likely to be found after hemorrhage and are more likely to harbor associated aneurysms. Heterogeneity of reporting, including variability in the choice of grading scales, to describe both the AVMs and the patient clinical condition renders the literature incapable of providing reliable guidance for treatment decisions. Standardized methods of grading and reporting, in addition to randomized clinical trials, remain necessary to be able to provide guidance regarding the best management of these lesions.
Abbreviations
- AVM:
-
Arteriovenous malformation
- pfAVM:
-
Posterior fossa AVM
- RBAS:
-
Radiosurgery-based AVM score
- mRS:
-
Modified Rankin scale
References
Arnaout OM, Gross BA, Eddleman CS, Bendok BR, Getch CC, Batjer HH (2009) Posterior fossa arteriovenous malformations. Neurosurg Focus 26:E12. https://doi.org/10.3171/2009.2.FOCUS0914
Batjer H, Samson D (1986) Arteriovenous malformations of the posterior fossa: clinical presentation, diagnostic evaluation and surgical treatment. Neurosurg Rev 9:287–296. https://doi.org/10.1007/bf01743635
Cenzato M, Boccardi E, Beghi E, Vajkoczy P, Szikora I, Motti E, Regli L, Raabe A, Eliava S, Gruber A, Meling TR, Niemela M, Pasqualin A, Golanov A, Karlsson B, Kemeny A, Liscak R, Lippitz B, Radatz M, La Camera A, Chapot R, Islak C, Spelle L, Debernardi A, Agostoni E, Revay M, Morgan MK (2017) European consensus conference on unruptured brain AVMs treatment (supported by EANS, ESMINT, EGKS, and SINCH). Acta Neurochir 159:1059–1064. https://doi.org/10.1007/s00701-017-3154-8
Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. Available from www.cochrane-handbook.org. Accessed 16 Sept 2018
da Costa L, Thines L, Dehdashti AR, Wallace MC, Willinsky RA, Tymianski M, Schwartz ML, ter Brugge KG (2009) Management and clinical outcome of posterior fossa arteriovenous malformations: report on a single-centre 15-year experience. J Neurol Neurosurg Psychiatry 80:376–379. https://doi.org/10.1136/jnnp.2008.152710
Darsaut TE, Magro E, Gentric JC, Batista AL, Chaalala C, Roberge D, Bojanowski MW, Weill A, Roy D, Raymond J (2015) Treatment of brain AVMs (TOBAS), care trial and registry: study protocol for a randomized controlled trial. Trials 16:497. https://doi.org/10.1186/s13063-015-1019-0
Kelly ME, Guzman R, Sinclair J, Bell-Stephens TE, Bower R, Hamilton S, Marks MP, Do HM, Chang SD, Adler JR, Levy RP, Steinberg GK (2008) Multimodality treatment of posterior fossa arteriovenous malformations. J Neurosurg 108:1152–1161. https://doi.org/10.3171/JNS/2008/108/6/1152
King G, Nielsen R (2019) Why Propensity Scores Should Not Be Used for Matching 2019 [Available from: http://j.mp/2ovYGsW. Accessed 23 Nov 2017] https://doi.org/10.1017/pan.2019.11
Lawton MT, Kim H, McCulloch CE, Mikhak B, Young WL (2010) A supplementary grading scale for selecting patients with brain arteriovenous malformations for surgery. Neurosurg 66:702–713; discussion 13. https://doi.org/10.1227/01.NEU.0000367555.16733.E1
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62:e1–e34. https://doi.org/10.1136/bmj.b2700
Magro E, Gentric JC, Darsaut TE, Raymond J, Tobas investigators (2017) Unruptured brain AVMs: it’s time we worked together to integrate care and clinical research. Acta Neurochir 159:2099–2100. https://doi.org/10.1007/s00701-017-3278-x
Mpotsaris A, Loehr C, Harati A, Lohmann F, Puchner M, Weber W (2010) Interdisciplinary clinical management of high grade arteriovenous malformations and ruptured flow-related aneurysms in the posterior fossa. Interv Neuroradiol 16:400–408. https://doi.org/10.1177/159101991001600406
Perret G, Nishioka H (1966) Report on the cooperative study of intracranial aneurysms and subarachnoid hemorrhage. Section VI. Arteriovenous malformations. An analysis of 545 cases of cranio-cerebral arteriovenous malformations and fistulae reported to the cooperative study. J Neurosurg 25:467–490. https://doi.org/10.3171/jns.1966.25.4.0467
Pollock BE, Kondziolka D, Flickinger JC, Patel AK, Bissonette DJ, Lunsford LD (1996) Magnetic resonance imaging: an accurate method to evaluate arteriovenous malformations after stereotactic radiosurgery. J Neurosurg 85:1044–1049. https://doi.org/10.3171/jns.1996.85.6.1044
Pollock BE, Flickinger JC (2002) A proposed radiosurgery-based grading system for arteriovenous malformations. J Neurosurg 96(1):79–85. https://doi.org/10.3171/jns.2002.96.1.0079
Rodriguez-Hernandez A, Kim H, Pourmohamad T, Young WL, Lawton MT, University of California STAMPS (2012) Cerebellar arteriovenous malformations: anatomic subtypes, surgical results, and increased predictive accuracy of the supplementary grading system. Neurosurg 71:1111–1124. https://doi.org/10.1227/NEU.0b013e318271c081
Spetzler RF, Martin NA (1986) A proposed grading system for arteriovenous malformations. J Neurosurg 65:476–483. https://doi.org/10.3171/jns.1986.65.4.0476
Spetzler RF, Ponce FA (2011) A 3-tier classification of cerebral arteriovenous malformations. Clinical article. J Neurosurg 114:842–849. https://doi.org/10.3171/2010.8.JNS10663
Starke RM, Yen CP, Ding D, Sheehan JP (2013) A practical grading scale for predicting outcome after radiosurgery for arteriovenous malformations: analysis of 1012 treated patients. J Neurosurg 119:981–987. https://doi.org/10.3171/2013.5.JNS1311
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 283:2008–2012. https://doi.org/10.1001/jama.283.15.2008
Tong X, Wu J, Lin F, Cao Y, Zhao Y, Wang S, Zhao J (2016) Microsurgical outcome of cerebellar arteriovenous malformations: single-center experience. World Neurosurg 95:469–479. https://doi.org/10.1016/j.wneu.2016.08.059
Author information
Authors and Affiliations
Contributions
All the authors of this manuscript have given substantial contributions to the conception or design of the work, drafting the work and revising it critically for important intellectual content, and final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements) or nonfinancial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Vascular Neurosurgery - Arteriovenous malformation
Rights and permissions
About this article
Cite this article
Magro, E., Darsaut, T.E., Mezui, E.D.O. et al. Arteriovenous malformations of the posterior fossa: a systematic review. Acta Neurochir 162, 905–910 (2020). https://doi.org/10.1007/s00701-020-04260-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-020-04260-6