Abstract
Purpose
To evaluate differential surgical interventions for obstructive sleep apnea (OSA) patients with single-level retropalatal based on the preoperative topographical diagnosis using nasoendoscopy with Müller’s maneuver during supine position (MM-P).
Subjects and methods
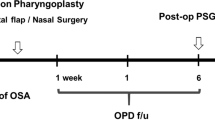
This case series included adult patients with OSA who showed a predominant single-level retropalatal collapse on MM-P. An anteroposterior pattern of collapse was managed by an anterior advancement procedure, while a transverse pattern of collapse was managed by lateral/anterolateral advancement procedures (double suspension sutures). A combined procedure was provided to the concentric type of collapse. All patients underwent evaluation of the polysomnography, Epworth Sleepiness Scale (ESS) values and snoring scores both preoperatively and 6–8 months after surgery.
Results
Among 102 patients, the most commonly reported pattern of collapse at the retropalatal level was the concentric pattern (48.04%) followed by the transverse pattern (27.45%). The AP-pattern of collapse was reported in 24.51%. In the postoperative follow-up visits, no early or late complications were reported. All included groups showed significant improvement in polysomnographic data (mean AHI and lowest O2 saturation level). Significant improvement of VAS of snoring was reported. The overall success rate was ˃90%.
Conclusion
Preoperative differential diagnosis of OSA with MM-P allows for tailored surgical management. Tailored procedures could yield good surgical outcomes when patients are properly selected and the technique is chosen according to preoperative topographical diagnostic assessment. This study might provide an available less-costly and effective preoperative planning for OSA intervention.
Level of evidence
4.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Sleep surgeons consider polysomnography (PSG) as the cornerstone diagnostic tool in patients with obstructive sleep apnea (OSA). PSG could detect the grade of severity of OSA. Moreover, it could be considered as the basic measure of postoperative outcome. However, PSG cannot provide a topographical mapping of the constriction sites of the upper airway (UA). The precise localization of the level and the pattern of UA collapse have a direct impact on the proper surgical planning of the OSA patient [1,2,3,4].
Many tools for topographical delineation of the UA are available. They include various types of radiological (CT, cephalometry and MRI) and endoscopic (drug-induced sleep endoscopy (DISE) and awake endoscopy with Müller’s maneuver (MM)). Each procedure has its limitations; no single procedure has gained universal agreement among sleep centers so far. Classically, various diagnostic tools are requested during preoperative topographical diagnostic work-up; however, economics should be considered when making recommendations of an individual tool [1, 5,6,7,8,9,10,11,12,13,14,15]. Eventually, surgical concerns about the existence of real surgical needs for these high costs and time-consuming tools might show up. More clearly, is there a single maneuver that could provide sufficient data for a right surgical decision? This is the question that needs to be answered.
The authors hypothesize that positional awake endoscopy with Müller’s maneuver (endoscopic examination of the UA while the patient in supine position; MM-P) might be a suitable single-session tool for preoperative UA evaluation and could be applied solely. MM-P could localize the sites and patterns of UA obstruction in OSA patients and could provide a three-dimensional anatomical topography of the collapsible area comparable to DISE; thus, it might support proper surgical planning and decisions. MM-P is a reliable radiation-free tool in the diagnostic protocol of OSA patients; it has other advantages as being an outpatient drug-free procedure and less costly than DISE. Moreover, MM-P could be easily employed for postoperative follow-up of OSA patients [1].
The aim of the current work was to evaluate the surgical outcomes after differential therapeutic surgical interventions for selected patients with OSA. Procedure selection was based solely on the preoperative topographical diagnosis using MM-P [1]. An anteroposterior pattern of collapse was managed by an anterior advancement procedure (modified anterior palatoplasty; MAP), while a transverse pattern of collapse was managed by lateral/anterolateral advancement procedures (double suspension sutures; DSS). A combined procedure was provided to the concentric type of collapse. This protocol might help individualized selection of appropriate surgical technique for patients with OSA, for whom the best maneuver is yet to come.
Patients and methods
Patients
This prospective study was conducted on adult patients with OSA who were managed at the ORL-HN Surgery Department, Zagazig University Hospitals, from January 2016 to February 2020. This study was conducted according to the declaration of Helsinki on Biomedical Research Involving Human Subjects. The institutional review board (Zag-IRB) approved the research methodology. A prior written informative consent was gained from all included patients. Included subjects were not exposed to any harm. Participants had the right to withdraw from the study at any time. All patients’ data were kept confidential.
This study was conducted on adult patients with OSA who had apnea hypopnea index (AHI) > 15 (on full-night, attended PSG) and body mass index (BMI) ≤ 35 kg/m2. All included patients were CPAP-intolerants and thus were candidates for sleep surgery. All patients reported a predominant single-level retropalatal collapse on MM-P and have tonsillar size of grades 1–2. Exclusion criteria included patients with multilevel collapse of UA. Patients with history of surgical intervention for snoring/OSA (e.g., UPPP), and patients who had previous tonsillectomy, adenoidectomy or nasal surgeries were excluded. Also, patients with high grades of tonsillar hypertrophy (grades 3–4) were excluded. Patients who missed follow-up scheduled visits were excluded.
Methods
All participants of the study had a detailed history taking, general and otorhinolaryngological examinations. Then, subjective Epworth Sleepiness Scale (ESS) analysis was done. Oral examination included assessment of dentition, soft palate (and uvula), tonsil size with estimation of palate/tongue relation and tongue base size. Friedman anatomical staging (FAS) was applied [9,10,11].
Thereafter, flexible nasoendoscope (FN) (Xion 3.2 mm diameter; Xion Medical, Berlin; Germany) was used for UA examination. The computerized tower included a camera and a light source (Xion medicals); the software enabled video recording and saving of the recorded material. During MM-P (patient in supine position), a FN was passed through the nose toward the nasopharynx. Müller's maneuver was performed after patients have been taught how to practice [1].
For MM-P recording, NOHL classification was applied to assess the sites and degrees of obstructions. This scale localizes the primary structures that contribute to the collapse of the UA. The possible patterns of collapse can be: lateral; L, anteroposterior (AP) or concentric (C) [16]. For grading during MM-P, collapse at a specific area was considered if it was more than 50% (grade 3, 4); a collapse less than 50% was considered non-collapse. Data of MM-P were evaluated by three independent examiners (with at least two agreements). During assessment, the examiners were blinded with the patient's identity. They were also blinded with other individual patient’s data.
Surgical interventions
According to preoperative data (as regards the pattern of collapse at the retropalatal area), included subjects were distributed into 3 groups: Group A) AP-collapse was managed by a palatal anterior advancement procedure (modified anterior palatoplasty; MAP), group B) L-collapse was managed by lateral/anterolateral advancement procedures (double suspension sutures; DSS) and group C) C-collapse for whom a combined procedure (MAP plus DSS) was provided. The MAP was performed via removal of a horizontal trapezoid strip of mucosa and then three sutures were passed in soft palate to include mucosa, submucosa and muscles in a multi-station, multilayer fashion. The end result of the procedure was anterior advancement of the soft palate. The DSS technique was performed via two absorbable sutures between the palate-pharyngeal myomucosal folds (posterior tonsillar pillars) and the ipsilateral pterygo-mandibular raphe. The procedure aimed to advance the soft palate in an anterolateral direction (Fig. 1) [8, 17].
Diagrammatic illustration of the surgical procedures showed the sutures (blue lines) of the anterior palatoplasty (red trapezoid) in the soft palate and the double suspension sutures (DSS); one (blue lines) around the pterygo-mandibular raphe (P). Blue lines represent the track of suturing. HP hard palate, PP posterior tonsillar pillar
The operative time was defined as the time for completion of the individual procedure whether MAP, DSS or combined (the time of tonsillectomy was not counted). All surgeries were performed by the senior author (SM Askar).
Postoperative follow-up
Six to eight months after surgery, patients underwent MM-P. All patients completed the postoperative protocol with subjective outcome measures (Epworth Sleepiness Scale (ESS) values, snoring scores and postoperative pain (Visual Analogue Scale—VAS values) and objective outcomes (PSG data).
The outcome of surgery was reported as successful in patients with a postoperative AHI < 10. Patients with AHI between 10 and 20 were reported as responders, while patients with a postoperative AHI > 20 (or an unchanged or increased AHI) were reported as non-responders [18,19,20,21,22,23].
Patient satisfaction was also evaluated on the basis of a 0–10 Visual Analogue Scale (VAS satisfaction: 0 = no patient satisfaction and 10 = maximum patient satisfaction). Patients’ partners also completed the snoring VAS by 6–8 months postoperatively.
Statistical analysis
The data were collected, tabulated and analyzed using SPSS statistical package Version 20 for windows (SPSS Inc., Chicago, Illinois; USA). Numerical data were presented with mean and standard deviation. 95% confidence interval (CI) was used. Ordinal data were presented as number and percentage. Paired T test was used to compare 2 variables. P value was considered statistically significant if < 0.05.
Results
Patient characteristics
Surgically eligible patients to this study were 235; 13 patients refused to share in the study, 116 patients had exclusion criteria (multilevel obstruction (104), previous UPPP (6), tonsillectomy and nasal surgeries (4) and those with tonsillar hypertrophy of grades 3–4 (2)) and were excluded. Four patients did not complete the follow-up scheduled visits. The current study was conducted on 102 adult OSA patients (with snoring and other OSA symptoms) who met the selection criteria and completed the follow-up schedules (Fig. 2). The included group was 59 males (57.84%), 43 females (42.16%) and had a mean age of 33.12 ± 9.14 years (range = 20–53 years). Their BMI ranged from 28.14 to 34.61 (mean = 33.12 ± 9.14). They had AHI range from 16.5 to 28.2 (on full-night PSG).
All included subjects showed a predominant single-level UA collapse at the retropalatal level only and reported high grades of collapse by NOHL scale (grade 4; 75–100%). On FAS (with exclusion of tonsil sizes 3–4), 79 patients (77.45%) were nominated as stage II and 23 patients (22.55%) were stage III.
The most commonly reported pattern of collapse was the C-pattern (49 patients; 48.04%) followed by the L-pattern (28 patients; 27.45%). The AP-pattern of collapse was reported in 25 patients (24.51%). Inter-observer full agreement (between three observers) of MM-P was reported in 93 patients (91.18%), while was not reported in 9 patients (8.82%), for whom the operative decision was based on two agreements.
According to the preoperative MM-P, group A had modified anterior palatoplasty (MAP), group B had double suspension sutures (DSS), while group C (C-pattern) had both MAP and DSS (Fig. 1). All participants had simultaneous tonsillectomy. The follow-up period ranged from 8 to 21 months (mean 14.32 ± 5.25).
Outcome
The mean operative time of DSS was 12.2 ± 1.3 min (range 10–14.6), MAP was 13.5 ± 0.9 min (range 12–15.3), while it was 21.7 ± 3.5 min (range 17–28) for both techniques (group C). Recovery from anesthesia was event-less in all included patients with no reported postoperative complications. Patients were sent home in the following morning and came back for examination after 7–10 days. In all groups, the postoperative pain was adequately controlled by oral analgesics and was relieved within 8–14 days. In the postoperative follow-up visits, there were no early complications (hemorrhage and infection) or late complications (globus sensation, velopharyngeal dysfunction or palatal fistula). No BMI significant changes were recorded.
At 6–8 months postoperatively, PSG was done for all the included patients; none of them reported worsening of AHI. Postoperative improvement (the reduction of AHI from the baseline) range was 56.49–88.76% (mean = 79 ± 7.16%). The overall successful outcome was ˃90%. VAS of satisfaction was ˃8 at one month postoperatively and remained the same throughout follow-up (Table 1, Figs. 3, 4).
In group A (25 patients), successful outcome was reported in 22 patients (88.0%), while three patients (12.0%) were considered as responders. The mean AHI dropped significantly (P < 0.0001; t = 18.0239) from 20.7 ± 3.3 preoperatively to 6.2 ± 2.3 postoperatively (95% CI 12.882 to 16.118). The mean lowest oxygen saturation level increased significantly from 81.2 ± 4.58 to 91.6 ± 4.02 (t = 8.5330; P < 0.0001; 95% CI − 12.8506 to − 7.9494). Significant improvements were reported as regards ESS and VAS of snoring (P < 0.0001) (Figs. 3, 4).
In group B (28 patients), successful outcome was reported in 26 patients (92.86%), while 2 patients (7.14%) were responders. The mean AHI dropped significantly (P < 0.0001; t = 21.8433; 95% CI 14.350 to 17.250) from 22.3 ± 3.6 preoperatively to 6.5 ± 1.3 postoperatively. The mean lowest oxygen saturation level increased significantly from 80.2 ± 3.9 to 90.1 ± 2.9 (t = 10.7789; P < 0.0001; 95% CI − 11.741 to − 8.059). Both ESS and VAS of snoring were significantly improved (P < 0.0001) (Figs. 3, 4).
In group (C) (49 patients), successful outcome was reported in 45 patients (91.84%), while 4 patients (8.16%) were responders. The mean AHI dropped significantly (P < 0.0001; t = 25.2343; 95% CI 14.557 to 17.043) from 23.1 ± 3.6 preoperatively to 7.3 ± 2.5 postoperatively. The mean lowest oxygen saturation level increased significantly from 79.8 ± 4.36 to 93.25 ± 2.8 (t = 18.1699; P < 0.0001; 95% CI − 14.9194 to − 11.9806) (Fig. 4). Both ESS and Visual analogue score (VAS) of snoring were significantly improved (P < 0.0001) (Table 1, Figs. 3, 4). There was nonsignificant difference between groups as regards to success of surgery for AHI relief (X2 = 0.438; P = 0.8).
Discussion
Background, idea and purpose
The medical, social, neuropsychiatric and economic problems of OSA are well described in the literature; thus, treatment of OSA should be considered to protect the patient, the family and the community. Although continuous positive airway pressure (CPAP) is considered the standard treatment for OSA, the low patient's compliance is a definite obstacle. The cost of the device remains a major concern especially in developing countries with limited health resources. CPAP intolerance might necessitate the surgical option [3, 6,7,8, 17,18,19,20,21,22,23,24,25,26,27,28,29,30].
The definitive localization with detailed description of the collapsible area in the OSA patients (as regards pattern and grade) and dealing with it by the suitable surgical procedure represents a main challenge for proper management of the individual patient and might be considered the cornerstone for successful outcomes. Different tools are employed for the definition of the sites and characters of UA collapse; however, an ideal single universally accepted preoperative tool of assessment of cases of OSA is still lacking [1, 4,5,6,7,8, 13, 18,19,20,21,22,23,24,25].
In the recent years, DISE is being practiced by many sleep surgeons, with reports of changing surgical planning; however, these changes did not lead to significantly higher success rates and were associated with surgical failures [30,31,32]. Pang et al. 2020 in a multicenter, non-randomized study stated that DISE reported no significant clinical/statistical impact on the surgical outcomes and had not increased the overall success rates of surgical interventions. They also reported better postoperative results in the no-DISE group of patients compared to patients who had undergone DISE [33].
The authors of this work support the assumption that the differential therapeutic management, based on proper preoperative differential topographical diagnosis of the UA (site and pattern), might help sleep surgeon for better planning of the surgical intervention and for avoidance of unnecessary procedures. In addition, it could positively influence the overall success rate of the surgical intervention. Moreover, a cost-effective strategic plan (for both pre- and postoperative assessments) might be suggested [1, 4, 7, 8, 17, 19,20,21].
Differential therapeutic surgery for OSA (i.e., tailored surgical plan according to preoperative definition of site of collapse) might have a pivotal importance in OSA surgery over the last two decades. Obviously, many surgical techniques were designed to address different sites of upper airway collapse in OSA patients [11, 17,18,19,20,21,22, 30,31,32,33,34,35,36,37,38]. However, paucity of studies that consider the pattern of the collapse as a parameter for surgical decision is noticed.
In this work, the planned surgical techniques for included OSA patients were designed according to the individual patient’s preoperative pattern of collapse. Nasoendoscopy with Müller’s maneuver while the patient in supine position (MM-P) was employed to carry out the job (preoperative definition of the site/pattern of collapse) for its advantages as an available and a drug/radiation-free tool. The maneuver does not require theater occupation and can be easily applied for follow-up; it is cost-effective. Moreover, in comparison with DISE, a more informative consent could be gained [1, 10,11,12,13].
The authors performed a pre-randomization MM-P to rule out patients with prevalent hypopharyngeal/base of tongue collapses and to select those with predominant retropalatal collapse so as to obtain better statistical surgical/outcomes.
Retropalatal region is considered the most common site of obstruction; isolated palatal collapse was reported to range from 30 to 40%. Moreover, surgical interventions at the palate might be the widest practiced surgical procedures to snoring and mild–moderate OSA.
More than 50% of our patients showed a concentric pattern of collapse followed by the transverse type; several studies reported similar patterns [1, 10, 12,13,14,15,16,17,18,19,20,21,22, 27, 28]. One important finding in our work is that group C showed a high success rate (˃ 91%); this may not agree with other researchers who reported that concentric collapse at the palate was more common among their non-responders [34]. Moreover, the lowest oxygen saturation was reported among patients of concentric collapse.
The basic idea of the current work was the planned differential surgeries; the individual procedure was chosen to combat the directions of tissue collapse, i.e., opposing the pattern of collapse at a definite site. Successful outcomes with postoperative improvement (more than 90%) were reported. Both objective and subjective data were comparable to other reports [7, 8, 17,18,19,20,21,22,23,24,25, 28, 31]. Iyngkaran et al. at 2006 reported good long-term outcomes with single-level palatal surgery; our results might agree with them [34]. Interestingly, upon application of Sher criteria for surgical success (at least 50% decrease from the baseline AHI), successful outcomes were reported in all our cases (100%) [36].
This work’s data showed that included patients had significant improvement of different PSG values and minimal morbidities. Therefore, we can conclude that the described techniques appear to be promising. Nine patients were responders with postoperative AHI range of 10.37 − 13.25. Seven of them (77.78%) were satisfied of the gained results (ESS and VAS of snoring) and refused to proceed for further interventions. Two patients were planned to have laser palatoplasty (LAUP) under local anesthesia.
The obtained results revealed that the described protocol for management of retropalatal OSA depending on the pattern of collapse at a specific site was reliable and effective. Moreover, the successful outcomes might agree with the provided idea: the importance of proper differential therapeutic management to optimize OSA tasks while minimizing the morbidity of the intervention.
Clinical relevance
Surgical intervention of OSA patients could be effectively planned according to preoperative definition of site/pattern of collapse. From the surgical point of view, the required data for a planned surgical procedure could be gained from awake endoscopy with Müller’s maneuver (while the patient in a supine position; MM-P). MM-P represents an easy, available, radiation-free and a less-costly procedure. Also (in comparison with DISE), MM-P provides a more informative consent [1].
Points of strength
First: the study has a prospective nature which provides accurate assessment of data without depending on archived data or patients re-calling; Second: blind reporting of results that would reflect on data validation; Third: the study obeyed the recent applicable tissue preserving/expansive surgical procedures (DSS and/or MAP) without excess tissue removal. Also, the study could employ awake endoscopy in supine position (MM-P) as a single preoperative tool.
Limitations
The current study is not free of limitations. First, it is a preliminary report of a new assumption that will call more discussions. Second, the limited number of patients; it could be partly attributed to the narrow-spectrum selection criteria. Third, the concomitant effect of tonsillectomy (which is a usual obstacle in sleep apnea surgery that needs more than a single procedure); we tried to avoid the effect of tonsillectomy by including early cases of tonsillar enlargement. Fourth, reporting MM-P can also be hampered by inter-observer variability; to minimize the influence of inter-observer variability in this work, MM-P were evaluated by three independent experienced examiners; a high inter-observer agreement was observed. Finally, it is a short-term study and represents a single institution experience. Further larger, long-term studies with prospective comparisons need to be run, in order to obtain stronger evidences and more stable results.
Conclusion
Preoperative differential topographical diagnosis of OSA with MM-P allows for tailored surgical management. Tailored procedures could yield good surgical outcomes when patients are properly selected and the technique is chosen according to preoperative topographical diagnostic assessment. This study might provide an available, less-costly and effective preoperative planning for OSA intervention.
References
Askar SM, Quriba AS, Hassan EM, Awad AM (2020) Positional awake endoscopy versus DISE in assessment of OSA: a Comparative Study. Laryngoscope 130:2269–2274. https://doi.org/10.1002/lary.28391
Young T, Finn L, Peppard PE, Szklo-Coxe M et al (2008) Sleep disordered breathing and mortality: 18-year follow-up of the Wisconsin sleep cohort. Sleep 31:1071–1078
Weaver TE, Grunstein RR (2008) Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc 5:173–178
El-Anwar MW, Askar SM (2019) Hyoid periosteum sutures: a modified tissue-preserving hyoid suspension technique for obstructive sleep apnea. J Craniofac Surg 30(3):1
Carrasco-Llatas M, Zerpa-Zerpa V, Dalmau-Galofre J (2017) Reliability of drug-induced sedation endoscopy: interobserver agreement. Sleep Breath 21(1):173–179
de Vito A, Carrasco Llatas M, Vanni A et al (2014) European position paper on drug-induced sedation endoscopy (DISE). Sleep Breath 18:453–465
El-Ahl MAS, El-Anwar MW (2016) Expansion pharyngoplasty by new simple suspension sutures without tonsillectomy. Otolaryngol Head Neck Surg 155(6):1065–1068
Askar SM, El-Anwar MW (2018) Double suspension sutures: a simple surgical technique for selected cases of obstructive sleep apnea: our experience with twenty-two patients. Clin Otolaryngol 43(2):753–757
Wang WM, Hsu YB, Lan MY et al (2018) The relationship between modified Mallampati score, Müller’s maneuver and drug-induced sleep endoscopy regarding retrolingual obstruction. Ann Otol Rhinol Laryngol 127(7):463–469
Fernandez-Julian E, Garcia-Perez MA, Garcia-Callejo J et al (2014) Surgical planning after sleep versus awake techniques in patients with obstructive sleep apnea. Laryngoscope 124:1970–1974
Friedman M, Ibrahim H, Bass L (2002) Clinical staging for sleep disordered breathing. Otolaryngol Head Neck Surg 127:13–21
Yilmaz Y, Kum R, Ozcan M et al (2015) Drug-induced sleep endoscopy versus Müller maneuver in patients with retropalatal obstruction. Laryngoscope 125:2220–2225
Jung AR, Koh TK, Kim SJ et al (2017) Comparison of level and degree of upper airway obstruction by Muller’s maneuver and drug-induced sleep endoscopy in obstructive sleep apnea patients. Auris Nasus Larynx 44:571–575
Yagi H, Nakata S, Tsuge H et al (2009) Morphological examination of upper airway in obstructive sleep apnea. Auris Nasus Larynx 36(4):444–449
Lovato A, Kotecha B, Vianello A et al (2015) Nasal and oral snoring endoscopy: novel and promising tools in OSAS patients. Eur Arch Otorhinolaryngol 272:1793–1799
Vicini C, De Vito A, Benazzo M et al (2012) The nose oropharynx hypopharynx and larynx (NOHL) classification: a new system of diagnostic standardized examination for OSAHS patients. Eur Arch Otorhinolaryngol 269:1297–1300
Askar SM, El-Anwar MW, Awad A (2018) Modified anterior palatoplasty and double suspension sutures (with or without tonsillectomy) in selected patients with obstructive sleep apnea: a preliminary report. Sleep Breath 22:789–795
Benazzo M, Pagella F, Matti E et al (2008) Hyoidthyroidpexia as a treatment in multilevel surgery for obstructive sleep apnea. Acta Otolaryngol 128:680–684
Tantawy A, Amer ASM, HS, et al (2018) Hyoid bone suspension as a part of multilevel surgery for obstructive sleep apnea syndrome. Int Arch Otorhinolaryngol 22(3):266–270. https://doi.org/10.1055/s-0037-1607227
Askar SM, El-Anwar MW, Amer HS et al (2017) Single triangular suture: a modified technique for hyoid suspension as a treatment for obstructive sleep apnea: Our experience with 24 patients. Clin Otolaryngol 42(6):1418–1421. https://doi.org/10.1111/coa.12925
De Corso E, Fiorita A, Rizzotto G, Mennuni GF et al (2013) The role of drug-induced sleep endoscopy in the diagnosis and management of obstructive sleep apnoea syndrome: our personal experience. Acta Otorhinolaryngica 33:405–413
Adzereil B, Wong EH, Saraiza A et al (2017) The effectiveness of combined tonsillectomy and anterior palatoplasty in the treatment of snoring and obstructive sleep apnea (OSA). Eur Arch Otorhinolaryngol 274:2005–2011
Pang KP, Tan R, Puraviappan P, Terris DJ (2009) Anterior palatoplasty for the treatment of OSA: three-year results. Otolaryngol Head Neck Surg 141(2):253–256
Pang KP, Terris DJ (2007) Modified cautery-assisted palatal stiffening operation: new method for treating snoring and mild obstructive sleep apnea. Otolaryngol Head Neck Surg 136:823–826
Rotenberg BW, Vicini C, Pang EB et al (2016) Reconsidering first-line treatment for obstructive sleep apnea: a systematic review of the literature. Rotenberg et al. J Otolaryngol Head Neck Surg 45:23.
Sorrenti G, Piccin O (2013) Functional expansion pharyngoplasty in the treatment of obstructive sleep apnea. Laryngoscope 123(11):2905–2908
Ravesloot MJL, De Vries N (2011) One hundred consecutive patients undergoing drug-induced sleep endoscopy: results and evaluation. Laryngoscope 121:2710–2716
Ugur KS, Ark N, Kurtaran H, Kizilbulut G et al (2014) Anterior palatoplasty for selected mild and moderate obstructive sleep apnea: preliminary results. Eur Arch Otorhinolaryngol 271:1777–1783
Binar and Karakoc (2018) Anterior palatoplasty for obstructive sleep apnea: a systematic review and meta-analysis. Otolaryngol Head Neck Surg 158(3):443–449
Kotecha B, De Vito A (2018) Drug induced sleep endoscopy: its role in evaluation of the upper airway obstruction and patient selection for surgical and nonsurgical treatment. J Thorac Dis 10(Suppl 1):S40–S47
DeVito A, Cammaroto G, Chong KB et al (2019) Drug-induced sleep endoscopy: clinical application and surgical outcome. Healthcare 7(3):100. https://doi.org/10.3390/healthcare7030100
Certal VF, Pratas R, Guimaraes L et al (2016) Awake examination versus DISE for surgical decision making in patients with OSA: a systematic review. Laryngoscope 126:768–774
Pang KP, Baptista PM, Olszewska E et al (2020) Does drug-induced sleep endoscopy affect surgical outcome? A multicenter study of 326 obstructive sleep apnea patients. Laryngoscope 130(2):551–555
Iyngkaran T, Kanaglingam J, Rajeswaran R et al (2006) Long-term outcomes of laser-assisted uvulopalatoplasty in 168 patients with snoring. J Laryngol Otol 120:932–938
Koutsourelakis I, Safiruddin F, Ravesloot M et al (2012) Surgery for obstructive sleep apnea: sleep endoscopy determinants of outcome. Laryngoscope 122:2587–2591
Sher AE, Schechtman KB, Piccirillo JF (1996) The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep 19(2):156–177
Mantovani M, Minetti A, Torretta S, Pincherle A, Tassone G, Pignataro L (2012) The velo-uvulo-pharyngeal lift or “roman blinds” technique for treatment of snoring: a preliminary report. Acta Otorhinolaryngol Ital 32(1):48–53
Moffa A, Rinaldi V, Mantovani M et al (2020) Different pharyngoplasty techniques for retropalatal collapse in obstructive sleep apnea patients: a systemic review. Sleep Breath 24:1115–1127. https://doi.org/10.1007/s11325-020-02088-z
Funding
The authors declare no financial support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors do not have any potential financial conflict of interest related to or could influence this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on sleep apnea syndrome. Guest Editors: Manuele Casale, Rinaldi Vittorio.
Rights and permissions
About this article
Cite this article
Askar, S.M., El-Anwar, M.W. & Quriba, A.S. Positional awake nasoendoscopic pattern-based surgical decision for correction of retropalatal obstruction in OSA. Eur Arch Otorhinolaryngol 278, 901–909 (2021). https://doi.org/10.1007/s00405-020-06559-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-020-06559-7