Abstract
Purpose
This meta-analysis study was designed to analyze the olfactory function in obstructive sleep apnea patients (OSA).
Methods
A comprehensive review of the English language literature regarding OSA patients and olfactory function/dysfunction was performed. The papers assessing olfactory dysfunction with Sniffin’ Sticks test were taken into consideration.
Results
A total of 420 OSA patients were judged eligible for the study. The average TDI score was found to be 24.3 ± 5.6. The olfactory identification (OD), the olfactory discrimination (OD), and the olfactory threshold (OT) average values were calculated resulting 9.9 ± 2.1, 9.8 ± 1.5, and 5.3 ± 2, respectively. There were 161 healthy control subjects in this meta-analysis. The average TDI of the control group was 30.7 ± 6.0 showing a statistical difference with the group of OSA patients (p = 0.03).
A linear correlation between Apnea–Hypopnea Index (AHI) increase and TDI decrease (R2 = 0.1, p = 0.05) was detected. Finally, the average values of TDI of 151 patients classified as mild–moderate OSA and 159 patients considered as severe OSA were calculated. The difference between these two groups resulted not statistically significant (p = 0.3).
Conclusion
The comparison between OSA patients and healthy subjects using Sniffin’ Sticks test showed lower values of the various olfactory parameters. Although a linear correlation between AHI increase and olfactory dysfunction was observed, no statistical difference between mild–moderate and severe OSA patients in terms of the severity of olfactory dysfunction could be proved.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) syndrome is a respiratory sleep disorder characterized by partial or complete recurrent episodes of upper airway collapse that impair normal ventilation during sleep [1, 2]. OSA manifests with a reduction (hypopnea) or complete cessation (apnea) of airflow in the upper airways, in the presence of breathing effort [3].
The repeated nocturnal desaturation events lead the OSA patients to develop cardiovascular co-morbidities such as resistant hypertension and increased risk of cardiovascular events such as stroke and heart attack [4]. The sleep fragmentation caused by this pathology is often related to excessive daytime sleepiness and reduced neurocognitive performance, with possible deficits of memory, learning, attention, executive function, psychological problems, and depression [5, 6].
The sense of smell is a sensorineural system with a high impact on the quality of life (QOL) when its function is impaired [7,8,9]. A recent study regarding the healthy population showed that the overall incidence of olfactory dysfunction was 19.1%, composed of 13.3% and 5.8% of patients with hyposmia and anosmia, respectively [10]. Similar data were reported by Hummel et al. with a 20% incidence of olfactory dysfunction in subjects between 36 and 55 years of age [11].
Sinonasal diseases, nasal obstruction, reduced neurocognitive function, drugs, and toxins are the most important causes of olfactory dysfunction (OD) [9, 12,13,14]. Such clinical conditions may be present in OSA patients, making these subjects inclined to developing an olfactory dysfunction [1, 2, 5, 6, 15,16,17].
In 2009, Miyamoto et al. were the first to demonstrate a reduction of olfactory function in patients with obstructive sleep apnea, by means of a comparative analysis of the Odor Stick Identification Test in other diseases such as idiopathic rapid-eye-movement (REM) sleep behavior disorder (iRBD), Parkinson’s disease (PD), and dementia with Lewy bodies (DLB) [18].
Nowadays, the most widely used test for evaluation of olfactory function is the Sniffin’ Sticks test. It allows a repetitive and inexpensive evaluation of olfactory function via the use of a pen-like odor-dispensing devices [19]. This test investigates hyposmia and anosmia conditions, and allows a reproducibility and comparison of the data obtained [20]. The Sniffin’ Sticks test includes three sub-tests which evaluate the olfactory threshold (OD), olfactory discrimination (OD), and identification (OI). The sum of the results from each of three different sub-tests results in a total score defined as TDI. According to the existing literature, the results of the TDI score indicate hyposmia when the total TDI score is < 30.5, anosmia when it is < 16.5, and no OD when the TDI score is > 30.5 [21].
Using the Sniffin’ Sticks test, Magliulo et al. showed that olfactory dysfunction was present in 36.6% of OSA patients [9]. Of these cases, 86.4% presented hyposmia and 13.6% anosmia. A strong negative correlation between olfactory dysfunction (measured with TDI) and the severity of sleep apnea (measured with the AHI) was found. Other author used the Sniffin’ Sticks test to investigate the correlation between OSA and olfactory function and published interesting results [8,9,10,11]. They found a lower olfactory function in OSA patients, variability of the olfactory parameters in relation to OSA sub-class severity, and differences in olfactory function compared with non-OSA healthy patients [8,9,10,11].
Considering the growing scientific evidence concerning olfactory dysfunction in OSA patients, we found useful to analyze the results obtained from the various clinical studies present in the literature regarding this topic.
The main objective of this study is to confirm the described evidence of a reduced olfactory function in OSAS patients, an aspect so far demonstrated only in isolated studies. Hence, a meta-analysis to evaluate the effect of OSA on olfactory function was performed to corroborate the data previously reported by other authors [7,8,9,10]. No meta-analysis studies regarding the olfactory dysfunction in OSA patients have been published to date.
Materials and methods
Literature review: research protocol
A comprehensive review of the English language literature regarding OSA patients and olfactory function/dysfunction was performed using PubMed, EMBASE, Cochrane Library, and CENTRAL electronic databases.
The search was conducted using the following keywords: “Sleep apnea and smell”, “Sleep apnea and olfactory dysfunction”, “Sleep apnea and olfactory function”, “OSA and smell”, and “OSA and olfactory dysfunction”.
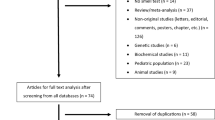
Fifteen records regarding the topics studied were initially identified by abstract reading. One paper was excluded, because found to be duplicated during research.
Six papers were excluded later for the following reasons: letter to the editor (one paper), absence of data about TDI/AHI (one paper), and olfactory dysfunction not tested using the Sniffin’ Sticks test (four papers).
The flowchart of study selection is reported in Fig. 1.
Meta‑analysis protocol
Articles were examined for data resolution with the intent of performing a meta-analysis.
Data from the studies were first extracted and assessed by the principal investigator (G. I.) and then independently evaluated by two coauthors (A. M. and G. M.) using standardized data forms. The Apnea–Hypopnea Index (AHI), Epworth Sleepiness Scale (ESS), body mass index (BMI) score, mean SpO2, and OSA sub-classes classification in according to the severity of the pathology were collected and analyzed.
Different methods of meta-analysis were considered in reviewing the literature to seek results that would provide meaningful analysis with the least risk of introducing biases.
This protocol was developed in line with the quality requirements of the preferred reporting items for systematic review and meta-analysis protocols (PRISMA) statement [22].
The quality assessment of studies (QUADAS-2) tool was used to evaluate the relevant study design characteristics of the included studies [23].
Statistical analysis was performed using statistical software (STATA 8.2; StataCorp LP, College Station, Texas).
Random-effects modeling (standard error estimate = inverse of the sample size) was used to calculate summary effect measures with corresponding 95% confidence intervals (CI), and forest plots were generated. The I2 statistic was used to assess between-study heterogeneity.
Results
A graphical display of QUADAS-2 results is shown in Fig. 2. This graphical display shows the possible risk of bias.
Eight studies were included in the meta-analysis aimed at evaluation of olfactory function in Obstructive Sleep Apnea [7,8,9, 11, 16, 17, 24, 25]. A total of 420 OSA patients (85 females, 335 males) were considered eligible for the study. Patient’s characteristics, AHI, ESS, BMI, mean SpO2, and Sniffin’ Sticks test results are summarized in Table 1. The mean age of OSA patients was 49.3 years. The average AHI of OSA patients evaluated was 34.2 ± 19.8. The average values of ESS, SpO2, and BMI were 10.4 ± 1, 93.3 ± 2.2, and 29.5 ± 2, respectively.
The average TDI score of the entire study group was found to be 24.3 ± 5.6. The OI, OD, and OT average values were calculated as 9.9 ± 2.1, 9.8 ± 1.5, and 5.3 ± 2, respectively.
The distribution of TDI values of different studies (forest plot defined according to OSAS severity sub-classes when reported in the studies) is reported in Fig. 3.
Using random-effects modeling (Fig. 4), the meta-analysis showed a significative relative risk of developing a lower TDI in relation to the severity of the AHI score (p = 0.00, I2 = 92.2%).
Six studies described a control group that was used to compare the olfactory results between sleep apnea patients and healthy patients [7,8,9, 17, 24, 25]. A total of 161 healthy control patients were considered in the meta-analysis (Table 1). The mean age was found to be 49.2 years with an average AHI of 3.2 ± 1.2. No statistical difference in average age emerged comparing OSA patients and the control group (p = 1).
The average TDI of the control group was 30.7 ± 6.0; a statistical difference with the group of OSA patients (p = 0.03) was calculated. The same statistical difference emerged in OI, OD, and OT values between OSA patients and the control group (p < 0.05 in each case). The differences in OSA characteristics between these two groups of patients are reported in Table 1.
These data were confirmed by comparing TDI and AHI in the healthy subjects of the control group using the meta-regression analysis model. A linear correlation between AHI increase and TDI decrease emerged (R2 = 0.1, p = 0.05). Meta-regression analysis results, comparing TDI with ESS, SpO2, and BMI, are reported in Fig. 5.
a Meta-regression model comparing the TDI scores and AHI scores showed correlation between TDI and AHI increase (p = 0.05); b meta-regression model comparing the TDI scores and ESS scores showed correlation between TDI and ESS increase (p = 0.04); c meta-regression model comparing the TDI scores and SpO2 scores showed no correlation between TDI and SpO2 increase (p = 0.08); d meta-regression model comparing the TDI scores and BMI scores showed no correlation between TDI and BMI increase (p = 0.09)
Five studies reported the olfactory function in the different severity classes of the OSA [7, 8, 16, 23, 24]. These studies were taken into consideration for the meta-analysis that compared the olfactory dysfunction in the different severity classes of the OSA. In these studies, 151 patients were classified as mild–moderate OSA, whereas 159 patients were considered as severe.
The average TDI of the mild–moderate group was 25.3 ± 5.5, whereas the severe group showed an average TDI of 21.7 ± 6.37. Despite a difference between these two groups in the average value of TDI, a statistical difference did not emerge (p = 0.3). Similarly, no difference emerged in OI, OD, and OT between mild–moderate and severe OSA patients (p > 0.05 in each case). The differences in OSA characteristics between these two groups of patients are reported in Table 1.
Discussion
Major findings of the literature and results emerging from the study
In the literature, it is well documented how the risk of olfactory dysfunction increases with age and can be related to various other pathologies such as nasal obstruction, chronic rhinosinusitis, head injuries, upper respiratory tract infections, or neurodegenerative diseases [10, 12, 26,27,28,29]. Furthermore, it is described in the literature how the patient with OSA may present different factors correlated to OD (nasal obstruction, neurocognitive deficits, chronic rhinosinusitis, etc.) [30, 31]. The available data regarding the incidence and grade of olfactory dysfunctions in OSA patients have increased over the last few years [24, 33, 34].
In 2015, Günbey et al. demonstrated how OSA patients, compared to healthy adults, present a reduced identification, discrimination and TDI scores of odors [8]. Similarly, in the study of Liu et al. the OD, OI, and TDI scores were significantly higher in a control group (snoring patients) than in the study groups (mild, moderate, and severe OSA patients) (p < 0.05) [11]. In their study, Versace et al. showed that OSA patients had a mean TDI of 22.4 ± 3.6, whereas control patients had a mean TDI of 32.7 ± 4.5 with an evident statistical difference (p < 0.001) [24].
In this meta-analysis, the average TDI score of the entire study group was 24.3 ± 5.6, classifying OSA patients in the TDI range of anosmic patients. The data that emerged from the six studies which considered a control group of healthy patients revealed a statistical difference between the mean TDI of patients with OSA and the control group (p = 0.03). A similar statistical difference emerged in the values of OI, OD, and OT. It was not possible to calculate the differences between the percentages of anosmic and/or hyposmic subjects among OSAS patients, because these percentages were reported in only two of the studies analyzed.
Various studies studying olfactory function in OSA patients have also shown the severity of OSA to be correlated with olfactory dysfunction. Günbey et al. found a strong negative correlation between all the olfactory scores of the Sniffin’ Sticks test and mean arterial oxygen saturation, lowest oxygen saturation, and AHI [8]. Similarly, Magliulo et al., using a regression analysis, found a strong correlation (p = 0.04; R2 = 0.05) between olfactory dysfunction (lower TDI) and the severity of sleep apnea assessed using the AHI [9]. A strong inverse correlation between AHI and TDI scores (r = − 0.62, p < 0.001) was also reported in a very recent study by Karakurt et al. [25].
The above data were confirmed in our meta-analysis study, using the regression analysis model to compare TDI and OSA scores. A linear correlation between AHI increase and reduction of TDI emerged (R2 = 0.1, p = 0.05). Significant correlations were also found between TDI and ESS (R2 = 0.2 and p = 0.04), whereas SpO2 and BMI did not show a statistical correlation (p > 0.05). Using random-effects modeling (Fig. 4), the meta-analysis revealed a significant relative risk of having a lower TDI in relation to the severity of the AHI (p = 0.00, I2 = 92.2%).
Is there a difference in olfactory function between mild–moderate and severe OSA patients? Although single studies seem to show that a difference exists between these two groups, our meta-analysis has shown different results. Five of the studies considered in the meta-analysis compared olfactory dysfunction in patients with mild-moderate OSA with that of severe OSA patients: 151 patients were classified as mild–moderate OSA and 159 patients were considered as severe OSA. The average TDI in the mild-moderate group was found to be 25.3 ± 5.5, while the severe group showed an average TDI of 21.7 ± 6.37. Despite the differences in the mean TDI values between these two groups, a statistically significant difference did not emerge (p = 0.3). Similarly, no differences were observed in the mean scores of OI, OD, and OT between mild–moderate and severe OSA patients (p > 0.05 in each case) (Table 1).
These findings lead us to conclude that the severity of OSA correlates with olfactory dysfunction, but mild–moderate and severe OSA patients do not present a difference in the olfactory scores resulting from the Sniffin’ Sticks test.
Possible reasons of correlation between OSA and olfactory dysfunction
Although the literature currently available indicates a possible correlation between OSA and olfactory function, little is known regarding the mechanism underlying this probable relationship.
The pathophysiological process underlying olfactory dysfunction in OSA patients could be attributable to the effects of a cognitive deterioration in such patients characterized by a disorder of the central cholinergic system [32]. Impairment of this system would lead to a deficit in odor memory, recognition of a familiar odor and the acquisition of a complex odor discrimination activity. Regarding this aspect, Versace et al. performed an evaluation of cholinergic neurotransmission and olfactory function in obstructive sleep apnea syndrome patients 24. They used the short latency afferent inhibition (SAI) that is a paired-pulse transcranial magnetic stimulation (TMS) protocol that makes it possible to test an inhibitory cholinergic circuit in the human cerebral motor cortex. Twenty patients with OSA and 20 healthy control subjects were tested: SAI was reduced in OSA patients in comparison to control subjects and impairment of cholinergic neurotransmission was observed in OSA patients. The Kendall rank test revealed a strong negative correlation between TDI and SAI in the patient group (tau = − 0.84, p < 0.001).
In addition to these findings, several studies have reported that deprivation/fragmentation of sleep and intermittent hypoxia is associated with reduced activity in the prefrontal and posterior parietal cortex such as neuronal loss in the hippocampus and the thalamus where the areas involved in neurological odor processing are localized [35,36,37]. Previous studies have shown that an individual’s cognitive performance exerts a significant influence on olfactory functions and that an improvement in cognitive performance, usually impaired in OSA patients, could be associated with a gain in olfactory function. These aspects have been demonstrated by Koseoglu et al. who used the Sniffin’ test to evaluate alterations in the olfactory indices before and after C-PAP treatment in OSA patients [16]. A total of 30 patients included in the study presented a significant improvement of OT, OD, and OI scores after C-PAP therapy (p = 0.001, p = 0.002, and p = 0.001, respectively). The post-treatment TDI score (32.50 ± 3.88) was also significantly higher than the pre-treatment scores (28.48 ± 4.71) (p = 0.001).
In our opinion, despite the published findings mentioned above, further studies are needed to clarify the pathophysiological factors responsible for impairment of olfactory function in OSA patients.
Finally, the high BMI of OSAS patients is in our opinion another important aspect that should be remembered and discussed. An elevated BMI is a well-established characteristic of OSA patients which could be correlated with the reduction of smell in OSA patients. Various studies have described a decline of TDI with increased BMI. In this regard, Peng et al. [38], in a meta-analyses study, reported that olfactory function is negatively correlated with body weight. In our meta-analysis, a statistical difference between OSA patients and the healthy control group emerged regarding BMI (p = 0.004; Table 1). However, as shown in Fig. 5d, despite a linear correlation between TDI and BMI, the meta-regression analysis failed to show a positive correlation (p = 0.09).
This might indicate that BMI is one of the possible co-factors of the olfactory dysfunction observed in OSAS patients, even though it cannot be considered the only one.
Implications of observed results
The main objective of this study is to confirm the reduced olfactory function of OSAS patients, an aspect so far demonstrated only by isolated studies.
The sense of smell is a sensorineural system with a high impact on the quality of life. Patients with olfactory loss have a reduction in QOL with consequences that affect both the emotional and psychological spheres and are related to a greater propensity to fall into a depressive state. In OSA patients, these aspects could be added to the neurocognitive disorders typical of this disease, further worsening the quality of life of these patients.
Further studies to evaluate the aspects of olfactory disfunction in OSA patients (e.g., quantifying odor-induced changes in electrical activity at the level of the olfactory epithelium by the electro-olfactogram and cortex using odor event-related potentials) such as the possibilities of improving the sense of smell in OSA patients (e.g., by olfactory training or drugs) are under way.
Limitations of the study
Nasal obstruction and/or chronic rhinosinusitis have not been analyzed in this meta-analysis, because almost all the selected studies failed to consider these aspects.
These conditions are frequently observed in OSA patients (patients with oral breathing). In our opinion, theseOtolaryngology, Head-Neck two factors should be considered among the underlying mechanisms of OD in OSA patients.
Another limitation to consider is that not all the studies included in this meta-analysis analyzed the differences in the OD of the different OSA sub-classes (mild, moderate, and severe according to the AHI values). In fact, in almost all the studies, patients with mild and moderate OSAS were considered as a single group. This did not allow us to evaluate differences in olfactory function between patients with mild OSAS and severe OSAS.
Conclusion
The authors performed this meta-analysis study to identify and characterize olfactory dysfunction in sleep apnea patients. OSA patients present lower values of olfactory parameters, tested with the use of the Sniffin’ Sticks test, when compared to healthy subjects. Despite the fact that a linear correlation between AHI increase and olfactory dysfunction emerged, there would seem to be no statistical difference between mild–moderate and severe OSA patients in terms of the severity of olfactory dysfunction.
References
Kapur VK, Auckley DH, Chowdhuri S, Clinical Practice Guideline for Diagnostic Testing for Adult et al (2017) Obstructive sleep apnea: an american academy of sleep medicine clinical practice guideline. J Clin Sleep Med 13(3):479–504
American Academy of Sleep Medicine (2014) International classification of sleep disorders, 3rd edn. American Academy of Sleep Medicine, Darien
Iannella G, Maniaci A, Magliulo G, Cocuzza S, La Mantia I, Cammaroto G, Greco A, Vicini C (2020) Current challenges in the diagnosis and treatment of obstructive sleep apnea syndrome in the elderly. Pol Arch Intern Med 130:649–654
Barbe F, Duran-Cantolla J, Sanchez-de-la-Torre M et al (2012) Effect of continuous positive airway pressure on the incidence of hypertension and cardiovascular events in nonsleepy patients with obstructive sleep apnea: a randomized controlled trial. JAMA 307(20):2161–2168
Jackson ML, Howard ME, Barnes M (2011) Cognition and daytime functioning in sleep-related breathing disorders. Prog Brain Res 190:53–68
Gulotta G, Iannella G, Vicini C et al (2019) Risk factors for obstructive sleep apnea syndrome in children: state of the art. Int J Environ Res Public Health 16(18):3235
Salihoğlu M, Kendirli MT, Altundağ A et al (2014) The effect of obstructive sleep apnea on olfactory functions. Laryngoscope 124(9):2190–2194
Günbey E, Güzel A, Karlı R, Ünal R (2015) The relationships between the clinical and polysomnographic findings and the olfactory function in patients with obstructive sleep apnea syndrome. Sleep Breath 19(4):1301–1307
Magliulo G, De Vincentiis M, Iannella G et al (2018) Olfactory evaluation in obstructive sleep apnoea patients. Acta Otorhinolaryngol Ital 38(4):338–345
Savage SA, Butler CR, Milton F, Han Y, Zeman AZ (2017) On the nose: olfactory disturbances in patients with transient epileptic amnesia. Epilepsy Behav 66:113–119
Boesveldt S, Postma EM, Boak D et al (2017) Anosmia-a clinical review. Chem Senses 42:513–523
Boesveldt S, Postma EM, Boak D et al (2017) Anosmia—a clinical review [published correction appears]. Chem Senses 42(7):513–523
Doty RL (2012) Olfaction in Parkinson’s disease and related disorders. Neurobiol Dis 46(3):527–552
Frasnelli J, Hummel T (2005) Olfactory dysfunction and daily life. Eur Arch Otorhinolaryngol 262:231–235
Brämerson A, Johansson L, Ek L, Nordin S, Bende M (2004) Prevalence of olfactory dysfunction: the skövde population-based study. Laryngoscope 114(4):733–737
Koseoğlu S, Derin S, Yilmaz M, Kutlu G, Sahan M (2017) Does positive airway pressure therapy improve olfactory function? Int Forum Allergy Rhinol 7(6):557–560
Shin DH, Ahn SH, Yang Y et al (2017) The effect of sleep disordered breathing on olfactory functions: analysis by apnea–hypopnea index. Clin Exp Otorhinolaryngol 10(1):71–76
Miyamoto T, Miyamoto M, Iwanami M, Suzuki K, Inoue Y, Hirata K (2009) Odor identification test as an indicator of idiopathic REM sleep behavior disorder. Mov Disord 24(2):268–273
Hummel T, Kobal G, Gudziol H, Mackay-Sim A (2007) Normative data for the "Sniffin' Sticks" including tests of odor identification, odor discrimination, and olfactory thresholds: an upgrade based on a group of more than 3000 subjects. Eur Arch Otorhinolaryngol 264(3):237–243
Kobal G, Hummel T, Sekinger B, Barz S, Roscher S, Wolf S (1996) “Sniffin’ Sticks”: screening of olfactory performance. Rhinology 34:222–226
Wolfensberger M, Schnieper I, Welge-Lüssen A (2000) Sniffin’ Sticks: a new olfactory test battery. Acta Otolaryngol 120(2):303–306
Moher D, Shamseer L, Clarke M, PRISMA-P Group (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4:1
Whiting PF, Rutjes AW, Westwood ME et al (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155(8):529–536
Versace V, Langthaler PB, Sebastianelli L et al (2017) Cholinergic neurotransmission and olfactory function in obstructive sleep apnea syndrome: a TMS study. Sleep Med 37:113–118
Karakurt SE, Karakuş MF, Çolak M et al (2019) Evaluation of olfactory function in patients with obstructive sleep apnea syndrome. Sleep Breath. https://doi.org/10.1007/s11325-019-01996-z
Roalf DR, Moberg MJ, Turetsky BI et al (2017) A quantitative meta-analysis of olfactory dysfunction in mild cognitive impairment. J Neurol Neurosurg Psychiatry 88(3):226–232
Iannella G, Vicini C, Colizza A et al (2019) Aging effect on sleepiness and apneas severity in patients with obstructive sleep apnea syndrome: a meta-analysis study. Eur Arch Otorhinolaryngol 276(12):3549–3556
Magliulo G, Iannella G, Ciofalo A, Angeletti D, Pulvirenti F, Quinti I (2019) The olfactory function in patients with common variable immunodeficiency. Eur Ann Otorhinolaryngol Head Neck Dis 136(6):429–434
Magliulo G, Iannella G, Ciofalo A et al (2019) Nasal pathologies in patients with obstructive sleep apnoea. Acta Otorhinolaryngol Ital 39(4):250–256
Iannella G, Magliulo G, Di Luca M et al (2020) Lateral pharyngoplasty techniques for obstructive sleep apnea syndrome: a comparative experimental stress test of two different techniques. Eur Arch Otorhinolaryngol 277:1793–1800
Iannella G, Vallicelli B, Magliulo G et al (2020) Long-term subjective outcomes of barbed reposition pharyngoplasty for obstructive sleep apnea syndrome treatment. Int J Environ Res Public Health 17(5):1542
Wilson RS, Arnold SE, Schneider JA, Tang Y, Bennett DA (2007) The relationship between cerebral Alzheimer’s disease pathology and odour identification in old age. J Neurol Neurosurg Psychiatry 78:30–35
Barnes DC, Wilson DA (2014) Sleep and olfactory cortical plasticity. Front Behav Neurosci 8:134
Tobler I (1995) Is sleep fundamentally different between mammalian species? Behav Brain Res 69(1–2):35–41
Brown RE, Basheer R, McKenna JT, Strecker RE, McCarley RW (2012) Control of sleep and wakefulness. Physiol Rev 92(3):1087–1187
Ciofalo A, Zambetti G, Romeo M et al (2015) Taste and olfaction in middle ear surgery. Ann Otol Rhinol Laryngol 124(4):312–316
Wagner U, Born J (2008) Memory consolidation during sleep: interactive effects of sleep stages and HPA regulation. Stress 11(1):28–41
Peng M, Coutts D, Wang T, Cakmak YO (2019) Systematic review of olfactory shifts related to obesity. Obes Rev 20(2):325–338
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on sleep apnea syndrome Guest Editors: Manuele Casale, Rinaldi Vittorio.
Rights and permissions
About this article
Cite this article
Iannella, G., Magliulo, G., Maniaci, A. et al. Olfactory function in patients with obstructive sleep apnea: a meta-analysis study. Eur Arch Otorhinolaryngol 278, 883–891 (2021). https://doi.org/10.1007/s00405-020-06316-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-020-06316-w