Abstract
Unique among solid organ tumors, hepatocellular carcinoma (HCC), may be diagnosed by imaging alone, without the need for biopsy. The Liver Imaging Reporting and Data System (LI-RADS) was developed to provide high-specificity diagnosis of HCC based on imaging while also standardizing the assessment and reporting of the entire spectrum of lesions and pseudolesions encountered in patients at risk for this malignancy. In this pictorial review, we discuss management recommendations associated with CT/MR LI-RADS observations. We emphasize the rationale for the recommendations and the role of multidisciplinary management discussion, and we provide a framework for standardized reporting. Management of patients who undergo ultrasound (US) for screening and surveillance or those who undergo diagnostic contrast-enhanced ultrasound (CEUS) is beyond the scope of this paper.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC), the most common primary liver malignancy worldwide, is the fifth most common cancer in men and seventh most common cancer in women [1]. The incidence of HCC in the U.S has increased by 2.3% per year between 2003 and 2012 [2]. Hepatitis C, non-alcoholic fatty liver disease (NAFLD), alcohol-related cirrhosis and other causes of cirrhosis, along with hepatitis B even in the absence of cirrhosis, are the major contributing factors for developing HCC.
Unique among solid organ tumors, HCC may be diagnosed by imaging alone, without the need for biopsy [3,4,5]. The Liver Imaging Reporting and Data System (LI-RADS) was developed to provide high-specificity diagnosis of HCC based on imaging while also standardizing the assessment and reporting of the entire spectrum of lesions and pseudolesions encountered in patients at risk for this malignancy.
LI-RADS categorizes observations from LR-1 to LR-5 depending on their relative probability of being HCC. LR-5 is definite HCC with an intended specificity approaching 100%. Two additional categories (LR-M: probable or definitely malignant but not specific for HCC; LR-TIV: tumor in vein) further hone the specificity of LR-5 for HCC and maintain sensitivity for the diagnosis of malignancy and more advanced disease [6]. In 2018, LI-RADS was integrated into AASLD HCC clinical practice guidelines. As a result, the AASLD management recommendations directly relate to the LI-RADS categories [7].
In this pictorial review, we discuss management recommendations associated with CT/MR LI-RADS observations. We emphasize the rationale for the recommendations and the role of multidisciplinary management discussion, and we provide a framework for standardized reporting. Management of patients who undergo ultrasound (US) for screening and surveillance or those who undergo diagnostic contrast-enhanced ultrasound (CEUS) is beyond the scope of this paper.
LI-RADS overview
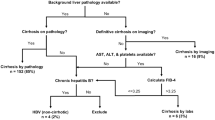
LI-RADS is a comprehensive system for diagnosing HCC. It consists of four separate algorithms: Ultrasound surveillance, CT/MRI diagnosis, CEUS diagnosis, and CT/MRI treatment response. The LI-RADS CT/MRI Diagnostic Algorithm can be applied to CT and MRI exams performed in patients at high risk for HCC, including those with cirrhosis, chronic hepatitis B, and current or prior HCC, as well as transplant candidates or recipients with HCC [8]. The LI-RADS Treatment Response algorithm is used to assess HCC response to locoregional therapy [8]. The choice of multi-phase CT or MRI is left to radiologist judgment, institutional preference, and regional practice patterns, among other factors, but LI-RADS may be used with either modality. LI-RADS may be applied to MRI performed with either extracellular or hepatobiliary (e.g., gadoxetate disodium) contrast agents.
Importantly, LI-RADS is not applied in patients who are less than 18 years old due to lack of data validating its use in these patients. Patients with cirrhosis secondary to congenital hepatic fibrosis or vascular disorders are also excluded because these patients have a high incidence of arterial-phase hyperenhancing benign nodules which may mimic HCC on imaging.
Technical considerations
When applying LI-RADS, a critical requirement is that the CT or MR examination is performed with appropriate technique. For CT, the recommendation includes a scanner with ≥ 8 detector rows, at least three acquired dynamic post contrast phases: arterial (late arterial phase strongly preferred over early arterial phase), portal venous, and 2- to 5-min delayed. If the patient has had prior locoregional therapy, then a non-contrast phase is suggested [9, 10].
For MR examinations, 1.5T or 3T field strength with a torso phased array coil is required. For studies performed with an extracellular contrast agent, the recommended sequences include unenhanced T1-weighted out-of-phase and in-phase, T2-weighted, and dynamic multi-phase T1-weighted imaging, the latter including pre-contrast, arterial (similar to CT recommendations, late arterial phase is strongly preferred), portal venous, and 2- to 5-minute delayed phases. Diffusion-weighted imaging is also suggested and may reveal ancillary features. Subtraction of the dynamic contrast-enhanced imaging may be performed to improve conspicuity of lesions. If gadoxetate disodium is used, a transitional phase is performed in lieu of the delayed phase, at 2–5 min post injection, as well as a hepatobiliary phase at about 20 min.
Only when patients have undergone technically adequate CT and MR examinations, can radiologists categorize observations using LI-RADS and guide management for these patients. Management options include return to routine surveillance in about 6 months, repeat imaging with the same method as the study just performed, or possibly with an alternative diagnostic method if such a method is likely to be advantageous diagnostically. For example, if poor liver function compromises uptake of gadoxetate disodium, then MRI with an extracellular agent may be preferable. Similarly if patients are not candidates for or cannot tolerate MRI, then CT would be preferred for diagnostic imaging.
Role of diagnostic radiologist as a member of a multidisciplinary management team
It is important for a radiologist to understand the role of imaging and other clinical and laboratory factors that contribute to establishing an HCC diagnosis and determine management options. A radiologist is an important member of a multidisciplinary team, whether explicitly by attending multidisciplinary conferences, or implicitly by issuing a report that will be an important contributor to management decisions.
Familiarity with the LI-RADS population is crucial in order to avoid inappropriate use of LI-RADS. For example, assigning an LR-5 category in a patient without risk factors for HCC may lead to aggressive treatment of a benign lesion (e.g., hepatocellular adenoma), or HCC-targeted treatment being applied to a non-HCC malignancy (e.g., carcinoid metastasis). Alternatively, not recognizing the appropriate patient for LI-RADS use may lead to unnecessary biopsy and delay in diagnosis (see Fig. 1).
A 52-year-old female with incidental 2 cm mass on abdominal CT done for flank pain. MRI using hepatobiliary phase contrast agent demonstrates non-rim arterial-phase hyperenhancement on arterial-phase image (a) and washout appearance on delayed phase imaging (b) (see white arrows, a–b). The history of chronic hepatitis B infection was not provided at the time of initial imaging, and the lesion was categorized as hepatic adenoma. 2.5 years later, the patient returns with abdominal pain, AFP >200,000 and repeat MRI using hepatobiliary phase contrast agent demonstrates the mass has now grown to 14 cm mass, continues to demonstrate non-rim arterial hyperenhancement mass on arterial-phase imaging (c, white arrow) with washout appearance on portal venous phase (white arrow, d). The observation was categorized as LR-5 observation, definitely HCC and confirmed at hepatectomy after tumor rupture
Knowledge of the LI-RADS algorithm and its diagnostic criteria is necessary in order to assign the most appropriate category for any given observation. Both under-categorizing and over-categorizing observations can lead to inappropriate management decisions, which in turn may have prognostic implications.
The LI-RADS categories were developed so that each category should have significant impact on decisions about diagnosis and treatment. Many factors other than imaging influence the final diagnosis and guide the management plan. It may help to think of this as “layers of diagnostic thinking,” beginning with the imaging test itself and eventually arriving at a management decision based on all factors, including but not restricted to the assigned LI-RADS category.
It is not necessary for radiologists to blind themselves to other data, but the LI-RADS category should be based on imaging features and able to stand on its own, as the radiologist’s estimation of the likelihood of HCC. A clinician’s estimated probability of HCC may differ. While informed by the LI-RADS category, clinicians also incorporate other factors such as circulating biomarkers and the patient’s pre-test probability of developing or having HCC. For example, a radiologist may assign LR-4 based on imaging findings, but a markedly elevated serum AFP level may permit non-invasive diagnosis of HCC with high certainty.
Proceeding further through the layers of diagnostic thinking, the likelihood of HCC, or even a definite diagnosis of HCC, do not directly determine management. Rather, the ultimate management decision follows from a clinical assessment that integrates all available medical information, including patient co-morbidities; patient preference; observation size and location; number, sizes, and LI-RADS categories of additional observations; and eligibility for liver transplantation or other treatment methods. For example, a decision about whether to biopsy may be affected by risk factors such as coagulation disorders, or whether a patient most fears a procedure or a short delay in diagnosis, or whether biopsy confirmation of a small (< 20 mm) HCC would affect priority for liver transplantation. Management after a definite diagnosis of HCC, as communicated by the presence of one or more LR-5 observations, will be decided by a patient’s managing clinician or multidisciplinary team.
Reporting considerations
Reporting is a vital communication tool between a radiologist and a clinician. LI-RADS recommends that up to five individual observations should be described individually, in order to maintain clarity of the report. In cases with greater than five observations, observations may be described in aggregate.
For each individually reported observation, LI-RADS recommends reporting location (e.g., segment or section), size, all major features, ancillary features (if used), change (if any) from the prior, and the final LI-RADS category[6]. Each observation should be assigned an identifying number (e.g., Observation #1), and the designated number should stay the same on all subsequent reports. Additionally, either key image numbers (e.g., series and slice) should be included in the report, and/or the key images should be saved to facilitate accurate identification and longitudinal follow-up of observations. Structured reports are more comprehensive and have greater clarity than free-text style reports, and are generally preferred by referring physicians [11,12,13,14]. Specifically, use of a structured LI-RADS template leads to both standardized description of categories and unequivocal reporting of the presence or absence of major features in nearly 100% of observations [15]. Sample structured reports can be downloaded through the American College of Radiology (ACR) (https://cortex.acr.org/RadsPreview/CaseView.aspx?CaseId=Y9JbzYund5s%3D) [16].
Key concepts/assumptions
For simplicity, we review management options for individual LI-RADS observations, although patients may have multiple observations. In such instances, management is usually governed by the highest category (or most malignant) observation. In this patient population, we assume that multi-phase CT or MRI is performed after a positive HCC surveillance test (ultrasound, elevated alpha fetoprotein), since the value of CT or MRI for surveillance has not been established by prospective studies.
Our management recommendations are general suggestions consistent with the guidelines recommended by the AASLD and LI-RADS, and may not apply in all cases as stated [7].
Management of each category
Negative study
This category indicates that there are no LI-RADS observations on diagnostic quality multi-phase CT or MR imaging. Management recommendation in this category is to return to routine surveillance (which is based on clinical data and surveillance guidelines). An exception to this management recommendation is when the radiologist or referring care provider believes the diagnostic study could be a false-negative exam because an unequivocal abnormality was evident on an antecedent screening study or there is an elevation in AFP. An alternative exam may be considered such as MRI with gadoxetate disodium or contrast-enhanced US.
LI-RADS non-categorizable (LR-NC)
A LI-RADS non-categorizable (LR-NC) category refers to a situation where the range of diagnostic possibilities cannot be meaningfully narrowed (e.g., cannot state whether the observation is more likely to be LR-1/2 or LR-4/5) due to omission of sequences or degradation of image quality. Depending on the reason for degradation of image quality, an alternative modality should be suggested. For example, if motion artifact is severe on MRI, consider recommending CT. Alternatively, immediate repeat imaging or short-term follow-up with modification of sequences with anti-anxiety medications or shorter-term follow-up could be recommended. In Fig. 2, there is a 2.8-cm T1 hypointense lesion identified on non-contrast MRI, and the patient was unable to complete the contrast-enhanced portion of the study. To appropriately categorize the observation and apply LI-RADS, a dedicated multi-phase dynamic enhanced study is required. In this scenario, repeat imaging with technical modification is needed, with either same or different modality. The patient in Fig. 2 returned for repeat imaging using an alternate modality and the lesion was categorized as a LR-5 observation based on multi-phase CT.
A 64-year-old male with HCV cirrhosis. a Non-contrast imaging reveals a 2.8-cm T1 hypointense lesion that is incompletely characterized because patient could not tolerate continuing the dynamic contrast-enhanced portion of the exam and study was categorized a LR- NC. Management guidelines suggest repeat imaging, in this case with dynamic contrast-enhanced CT which demonstrates (b) 2.8 cm lesion with arterial-phase hyperenhancement on arterial-phase imaging and c portal venous phase washout on portal venous phase imaging, and categorized as a LR-5 observation
LR-NC should not be applied if the case is difficult to interpret because of unusual imaging features or the inability to categorize ancillary features.
LI-RADS 1 (LR-1)
LR-1 observations are considered definitely benign, for example, hepatic cysts, hemangiomas, perfusion alterations (arterioportal shunts), hepatic fat deposition/sparing, hypertrophic pseudomass, confluent hepatic fibrosis, focal scar, or complete disappearance of previously seen observation. Perfusion alterations are often wedge-shaped or geographic in appearance and are seen only on the arterial phase, without T2 correlate or portal venous washout, giving the radiologist confidence in categorizing the observation as LR-1. The preferred management option in such cases is the same as LR-negative, return to routine surveillance (typically, 6 months imaging) (Fig. 3).
A 40-year-old female with HCV cirrhosis. Ax SSFSE (image a) demonstrates a 1.5-cm segment VII T2 hyperintense observation that demonstrates progressive centripetal enhancement on arterial-phase sequence (image b) and portal venous phase (image c). Lesion categorized as a LR-1 observation, probable hemangioma. Management recommendation was to return to routine surveillance (6 months)
LI-RADS 2 (LR-2)
LR-2 observations are probably benign including the differential above, a perfusion alteration (arterioportal shunt) or distinctive nodule less than 20 mm without malignant imaging features (i.e., no major features, LR-M features, or ancillary features of malignancy) (Table 1). Figure 4 shows a 1.5-cm segment VII T2 hyperintense non-arterial hyperenhancing observation that demonstrates minimal enhancement on portal venous phase that does not take up contrast on hepatobiliary phase imaging and has been stable for over 1 year. This lesion was categorized LR-2 (probable focal scar). The preferred management in this scenario is to return to routine surveillance (e.g., in 6 months). In some scenarios, alternative imaging at follow-up may be recommended to problem solve. For example, if a lesion is likely to represent a hemangioma but demonstrates atypical features on gadoxetate-enhanced MRI, ECA-MRI could be performed to confirm suspected diagnosis. Alternatively, if a < 2.0 cm nodule is thought to represent a regenerative or siderotic nodule on CT or ECA-MRI, a gadoxetate-enhanced MRI may provide additional characterization by determining if the nodule retains contrast on hepatobiliary phase imaging.
A 52-year-old male with HCV cirrhosis imaged with hepatobiliary contrast agent. Axial arterial phase and T2W FS (a, b) demonstrate a 1.5-cm segment VII T2 hyperintense non-arterial hyperenhancing non-mass-like observation that demonstrates minimal enhancement on portal venous phase (c) and lack of uptake of hepatobiliary contrast on the delayed 20 min hepatobiliary phase (d). This was categorized as LR-2 (probably benign) thought to represent focal fibrosis or scar. Preferred management is return to surveillance (usually 6-month serial imaging). The lesion has been stable for over 1 year
LI-RADS 3 (LR-3)
LR-3 observations have an intermediate probability of malignancy. Management options include follow-up in 3–6 months (Table 2). If the observation is larger (> 2 cm) or if a change in size might alter staging unfavorably, closer follow-up in about 3 months and/or multidisciplinary discussion is warranted (Fig. 5). When short-term follow-up is recommended, radiologists should use their clinical judgment to recommend an appropriate modality/contrast agent for the follow-up exam. Since there is a non-negligible possibility of malignancy (39–40% [8, 17]), the multidisciplinary group may elect to biopsy the observation if the results would change management.
A 71-year-old female with HCV cirrhosis with a history of treated HCC, imaged with hepatobiliary contrast. Stable 2.9 cm segment II/III (a) T1W hyperintense observation on T1 weighted pre-contrast imaging without b arterial hyperenhancement (APHE) or c portal venous enhancement as compared to background liver is unchanged in size since 3 months earlier. The observation is (d) isointense on hepatobiliary phase imaging. This lesion was categorized as LR-3 (intermediate probability for HCC) because of its size, >2 cm, and lack of any major features. 3–6-month follow-up could be obtained. Given the stability over 3 months, conservative management of follow-up in another 3 months may be warranted. Subsequently if stable, follow-up could return to 6 months. Note, a segment VIII lesion has been treated with TACE and is non-viable (LR-Treated Non-viable, pink arrow)
LI-RADS 4 (LR-4)
LR-4 observations have a high probability of being HCC (Table 3). LR-4 observations do not contribute to OPTN staging/MELD exception points. Management choice is individualized and based on transplant/surgical candidacy, co-morbidities, and liver function. Multidisciplinary discussion is recommended to determine individualized management, and may include repeat or alternative imaging modality, biopsy, or presumptive treatment, (Fig. 6). Diagnosis needs to be confirmed for LR-4 observations prior to locoregional therapy if the patient is a transplant candidate.
A 76-year-old female with NASH cirrhosis and a 2.6-cm segment VIII (a) T1 hyperintense observation without arterial hyperenhancement or portal venous washout (b, c), that is (d) hypointense to liver parenchyma on hepatobiliary phase. Lesion categorized as LR-4 observation (high probability for HCC). Multidisciplinary discussion is recommended. Biopsy or short-term follow-up are both treatment options but given the size of the observation, radioembolization (Y90) treatment recommended
LI-RADS 5 (LR-5)
LR-5 observations have 100% probability of being HCC. Presence of non-rim-like arterial-phase hyperenhancement (APHE) and size ≥ 10 mm are required for LR-5 categorization (Fig. 7). The definition of non-rim-like arterial-phase hyperenhancement is provided in detail in the LI-RADS v2018 CT/MRI core and is defined as enhancement unequivocally greater in whole or in part than the liver. The enhancing part must be higher in attenuation or intensity than the surrounding liver in arterial phase. It is important to understand the definition of non-rim-like arterial-phase hyperenhancement to contrast it with rim arterial-phase hyperenhancement, which is part of the inclusion criteria for LI-RADS M category (which will be a category discussed in further detail later in this paper[8]). Table 4 summarizes the v2018 LR-5 diagnostic criteria.
A 41-year-old male, HBV with ruptured HCC. A 7.1-cm segment V/VII observation demonstrates AP hyperenhancement and “washout” (a, b), categorized as LR-5 observation, (definitely HCC, see white arrow). However, there are also multiple subcentimeter HBP hypointense nodules without APHE (c, d, see pink arrows). These nodules lack arterial hyperenhancement, portal venous “washout” appearance, capsule, or threshold growth. The small HBP nodules without APHE are LR-3 observations and management should be dictated by the highest LR categorization, in this case the dominant LR-5 observation
With AASLD unification, a revision to the LR-5 category was made for LI-RADS 2018: observations 10–19 mm in size with non-rim APHE and non-peripheral “washout” are now categorized LR-5, even if not visible on antecedent screening ultrasound. A LR-5 observation with the above features does not meet OPTN Class 5 criteria and therefore, is not eligible for OPTN exception points, which is important point to keep in mind for radiologists practicing in the United States. Otherwise, LI-RADS and OPTN now have identical criteria for HCC.
Of note, LI-RADS version 2018 simplified the definition of “threshold growth” to align with AASLD and OPTN. Threshold growth is now defined as greater than or equal to 50% size increase of a mass within 6 months. As such, observations 10–19 mm in size with non-rim arterial-phase hyperenhancement and threshold growth are considered LR-5 observations and equivalent to OPTN 5A-g category. Observations greater than or equal to 20 mm with non-rim arterial-phase hyperenhancement and one or more of the following: non-peripheral washout, enhancing capsule, or threshold growth are considered LR-5 observations and now equivalent to OPTN 5B or OPTN 5X (depending on size).
A biopsy is usually not needed once an observation is categorized LR-5 unless molecular analysis is needed for determining choice of targeted therapy. However, next steps should be dictated by the patient’s surgical or transplantation candidacy, co-morbidities, and underlying liver disease. For management of patients with LR-5 observations, multidisciplinary discussion is recommended.
LI-RADS M (LR-M)
LR-M observations have a high probability of malignancy, but the imaging features are not specific for HCC (Fig. 8). LR-M observations can demonstrate a targetoid appearance or non-targetoid appearance. Non-targetoid appearances include infiltrative appearance or at least one imaging feature that suggests hepatocellular origin. The differential diagnosis for LR-M includes non-HCC malignancies (e.g., intrahepatic cholangiocarcinoma or metastases) and HCCs with atypical features or combined bi-phenotypic tumors (combine hepatocellular carcinoma-cholangiocarcinoma), see Table 5. Multidisciplinary discussion is recommended to determine individualized management. Biopsy is often needed to determine the malignancy type and direct appropriate therapy.
A 69-year-old male with HCV liver cirrhosis presents with 2.3 cm hepatic observation in segment 8. Arterial-phase images demonstrate rim arterial-phase hyperenhancement (a) with peripheral washout on portal venous phase image (b) and suggestion of progressive enhancement on delayed phase image (c). T2 FS sequence demonstrates mild hyperintensity within the lesion (d), hepatobiliary phase image demonstrates hypointensity of the lesion (e) and there is restricted diffusion in the lesion on high b value diffusion-weighted sequence (f) with suggestion of an adjacent satellite lesion (pink arrow). Due to rim APHE and targetoid dynamic enhancement pattern, this observation was categorized as LR-M, with a differential diagnosis of HCC with atypical imaging features, intrahepatic cholangiocarcinoma, and combined HCC-cholangiocarcinoma. At multidisciplinary discussion, the decision was made to biopsy the lesion, and pathology yielded well-differentiated HCC. Patient subsequently underwent radioembolization of the lesion
LI-RADS TIV (LR-TIV)
LR-TIV indicates a malignant neoplasm within the portal or hepatic venous system and is defined by the unequivocal presence of enhancing soft tissue in a vein, regardless of whether there is an associated parenchymal mass. If LR-TIV is contiguous with targetoid mass, it should be reported as “LR-TIV, may be due to non-HCC malignancy.” If LR-TIV is contiguous with LR-5 mass, it should be reported as “LR-TIV, definitely due to HCC.” In all other instances, this should be reported as “LR-TIV, probably due to HCC.“ This nomenclature is provided in recognition of literature that suggests that TIV may be due to non-HCC malignancies [18, 19]. The management recommendation for LR-TIV is multidisciplinary discussion for consensus management. Contrast-enhanced ultrasound may be useful to differentiate bland thrombus from tumor in vein in questionable cases.
Pathologically confirmed lesions
LI-RADS categories should not be assigned for path-proven lesions. Clinically relevant imaging features should be mentioned in the report and any change since prior should be stated clearly. Confirmation that the imaging observation corresponds to the biopsied lesion and is consistent with pathology-proven diagnosis should be stated in the report. However, if the observation has been sampled and results reveal a non-malignant lesion of hepatocellular origin such as a dysplastic nodule, then the observation should be given a LI-RADS category at follow-up imaging and the pathology diagnosis should be stated along with interval changes. The rationale for this is that sampling error may cause an HCC or combined HCC-cholangiocarcinoma to be misdiagnosed as a non-malignant hepatocellular nodule based on biopsy. Additionally, dysplastic nodules are considered pre-malignant and may transform into early or progressed HCC.
If there is discordance between the pathology report and the imaging observations and/or category, consider review of the histology, imaging, and clinical data with the multidisciplinary team. False-negative biopsies or inconclusive biopsies can occur in up to 19–30% of patients due to lesion size, sampling errors or overlap of pathologic features such as cholangiocarcinoma, scirrhous hepatocellular carcinoma, and combined hepatocellular carcinoma–cholangiocarcinomas, and repeat biopsies may be needed in up to 16% [20, 21]. While management is guided by pathologic diagnosis and stage, multidisciplinary discussion is recommended to discuss treatment options, determine length of follow-up, and resolve discrepancies.
Additional considerations
Global differences
It is important to recognize that there remain global differences in surveillance, diagnosis, and management of HCC. Since 2001 when the European Association for the Study of Liver (EASL) issued their HCC guidelines, at least 20 guidelines have been published worldwide between 2001 and 2017. In a recent review article by Song et al, 18 of these guidelines were reviewed, 8 guidelines from Asia, 5 from Europe, and 5 from the United States of America. 14 of the 18 guidelines clearly describe risk factors and surveillance, but there are discrepancies in the guidelines based on regional differences in disease and other variables. Among risk factors, hepatitis B is the leading cause of HCC in Africa and East Asia, while hepatitis C is the leading risk factor in Europe, Japan, and North America. A combination of ultrasound and measurement of AFP are the most widely used and effective methods for detecting HCC worldwide. However, AFP has been excluded from surveillance and/or diagnostic criteria in guidelines issued by some Western countries, including the 2005 and 2011 versions of the American Association for the Study of Liver Diseases (AASLD) Guidelines, EASL Guidelines, and the National Comprehensive Cancer Network (NCCN) Guidelines. Over time, these regional differences may change. For example, HBV as a cause of HCC is declining, while the importance of non-alcoholic fatty liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH) as risk factors for HCC are on the rise. HCV is now a potentially curable disease, which will reduce its incidence worldwide, over time. Future guidelines should pay attention to these changes and each country should devise its own method of HCC surveillance based on local epidemiology.
Criteria for diagnosis of HCC also vary based on different guidelines. If screening ultrasound detects a nodule, diagnostic criteria for HCC are based on one of the two general pathways, either a size-based pathway or a non-size-based pathway. Worldwide, all of the guidelines conclude that a definitive diagnosis of HCC can be made when dynamic CT/MRI reveals intense arterial uptake of contrast followed by “washout” of contrast.
The updated Japan Society of Hepatology (JSH) guidelines include Gd-EOB-DTPA MRI (gadoxetic acid disodium, a liver-specific contrast agent) as a first-line tool for diagnosis and surveillance of HCC. Because this contrast agent is specifically absorbed by hepatocytes, HCC nodules lacking normal hepatocytes are hypointense, and this helps distinguish tumors from non-tumorous nodules. Worldwide, guidelines differ on diagnostic criteria for HCC when the nodule is hypervascular without definite “washout” of contrast (LR-4 observations). Guidelines also differ on what to consider diagnostic criteria for HCC when the observation is hypovascular mass on the arterial phase (LR-4 observation) [22].
Differences also exist globally with regard to access to liver transplantation. In Asia, living donor liver transplantation is common and makes up 90% of all liver transplants performed. Deceased donor liver transplantation is uncommon due to cultural, religious, and political reasons (although recent trends have noted an increase in cadaver organ donation in certain countries such as China and South Korea). Certain countries such as India face unique challenges in terms of accessibility to liver transplantation, which is currently only available in large private hospitals, and patients who cannot afford the high costs are unable to undergo the procedure. The national cadaveric organ donation rate in India at the moment is very low, only about 0.08 per million population.
The application and selection criteria for transplantation due to HCC also differ in Asia. The most common reason for liver transplantation in Asia in adults has been HCC secondary to hepatitis B, followed by hepatitis B without HCC and HCV-related cirrhosis without HCC. In the Far East, Japan is the only exception where HCV is more common than Hepatitis B [23].
Imaging follow-up and reporting
Imaging follow-up and the decision to treat is based on a patient’s transplantation candidacy and potential for model for end-stage liver disease (MELD) exception points. Once on the transplant list in the West, imaging must be performed to monitor tumor burden every 90 days or more frequently. Patients may be bridged or downstaged to transplantation with directed therapy. Additional important factors influencing the decision to treat observations include liver function and co-morbidities.
As discussed above, in some instances use of an alternative modality as the next step in management may provide additional benefit. For example, if a lesion may represent a vascular shunt (LR-2) versus a tumor, use of MRI with a hepatobiliary contrast agent may help in the differentiation. It is helpful for the radiologists to clearly state if alternative imaging should be performed immediately or at follow-up and the reasoning for the recommended, so the clinician can order the appropriate study and the radiologists reviewing the follow-up study understands the differential.
Multidisciplinary discussion can take the form of formal conference or informal discussion (e.g., radiologist calls clinician and discusses management options informally). However, it is recommended that these discussions and recommendations be documented in the medical record or radiology report to avoid mis-communications [24].
Report content should include description of major features, contributory ancillary and other features, and any relevant change since the prior study. If the patient has a path-proven diagnosis, LI-RADS recommends reporting the observation’s pathologic diagnosis, clinically relevant imaging features, and change since the prior study. Multidisciplinary discussion should include consensus review of histology, imaging, and other clinical data to resolve the discordance.
Conclusion
LI-RADS provides a construct for communicating the relative probability of HCC and malignancy for liver observations. The categories have been iteratively refined as evidence accumulates, user feedback is provided, and expert consensus dictates. Validation of the latest v2018 to define natural history and diagnostic accuracy of different observation categories will help further refine LI-RADS categories and management recommendations, with an anticipated next version release slated for 2021. Additional work is needed to bridge the gaps between different imaging systems in North America and worldwide. The AASLD and LI-RADS unification in v2018 was a major step forward (Tables 6 and 7). However, there remain discrepancies when utilizing LI-RADS in transplant patients due to inconsistencies with OPTN criteria. Further unification with OPTN and other international systems will only strengthen the level of evidence and promote more cohesive literature supporting the imaging diagnosis and subsequent management of HCC.
References
Mittal S, El-Serag HB. Epidemiology of HCC: Consider the Population. J Clin Gastroenterol. 2013;47(0):S2-S6. https://doi.org/10.1097/MCG.0b013e3182872f29
CDC-Liver Cancer. February 2018. https://www.cdc.gov/cancer/liver/index.htm. Accessed April 17, 2018.
Chou R, Cuevas C, Fu R, et al. Imaging Techniques for the Diagnosis of Hepatocellular Carcinoma: A Systematic Review and Meta-analysis. Ann Intern Med. 2015;162(10):697. https://doi.org/10.7326/M14-2509
Chou R, Cuevas C, Fu R, et al. Imaging Techniques for the Diagnosis and Staging of Hepatocellular Carcinoma. Rockville (MD): Agency for Healthcare Research and Quality (US); 2014. http://www.ncbi.nlm.nih.gov/books/NBK254191/. Accessed June 26, 2018.
Hanna RF, Miloushev VZ, Tang A, et al. Comparative 13-year meta-analysis of the sensitivity and positive predictive value of ultrasound, CT, and MRI for detecting hepatocellular carcinoma. Abdom Radiol N Y. 2016;41(1):71-90. https://doi.org/10.1007/s00261-015-0592-8
Elsayes KM, Hooker JC, Agrons MM, et al. 2017 Version of LI-RADS for CT and MR Imaging: An Update. RadioGraphics. 2017;37(7):1994-2017. https://doi.org/10.1148/rg.2017170098
Marrero JA, Kulik LM, Sirlin C, et al. Diagnosis, Staging and Management of Hepatocellular Carcinoma: 2018 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. April 2018. https://doi.org/10.1002/hep.29913
LI-RADS. https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/LI-RADS. Accessed June 26, 2018.
Kambadakone AR, Fung A, Gupta RT, et al. LI-RADS technical requirements for CT, MRI, and contrast-enhanced ultrasound. Abdom Radiol N Y. 2018;43(1):56-74. https://doi.org/10.1007/s00261-017-1325-y
Kielar A, Fowler KJ, Lewis S, et al. Locoregional therapies for hepatocellular carcinoma and the new LI-RADS treatment response algorithm. Abdom Radiol N Y. 2018;43(1):218-230. https://doi.org/10.1007/s00261-017-1281-6
Schwartz LH, Panicek DM, Berk AR, Li Y, Hricak H. Improving communication of diagnostic radiology findings through structured reporting. Radiology. 2011;260(1):174-181. https://doi.org/10.1148/radiol.11101913
Marcovici PA, Taylor GA. Journal Club: Structured radiology reports are more complete and more effective than unstructured reports. AJR Am J Roentgenol. 2014;203(6):1265-1271. https://doi.org/10.2214/AJR.14.12636
Larson DB, Towbin AJ, Pryor RM, Donnelly LF. Improving consistency in radiology reporting through the use of department-wide standardized structured reporting. Radiology. 2013;267(1):240-250. https://doi.org/10.1148/radiol.12121502
Powell DK, Silberzweig JE. State of structured reporting in radiology, a survey. Acad Radiol. 2015;22(2):226-233. https://doi.org/10.1016/j.acra.2014.08.014
Flusberg M, Ganeles J, Ekinci T, et al. Impact of a Structured Report Template on the Quality of CT and MRI Reports for Hepatocellular Carcinoma Diagnosis. J Am Coll Radiol JACR. 2017;14(9):1206-1211. https://doi.org/10.1016/j.jacr.2017.02.050
ACR LI-RADS. https://cortex.acr.org/RadsPreview/CaseView.aspx?CaseId=Y9JbzYund5s%3D. Accessed September 29, 2018.
Chernyak V, Fowler KJ, Kamaya A, et al. Liver Imaging Reporting and Data System (LI-RADS) Version 2018: Imaging of Hepatocellular Carcinoma in At-Risk Patients. Radiology. September 2018:181494. https://doi.org/10.1148/radiol.2018181494
Fraum TJ, Tsai R, Rohe E, et al. Differentiation of Hepatocellular Carcinoma from Other Hepatic Malignancies in Patients at Risk: Diagnostic Performance of the Liver Imaging Reporting and Data System Version 2014. Radiology. 2017;286(1):158-172. https://doi.org/10.1148/radiol.2017170114
Ronot M, Fouque O, Esvan M, Lebigot J, Aubé C, Vilgrain V. Comparison of the accuracy of AASLD and LI-RADS criteria for the non-invasive diagnosis of HCC smaller than 3cm. J Hepatol. 2018;68(4):715-723. https://doi.org/10.1016/j.jhep.2017.12.014
Sherman CB. Utilization and Accuracy of Biopsy in Patients with Hepatocellular Carcinoma in a Community based Setting. https://clinmedjournals.org/articles/jcgt/journal-of-clinical-gastroenterology-and-treatment-jcgt-2-026.php?jid=jcgt. Accessed August 12, 2018.
Forner A, Vilana R, Ayuso C, et al. Diagnosis of hepatic nodules 20 mm or smaller in cirrhosis: Prospective validation of the noninvasive diagnostic criteria for hepatocellular carcinoma. Hepatology. 2008;47(1):97-104. https://doi.org/10.1002/hep.21966
Song P, Cai Y, Tang H, Li C, Huang J. The clinical management of hepatocellular carcinoma worldwide: A concise review and comparison of current guidelines from 2001 to 2017. Biosci Trends. 2017;11(4):389-398. https://doi.org/10.5582/bst.2017.01202
Shukla A, Vadeyar H, Rela M, Shah S. Liver Transplantation: East versus West. J Clin Exp Hepatol. 2013;3(3):243-253. https://doi.org/10.1016/j.jceh.2013.08.004
Practice Parameters for Documentation and Reporting | American College of Radiology. https://www.acr.org/Clinical-Resources/Practice-Parameters-and-Technical-Standards/Practice-Parameters-for-Documentation-and-Reporting. Accessed August 12, 2018.
Author information
Authors and Affiliations
Corresponding author
Additional information
CME activity
This article has been selected as the CME activity for the current month. Please visit https://ce.mayo.edu/node/81590 and follow the instructions to complete this CME activity.
Rights and permissions
About this article
Cite this article
Kamath, A., Roudenko, A., Hecht, E. et al. CT/MR LI-RADS 2018: clinical implications and management recommendations. Abdom Radiol 44, 1306–1322 (2019). https://doi.org/10.1007/s00261-018-1868-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-018-1868-6