Abstract
The vulnerability–stress model is a hypothesis for symptom development in schizophrenia patients who are generally characterized by cardiac autonomic dysfunction. Therefore, measures of heart rate variability (HRV) have been widely used in schizophrenics for assessing altered cardiac autonomic regulations. The goal of this study was to analyze HRV of schizophrenia patients and healthy control subjects with exposure to auditory stimuli. More specifically, this study examines whether schizophrenia patients may exhibit distinctive time and frequency domain parameters of HRV from control subjects during at rest and auditory stimulation periods. Photoplethysmographic signals were used in the analysis of HRV. Nineteen schizophrenic patients and twenty healthy control subjects were examined during rest periods, while exposed to periods of white noise (WN) and relaxing music. Results indicate that HRV in patients was lower than that of control subjects indicating autonomic dysfunction throughout the entire experiment. In comparison with control subjects, patients with schizophrenia exhibited lower high-frequency power and a higher low-frequency to high-frequency ratio. Moreover, while WN stimulus decreased parasympathetic activity in healthy subjects, no significant changes in heart rate and frequency-domain HRV parameters were observed between the auditory stimulation and rest periods in schizophrenia patients. We can conclude that HRV can be used as a sensitive index of emotion-related sympathetic activity in schizophrenia patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
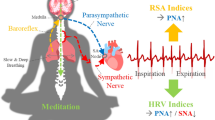
Heart rate variability (HRV) explains the variation in heart beat intervals, and is an important, reliable and noninvasive index for evaluation of autonomic nervous system (ANS) activity [1, 2]. In recent years, HRV analysis has become a powerful tool for assessing the equilibrium between sympathetic and parasympathetic activity of the ANS.
The analysis of HRV is usually obtained from the sequences of R-wave intervals (RR) in electrocardiogram (ECG) signals. Besides, photoplethysmographic (PPG) signals have also been used for HRV analysis in numerous studies [3–5]. PPG is a noninvasive, optical and simple signal to monitor the changes of blood volume in the vessels. Information regarding HRV can be obtained from the PPG signal, which oscillates with the period of the heart beat. Researchers have found that the peak-to-peak (PP) intervals obtained from PPG can be used for HRV analysis instead of the RR intervals of ECG signals of healthy subjects [2–6]. This correlation is not only reported for studies with healthy subjects, but also confirmed for some other conditions. For example, in a sleep study a significant correlation was found in HRV measures between ECG and PPG recordings of the large sample children data [7]. In addition, it has been reported that the PPG based HRV can be used as a tool for large patient populations with increased risk of heart failure [8].
To assess ANS activity, usually the HRV signal is analyzed in the time and frequency domain [9]. Time domain measures of HRV have been used to evaluate the interbeat interval variability. Spectral analysis of sequences of interbeat intervals can be used to assess the distribution of power across different frequency bands. The power spectrum of the HRV signal is divided into a very low frequency (VLF) band, low frequency (LF) band, and high frequency (HF) band. While the LF band (0.04–0.15 Hz) reflects both sympathetic and parasympathetic activities, the HF band (0.15–0.40 Hz) is only related to parasympathetic activity [10]. Therefore, the ratio of the LF to HF power (LF/HF) is an important measure for evaluating sympathovagal balance that reflects the equilibrium between sympathetic and parasympathetic activity of the ANS.
HRV analysis has been widely used to investigate ANS regularization in numerous conditions, including myocardial infarction, cardiac transplantation, tetraplegia, myocardial dysfunction, diabetic neuropathy [10], diabetes mellitus and renal failure [3]. Furthermore, HRV analysis has been used in schizophrenia patients due to the relationship between symptoms of the disorder and cardiac autonomic irregularities [1, 9, 11–13].
Schizophrenia is a complex psychiatric disorder defined by several signs and symptoms, such as abnormalities in motor skills, cognitive impairment, distorted perception and thinking, and difficulty in communication and emotion processing [14]. While strange behavior, false beliefs (delusions), and perceptions in the absence of a stimulus (hallucinations) are classified as positive symptoms, loss of pleasure (anhedonia), disorganized speech, loss of motivation, and lack of interest are common negative symptoms of schizophrenia [15–17]. According to the vulnerability–stress theory, stress by environmental factors affects the time of appearance of symptoms [18]. Although many of these symptoms are related to cognitive dysfunction, some symptom development theories associate autonomic dysfunction with schizophrenia [13].
Since the emotions moderated by ANS, there are some studies that investigate the relationship between symptom development and autonomic dysfunction. Some of them report that altered autonomic regulation is associated with cardiac morbidity in schizophrenia [19, 20]. In some studies, increased heart rate was reported [9, 13, 21, 22], whereas others [23] reported no difference or a decrease in heart rate of schizophrenia patients when compared to healthy subjects [24]. Decreased parasympathetic activity over the cardiovascular system of schizophrenic patients is consistent with research conducted to date [9, 11, 12, 25, 26]. In another study [13], aside from resting conditions, mental arithmetic tests have also been used as a type of stressful stimulus to determine alterations in the cardiac autonomic response of schizophrenia patients. Similarly, decreased parasympathetic activity was reported in schizophrenia patients during this experiment. Therefore, previous studies have used time domain and spectral analysis of HRV to investigate ANS activity changes in patients with schizophrenia. Most of these studies (in rest or stressful conditions) are restricted to ECG based HRV analysis. However, electromagnetic and biologic interference, drift, the large number of wires, and the complex morphology of the technique are reported as some of the problems of the ECG based studies [27]. Moreover, in some experiments that uses standard ambulatory ECG recording systems for heart beat analysis, it has been reported that these devices can be uncomfortable due to the cumbersome wires and adhesive electrode patches [28]. On the other hand, PPG has been reported as a simpler and easier process than analyzing HRV parameters from ECG data according to the results of a previous study [5]. Furthermore, it has been suggested that PPG is easy to take in ambulatory situations due to its requirement for only one wire [27]. Therefore, in this study with ambulatory patients suffering from schizophrenia, the PPG data were acquired for HRV analysis.
In light of previous studies, we hypothesized that patients would have an increased sympathovagal balance and have a reduced HRV response during stimulation periods compared with that of control subjects. Therefore, we intended to investigate the dysfunctions of cardiac autonomic activity in schizophrenia patients using HRV measures at rest and in response to stimulation periods. To our knowledge, no study has yet explored the time and frequency domain measures of HRV signals obtained from the PPG signal in a procedure as specified in this paper. Moreover, according to the results of a study [29] that assess the perceptual detection of schizophrenic patients, it was found that schizophrenic individuals might have impairments in auditory detection and discrimination or in auditory attention as compared to healthy people. In this respect, HRV analysis can provide additional information about cardiac autonomic dysregulation in schizophrenia patients during sequential stimuli with different emotional content. To this end, PPG signals were recorded during acoustic white noise (WN), relaxing Classical Turkish Music (CTM), and restive (no stimulation) periods from all participants.
2 Materials and methods
2.1 Participants
Nineteen schizophrenia patients and twenty healthy subjects, matched for age and gender, participated in the study (Table 1). The diagnosis of schizophrenia was confirmed according to the DSM-IV (Diagnostic and Statistical Manual, Fourth Edition, 2000) criteria [30]. Subjects with diabetes mellitus, hypertension, respiratory diseases, cardiovascular diseases, and co-morbidity were excluded. Both the university and hospital (Bakirköy Mental and Nervous Diseases Training and Research Hospital) ethics committee approved the protocol, and a written informed consent was obtained from all participants before enrollment. Data were taken from all normal hearing subjects (confirmed using audiometry).
2.2 Experimental procedure
The experiments consisted of four periods with stimulation in following order: a pre-stimulation 2 min resting period (R1), a WN period (2 min.), followed by a relaxing music period (2 min), and a 2 min post-stimulation restive baseline (R2) period (Fig. 1). In past studies [31, 32], it was found that stimulation of 2–4 min duration was sufficient to measure physiological parameters, such as fear, stress, happiness and anxiety. Thus, in this study, the duration of each excitation period was selected as 2 min.
The WN, comprised of the sound of rain falling on a river, was used in the control period. According to the reports of previous studies, WN has been used as a neutral stimulus to discriminate cardiovascular responses related to auditory-induced emotions [33]. The music played during the relaxing period was a melodic mode (makam, in Turkish) of CTM that was shown to induce serenity [34]. More specifically, an instrumental clip by Tanburi Cemil Bey named “Çeçen Kızı” that belongs to the Hüseyni makam. We select this mode because of its positive emotional effect on respiratory responses of participants according to the findings of our previous study [35]. All participants listened to these stimuli binaurally through headphones with 75 dB intensity.
2.3 Measurement
The study was conducted in a temperature controlled (23 °C), quiet, and illuminated room in Bakırköy Mental and Nervous Diseases Training and Research Hospital. During the experiments, participants were instructed to sit on a chair without moving and were requested to breathe regularly and keep their eyes closed. PPG data acquisition was performed after the subject had rested for an adaptation period of approximately 3 min. The PPG signals were recorded using the BIOPAC MP150WSW data acquisition system and the associated Acknowledge® software. The TSD200 PPG transducer was strapped on to the middle finger of the non-dominant hand of the subject and connected to a PPG amplifier (PPG100C) of gain 100 and band-pass cut-off frequencies of 0.05 and 10 Hz, with which the blood volume pulse waveform was recorded. Data were recorded for about 8 min under experimental conditions from every subject and were digitized at a sampling rate of 250 Hz.
2.4 Data preprocessing and analysis
The PPG data were analyzed using the MATLAB 7.6® software package. The PPG signal was first low-pass filtered using an 8th order Butterworth filter (cutoff—8 Hz). After recording, the data were high-pass filtered using a fourth-order Butterworth filter with a 10-Hz cutoff frequency in order to eliminate any motion artifact. Occasional ectopies and/or arrhythmic beats were first visually identified using the PP interval shortenings or prolongations and then they were replaced with PP intervals resulting from linear interpolation. Since the most common beat correction method is the linear interpolation which reduces the distortion [36], we preferred to use this technique. Therefore, only normal-to-normal beats were included in the HRV analysis. Then, to detect the systolic peaks of the PPG signal and determine the intervals between them, a min–max detection algorithm was implemented (Fig. 2). Using the peak intervals and related beat numbers obtained, tachograms were plotted. The horizontal axis in the tachogram indicates beat number, which was converted to time for spectral analysis using the relation
where t is time, PP is the peak-to-peak time interval and k is the number of beats (Fig. 3). Then, the PP series obtained was interpolated with a sampling rate of 4 Hz. To remove the quasi DC signal that corresponds to changes in venous pressure [37] in the PPG waveform, a detrending technique based on least-squares polynomial fitting [38] was applied to the resampled data. This method makes calculations about the least squares fit of a straight line to the data and finds the difference between data and the resulting function to remove the linear trend [39].
2.4.1 Time domain HRV analysis
The mean length of all PP intervals (PPint), the standard deviation of all PPints (SDNN), the root mean square differences of successive normal sinus intervals (RMSSD), and the standard deviation of differences between adjacent PPints (SDSD) were computed for each measurement period in the time domain analysis of HRV. While SDNN that is mediated by sympathetic and parasympathetic systems, predicts global HRV, SDSD and RMSSD reflect short-term HRV.
2.4.2 Frequency domain HRV analysis
After detrending and resampling the sequential PPints, Welch’s algorithm was implemented to estimate the power spectral density (PSD). The Welch method is a nonparametric technique and a modified periodogram. The data are divided into several overlapping segments (windows) and then the periodogram is calculated by averaging these periodograms of each data segment. The periodogram can be calculated using the ith modified periodogram of x[n] samples, w[n] windows, and K data segments of length L as [40]
The Welch spectrum is calculated as averaging these resulting periodograms by
The power spectrum of the HRV signal was divided into three bands: VLF (0–0.04 Hz), LF (0.04–0.15 Hz) and HF (0.15–0.5 Hz). The power spectra for the LF band and the HF band were computed by integration of the power spectrum over the related frequency range and were presented in absolute (square milliseconds-ms2) unit in each measurement period. To evaluate the sympathovagal balance indicating the ANS activity, the LF/HF ratio was calculated.
2.5 Statistical analysis
All statistical analyses were performed using the SPSS® (version 20.0) statistical software package. Comparisons of HRV features between the patients and controls in each period were executed using an independent sample Student’s t test. Under the null hypothesis, defined as “no difference in the HRV features of patients and controls”, the data follows a normal distribution. Within-subject comparisons of HRV measures obtained during resting baseline, WN, and CTM stimulation periods were performed a two-way ANOVA with repeated measures on one factor. Due to confidence level of 95 %, results were considered as significant at the level of p < 0.05.
3 Results
In this study, PPG signals were recorded to investigate whether changes in consistent time and frequency domain HRV measures occur at rest and during exposure to auditory stimuli. Therefore, PPG data were recorded and analyzed for both schizophrenia patients and healthy control subjects. Table 2 shows the differences in measures of HRV observed between patients with schizophrenia and control subjects. We found statistically significant differences in time and frequency domain measures of HRV between patients and control subjects. The statistical analysis revealed that there was a significant ‘group’ main effect in the PPint between R1–WN periods (F = 11.72; p = 0.002), WN–CTM periods (F = 13.18; p = 0.001) and CTM–R2 periods (F = 12.80; p = 0.002).
3.1 Baseline heart rate variability
Baseline R1 time domain HRV data of patients and controls are shown in Fig. 4. Schizophrenia patients had a higher heart rate (shorter PPint) and a smaller SDNN and RMSSD during this period as compared to the control subjects’ values. It means they had reduced HRV. The baseline tachograms (top panels) and their corresponding power spectra (bottom panels) of a patient in the schizophrenia group (left) and an individual in the control group (right) are shown in Fig. 5. The patient shows a higher HR, shorter PPint and a decreased HRV at R1 baseline compared to the control subject. Moreover, SDNN, SDSD and RMSSD were lower in the patient group compared to control subjects in the baseline period according to the ANOVA results that show a main effect of ‘group’ on SDNN (F = 9.52; p < 0.05), SDSD (F = 9.58; p < 0.01), and RMSSD (F = 7.87; p < 0.01). On the other hand Fig. 5 shows spectral measures of HRV as LF and HF band powers. While the LF power in schizophrenia patients was not statistically different from that in control subjects (Fig. 6a, left), the HF power was found as significantly smaller in the patients (p < 0.05) at rest (Fig. 6a, right).
Spectral analysis of heart rate variability in restive condition in a healthy subject and schizophrenia patient. Top interbeat interval tachogram of a schizophrenia patient (left) and a healthy individual (right). Bottom corresponding power spectrum obtained from the patient (left) and control subject (right)
Box and whisker plot comparison of frequency domain measures of HRV between schizophrenia and control groups during different experimental periods. The significant differences between groups is illustrated with asterisk symbols (R1 restive 1, WN white noise, CTM Classical Turkish Music, R2 restive 2). Top LF (left) and HF (right) power. Bottom normalize LF (left) and normalize HF (right)
3.2 Heart rate variability during auditory stimuli
The PPint feature of the schizophrenia patients during the whole procedure was significantly lower than that of the control subjects. Auditory stimulation caused an increase in HR (shortening of mean PPint) in both groups as compared to that during restive baseline period. However, the result of main effect of ‘period’ was only significant in the control group in terms of, PPint and SDNN (F = 11.074; p < 0.01). It means that control subjects showed a decrease in PPint and SDNN values from baseline resting state to WN period. In contrast to healthy group, patients did not show a significant difference in these time domain measures between R1 and WN periods. In other sequential periods, the difference between these measures not reached a statistically significant level.
There was not a statistically significant interaction in terms of all time and frequency domain HRV measures between groups and each sequential period. While the control and patient groups showed the greatest HR during the WN exposure, no significant HR change was reported during the WN and CTM periods in schizophrenia patients. Although HR decreased during CTM as compared to the WN period, this difference did not reach a significant level in either the control subjects or schizophrenic patients. The decrease in HR continued in the R2 period for both the control subject and patient groups. However, for both groups, no significant change was reported over the CTM and R2 periods.
While the LF power in schizophrenia patients was not different from that in control subjects (Fig. 6a, left), the HF power was significantly reduced in the patients (p < 0.05) during all periods of the procedure (Fig. 6a, right). Auditory stimulation evoked an increase in LF power and LF/HF ratio from the baseline and a decrease of HF power in the HRV in both groups (p < 0.05). While the LF power increased more during WN than during CTM, the WN evoked a more deceleration of HF power from the baseline as compared to CTM in the control group (Fig. 6a). The LF/HF ratio of healthy subjects was higher during WN than during CTM. In contrast, there were no significant differences in terms of LF, HF, and LF/HF ratio when the different auditory stimuli were heard by the group of schizophrenia patients. The restive period (R2) after stimulation periods caused a significant decrease in LF power in healthy individuals, whereas LF power did not change significantly during the R2 period in the schizophrenia group. Moreover, schizophrenia patients exhibited increased LF/HF ratio as compared to control subjects during both stimulation and restive periods (Fig. 7).
4 Discussion
Schizophrenia is a mental disorder in which some symptom development theories associate autonomic dysfunction with disorder. Altered autonomic function is correlated with higher rates of cardiac disease and morbidity in schizophrenia patients [41]. Therefore, HRV analysis has become a powerful and useful tool in clinical research to assess ANS activities in schizophrenia patients.
To date, HRV of schizophrenia has only been studied under restive and mental arithmetic test conditions [1, 9, 11–13]. Moreover, HRV analysis was mostly performed on ECG signals in these studies. By combining the knowledge about impairment in auditory stimuli discrimination with altered autonomic regulation of schizophrenia patients, we aimed to investigate the HRV parameters during different types of auditory stimuli with emotional content in patients. This research may be one of the first studies that use the HRV measures obtained from PPG signals to investigate vulnerability–stress hypothesis in terms of dysregulations in cardiac autonomic activity of schizophrenia patients at rest and during different auditory stimulation periods. The PPG signals were recorded and analyzed under four sequential periods: restive baseline, WN, sedative CTM and restive baseline. In our study, auditory stimuli were presented in a fixed order as first WN and then a CTM exposure period. To investigate the sedative effect of CTM on HRV responses, we prefer to use the stimuli with this order. In future studies, the effects of the sequence of these periods can be studied.
It can be noted that as easy to measure and low-cost optical technique, PPG has been used instead of ECG to estimate HRV measures [6]. On the other hand, although ambulatory ECG monitoring can be used for HRV analysis, it has some important limitations such as its requirement for many wires. Since these devices have been accepted as uncomfortable, single-lead ambulatory systems can be used for HRV calculations. However, it is not always possible to make a precise diagnosis of the arrhythmia type when single-lead ECGs are used. The requirement for advanced methods or calculations for detection and removal of these abnormal beats makes the HRV calculation procedure hard. In some studies, a high degree of correlation has been reported between HRV measures from the PPG and ECG during spontaneous breathing and during forced metronomic breathing, during tilt table test, in a sleep study and in a study with large patient populations with increased risk of heart failure. However, there are conflicting reports when comparing HRV measures derived from PPG and ECG recordings. The correlation is not found in some studies with ambulatory recordings, exercise and sleep [2, 42]. Generally, this variance between different reports seems to be caused by PPG signal susceptibility to motion artifacts [43]. Therefore, the reduction or elimination of these artifacts using some filters has been reported as an important step when monitoring the cardiovascular system by PPG [44]. In our study, the participants were instructed to sit on a chair without moving and were requested to breathe regularly to eliminate any artifact that occurs due to the movement of the emitter with respect to the skin. Besides, a Butterworth filter was used to eliminate any artifact.
Our study demonstrates that schizophrenia patients had higher HR and shorter PPints and reduced HRV than control subjects during all periods of the procedure. In contrast to some studies which report a decrease [24] or no difference [23] in HR of schizophrenia patients when compared to healthy subjects, we have found an increase in HR of patients. This evidence confirms previous reports on HR increase at rest [9, 21, 22] and during mental arithmetic test condition [13]. This may be a symptom of disorder-related ANS changes [9] or impaired parasympathetic input to the heart.
Frequency domain analyses reveal that the schizophrenia group also exhibited a similar LF power, a significant decrease in HF power and an increase in the LF/HF ratio as compared to healthy subjects during all the periods of the procedure. This is consistent with the results of past studies, which investigate the differences in HRV measures between schizophrenic and healthy subjects [9, 41, 45, 46]. The decrease in HF power and related increase in LF/HF ratio in schizophrenics are suggested as a result of reduced parasympathetic activity in patients with schizophrenia [11]. A recently published study is consisted with the present findings about dysfunctional parasympathetic functioning in schizophrenia patients [46].
Our study demonstrates that HRV is sensitive to differences in experimental periods. Although HR increased during auditory stimulation periods in both groups, changes between the two stimulus periods were not significant for schizophrenia patients. The LF power and the LF/HF ratio increased during stimulation periods as compared to restive periods in both schizophrenia and control groups. However, the LF power was higher during WN exposure than during sedative CTM exposure in the control group. On the other hand, HF power was higher during CTM than WN, but remained the same in both restive and CTM periods. Namely, while WN stimulus increased sympathetic activity more, it caused a reduction in parasympathetic activity in the control subjects. Therefore, the LF/HF ratio was highest during the WN in the control group. This confirms the result of a past study that states the HF power, which is decreased by uncomfortable stimuli, may be sensitive to stress reduction in resting state [47]. In contrast, there were no significant differences in terms of LF, HF, and LF/HF ratio in schizophrenia patients during these two different auditory stimuli periods. This may be related to cardiac autonomic dysfunction or impairments in auditory discrimination of schizophrenia patients [29]. Moreover, it can be noted that the change observed in autonomic activity on HF power is responsible for the increase of HR in stress condition [45].
The WN evoked a shortening of PPints and an increase in LF power when it is compared with the values of baseline in both groups. However, the sedative CTM caused a significant decrease in LF power of the control subjects. It might mean that while the sympathetic inputs to the heart of patients were similar to control subjects, their parasympathetic activity was reduced during both baseline and stimulation periods.
5 Conclusion
In conclusion, the results obtained for time and frequency domain HRV measures support our hypothesis that the variations in cardiac autonomic activity during the restive baseline and other stimulation periods are different between schizophrenia patients and healthy individuals. First, a significant decrease in HF power and an increase in the LF/HF ratio as compared to healthy control subjects during all the periods of the procedure were obtained in schizophrenia patients. Therefore, our results suggest that HF power and LF/HF ratio of HRV are sensitive variables and can be used as a supplementary tool for discriminating between patients with schizophrenia and control subjects.
Second, the patients in our study have a reduced HRV response during stimulation periods compared with control subjects and have an increased sympathovagal balance as a result of the dysregulation of autonomic arousal in schizophrenics. Besides, the increased LF/HF ratio may be suggested as an indirect sign of shift of sympathovagal balance to diminished vagal modulatory activity [48]. This finding is in line with previous studies that report the incidence of coronary heart disease that is related to the reduced HRV and HRV imbalance reflects autonomic dysfunction in clinical investigations [49]. The decreased HF-HRV in some conditions characterized by deficient emotional regulation such as high trait anxiety and negative affect also supports this result [50, 51]. To our knowledge, this is the first study demonstrating reduced HRV in patients with schizophrenia during different stimulation periods with emotional content. Therefore, we can conclude that HRV can be used as a sensitive index of emotion-related sympathetic activity in schizophrenia patients. Third, the reduced parasympathetic activity in schizophrenic patients can be considered as strongly relating the risk factor of cardiac diseases and/or morbidity. The emerging evidence indicates that decreased parasympathetic input to the heart may be related to increased rate of cardiovascular problems in schizophrenia. This result about reductions in HRV of schizophrenics is found in both medicated and medication-free patients. Therefore, it can be suggested that disease-related ANS activity change may be affected by the psychotic symptom severity. However, the precise mechanism of this dysregulation is still unknown because of the complexity of the coordinate system of autonomic activity. To understand the correlation between symptoms and dysregulations in cardiac autonomic activity of schizophrenia patients, further investigations in large groups with other autonomic measures such as respiration, blood resistance and blood pressures will be required.
References
Mohan A, James F, Fazil S, Joseph PK. Design and development of a heart rate variability analyzer. J Med Syst. 2012;36:1365–71.
Charlot K, Cornolo J, et al. Interchangeability between heart rate and photoplethysmography variabilities during sympathetic stimulations. Physiol Meas. 2009;30(12):1357–69.
Yoon Y, Cho JH, Yoon G. Non-constrained blood pressure monitoring using ECG and PPG for personal healthcare. J Med Syst. 2009;33:261–6.
Nitzan M, Babchenko A, et al. The variability of the photoplethysmographic signal a potential method for the evaluation of the autonomic nervous system. Physiol Meas. 1998;19(1):93–102.
Selvaraj N, Jaryal A, et al. Assessment of heart rate variability derived from finger-tip photoplethysmography as compared to electrocardiography. J Med Eng Technol. 2008;32(6):479–84.
Lu S, Zhao H, et al. Can photoplethysmography variability serve as an alternative approach to obtain heart rate variability information? J Clin Monit Comput. 2008;22(1):23–9.
Dehkordi P, Garde A, et al. Pulse rate variability compared with heart rate variability in children with and without sleep disordered breathing. Conf Proc IEEE Eng Med Biol Soc. 2013:6563–6. doi:10.1109/EMBC.2013.6611059.
Srinivas K, Reddy LRG. Detecting congestive heart failure using heart rate sequential trend analysis plot. Int J Eng Sci Technol. 2010;2(12):7329–34.
Bar KJ, Letzsch A, et al. Loss of efferent vagal activity in acute schizophrenia. J Psychiatr Res. 2005;39(5):519–27.
Anonymous. Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur Heart J. 1996;17(3):354–81.
Chang JS, Yoo CS, et al. Differential pattern of heart rate variability in patients with schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2009;33(6):991–5.
Chang JS, Yoo CS, et al. Changes in heart rate dynamics of patients with schizophrenia treated with risperidone. Prog Neuropsychopharmacol Biol Psychiatry. 2010;34(6):924–9.
Castro MN, Vigo DE, et al. Heart rate variability response to mental arithmetic stress in patients with schizophrenia: autonomic response to stress in schizophrenia. Schizophr Res. 2008;99(1–3):294–303.
Tandon R, Nasrallah HA, et al. Schizophrenia, “just the facts” 4. Clinical features and conceptualization. Schizophr Res. 2009;110(1–3):1–23.
Mueser KT, McGurk SR. Schizophrenia. Lancet. 2004;363(9426):2063–72.
Raghavendra BS, Dutt DN, et al. Complexity analysis of EEG in patients with schizophrenia using fractal dimension. Physiol Meas. 2009;30(8):795–808.
Cohen AS, Alpert M, et al. Computerized measurement of negative symptoms in schizophrenia. J Psychiatr Res. 2008;42:827–36.
Liu SK, Hsieh MH, et al. Re-examining sustained attention deficits as vulnerability indicators for schizophrenia. J Psychiatr Res. 2006;40:613–21.
Jindal R, MacKenzie EM, et al. Cardiac risk and schizophrenia. J Psychiatry Neurosci. 2005;30(6):393–5.
Mujica-Parodi LR, Yeragani V, et al. Nonlinear complexity and spectral analyses of heart rate variability in medicated and unmedicated patients with schizophrenia. Neuropsychobiology. 2005;51(1):10–5.
Rechlin T, Claus D, et al. Heart rate variability in schizophrenic patients and changes of autonomic heart rate parameters during treatment with clozapine. Biol Psychiatry. 1994;35(11):888–92.
Zahn TP, Jacobsen LK, et al. Autonomic nervous system markers of psychopathology in childhood-onset schizophrenia. Arch Gen Psychiatry. 1997;54(10):904–12.
Nielsen BM, Mehlsen J, et al. Altered balance in the autonomic nervous system in schizophrenic patients. Clin Physiol. 1988;8(2):193–9.
Dykman RA, Reese WG, et al. Autonomic responses in psychiatric patients. Ann N Y Acad Sci. 1968;147(7):239–303.
Toichi M, Kubota Y, et al. The influence of psychotic states on the autonomic nervous system in schizophrenia. Int J Psychophysiol. 1999;31(2):147–54.
Hempel RJ, Tulen JH, et al. Cardiovascular variability during treatment with haloperidol, olanzapine or risperidone in recent-onset schizophrenia. J Psychopharmacol. 2009;23(6):697–707.
Bolanos M, Nazeran H, et al. Comparison of heart rate variability signal features derived from electrocardiography and photoplethysmography in healthy individuals. Conf Proc IEEE Eng Med Biol Soc. 2006;1:4289–94.
Poh MZ, Swenson NC, Picard RW. Motion-tolerant magnetic earring sensor and wireless earpiece for wearable photoplethysmography. IEEE Trans Inf Technol Biomed. 2010;14:786–94.
Li CS, Chen MC, et al. Altered performance of schizophrenia patients in an auditory detection and discrimination task: exploring the ‘self-monitoring’ model of hallucination. Schizophr Res. 2002;55(1–2):115–28.
Falkum E, Pedersen G, et al. Diagnostic and statistical manual of mental disorders, fourth edition, paranoid personality disorder diagnosis: a unitary or a two-dimensional construct? Compr Psychiatry. 2009;50(6):533–41.
Pecchinenda A, Smith CA. The affective significance of skin conductance activity during a difficult problem-solving task. Cogn Emot. 1996;10(5):481–503.
Rani P, Liu CC, et al. An empirical study of machine learning techniques for affect recognition in human–robot interaction. Pattern Anal Appl. 2006;9(1):58–69.
Nyclicek I, Thayer JF, Van Doornen LJP. Cardiorespiratory differentiation of musically-induced emotions. J Psychophysiol. 1997;11:304–21.
Somakcı P. Türklerde Müzikle Tedavi. Sos Bilim Enst Derg. 2003;2:131–40 (Turkish).
Akdemir Akar S, Kara S, Bilgiç V. Respiratory variability during different auditory stimulation periods in schizophrenia patients. Methods Inf Med. 2012;51(1):29–38.
Brennan M, Palaniswami M, Kamen P. A new model-based ectopic beat correction algorithm for heart rate variability. In: Proceedings of 23rd annual international conference of the IEEE engineering in medicine and biology society, vol 1–4, 2001;23. p. 567–70.
Murthy VS, Ramamoorthy S, et al. Analysis of photoplethysmographic signals of cardiovascular patients. In: Proceedings of the 23rd annual international conference of the IEEE engineering in medicine and biology society, vol 1–4, 2001;23. p. 2204–07.
The Mathworks, Inc., Signal Processing ToolboxTM User’s Guide, R2014.
Alkan A, Kiymik MK. Comparison of AR and Welch methods in epileptic seizure detection. J Med Syst. 2006;30:413–9.
Hennekens CH, Hennekens AR, et al. Schizophrenia and increased risks of cardiovascular disease. Am Heart J. 2005;150(6):1115–21.
Boettger S, Hoyer D, et al. Altered diurnal autonomic variation and reduced vagal information flow in acute schizophrenia. Clin Neurophysiol. 2006;117(12):2715–22.
Khandoker AH, Karmakar CK, Palaniswami M. Comparison of pulse rate variability with heart rate variability during obstructive sleep apnea. Med Eng Phys. 2011;33:204–9.
Lu G, Yang F. Limitations of oximetry to measure heart rate variability measures. Cardiovasc Eng. 2009;9:119–25.
Han H, Kim J. Artifacts in wearable photoplethysmographs during daily life motions and their reduction with least mean square based active noise cancellation method. Comput Biol Med. 2012;42:387–93.
Hempel RJ, Tulen JH, et al. Physiological responsivity to emotional pictures in schizophrenia. J Psychiatr Res. 2005;39:509–18.
Moon E, Lee SH, Kim DH, Hwang B. Comparative study of heart rate variability in patients with schizophrenia, bipolar disorder, post-traumatic stress disorder, or major depressive disorder. Clin Psychopharmacol Neurosci. 2013;11(3):137–43.
Iwanaga M, Kobayashi A, et al. Heart rate variability with repetitive exposure to music. Biol Psychol. 2005;70(1):61–6.
Milicevic G. Low to high frequency ratio of heart rate variability spectra fails to describe sympatho-vagal balance in cardiac patients. Coll Antropol. 2005;1:295–300.
Chevalier G, Sinatra S. Emotional stress, heart rate variability, grounding, and improved autonomic tone: clinical applications. Integr Med Clin J. 2011;10(3):16–21.
Mujica-Parodi LR, Korgaonkar M, Ravindranath B, Greenberg T, Tomasi D, Wagshul M, et al. Limbic dysregulation is associated with lowered heart rate variability and increased trait anxiety in healthy adults. Hum Brain Mapp. 2009;30:47–58.
Bleil ME, Gianaros PJ, Jennings JR, Flory JD, Manuck SB. Trait negative affect: toward an integrated model of understanding psychological risk for impairment in cardiac autonomic function. Psychosom Med. 2008;70:328–37.
Acknowledgments
This study has been financially supported by the Fatih University Research and Development Management Office under Project Number P50060901.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Akar, S.A., Kara, S., Latifoğlu, F. et al. Analysis of heart rate variability during auditory stimulation periods in patients with schizophrenia. J Clin Monit Comput 29, 153–162 (2015). https://doi.org/10.1007/s10877-014-9580-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-014-9580-8