Abstract
Purpose
This study aimed to compare the effects of virtual reality (VR) training and resistance exercises training on lymphedema symptom severity as well as physical functioning and QoL in women with breast cancer–related lymphedema (BCRL).
Methods
In a single blinded randomized trial, women diagnosed with unilateral BCRL were randomly divided into two groups: the Xbox Kinect group received VR Kinect-based games (n = 30) and resistance exercise group received resistance training (n = 30). In addition, both groups received complex decongestive physiotherapy (manual lymphatic drainage, compression bandages, skin care, and exercises). The intervention was conducted five sessions per week for 8 weeks. The outcome measures included excessive limb volume, visual analogue scale (VAS), the Disability of the Arm, Shoulder, and Hand (DASH) questionnaire, shoulder range of motion (ROM), shoulder muscles strength, hand grip strength, and Study Short-Form (SF-36). The outcomes were evaluated pre and post intervention (week 8).
Results
Statistical significant differences were recorded in VAS (pain intensity), DASH, shoulder ROM (p < 0.001), bodily pain (p = 0.002), general health (p < 0.001), and vitality (p = 0.006) in favor of the Xbox Kinect group. However, there were statistically significant differences in shoulder flexion strength (p = 0.002), external rotation strength (p = 0.004), and abduction strength and handgrip strength (p < 0.001) in favor of the resistance exercise group.
Conclusions
The VR training was superior to resistance exercises training in BCRL management. The empirical findings support the VR as a new effective and encouraging intervention modality which can assist in improving physical functioning and quality of life in women with BCRL.
Trial registration
This study is retrospectively registered at ClinicalTrials.gov (ID: NCT04724356).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer–related lymphedema (BCRL) is a specific type of secondary lymphedema in 14 to 54% of breast cancer survivors following axillary surgical interventions and/or irradiation [1]. Women with BCRL exhibit considerable pain, heaviness, tightness, numbness, and other problems such as cellulitis, infections, loss of muscle strength, and lymphangiosarcoma in the affected arm; as a result, significant deterioration of physical function has been documented in both fine and gross motor skills [2, 3]. Furthermore, these patients showed maladjustment to disease as well as significantly increased psychosocial disorders such as distress, anxiety, and depression [4]. These variables influence all aspects of quality of life (QoL), including home, work, social and recreational relationships, and personal care functions [3, 5].
Clinical guidelines for BCRL suggest that women should minimize daily physical activity and restrict vigorous exercise as it may intensify lymphedema [6, 7]. This suggestion, therefore, induces diminished physical activity and functional decline, and decreased range of motion (ROM), muscle strength, and QoL [8]. The American Cancer Society, on the other hand, recommends primary treatment to eliminate or minimize lymphedema risk, which includes use of personalized exercise rehabilitation [9], and recent evidence supports exercise as safe and effective for BCRL [10,11,12].
In rehabilitation, the use of technology is growing progressively, as emerging technologies are further encouraging patients to engage in their own daily treatment and traditional programs. The virtual reality (VR) training has revealed positive outcomes for the functional development of the upper limbs and offers the ability to perform daily life tasks. Xbox Kinect-based training offers interactive user technology that makes multiple therapeutic options easy to accomplish and offers more contributions to the existing rehabilitation programs [13, 14]. The VR programs are being used in different diseases to enhance upper limb performance and function [15,16,17,18].
The majority of research regarding resistance exercises (RE) in BCRL has concentrated on the safety of exercises, exhibiting that exercises do not accelerate or intensify lymphedema regardless of alterations in the intensity of exercises [19,20,21]. Few trials have demonstrated that RE diminish the lymphedema volume [22]. However, there is a paucity of trials to study the efficacy of VR or compare the impacts of the different types of exercises in women with BCRL.
Acquiring more knowledge about how each exercise setting influences lymphedema, in addition to other health-related results, will allow better prescription of exercise guidance related to BCRL. So, the aim of this trial was to compare the impacts of Xbox Kinect training and RE training on lymphedema symptom severity as well as physical functioning and QoL in women with BCRL.
Methods
Design and setting
A single blinded, randomized trial was conducted between January 2019 and May 2020. All women were recruited from the outpatient clinics at the National Cancer Institute and El-Sahel Teaching Hospital, Cairo, Egypt. The intervention was received at an outpatient rehabilitation center, and all women signed an informed consent. Approval for this trial was gained from the Research Ethics Committee of Physical Therapy Faculty in Cairo University and was conducted in compliance with the Declaration of Helsinki. This trial was registered in ClinicalTrials.gov (ID: NCT04724356).
Participants
Females with BCRL, age more than 30 years old, were selected to engage in this trial. Females had a histological finding of breast cancer at least 1 year preceding the experiment, a clinical diagnosis of unilateral BCRL, and attained medical clearance from their medical oncologists or surgeons. Lymphedema was clinically diagnosed in case of presence of 5% discrepancy at least in volume or circumference between limbs [23]. Females were excluded in case of unstable lymphedema (getting antibiotics for infection in the last 3 months), and a neurological, musculoskeletal, and/or cardiovascular disorder that could inhibit them from exercising. All females were informed to keep up their levels of physical activities, diet, and lymphedema self-care all throughout the treatment time frame.
Sample size and randomization
G*Power (version 3.1.9.2; Germany) was used (F tests-MANOVA: repeated measures, within-between interaction) to calculate the minimal estimated sample size before the start of study, with 0.4 effect size, 80% power analysis, and a two-sided 5% alpha level. Therefore, fifty-two patients were estimated as a minimal sample size. The sample size was increased by 20% for a possible drop out. This effect size was calculated from a pilot study of 10 participants (5 in each group). Computer-generated block randomization method was used to randomly assign the participants equally either to Xbox Kinect group (n = 30) or RE group (n = 30). Randomization was conducted by a therapist who was not involved in data gathering procedures. The block size was 4 to minimize inter-group variability and avoid selection bias. Participants’ allocation was concealed through using sealed, sequentially numbered opaque envelopes. Once the therapist unfolded the envelope, the treatment procedures were conducted depending on group distribution. A blinded therapist to group allocation collected the outcome measures at baseline and at the 8th week after treatment.
Intervention
The intervention was conducted once per day, 5 days a week, over 8 weeks. Small groups of 1 to 4 women received the intervention session at a time, supervised by qualified physiotherapists. Both groups received complex decongestive physiotherapy.
Complex decongestive physiotherapy included manual lymphatic drainage, compression therapy, skin care, and exercises. Földi method was used for the conduction of manual lymphatic drainage and accompanied with daily multilayer short stretching bandage. Patients were instructed to keep the bandage on during exercising. The remedial exercises were conducted as follows with breathing exercises in between: large joint mobilization (5 min with moderate speed); mobilization of shoulder girdle with scapular protraction, retraction, and depression; extension of shoulder; flexion and extension of elbow and wrist; ball squeezing; and stretching of both trapezius and pectoralis muscles [24].
In the Xbox Kinect group, the games were analyzed in order to identify the fictional and technical features of the games and movement patterns required during the games. Our team has defined the therapeutic objectives and fictional features of Xbox Kinect games. The “Macarena” dance typically consisting of upper extremity activities was given as warm-up (5 min) to reduce joint stiffness. Other Xbox Kinect games (darts, bowling, boxing, table tennis, fruit ninja, and beach volleyball) were chosen as per the participant’s performance level. All games depend on active motions of the upper limb including all movements of shoulder joint, elbow flexion and extension, and forearm supination and pronation, and all movements of the wrist and fingers. Within all games, specific adjustments of the games were done including increase or decrease of execution time or adding additional levels with more difficulty. Prior to first session, participants were asked to imitate the act of the avatar shown on the screen just like mirror image. The more the motions of the participants were similar to the avatar’s behavior in fluency, velocity, and angle, the greater the score. Then, verbal explanation and instructions of the game were given, and the participants were asked to complete a round of each game as an introduction; after the game started, no hints were given. A technical guideline was given for each game.
In the RE group, the participants performed stretching exercises then RE using dumbbells in the form of seated rows, pulling down of latissimus dorsi, one arm bent over row, biceps brachii curl, bench press, and extension of triceps. These exercises were conducted at 50 to 60% of their estimated one repetition-maximum, 2 sets of 10 to 12 repetitions for each one; a 2-min rest in between sets was allowed; and repetition of exercises was done with gradual increment of weight (5 to 10%) when patients finished 3 sets of 12 repetitions without any complaint [22].
Outcome measurements
The outcome measures included lymphedema symptom severity, physical function, and QoL. The lymphedema symptom severity was assessed using limb volume measurement; visual analogue scale (VAS); and the Disability of the Arm, Shoulder, and Hand (DASH) questionnaire. Physical function assessment includes shoulder ROM, muscle strength, and hand grip strength. The QoL was assessed by the Medical Outcomes Study Short-Form (SF-36).
Limb volume measurement circumference measurements of the extremity volume were done by using an inelastic tape and were started only distal to the metacarpophalangeal joints and measured at 4-cm stretches up to the arm until the axilla base. A mean of two measurements was taken; circumferential measurements intra- and inter-rater reliability were ICC = 0.998 and 0.997, respectively. Standard errors of measurements were 0.13 cm (0.5%) for intra-rater assessment and 0.17 cm (0.7%) for inter-rater assessment of the forearm [25]. The extremity volume was estimated depending on the frustum equation which yielded excellent inter- and intra-observer reproducibility (0.97 and 0.98, respectively) in comparison to water displacement [26], and the excess limb volume (ELV) and percent of ELV were calculated.
The VAS is a reliable scale (ICC = 0.97). It was utilized to measure tightness, heaviness, and pain severity; this scale consists of a 100-mm line (10 cm), where a score zero indicates no pain or discomfort, and a score of ten indicates severe pain or discomfort [27].
The DASH was used to assess disorders and measure disability of the upper limb and monitor change and function over time. The Arabic version of this questionnaire is considered a simple validated (r = 0.94) and reliable (r = 0.97) assessment tool. The higher the scores, the higher the symptom severity [28].
Digital goniometer is a reliable measurement (r > 0.84) used to assess active shoulder flexion and abduction ROM in supine position with elbow extension, while external rotation measurement was done in sitting position. All measurement was conducted three times, and the mean of the three measurements was recorded [29, 30].
A handheld dynamometer (J Tech Commender Muscle Tester, Salt Lake City, UT, USA) has a good validity (r = 0.81); it was used to assess shoulder flexion, abduction, and external rotation muscle strength in the lymph edematous limb through maximum isometric muscle contraction that was recorded in kilograms. All estimations were conducted three times, and the mean of the three estimations was recorded [31].
Hand grip strength was measured by the Saehan “SH5001” hand dynamometer in kilograms. Measurement was conducted in the defined position by the American Society of Hand Therapists. The measurement was conducted three times with a 1-min interval, and the mean of the three estimations was recorded. The inter-rater reliability of handgrip using the dynamometer was ICC = 0.98 [32].
The SF-36 was utilized for evaluation of health-related QoL. The inter-rater reliability was excellent (ICC = 0.98) and Cronbach alpha coefficient was 0.94. It includes physical functioning, role physical, general health, vitality, bodily pain, mental health, role emotional, and social functioning [33].
Statistical analysis
SPSS software for Windows, version 25.0 (Armonk, NY, USA), was used to conduct the statistical analysis. It was done in accordance to intention to treat analysis with multiple imputation models for the missing data from the 8 weeks after intervention. Calculation of means, standard deviations, counts, and percentages for each group was done prior to the study and after 8 weeks. Shapiro–Wilk’s test was used for testing the normal distribution of data. Differences of the combined outcome measures between both groups were detected by 2-way mixed-model multivariate analyses of variance (MANOVA). The F value was utilized according to Wilks’ lambda, and when the MANOVA demonstrated a statistical effect (p < 0.05), post intervention univariate ANOVAs were conducted by Bonferroni-adjusted p-values to avoid potential type I error.
Results
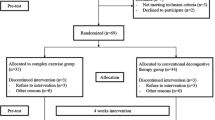
The patients’ flow diagram through the trial is illustrated in Fig. 1. Sixty participants met the inclusion criteria and underwent pre-intervention evaluation at baseline. Tow participants from the RE group were lost at week 8, and their missing data were replaced with multiple imputation model. The demographic data and clinical characteristics of participants are shown in Table 1.
The Shapiro-Wilks test for normality showed that the measured variables were normally distributed (p > 0.05). Two-way mixed design MANOVA was conducted to evaluate the difference between patients in both groups in the amount of change in their scores on the combined outcome measures. Statistically significant multivariate effect was found for the main effects of groups, Wilk’s A = 0.24, F(21,38) = 5.61, p < 0.001, ƞ2 = 0.76; for time, Wilk’s A = 0.002, F(21,38) = 854.35, p < 0.001, ƞ2 = 0.99; and for the groups and time interaction, Wilk’s A = 0.04, F(21,38) = 48.73, p < 0.001, ƞ2 = 0.96.
Post intervention univariate ANOVAs demonstrate statistically significant change for ELV, F(1,58) = 1.44, p = 0.24, ƞ2 = 0.02; for percentage of ELV, F(1,58) = 0.12, p = 0.73, ƞ2 = 0.002; for VAS-pain, F(1,58) = 102.0, p < 0.001, ƞ2 = 0.64; for VAS-heaviness, F(1,58) = 3.28, p = 0.08, ƞ2 = 0.05; for VAS-tightness, F(1,58) = 2.51, p = 0.12, ƞ2 = 0.04; for DASH, F(1,58) = 15.4, p < 0.001, ƞ2 = 0.21; for flexion ROM, F(1,58) = 64.1, p < 0.001, ƞ2 = 0.52; for abduction ROM, F(1,58) = 224, p < 0.001, ƞ2 = 0.79; for external rotation ROM, F(1,58) = 68.9, p < 0.001, ƞ2 = 0.54; for flexion strength, F(1,58) = 44.0, p < 0.001, ƞ2 = 0.43; for abduction strength, F(1,58) = 36.7, p < 0.001, ƞ2 = 0.39; for external rotation strength, F(1,58) = 16.9, p < 0.001, ƞ2 = 0.23; for handgrip strength, F(1,58) = 50.8, p < 0.001, ƞ2 = 0.47; for physical functioning, F(1,58) = 2.78, p = 0.1, ƞ2 = 0.05; for role physical, F(1,58) = 0.47, p = 0.5, ƞ2 = 0.01; for bodily pain, F(1,58) = 31.4, p < 0.001, ƞ2 = 0.35; for general health, F(1,58) = 97.7, p < 0.001, ƞ2 = 0.63; for vitality, F(1,58) = 205.0, p < 0.001, ƞ2 = 0.78; for social functioning, F(1,58) = 2.07, p = 0.16, ƞ2 = 0.03; for role emotional, F(1,58) = 0.64, p = 0.16, ƞ2 = 0.01; and for mental health, F(1,58) = 1.55, p = 0.22, ƞ2 = 0.03.
After 8 weeks of intervention, statistically significant differences were recorded in VAS (pain intensity only); DASH (p < 0.001); ROM of shoulder flexion, abduction, external rotation (p < 0.001); and some domains in SF 36 scale as: bodily pain (p = 0.002), general health (p < 0.001), and vitality (p = 0.006) in favor of the Xbox Kinect group. However, there were statistically significant differences in strength of shoulder flexion (p = 0.002), abduction (p < 0.001), external rotation (p = 0.004), and handgrip strength (p < 0.001) in favor of the RE group as in Table 2. Regarding effects within each group, statistically significant improvements were recorded in all measurements after the intervention compared with that of the baseline in each group (p < 0.001) as in Table 3.
Discussion
This study was designed to compare the effects of Xbox Kinect training and RE training on lymphedema symptom severity as well as physical functioning and QoL in women with BCRL. Our results showed a statistically significant improvement in symptom severity (pain intensity (VAS) and DASH scores), as well as physical functioning (ROM of shoulder flexion, abduction, and external rotation), and QoL (bodily pain, general health, and vitality) in favor of the Xbox Kinect group. On the contrary, the RE group achieved a statistically significant improvement in physical functioning as strength of shoulder flexion, abduction, and external rotation and handgrip strength. No lymphedema exacerbation or adverse effects were recorded during the study.
Fear of movement and pain in lymph edematous limb are considered one of the main causes that participate in upper limb dysfunction and limitation of ROM [2]. In this trial, the results showed the decrease in pain intensity (VAS) and significant improvement in shoulder ROM in the Xbox Kinect group. A possible explanation for this might be that one of the several advantages of the VR is the games of Xbox Kinect which have the simplicity in interaction and the ability of pain distraction which in turn enable and encourage the patients to participate and perform more normal motion [34,35,36]. This study coincides with Chirico et al. [37] about the efficacy and ability of VR to transfer the participant to a different world that captures the participant’s attention with less awareness of pain signal process; hence, the study supposes that most of participants’ concentration and interest were on the selected screenplay path, which introduced emotions of jocosity and excitation.
The participants accomplished an average of 139° shoulder flexion ROM using Xbox Kinect, which equaled or exceeded the reported shoulder ROM for hand combing (75–102°) and high extension (111–142°). [38] In spite of the fact that the utilization of Xbox Kinect does not symbolize training for a particular task, this trial can afford objective data of the gaming needs of Kinect, and stimulate ROM similar to that required for prevalent functional assignments. Women with BCRL might exhibit diminishing in their activities of daily living at home and work environment; also, their social activities are restricted considering diminished confidence [2, 3] In this study, the improvement in the activities of daily living regarding the DASH scores in the Xbox Kinect group is in line with other studies [10, 19,20,21, 39], as the Xbox Kinect training affords enriched and more entertaining and competitive environment that breaks the barrier of movement scare and allows participants to be interested in engaging in many video games and interacting with the system in a 3D environment, where they perform multiple movement combinations without the need of an attached device or a controller [15,16,17,18].
Moreover, the participants wished to continue, although finishing the training, reflecting the prominent role of VR in proceeding to the rehabilitation easily, achieving the target outcomes and improving activities of daily living which in turn improve general health and arm disability. According to our knowledge, no experiments have been evaluating the effect of VR in the management of BCRL. However, Kinect-based VR might be preferred over other modalities due to its effect in increasing upper extremity function, activity performance, and shoulder ROM, as in burn [14], breast cancer patients [15, 16], neurodegenerative disorders [17], and hemiplegia [18].
Women in the Xbox Kinect group demonstrated higher statistical improvement of QoL for bodily pain, general health, and vitality, compared to the other groups. This study reported that the Xbox Kinect is a therapy that participates in the diminishing of symptom severity and improvement of physical function which are translated into improvement in different domains of QoL; more studies are needed to examine this hypothesis. Consistent with previous research (15, 34–36), VR could ameliorate the emotional, cognitive, and physical health of cancer patients. Also, VR interventions demonstrated significant management of several cancer-related symptoms including fatigue, nervousness, pain, and psychological dysfunctions.
The RE group achieved higher statistical results only in muscle strength, and this result may be explained by the fact that RE induces large physiological changes inside skeletal muscles involving contractile and/or non-contractile components of the muscles. During mechanical stress, disturbance of myofibers and extracellular matrix occurs causing stimulation of protein synthesis, which in turn induces muscle growth through increasing the number of sarcomeres leading to increment of both pennation angle and fascicle length, and hence muscle enlargement [40].
Results from this trial shows that both groups decrease BCRL symptom severity and these are lined with other studies that have used various types of physical exercise [22, 41,42,43]. Another perspective worth noting is the exercise frequency in these trials [22, 41,42,43] that included nearly daily exercise sessions or only 5 weekly sessions as in this study; subsequently, the exercises’ frequency instead of the length of an exercise session or mode of exercise is a significant factor to be considered during planning exercise rehabilitation programs for patients with BCRL.
The fundamental mechanisms behind the utilization of exercise training and decongestive physiotherapy to diminish lymphedema size and severity are obscure; exercising can induce muscle pumping action of venous and lymphatic fluid and lymphatic vessel constriction which in turn increases lymphatic drainage and venous return; additionally, stretching exercises keep the muscles flexible, minimize tissue contracture, and subsequently reduce occlusion of blood and lymphatic vessels [24, 44], and diminish the pressure on free nerve endings with consequent amelioration of pain sensation and tightness of neighboring tissues [44]. Utilizing a pressure garment with exercises makes counterforce that assists in lymphatic drainage and minimizes capillary permeability influenced by vascular tension [45].
Explanation of the results must take into consideration many limitations; the fundamental constraint of this trial was absence of control group that would have permitted evaluation of expected bias because of accompanying lymphedema intervention impacts. The generally little sample size prohibits sub-group analyses needed to analyze if the reaction to the exercises varied by lymphedema severity. The lack of blinding during exercise sessions is another limitation of this study. Moreover, assessment of extremity volume via circumference technique only is also another restriction; nonetheless, it could not identify alterations in intra/extracellular tissue fluid as a result of intervention; hence, further studies, with different non-invasive assessment modalities, are recommended.
Conclusion
The Xbox Kinect revealed higher significant improvements in pain intensity and shoulder ROM, and hence improved the patients’ activities of daily living and QoL and motivated more social and activity interaction. The Xbox Kinect is a new efficient and encouraging intervention modality that should be introduced in the rehabilitation program. The results of this study suggest that at least in the clinical setting, the prescription of exercise mode can be individualized toward improving specific physiological concerns, without adversely affecting lymphedema.
Data availability
This manuscript is an honest, accurate, and transparent account of the study being reported; no important aspects of the study have been omitted; and any discrepancies from the study as planned have been explained.
Code availability
Not applicable.
Abbreviations
- BCRL:
-
Breast cancer–related lymphedema
- QoL:
-
Quality of life
- ROM:
-
Range of motion
- RE:
-
Resistance exercise
- SF-36:
-
Study Short-Form
- DASH:
-
The Disability of the Arm, Shoulder, and Hand questionnaire
- VR:
-
Virtual reality
- VAS:
-
Visual analogue scale
References
Vicini F, Shah C, Arthur D (2016) The increasing role of lymphedema screening, diagnosis and management as part of evidence-based guidelines for breast cancer care. Breast J 22(3):358–359. https://doi.org/10.1111/tbj.12586
Hayes S, Rye S, Battistutta D, Newman B (2010) Prevalence of upper-body symptoms following breast cancer and its relationship with upper-body function and lymphedema. Lymphology 43(4):178–187
Morgan PA, Franks PJ, Moffatt CJ (2005) Health-related quality of life with lymphoedema: a review of the literature. Int Wound J 2(1):47–62. https://doi.org/10.1111/j.1742-4801.2005.00066.x
Fu MR, Ridner SH, Hu SH, Stewart BR, Cormier JN, Armer JM (2013) Psychosocial impact of lymphedema: a systematic review of literature from 2004 to 2011. Psychooncology 22(7):1466–1484. https://doi.org/10.1002/pon.3201
McWayne J, Heiney SP (2005) Psychologic and social sequelae of secondary lymphedema: a review. Cancer 104(3):457–66. https://doi.org/10.1002/cncr.21195
National Lymphedema Network Medical Advisory Committee (2011) Exercise. San Francisco (CA): NLN
Lane KN, Dolan LB, Worsley D, McKenzie DC (2007) Upper extremity lymphatic function at rest and during exercise in breast cancer survivors with and without lymphedema compared with healthy controls. J Appl Physiol 103(3):917–925. https://doi.org/10.1152/japplphysiol.00077.2007
Schmitz KH (2010) Balancing lymphedema risk: exercise versus deconditioning for breast cancer survivors. Exerc Sport Sci Rev 38(1):17. https://doi.org/10.1097/JES.0b013e3181c5cd5a
Runowicz CD, Leach CR, Henry NL, Henry KS, Mackey HT, Cowens-Alvarado RL, Cannady RS, Pratt-Chapman ML, Edge SB, Jacobs LA, Hurria A (2016) American cancer society/American society of clinical oncology breast cancer survivorship care guideline. CA Cancer J Clin 66(1):43–73. https://doi.org/10.3322/caac.21319
Buchan J, Janda M, Box R, Schmitz K, Hayes S (2016) A randomized trial on the effect of exercise mode on breast cancer-related lymphedema. Med Sci Sports Exerc 48(10):1866–1874. https://doi.org/10.1249/MSS.0000000000000988
Singh B, Disipio T, Peake J, Hayes SC (2016) Systematic review and meta-analysis of the effects of exercise for those with cancer-related lymphedema. Arch Phys Med Rehabil 97(2):302–315. https://doi.org/10.1016/j.apmr.2015.09.012
Baumann FT, Reike A, Hallek M, Wiskemann J, Reimer V (2018) Does exercise have a preventive effect on secondary lymphedema in breast cancer patients following local treatment-a systematic review. Breast Care 13(5):380–385. https://doi.org/10.1159/000487428
Yang Z, Rafiei MH, Hall A, Thomas C, Midtlien HA, Hasselbach A, Adeli H, Gauthier LV (2018) A novel methodology for extracting and evaluating therapeutic movements in game-based motion captures rehabilitation systems. J Med Syst 42(12):1–4. https://doi.org/10.1007/s10916-018-1113-4
Parry I, Carbullido C, Kawada J, Bagley A, Sen S, Greenhalgh D, Palmieri T (2014) Keeping up with video game technology: objective analysis of Xbox KinectTM and PlayStation 3 MoveTM for use in burn rehabilitation. Burns 40(5):852–859. https://doi.org/10.1016/j.burns.2013.11.005
Zeng Y, Zhang JE, Cheng AS, Cheng H, Wefel JS (2019) Meta-analysis of the efficacy of virtual reality–based interventions in cancer-related symptom management. Integr Cancer Ther 18:1534735419871108. https://doi.org/10.1177/1534735419871108
Feyzioğlu Ö, Dinçer S, Akan A, Algun ZC (2020) Is Xbox 360 Kinect-based virtual reality training as effective as standard physiotherapy in patients undergoing breast cancer surgery? Support Care Cancer 6:1–9. https://doi.org/10.1007/s00520-019-05287-x
Aguilar-Lazcano CA, Rechy-Ramirez EJ, Hu H, Rios-Figueroa HV, Marin-Hernandez A (2019) Interaction modalities used on serious games for upper limb rehabilitation: a systematic review. Games Health J 8(5):313–325. https://doi.org/10.1089/g4h.2018.0129
Sin H, Lee G (2013) Additional virtual reality training using Xbox Kinect in stroke survivors with hemiplegia. Am J Phys Med Rehabil 92(10):871–880. https://doi.org/10.1097/phm.0b013e3182a38e40
Cormie P, Pumpa K, Galvão DA, Turner E, Spry N, Saunders C, Zissiadis Y, Newton RU (2013) Is it safe and efficacious for women with lymphedema secondary to breast cancer to lift heavy weights during exercise: a randomised controlled trial. J Cancer Surviv 7(3):413–424. https://doi.org/10.1007/s11764-013-0284-8
Paramanandam VS, Roberts D (2014) Weight training is not harmful for women with breast cancer-related lymphoedema: a systematic review. J Physiother 60(3):136–143. https://doi.org/10.1016/j.jphys.2014.07.001
Schmitz KH, Ahmed RL, Troxel A, Cheville A, Smith R, Lewis-Grant L, Bryan CJ, Williams-Smith CT, Greene QP (2009) Weight lifting in women with breast-cancer–related lymphedema. N Engl J Med 361(7):664–673. https://doi.org/10.1056/nejmoa0810118
Sim YJ, Jeong HJ, Kim GC (2010) Effect of active resistive exercise on breast cancer–related lymphedema: a randomized controlled trial. Arch Phys Med Rehabil 91(12):1844–1848. https://doi.org/10.1016/j.apmr.2010.09.008
Cheville AL, McGarvey CL, Petrek JA, Russo SA, Thiadens SR, Taylor ME (2003) The grading of lymphedema in oncology clinical trials. Semin Radiat Oncol 13(3):214–225. https://doi.org/10.1016/S1053-4296(03)00038-9
Strossenreuther RHK (2003) Guidelines for the application of MLD/ CDT for primary and secondary lymphedema and other selected pathologies: treatment of secondary arm, breast and trunk lymphedema. In: Foldi M, Foldi E, Kubik S (eds) Textbook of lymphology for physicians and lymphedema therapists. Urban & Fischer, München, pp 604–613
Sander AP, Hajer NM, Hemenway K, Miller AC (2002) Upper-extremity volume measurements in women with lymphedema: a comparison of measurements obtained via water displacement with geometrically determined volume. Phys Ther 82(12):1201–1212. https://doi.org/10.1093/ptj/82.12.1201
Chen YW, Tsai HJ, Hung HC, Tsauo JY (2008) reliability study of measurements for lymphedema in breast cancer patients. Am J Phys Med Rehabil 87(1):33–38. https://doi.org/10.1097/PHM.0b013e31815b6199
Bijur PE, Silver W, Gallagher EJ (2001) Reliability of the visual analog scale for measurement of acute pain. Acad Emerg Med 8(12):1153–1157. https://doi.org/10.1111/j.1553-2712.2001.tb01132.x
Alotaibi NM, Aljadi SH, Alrowayeh HN (2016) Reliability, validity and responsiveness of the Arabic version of the Disability of Arm, Shoulder and Hand (DASH-Arabic). Disabil Rehabil 38(25):2469–2478. https://doi.org/10.3109/09638288.2015.1136846
Sabari JS, Maltzev I, Lubarsky D, Liszkay E, Homel P (1998) Goniometric assessment of shoulder range of motion: comparison of testing in supine and sitting positions. Arch Phys Med Rehabil 79(6):647–651. https://doi.org/10.1016/S0003-9993(98)90038-7
Riddle DL, Rothstein JM, Lamb RL (1987) Goniometric reliability in a clinical setting. Shoulder measurements. Phys Ther 67:668
Roy JS, MacDermid JC, Orton B, Tran T, Faber KJ, Drosdowech D, Athwal GS (2009) The concurrent validity of a hand-held versus a stationary dynamometer in testing isometric shoulder strength. J Hand Ther 22(4):320–327. https://doi.org/10.1016/j.jht.2009.04.008
Peolsson A, Hedlund R, Oberg B (2001) Intra- and inter-tester reliability and reference values for hand strength. J Rehabil Med 33:36. https://doi.org/10.1080/165019701300006524
Guermazi M, Allouch C, Yahia M, Huissa TB, Ghorbel S, Damak J, Mrad MF, Elleuch MH (2012) Translation in Arabic, adaptation and validation of the SF-36 Health Survey for use in Tunisia. Ann Phys Rehabil Med 55(6):388–403. https://doi.org/10.1016/j.rehab.2012.05.003
Indovina P, Barone D, Gallo L, Chirico A, De Pietro G, Giordano A (2018) Virtual reality as a distraction intervention to relieve pain and distress during medical procedures: a comprehensive literature review. Clin J Pain 34:858–877. https://doi.org/10.1097/AJP.0000000000000599
Mohammad BE, Ahmad M (2018) Virtual reality as a distraction technique for pain and anxiety among patients with breast cancer: a randomized control trial. Palliat Support Care 10:1–6. https://doi.org/10.1017/S1478951518000639
House G, Burdea G, Grampurohit N et al (2016) A feasibility study to determine the benefits of upper extremity virtual rehabilitation therapy for coping with chronic pain post-cancer surgery. Br J Pain 10:186–197. https://doi.org/10.1177/2049463716664370
Chirico A, Lucidi F, De Laurentiis M, Milanese C, Napoli A, Giordano A (2016) Virtual reality in health system: beyond entertainment. A mini-review on the efficacy of VR during cancer treatment. J Cell Physiol 231(2):275–87. https://doi.org/10.1002/jcp.25117
Magermans DJ, Chadwick EK, Veeger HE, Van Der Helm FC (2005) Requirements for upper extremity motions during activities of daily living. Clin Biomech 20(6):591–599. https://doi.org/10.1016/j.clinbiomech.2005.02.006
Johansson K, Hayes S, Speck RM, Schmitz KH (2013) Water-based exercise for patients with chronic arm lymphedema: a randomized controlled pilot trial. Am J Phys Med Rehabil 92(4):312–319. https://doi.org/10.1097/phm.0b013e318278b0e8
Hedayatpour N, Falla D (2015) Physiological and neural adaptations to eccentric exercise: mechanisms and considerations for training. Biomed Res Int 12:2015. https://doi.org/10.1155/2015/193741
Jeffs E, Wiseman T (2013) Randomised controlled trial to determine the benefit of daily home-based exercise in addition to self-care in the management of breast cancer-related lymphoedema: a feasibility study. Support Care Cancer 21(4):1013–1023. https://doi.org/10.1007/s00520-012-1621-6
Bok SK, Jeon Y, Hwang PS (2016) Ultrasonographic evaluation of the effects of progressive resistive exercise in breast cancer-related lymphedema. Lymphat Res Biol 14(1):18–24. https://doi.org/10.1089/lrb.2015.0021
McClure MK, McClure RJ, Day R, Brufsky AM (2010) Randomized controlled trial of the breast cancer recovery program for women with breast cancer–related lymphedema. Am J Occup Ther 64(1):59–72. https://doi.org/10.5014/ajot.64.1.59
Leduc O, Bourgeois P, Leduc A (1988) Manual of lymphatic drainage: scintigraphic demonstration of its efficacy on colloidal protein resorption. In: Partsch H (ed) Progress in lymphology IX. Elsevier, Amsterdam, 421–423. NII Article ID (NAID) 20001294411
Singh B, Buchan J, Box R, Janda M, Peake J, Purcell A, Reul-Hirche H, Hayes SC (2016) Compression use during an exercise intervention and associated changes in breast cancer–related lymphedema. Asia Pac J Clin Oncol 12(3):216–224. https://doi.org/10.1111/ajco.12471
Acknowledgements
We are grateful to our patients for taking part in this study.
Author information
Authors and Affiliations
Contributions
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Conceptualization: FatmaAlzahraa H. Kamel; methodology: Nancy H. Aboelnour; formal analysis and investigation: Maged A. Basha; writing—original draft preparation: Maged A. Basha, FatmaAlzahraa H. Kamel; writing—review and editing: Maged A. Basha Ph.D., Nancy H. Aboelnour Ph.D., Ashwag S. Alsharidah, FatmaAlzahraa H. Kamel; resources: Maged A. Basha Ph.D., Nancy H. Aboelnour Ph.D., Ashwag S. Alsharidah, FatmaAlzahraa H. Kamel; supervision: Maged A. Basha Ph.D., FatmaAlzahraa H. Kamel. All authors read and approved this manuscript.
Corresponding author
Ethics declarations
Ethics approval
All study procedures were conducted in line with the rules and principles of the Declaration of Helsinki of the World Medical Association. The study was approved by the Research Ethics Committee of Physical Therapy Faculty in Cairo University (P.T.REC/012/002449). This trial was registered in ClinicalTrials.gov (ID: NCT04724356).
Consent to participate
The participants were explained the details of the study and signed an informed consent in compliance with ethical standards prior to participating in the study.
Consent for publication
The participants gave consent for publication of de-identified information through informed consent.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Basha, M.A., Aboelnour, N.H., Alsharidah, A.S. et al. Effect of exercise mode on physical function and quality of life in breast cancer–related lymphedema: a randomized trial. Support Care Cancer 30, 2101–2110 (2022). https://doi.org/10.1007/s00520-021-06559-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06559-1