Abstract
A novel alternative approach for extracellular synthesis of CdS quantum dots using Escherichia coli bacteria, the fungus Pleurotus ostreatus, and the plant Linaria maroccana as biological matrices was previously developed. The nanoparticles obtained had stable luminescent properties and diameters of 2–10 nm. This paper presents the results of MTT assay- and flow cytometry-based analysis of cytotoxic/cytostatic effects, proliferative activity, and the ability of the CdS quantum dots synthesized to adhere to HeLa cells (human cervical cancer), malignized human T- and B-lymphocytes, and tumor cells of the AGS line (stomach cancer). The toxicity of the CdS quantum dots obtained by the “green” synthesis method was lower than that of inorganic cadmium sulfide, and this makes the quantum dots attractive candidates for a new type of nontoxic luminescent probes for bioimaging in cytological studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Quantum dots are fluorescent semiconductor particles that can be used as novel fluorescent probes [1]. Quantum dots have unique photophysical properties different from those of the conventional organic dyes, such as adjustable brightness of emitted light, high fluorescence intensity, resistance to photobleaching, and simultaneous excitation of fluorescence of multiple colors. Moreover, quantum dots can be obtained for various biological applications, including immunohistochemical detection, drug delivery and therapy, and visualization and tracking of single molecules [2, 3].
CdS quantum dots are the most important semiconductors of groups II–VI among various semiconductor materials; they are characterized in detail because of their size-dependent photoluminescence tunable in the visible spectrum. The main interest towards the study of CdS quantum dots is actually associated with their photoluminescent properties, which make the quantum dots suitable for biological and biomedical research [4].
Production of CdS quantum dots with various chemical methods, such as microwave heating, microemulsion synthesis, and ultrasonic irradiation, was reported [5, 6]. However, chemical methods require expensive equipment and highly toxic reagents, and large amounts of toxic waste produced during the synthesis pollute the environment. Therefore, the use of biological systems for the synthesis of nanomaterials is proposed as an alternative approach [7]. Living organisms have a unique potential for obtaining nanoparticles of various shapes and sizes. For instance, successful extracellular synthesis of cadmium sulfide nanoparticles using various living organisms (bacteria, fungi, and plants) as matrices was reported in our previous studies [8–12]. Cell cultures used to synthesize nanoparticles are easy to grow under laboratory conditions, safe for the environment, and capable of producing a large amount of biomass in a short time.
However, the question of the cytotoxicity of quantum dots is important for their subsequent practical use. The toxicity of quantum dots is reportedly determined by their physicochemical parameters, such as size, charge, and stability, and by the chemical composition. Therefore, thorough testing of the CdS quantum dots obtained by “green” synthesis methods is necessary to characterize the toxic effects on various cell types in view of the subsequent biological and biomedical applications.
Consequently, the aim of the present study was to evaluate the possible cytotoxic effect of CdS semiconductor nanoparticles that we previously synthesized [8–12]. HeLa cells (human cervical cancer), transformed human T- and B-lymphocytes, and the AGS tumor cell line (stomach cancer) were used for evaluation of cytotoxic/cytostatic action, proliferative activity, and adhesion properties. Cytotoxicity of the synthesized nanoparticles and cell viability were investigated using MTT analysis and flow cytometry. The toxic effects of obtained CdS nanoparticles on various biological matrices were compared with toxic cadmium sulfide salt.
MATERIALS AND METHODS
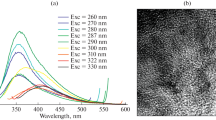
The procedure of “green” synthesis and the physicochemical properties of CdS quantum dots were described in detail in our previous works [8–11]. A JEM-2100F electron microscope (Japan) with an accelerating voltage of 200 kV was used to characterize the CdS quantum dots. Each sample was treated with ultrasound to separate the particles.
The concentration of CdS nanoparticles obtained from a stock solution with Escherichia coli bacteria was 3.6 mg/mL; that with the fungus Pleurotus ostreatus was 3.75 mg/mL and that with the plant Linaria maroccana was 1.2 mg/mL. The concentration of the CdS salt obtained without any matrix added was 4 mg/mL.
The toxicity of CdS quantum dots was studied with the following cell lines: transformed HeLa cells (cervical cancer), Namalwa cell line (Burkitt’s lymphoma), MT-4 (T-cell leukemia), and the AGS cell line (stomach cancer).
HeLa cells were incubated under standard conditions in a thermostat at 37°C, 100% humidity, and 5% CO2, in the RPMI nutrient medium (Sigma, United States) supplemented with 10% FBS (Sigma, United States), 2 mM L-glutamine, and 40 mg/mL gentamicin. T- and B-lymphocytes were resuspended in a medium (DMEM or RPMI-1640 (Sigma, United States)) supplemented with 10–15% FBS (Sigma, United States). The mitogenic effects of quantum dots on tumor cells were studied during the stationary growth phase, when most of the cells were in the G0 phase of the cell cycle. Lymphocytes were isolated from the peripheral blood of healthy donors by centrifugation in a ficoll-verografin gradient (ρ = 1.077 g/cm3) at 1000 g for 40 min. The lymphocytes were incubated at a concentration of 1 × 106 cells/mL in RPMI-1640 nutrient medium supplemented with 10% FBS, 200 μM L-glutamine, 100 μg/mL penicillin, and 100 μg/mL streptomycin for 3 days at 37°C and 5% CO2.
The cytotoxic/cytostatic effect of CdS and its effect on proliferative activity and cell viability were determined using the MTT-colorimetric assay [13]. The method is based on the ability of the mitochondrial enzymes of living cells to transform the yellow salt 3-(4,5-dimethyl-thiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) into an insoluble purple formazan. A solution of MTT (Sigma, United States) was added to 96-well plates at 20 μL/well and incubated with the cells for 3 h. The plates were centrifuged (1500 rpm), the supernatant was removed, and 100 μL dimethyl sulfoxide (Sigma) were added to each well to dissolve the formazan crystals. Optical absorbance was measured using a spectrophotometer (wavelength 540 nm).
The toxicity of CdS quantum dots was also assessed using flow cytometry. Cells in the G2 + M phase are known to contain twice the amount of DNA and, consequently, fluorochrome as compared to those at the G1/0 phase of the cell cycle. The amount of DNA increases gradually in the S-phase, and this is recorded by the device. The number of pulses per channel is plotted on the y-axis: the higher the curve at a specific point, the more cells with the corresponding DNA content are present in the corresponding channel. The DNA of the studied cells was stained with propidium iodide (PI), a fluorescent dye that selectively binds to intercalation sites in the DNA. The cell density in the sample was 106. Distribution histograms were constructed in the ModFit LT 2.0 mathematical software (BDIS, United States) in order to assess the relative content of cells at different phases of the cell cycle (G1/0, S, and G2 + M). A 585/42-nm narrowband filter was used for PI fluorescence measurements.
Adhesion properties were inferred from the number (%) of attached cells stained with crystal violet. The cells used for this experiment were incubated with CdS quantum dots and the biological matrices used to synthesize the quantum dots (positive control) in 96-well plates for 48 h. The cells were subsequently washed with two changes of PBS, and the attached cells were fixed in a 70% ethanol solution. The samples were stained with crystal violet for 15–30 min and then washed three times in PBS. The dye was dissolved in dimethyl sulfoxide, and the optical absorption was measured at a wavelength of 570 nm.
The counting of cells after staining with trypan blue was used to assess the survival of HeLa cells treated with CdS nanoparticles. The cells’ ability to survive was defined as the percentage of living cells after treatment with the nanoparticles compared to the corresponding control (bacterial, fungal, and plant matrices used to synthesize the nanoparticles).
Luminescence microscopy. The cells were incubated with CdS quantum dots for 48 h in order to study the penetration and intracellular localization of the nanoparticles synthesized in our study. Cell nuclei were stained with 10 μL DAPI (4',6-diamidino-2-phenylindol) in phosphate-buffered saline and glycerol. The samples were analyzed using an AxioImager M1 fluorescent microscope (Carl Zeiss, Germany) equipped with a filter for FITC and DAPI. The images obtained with the DAPI and FITC filters were compared in Isis v. 5.3 software (Meta Systems, Germany).
Statistical analysis was performed using the standard Statistica 8.0 software. Student’s t-test was used to compare the mean values for the different samples [14].
RESULTS AND DISCUSSION
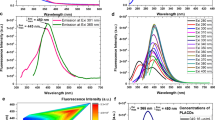
Characterization of the synthesized CdS quantum dots by transmission electron microscopy (TEM). The TEM method was used to study the morphology and crystal structure of CdS nanoparticles (Figs. 1–3). The experiments showed that the quantum dots obtained by the “green” synthesis method had a spherical shape, a smooth surface, and a diameter in the 3–8 nm range that depended on the biological matrix used for the synthesis. The CdS nanoparticles obtained were filtered through sterile Millipore filters for further cytotoxicity studies.
The cytotoxic effect of CdS quantum dots on HeLa cells. Evaluation of the cytotoxicity of quantum dots is crucial for the subsequent practical application in biological and biomedical research. The classical MTT assay, which provides a characteristic of the metabolic activity of intracellular enzymes [15], is used for this purpose. In our study, we analyzed the toxicity of three types of CdS quantum dots synthesized using matrices derived from the bacterium E. coli, the fungus P. ostreatus, and the plant L. maroccana.
CdS quantum dots obtained using E. coli as a matrix exerted a significant cytostatic effect. The number of dead HeLa cells was 2 and 2.8 times higher in the samples treated with this type of nanoparticles than in the negative control. The apoptotic index of HeLa cells was 9.5% after treatment with CdS quantum dots (E. coli) and 7.5% in the negative control (Table 1). The CdS quantum dots synthesized using P. ostreatus exerted an antiproliferative effect: there were 29.2% less cells in the sample than in the control. Treatment with CdS quantum dots (L. maroccana) led to inhibition of the proliferative activity of HeLa cells as compared to the intact tumor cells. The apoptotic, cytostatic, and cytotoxic effects of nanoparticles were also detected. The apoptotic and cytostatic effects were enhanced three and two times over the control, respectively, when CdS (L. maroccana) was applied. For instance, the number of dead cells increased to 21% after treatment of HeLa cells with CdS quantum dots (L. maroccana), and the apoptotic index of HeLa cells amounted to 17.5% (Table 1).
Cell adhesion molecules play a significant role in cancer progression and the metastatic process [16]. The capacity for intercellular adhesion, which causes invasion into the vascular system and the development of metastases, is an important indicator of the functional state of cancer cells. The decrease of adhesion capacity of tumor cells appears to correlate with a decrease in the malignancy of these cells. In this regard, the adhesion potential of HeLa cells was studied before and after treatment with CdS quantum dots. The treatment of HeLa cells with quantum dots obtained with E. coli and applied at high concentrations (0.9–1.8 mg/L) led to a decrease in the cells’ adhesion potential, with the corresponding parameter dropping from 70 to 20% (Fig. 4).
The adhesion potential of HeLa cells treated with cadmium sulfide salt at the same concentration amounted to 30%. We showed that CdS quantum dots synthesized using P. ostreatus had a capacity for substantial reduction of the adhesion potential of HeLa cells relative to CdS. The study demonstrated a decrease of the adhesion potential of cancer cells from 55 to 22% after the exposure to CdS quantum dots (P. ostreatus) at concentrations of 0.1–1.8 mg/mL. However, CdS salt applied at the same concentrations did not significantly change the adhesion potential of HeLa cells. The adhesion potential was approximately 29% and decreased to 25% only when inorganic CdS was used at high concentrations (Fig. 5). HeLa cells treated with CdS quantum dots (L. maroccana) at concentrations from 0.037 to 0.6 mg/L maintained the adhesive capacity at a high level (up to 90%; Fig. 6).
The results obtained allow for the conclusion that treatment with cadmium sulfide salt reduced the adhesion potential of HeLa cells to 25–29%, whereas the treatment with CdS quantum dots (E. coli) and CdS quantum dots (P. ostreatus) caused a dose-dependent decrease in the adhesion potential of cancer cells. For instance, an increase in the concentration of CdS quantum dots in the samples was shown to lead to a decrease in the adhesion properties of HeLa cells (Figs. 4, 5).
The effect of various types of CdS quantum dots, which we previously synthesized on different biological matrices, on the proliferation of HeLa cells was also assessed with the MTT assay. A decrease of the proliferative activity of HeLa cells from 86 to 40% after treatment with CdS quantum dots (E. coli) taken at increasing concentrations was observed. The proliferative activity of the cells treated with inorganic CdS at the same concentrations varied in the range of 20–28% (Fig. 7).
Treatment with CdS quantum dots (P. ostreatus) resulted in dose-dependent inhibition of cancer cell proliferation. Thus, cell proliferation was reduced to 22% when the concentrations of quantum dots (P. ostreatus) were 0.9–1.8 mg/L. Treatment with cadmium sulfide salt at these concentrations reduced the proliferative activity of cells to 23–28% (Fig. 8).
CdS quantum dots (L. maroccana) applied at low concentrations increased the proliferation of cancer cells significantly (up to 100%). Proliferative activity of HeLa cells exposed to inorganic CdS varied in the range of 22–30% (Fig. 9). Thus, the CdS quantum dots synthesized using E. coli and P. ostreatus were the most promising, because they reduced the adhesion potential of HeLa cells and had an antiproliferative effect.
The toxicity of CdS quantum dots towards transformed T and B lymphocytes. The putative toxic effect of quantum dots on immune cells and their function remains poorly studied. Therefore, the cytotoxic/cytostatic effects of the CdS quantum dots (P. ostreatus) that we synthesized were investigated with transformed human T- and B-lymphocytes as the target cells and cadmium sulfide salt as the reference substance. It should be noted that inorganic CdS has a pronounced toxic effect on T-cells (MT-4 cell line) (Fig. 10). According to the results of the MTT assay, the enzyme activity in the treated cells decreased gradually depending on the cadmium sulfide concentrations used. Treatment of T-lymphocytes with inorganic CdS at concentrations of 0.04–0.3 mg/mL caused a decrease in enzymatic activity and resulted in inhibition of cell viability. The proliferative activity of the cells decreased from 70 to 50% under these conditions. The cytotoxic/cytostatic effect of CdS quantum dots (P. ostreatus) on T-lymphocytes of the MT-4 cell line was also evaluated at quantum dot concentrations of 2.5–5 mg/mL. We demonstrated that the treatment with quantum dots led to clustering of T-lymphocytes. Induction of apoptosis was only detected when the CdS quantum dots were used at a high concentration (1.5 mg/mL).
Treatment of cells with quantum dots showed that the latter were less toxic than inorganic cadmium sulfide (Fig. 11). Treatment with quantum dots at low concentrations (0.015–0.25 mg/mL) had only a slight effect on the proliferative activity of T-lymphocytes, which decreased from 88 to 70%. Thus, quantum dots synthesized using biological matrices did not exert a significant effect on the viability of T-lymphocytes. Comparison to the effect of inorganic CdS allows for the conclusion that the inorganic salt strongly inhibited the proliferative activity of T-lymphocytes, which was reduced to 50%, whereas the proliferative activity of cells treated with CdS quantum dots was 70–90%.
The cytotoxic/cytostatic effects of inorganic CdS and synthesized CdS quantum dots on tumor B-lymphocytes (Namalwa phenotype), as well as the effects on the proliferative potential of the cells, were also compared. In contrast to T-lymphocytes, inorganic cadmium ions exerted a strong mitogenic effect on B-lymphocytes. The effect of 0.01–0.3 mg/mL CdS on the induction of cell proliferation in B-lymphocytes is illustrated in Fig. 12.
It should be noted that the treatment of B-lymphocytes with inorganic cadmium led to an increase in the proliferative activity of the cells, which was 78–108% of the value for the intact cells, in the entire range of concentrations tested. Earlier studies showed that cadmium had pleiotropic effects on the immune system. For instance, cadmium can enhance the monocytic differentiation of ERK1/2, and this leads to an increase in the generation of functional monocytes [17]. Moreover, low micromolar concentrations of Cd2+ stimulate cell growth and induce certain proto-oncogenes in some mammalian cell lines [18]. Therefore, one can assume that inorganic cadmium ions exerted a stimulating effect on B-lymphocytes in contrast to T-lymphocytes.
We showed that treatment of B-lymphocytes with CdS quantum dots (at concentrations of 0.04–0.45 mg/mL) obtained with P. ostreatus did not lead to a decrease in cell proliferation activity, which remained close to 90%. No cytotoxic effect was observed either, since the proliferative activity of the cells ranged from 76 to 94% (Fig. 13).
According to the results of the MTT test, no significant decrease in the enzymatic activity was observed in the tumor cells. Application of quantum dots at higher concentrations, namely, 0.45 mg/mL, did not lead to inhibition of the proliferation of B-lymphocytes either. Proliferative activity was approximately 90%. These results are comparable with the data obtained in studies of the influence of CdS quantum dots on T-lymphocytes, since the proliferative activity was also 70–90% in this case.
Fluorescence microscopy of CdS quantum dots. The successful use of quantum dots for the detection of tumor-specific biomarkers and cell imaging demonstrates great potential for their further use in high-throughput screening, early clinical diagnosis, and surgery [26, 27]. We also studied the penetration of CdS quantum dots into HeLa cells and their intracellular localization. For this purpose, HeLa cells were incubated for 48 h with synthesized CdS quantum dots (P. ostreatus) at concentrations of 0.1–0.5 mg/mL. The selective DNA-binding fluorochrome DAPI was used to stain the nuclei. CdS quantum dots were found to penetrate easily into cells and fluoresce in the green spectral range in the cytoplasm (Fig. 14).
We also studied the morphological changes in HeLa and AGS cells treated with cadmium sulfide and CdS quantum dots (P. ostreatus). Inorganic cadmium ions were shown to exert a strong toxic effect as compared to the CdS nanoparticles (Fig. 15). Treatment of the tumor cells with quantum dots led to a slight aggregation of the cells, but cell shape and structure did not change. Earlier studies showed that the toxicity of CdS quantum dots might be associated with the release of free cadmium ions [19]. The cytotoxicity of chemically synthesized CdS quantum dots towards isolated hemocytes and gill cells of the mussel Mytilus galloprovincialis was investigated in [20]. The treatment of M. galloprovincialis cells with quantum dots at sublethal concentrations (0.31–5 mg/mL) led to the formation of reactive oxygen species (ROS), increased catalase (CAT) activity, DNA damage, increased lysosomal acid phosphatase (AcP) activity, increased Na-K-ATPase activity (in gill cells only), and phagocytic activity and damage to the actin cytoskeleton (in hemocytes only) [20]. However, cadmium ions were more toxic towards both cell types than the CdS quantum dots were.
Moreover, another study convincingly demonstrated the genotoxic and cytotoxic effect of CdS quantum dots on a rainbow trout cell line. The results showed that chemically synthesized quantum dots had a high cytotoxicity at concentrations of 10 and 50 μg/mL and showed a concentration-dependent genotoxicity in the subtoxic concentration range (0.01–1 μg/mL) after 24-h treatment [21]. Such concentrations are significantly lower than those studied in the present work. Several studies have suggested that the cytotoxic effects of quantum dots may be mediated by cadmium ions released from the quantum dot core and the imbalance of the intracellular oxidative status evoked by these ions [22, 23].
The toxic effect of chemically synthesized CdS nanoparticles on E. coli and HeLa cells was also studied [24]. The viability of HeLa cells decreased with increasing concentrations of CdS nanoparticles, and the IC50 value for the cells was 4 μg/mL. Altered morphology and the condensation and fragmentation of nuclei of the treated HeLa cells was demonstrated. A concentration of 2.5 μg/mL was used to study the toxic effects of CdS nanoparticles on cell viability, and cell viability was found to decrease with increasing duration of treatment. The negative correlation between reduced cell growth and increased ROS levels suggests that oxidative stress can be a part of the pathway whereby CdS nanoparticles induce cytotoxicity in both prokaryotic and eukaryotic cells [24].
Thus, chemically synthesized CdS nanoparticles exert cytotoxic effects on living cells at concentrations significantly lower than the concentrations used in our study. Capping of the nanoparticle surface with organic molecules was shown to significantly reduce the toxicity of cadmium ions [25]. Proteins, enzymes, secondary metabolites, or other molecules that are an integral part of the process of synthesis on biological matrices form a protective layer, which can prevent the release of cadmium ions and thus significantly reduce the toxicity of quantum dots. It is important to note that CdS quantum dots synthesized using E. coli and P. ostreatus in our previous studies neither had a significant negative effect in vivo nor exerted a genotoxic effect on Drosophila melanogaster when applied at a concentration of 0.45 mg/mL [26].
To summarize the obtained data, we can conclude that the treatment of different types of tumor cells with CdS quantum dots leads to different effects. For instance, the treatment of HeLa cells with quantum dots led to a decrease in cell proliferation, with the exception of CdS (L. maroccana), which, on the contrary, increased the proliferative activity of the cells. Treatment of T- and B-lymphocytes with quantum dots synthesized using P. ostreatus resulted in an increase of proliferative activity of the cells (70–90%), whereas the CdS salt reduced the cell viability to 30 (HeLa cells) or 50% (T-lymphocytes) and stimulated cell proliferation to a level of 108% in B-lymphocytes. We demonstrated that the quantum dots did not induce substantial changes in the morphology of tumor cells. The high brightness and the adjustable size-dependent narrow peak of luminescence distinguish them from the ordinary fluorescent dyes. Due to the properties mentioned above and the low cytotoxicity, CdS quantum dots can be considered promising fluorescent probes for the visualization and labeling of intracellular molecules and structures as well as the cells themselves.
CONCLUSIONS
Our results suggest that CdS quantum dots synthesized using different (bacterial, fungal, or plant) biological matrices exert different effects on tumor cells. The mechanisms and factors that control the accumulation and toxicity of semiconductor nanomaterials are quite complex and will be addressed in detail in our future studies. However, in the framework of this study, we demonstrated the inherent antiproliferative activity of CdS quantum dots synthesized using E. coli and P. ostreatus. These nanoparticles also reduced the adhesion properties of cancer cells in a dose-dependent manner. On the contrary, the quantum dots synthesized using L. maroccana increased the proliferative activity and adhesion properties of tumor cells. Inorganic cadmium showed much greater toxicity than all three types of CdS quantum dots tested. Treatment of immune cells with quantum dots led to an increase in the level of lymphocyte proliferation. CdS nanoparticles did not cause any morphological changes in the cells studied. We have also shown that quantum dots can easily penetrate into cells, where they mainly localize to the cytoplasm, and have high brightness and photostability. Thus, CdS semiconductor quantum dots synthesized using biological matrices can be further functionalized and potentially used as nontoxic fluorescent probes for various kinds of biological and biomedical studies.
REFERENCES
Zhao, M.X. and Zeng, E.Z., Application of functional quantum dot nanoparticles as fluorescence probes in cell labeling and tumor diagnostic imaging, Nanoscale Res. Lett., 2015, vol. 10, pp. 1–9. https://doi.org/10.1186/s11671-015-0873-8
Rosentha, S.J., Chang, J.C., Kovtun, O., McBride, J.R., and Tomlinson, I.D., Biocompatible quantum dots for biological applications, Chem. Biol., 2011, vol. 18, no. 1, pp. 10–24. https://doi.org/10.1016/j.chembiol.2010.11.013
Medintz, I.L., Mattoussi, H., and Clapp, A.R., Potential clinical applications of quantum dots, Int. J. Nanomed., 2008, vol. 3, no. 2, pp. 151–167.
Hoshino, A., Fujioka, K., Oku, T., Nakamura, S., Suga, M., Yamaguchi, Y., Suzuki, K., Yasuhara, M., and Yamamoto, K., Quantum dots targeted to the assigned organelle in living cells, Microbiol. Immunol., 2004, vol. 48, no. 12, pp. 985–994.
Tamašauskaitė-Tamašiūnaitė, L., Grincienė, G., Šimkūnaitė-Stanynienė, B., Naruškevicius, L., Pakštas, V., Selskis, A., and Norkus, E., Preparation of CdS nanoparticles by microwave-assisted synthesis, Chemija, 2015, vol. 26, no. 3, pp. 193–197.
Wang, G.Z., Chen, W., Liang, C.H., Wang, Y.W., Meng, G.W., and Zhang, L.D., Preparation and characterization of CdS nanoparticles by ultrasonic irradiation, Inorg. Chem. Commun., 2001, vol. 4, no. 4, pp. 208–210.
Marchiol, L., Synthesis of metal nanoparticles in living plants, Ital. J. Agron., 2012, vol. 7, no. 3, pp. 274–282. https://doi.org/10.4081/ija.2012.e37
Borovaya, M.N., Naumenko, A.P., Matvieieva, N.A., Blume, Y.B., and Yemets, A.I., Biosynthesis of luminescent CdS quantum dots using plant hairy root culture, Nanocsale Res. Lett., 2014, vol. 9, pp. 1–7. https://doi.org/10.1186/1556-276X-9-686
Borovaya, M.N., Naumenko, A.P., Yemets, A.I., and Blume, Y.B., Stability of the CdS quantum dots, synthesized by the bacteria Escherichia coli, Rep. Natl. Acad. Sci. Ukraine, 2014, vol. 7, pp. 145–151.
Borovaya, M.N., Naumenko, A.P., Pirko, Y.V., Krupodorova, T.A., Yemets, A.I., and Blume, Y.B., Production of CdS quantum dots with the use of the fungus Pleurotus ostreatus, Rep. Natl. Acad. Sci. Ukraine, 2014, vol. 2, pp. 153–159.
Borovaya, M., Pirko, Y., Krupodorova, T., Naumenko, A., Blume, Y., and Yemets, A., Biosynthesis of cadmium sulphide quantum dots by using Pleurotus ostreatus (Jacq.) P. Kumm, Biotechnol. Biotechn. Equipm., 2015, vol. 29, no. 6, pp. 1156–1163. https://doi.org/10.1080/13102818.2015.1064264
Borovaya, M.N., Burlaka, O.M., Naumenko, A.P., Blume, Ya.B., and Yemets, A.I., Extracellular synthesis of luminescent CdS quantum dots using plant cell culture, Nanoscale Res. Lett., 2016, vol. 11, no. 1, pp. 1–8. https://doi.org/10.1186/s11671-016-1314-z
Mosmann, T., Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxic assays, J. Immun. Meth., vol. 65, nos. 1–2, pp. 55–63.
McDonald, J.H., Handbook of Biological Statistics, Baltimore, Maryland: Sparky House Publishing, 2008.
Kong, B., Seog, J.H., Graham, L.M., and Lee, S.B., Experimental considerations on the cytotoxicity of nanoparticles, Nanomedicine, 2011, vol. 6, pp. 929–941. https://doi.org/10.2217/nnm.11.77
Bendas, G. and Borsig, L., Cancer cell adhesion and metastasis: selectins, integrins, and the inhibitory potential of heparins, Int. J. Cell Biol., 2012, vol. 2012, p. 10. https://doi.org/10.1155/2012/676731
Goo, S., Choi, Y.J., Lee, Y., Lee, S., and Chung, H.W., Selective effects of curcumin on CdSe/ZnS quantum-dot-induced phototoxicity using UVA irradiation in normal human lymphocytes and leukemia cells, Toxicol. Res., 2013, vol. 29, no. 1, pp. 35–42. https://doi.org/10.5487/TR.2013.29.1.035
Ober-Blobaum, J.L., Engelhardt, G., Hebel, S., Rink, L., and Haase, H., Cadmium ions promote monocytic differentiation of humanleukemia HL-60 cells treated with 1a,25-dihydroxyvitamin D3, Biol. Chem., 2010, vol. 391, no. 11, pp. 1295–303. https://doi.org/10.1515/BC.2010.135
Zhou, J., Yang, Y., and Zhang, C., Toward biocompatible semiconductor quantum dots: from biosynthesis and bioconjugation to biomedical application, Chem. Rev., 2015, vol. 115, no. 21, pp. 11669–11717. https://doi.org/10.1021/acs.chemrev.5b00049
Katsumiti, A., Gilliland, D., Arostegui, I., and Cajaraville, M.P., Cytotoxicity and cellular mechanisms involved in the toxicity of CdS quantum dots in hemocytes and gill cells of the mussel Mytilus galloprovincialis, Aquat. Toxicol., 2014, vol. 153, pp. 39–52. https://doi.org/10.1016/j.aquatox.2014.02.003
Munari, M., Sturve, J., Frenzilli, G., Sandersd, M.B., Brunelli, A., Marcomini, A., Nigroc, M., and Lyons, B.P., Genotoxic effects of CdS quantum dots and Ag2S nanoparticles in fish cell lines (RTG-2), Mutat. Res. Gen. Toxicol. Environ. Mutagen., 2014, vols., 775–776, pp. 89–93. https://doi.org/10.1016/j.mrgentox.2014.09.003
Cho, S.J., Maysinger, D., Jain, M., Roder, B., Hackbarth, S., and Winnik, F.M., Long-term exposure to CdTe quantum dots causes functional impairments in live cells, Langmuir, 2007, vol. 23, no. 4, pp. 1974–1980. https://doi.org/10.1021/la060093j
Li, K.G., Chen, J.T., Bai, S.S., Wen, X., Song, S.Y., Yu, Q., Li, J., and Wang, Y.Q., Intracellular oxidative stress and cadmium ions release induce cytotoxicity of unmodifiedcadmium sulphide quantum dots, Toxicol. In Vitro, 2009, vol. 23, no. 6, pp. 1007–1013. https://doi.org/10.1016/j.tiv.2009.06.020
Hossain, Sk.T. and Mukherjee, S.K., Toxicity of cadmium sulfide (CdS) nanoparticles against Escherichia coli and HeLa cells, J. Hazard. Mater., 2013, vol. 260, pp. 1073–1082. https://doi.org/10.1016/j.jhazmat.2013.07.005
Galeone, A., Vecchio, G., Malvindi, M.A., Brunetti, V., Cingolani, R., and Pompa, P.P., In vivo assessment of CdSe-ZnS quantum dots: coating dependent bioaccumulation and genotoxicity, Nanoscale, 2012, vol. 4, no. 2, pp. 6401–6407. https://doi.org/10.1039/c2nr31826a
Protsenko, O.V., Dudka, O.A., Kozeretskaya, I.A., Inomystova, M.V., Borovaya, M.N., Pirko, Ya.V., Tolstanova, A.N., Ostapchenko, L.I., and Yemets, A.I., Estimation of toxicity and genotoxicity of CdS quantum dots synthesized with the help of biological matrices, Proc. Natl. Acad. Sci. Ukraine, 2016, vol. 4, pp. 111–117.
Borovaya, M.N., Burlaka, O.M., Yemets, A.I., and Blume, Ya.B., Biosynthesis of Quantum Dots and Their Potential Applications in Biology and Biomedicine, Springer International Publishing Switzerland, 2015, vol. 167, no. 24, pp. 339–362. https://doi.org/10.1007/978-3-319-18543-9_24
COMPLIANCE WITH ETHICAL STANDARDS
The authors declare that they have no conflict of interest. This article does not contain any studies involving animals or human participants performed by any of the authors.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Translated by S. Semenova
About this article
Cite this article
Garmanchuk, L.V., Borovaya, M.N., Nehelia, A.O. et al. CdS Quantum Dots Obtained by “Green” Synthesis: Comparative Analysis of Toxicity and Effects on the Proliferative and Adhesive Activity of Human Cells. Cytol. Genet. 53, 132–142 (2019). https://doi.org/10.3103/S0095452719020026
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.3103/S0095452719020026