Abstract
Objective
To assess the association between consumption of ultra-processed foods and obesity, diabetes, hypertension and heart disease in a nationally representative sample of Canadian adults.
Methods
This study used cross-sectional data from 13,608 adults (aged 19+ years) from the 2015 Canadian Community Health Survey–Nutrition. The survey provided data on food consumption (from 24-h recall) and prevalent obesity (BMI ≥ 30 kg/m2) and self-reported diabetes, hypertension and heart disease. All foods and drinks consumed were classified according to the extent and purpose of industrial processing using the NOVA classification. Ultra-processed food consumption was estimated as proportion of total daily energy intake. Multivariable logistic regression models assessed the association between ultra-processed food consumption and obesity, diabetes, hypertension and heart disease, adjusting for a range of socio-demographic and lifestyle factors.
Results
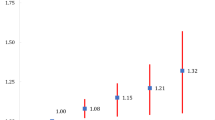
In 2015, ultra-processed food contributed, on average, to 24% of total daily energy intake in the lowest tertile of ultra-processed food consumption and 73% in the highest tertile. Compared with those in the lowest tertile, adults in the highest tertile of ultra-processed food consumption had 31% higher odds of obesity (OR = 1.31, 95% CI: 1.06–1.60), 37% higher odds of diabetes (OR = 1.37, 95% CI: 1.01–1.85) and 60% higher odds of hypertension (OR = 1.60, 95% CI: 1.26–2.03), adjusting for a range of covariates.
Conclusion
Higher consumption of ultra-processed foods is associated with higher prevalence of obesity, diabetes and hypertension among Canadian adults. A comprehensive set of strategies and policies is needed to discourage consumption of ultra-processed foods in Canada and to make unprocessed or minimally processed foods more affordable, available and appealing.
Résumé
Objectif
Évaluer l’association entre la consommation d’aliments ultra-transformés et l’obésité, le diabète, l’hypertension et les maladies cardiaques dans un échantillon nationalement représentatif d’adultes canadiens.
Méthodes
Cette étude a utilisé des données transversales provenant de 13 608 participants adultes (âgés de 19+ ans) dans le cadre de l’Enquête sur la santé dans les collectivités canadiennes 2015–nutrition. L’enquête a fourni des données sur la consommation alimentaire (rappel de 24h) et la prévalence de l’obésité mesurée (IMC ≥ 30 kg/m2), et le diabète, l’hypertension et les maladies cardiaques auto-rapportés. Tous les aliments et boissons consommés ont été classés selon la classification NOVA. La consommation d’aliments ultra-transformés a été estimée en utilisant l’apport énergétique relatif des aliments ultra-transformés. Des modèles de régression logistique multiple ont été utilisés pour vérifier l’association entre la consommation d’aliments ultra-transformés et l’obésité, le diabète, l’hypertension et les maladies cardiaques, en ajustant pour plusieurs facteurs sociodémographiques et comportementaux.
Résultats
En 2015, les aliments ultra-transformés ont contribué, en moyenne, à 24 % de l’apport énergétique quotidien total dans le tertile le plus bas de la consommation d’aliments ultra-transformés et 73 % dans le tertile le plus élevé. Comparativement au premier tertile, les adultes du tertile supérieur de la consommation d’aliments ultra-transformés avaient de chance 31 % plus élevée d’avoir l’obésité (RC = 1,31, IC 95% : 1,06-1,60), 37 % plus élevée d’avoir le diabète (RC = 1,37, IC 95% : 1,01-1,85), et 60 % plus élevée d’avoir l’hypertension (RC = 1,60, IC 95% : 1,26-2,03), en ajustant pour une gamme de variables.
Conclusion
Une consommation plus élevée d’aliments ultra-transformés est associée à une prévalence plus élevée d’obésité, de diabète et d’hypertension chez les adultes canadiens. Des stratégies et des politiques sont nécessaires pour décourager la consommation d’aliments ultra-transformés au Canada, ainsi que des stratégies qui rendent les aliments non transformés ou peu transformés plus abordables, disponibles et attrayants.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Unhealthy diets are a major modifiable risk factor of cardiometabolic disorders, including obesity, diabetes, hypertension and heart disease (Branca et al. 2019; Swinburn et al. 2019). After tobacco, excess weight and dietary risk factors are the second and third largest contributors to disease burden and premature death in Canada (Institute for Health Metrics and Evaluation 2018). Nearly one in three (28%) Canadian adults has obesity, one in four (25%) has hypertension, one in ten has diabetes (9%) and 6% have diagnosed cardiovascular disease (Diabetes Canada 2019; Public Health Agency of Canada 2017b).
A growing and compelling body of evidence suggests that the quality of diets is determined not only by specific foods or nutrients but also by dietary patterns and types of food processing (Hall et al. 2019; Monteiro et al. 2017). While many types of food processing are beneficial, ultra-processing often results in low-quality, energy-dense food products (Monteiro et al. 2019; Moubarac et al. 2017). The NOVA food classification system was developed in order to classify all foods according to the extent and purpose of industrial processing and classifies foods into four groups: (1) unprocessed and minimally processed foods, including fresh, frozen or dry fruits, vegetables, nuts, legumes and plain meats and milk; (2) processed culinary ingredients like salt, sugar, oils and butter; (3) processed foods, including canned fruits and vegetables; and (4) ultra-processed foods (Monteiro et al. 2017). Ultra-processed foods are industrial formulations made mostly from refined food substances and additives (Monteiro et al. 2017). Examples include carbonated drinks; packaged sweetened juices and drinks; mass-produced packaged breads, cakes, confectionary and ice cream; sweetened breakfast cereals; sweetened and flavoured yogurts and other milk-based drinks; packaged soups and noodles; margarine; and many ready-to-eat or ready-to-heat meals and “fast” foods and dishes (Monteiro et al. 2017).
The industrialization of food systems has facilitated the displacement of freshly prepared dishes and meals by ultra-processed foods and has profoundly changed the nature and quality of human diets worldwide (Monteiro et al. 2019; Moubarac et al. 2014). In high-income nations, the sales and consumption of ultra-processed foods remain very high despite having reached a plateau in the past one to two decades (PAHO 2015; Vandevijvere et al. 2019). In Canada, just under half of all daily energy intake, on average, comes from ultra-processed foods (Moubarac et al. 2017). Analyses of national dietary surveys from Canada and other high-income countries show dose-response associations between the dietary share of ultra-processed foods (i.e., % of total daily energy) and excessive intakes of free sugars, saturated fats and sodium, and lower intake of fibre (Monteiro et al. 2019). Also, the more ultra-processed foods consumed, the less fresh and minimally processed foods are eaten (including fruits, vegetables and legumes) (Moubarac et al. 2017).
A recent randomized controlled trial showed that diets based on ultra-processed foods cause excess energy intake and weight gain (Hall et al. 2019). However, the impact of ultra-processed foods goes beyond weight gain: a number of prospective studies show that consuming a diet high in ultra-processed foods increases the risk of developing a number of chronic conditions, including hypertension, cardiovascular disease, cancer, gastrointestinal disorders, and depression, and increases the risk of all-cause mortality (Monteiro et al. 2019). Collectively, this evidence suggests that consumption of ultra-processed food is a potent marker for diet quality and risk of non-communicable chronic disease. The 2019 Canada’s Food Guide now explicitly recommends limiting consumption of “highly processed foods,” defined as those contributing to excessive intake of sugars, sodium and saturated fats (Health Canada 2019).
To date, very few studies have explored the association between ultra-processed food intake and chronic disease in Canada. Using the most recent nationally representative data on dietary intakes of Canadian adults in 2015, this study assessed whether consumption of ultra-processed foods is associated with multiple cardiometabolic outcomes, namely, obesity, diabetes, hypertension and heart disease.
Methods
Data source
This study was based on data from the 2015 Canadian Community Health Survey (CCHS)–Nutrition, a survey with a total sample size of 20,487 participants (Health Canada 2017; Statistics Canada 2017). The survey’s target population were Canadian household residents aged 1+ living in the ten Canadian provinces. Excluded were full-time members of the Canadian Forces and individuals who lived on reserves or in other Indigenous settlements, in some remote areas, or in institutions. The survey contained two components: (1) general health and (2) 24-h dietary recalls of all food and beverages consumed in the previous 24 h of the interview day. All respondents completed one 24-h recall (data mainly collected in person) and a subset completed a second recall, 3–10 days later. The Automated Multiple Pass Method adapted for Canada was used to maximize participants’ recall of foods and drinks consumed. Data access was granted by Statistics Canada (under contract no. 18-SSH-MTL-5282-S001) and was analyzed at the Quebec Inter-University Centre for Social Statistics in Montreal, Quebec.
Study sample
The study sample were adult participants in the 2015 CCHS–Nutrition aged 19 years or older. We excluded pregnant and breastfeeding women (n = 303), participants who did not consume any calories in the previous day, and those with an invalid 24-h recall (n = 8). The final analytic sample was 13,608 adults.
Ultra-processed food consumption
Data from the first 24-h recall were used to estimate mean intakes at the population level (Thompson et al. 2015). All food and drinks (excluding alcohol drinks) were classified into the four NOVA groups as unprocessed and minimally processed foods; processed culinary ingredients; processed foods; or ultra-processed foods. Details of the classification procedures have been published previously (Moubarac et al. 2017). Consumption of ultra-processed food was defined as their relative energy contribution (% of total daily energy intake).
Cardiometabolic outcomes
We investigated four cardiometabolic outcomes: obesity, diabetes, hypertension and heart disease. Obesity (BMI ≥ 30 kg/m2) was estimated using measured height and weight values; however, for several reasons (refusal, problems with equipment, physical inability), heights and weights were not measured for about 30% of the survey participants. However, the majority of these individuals (85%) agreed to self-report their weight and height (Health Canada 2017). In the absence of data on measured height and weight, we corrected self-reported values using equations created based on 2004 CCHS–Nutrition data (Nardocci et al. 2018), following Gorber et al.’s (2008) methods. Diabetes, hypertension and heart disease were self-reported in the context of asking participants about long-term health conditions diagnosed by a health professional (i.e., “Do you have diabetes / high blood pressure / heart disease?”).
Covariates
Socio-demographic covariates included age (grouped as 19–30, 31–50, 51–64, 65+ years); sex; smoking status (non-smoker or smoker); leisure-time physical activity (min/week, continuous); alcohol consumption (% of energy intake, continuous); individual-level educational attainment (less than high school; high school; trade, college or CEGEP; or university diploma or above); household income adequacy (grouped into quintiles); residential zone (urban or rural); immigrant status (Canadian-born or immigrant); self-reported Indigenous identity (Indigenous or non-Indigenous); and energy reporting group (plausible energy reporter; under-reporter; over-reporter; described below). For obesity, we additionally controlled for measurement type (both height and weight measured; both height and weight reported; or one measured and the other reported).
Energy misreporting
Self-reported food intake data are subject to systematic misreporting: for instance, under-reporting is more frequent among adults with obesity and for foods perceived as less healthful (Health Canada 2017). To correct for energy misreporting, we compared participants’ reported energy intake (EI) with the estimated energy requirement (EER) to identify plausible and implausible energy reporters (under- or over-reporters), based on previously described methods (Garriguet 2008). A ratio of EI:EER below 0.70 classified energy under-reporters and a ratio above 1.49 classified energy over-reporters. Because these equations are not available for underweight individuals, this variable was not calculated for those with BMI < 18.5 kg/m2 (n = 249) and for those with missing values for weight and height (measured or self-reported, n = 685) and physical activity (n = 31).
Statistical analyses
Descriptive characteristics of participants and the prevalence of cardiometabolic outcomes were generated overall and by tertiles of ultra-processed food consumption. Differences across tertiles were tested using χ2 tests (for categorical variables) and ANOVA (for continuous variables).
To assess the association between consumption of ultra-processed foods and self-reported cardiometabolic outcomes, we generated a series of logistic regression models for each health outcome separately. We modelled ultra-processed food consumption as a continuous variable (per 10% increase in relative intake) and divided into tertiles. Covariates were informed by previous literature and selected for each health outcome separately. Model 1 was unadjusted for any covariates, model 2 was adjusted for age and sex and model 3 was adjusted for age, sex, smoking status, physical activity, educational attainment, income, residential zone, immigrant status, and self-reported Indigenous identity. For hypertension and heart disease, model 3 was additionally adjusted for alcohol consumption. For obesity, model 3 was additionally adjusted for alcohol consumption, measurement type and energy reporting group. Because previous reports showed that the effect of ultra-processed food intake on health may vary across socio-demographic characteristics (Juul et al. 2018; Louzada et al. 2015), we tested for interactions between the energy contribution of ultra-processed foods and age, sex and education by adding multiplicative interactions terms to each model 3, one at a time (alpha set at 0.10). Where significant interactions were found, stratified models were generated in addition to the main effect models.
Two sensitivity analyses were performed to test the robustness of findings to alternative variable and model specifications. These were (i) adjusting the final models for diabetes, hypertension and heart disease for energy reporting group and (ii) modelling weight status as BMI (kg/m2, continuous), using linear regression.
All analyses were conducted in SAS 9.4 and applied survey sampling weights provided by Statistics Canada to account for the complex sampling design and unequal probability of selection. Bootstrap weights were used to calculate robust standard errors using the Balanced Repeated Replication method. Alpha level was set at 0.05, unless otherwise specified.
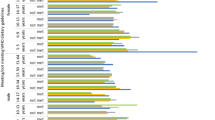
Results
Canadian adults consumed, on average, 1819 kcal per day, 47% of which came from ultra-processed foods (Table 1). The energy contribution of ultra-processed foods in the diet ranged from an average of 24% of total energy intake among Canadians with the lowest levels of ultra-processed food consumption (tertile 1), to 48% in the second tertile and 73% in the highest consumption group (tertile 3). Compared with participants in the lowest tertile, individuals in the highest consumption tertile were less likely to have a university diploma, to be an immigrant, and to live in rural areas, and more likely to be younger, to self-identify as Indigenous, to smoke, and to be more physically active. The prevalence of obesity and of self-reported diabetes, hypertension and heart disease in the study sample was 26%, 7%, 20% and 5%, respectively.
Consumption of ultra-processed foods was significantly associated with increased odds of obesity, diabetes and hypertension (Table 2). In models adjusted for the full range of covariates, a 10-percentage-point increase in the relative energy intake of ultra-processed foods was associated with 6% higher odds of obesity and diabetes and 9% higher odds of hypertension. Likewise, adults in the highest tertile of ultra-processed food consumption had 31%, 37% and 60% higher odds of obesity, diabetes and hypertension, respectively, compared with the lowest consumers. For heart disease, the association was positive but not statistically significant in the fully adjusted model. Similar results were obtained when the final models for diabetes, hypertension and heart disease were additionally adjusted for energy reporting group (data not shown), and when weight status was modelled as BMI (Table S1).
Significant interactions were found between the energy contribution of ultra-processed food with education level in the obesity model (p value for interaction = 0.01), and with age in the hypertension model (p = 0.09). As a result, stratified models were also generated (Table 3). The odds of obesity related to high levels of ultra-processed food intake was most pronounced among adults with a university diploma (OR = 2.17, 95% CI: 1.45–3.24, for tertile 3 vs. tertile 1), while no association was observed among adults with a high school degree or less. For hypertension, the effects of greater levels of ultra-processed food consumption showed some variation by age group: associations were strongest among adults aged 19 to 50, followed by older adults aged 65 or older, and elevated but not significant among those aged 51–64.
Discussion
This study provides the first Canadian evidence that consuming high levels of ultra-processed foods is associated with elevated prevalence of multiple cardiometabolic outcomes, namely, obesity and self-reported diabetes and hypertension. These results are not surprising considering that Canadians consume, on average, almost half of their daily energy intake from ultra-processed foods (Moubarac et al. 2017) and that diets high in ultra-processed foods tend to be energy dense and high in nutrients associated with an elevated risk of cardiometabolic disorders (e.g., sodium, saturated fat, free sugar) and low in fibre and foods beneficial to cardiometabolic health, like fruits and vegetables (Monteiro et al. 2019; Moubarac et al. 2017). A growing number of studies from multiple countries document the detrimental effects of ultra-processed food consumption on a range of health outcomes (Monteiro et al. 2019).
This study’s findings related to obesity prevalence are consistent with results of a previous cross-sectional study based on the 2004 CCHS–Nutrition data which similarly showed that consumption of high levels of ultra-processed foods was associated with 32% higher odds of obesity among Canadian adults (Nardocci et al. 2018). In the United States, another cross-sectional study based on national-level dietary intake data found positive associations between consumption of ultra-processed foods with overweight, obesity and abdominal obesity (Juul et al. 2018). A prospective study of Spanish middle-aged adults found that those in the highest quartile of ultra-processed food intake had a 26% higher risk of developing overweight or obesity compared with individuals in the first quartile (Mendonça et al. 2016a). A recent 1-month randomized controlled trial compared ultra-processed vs. non-ultra-processed diets (i.e., based on fresh or minimally processed foods, processed ingredients and processed foods) and found that the former led to increased energy intake and weight gain. According to the authors, the observed gain in body weight cannot be solely explained by nutrient composition, since both the ultra-processed and non-ultra-processed diets were matched to offer the same amounts of calories, sugar, fat, sodium, fibre and macronutrients (Hall et al. 2019). Additional evidence from longitudinal and experimental studies would help to elucidate the relative influence of various aspects of ultra-processed foods (e.g., nutrient content, food additives, energy density) on weight gain and health (Lawrence and Baker 2019).
This study also documented a positive association between high levels of ultra-processed food intake and prevalence of diabetes. Our findings are in line with those from a large prospective study of over 100,000 French adults which, to our knowledge, is the only other study to examine the association of ultra-processed food intake with diabetes (Srour et al. 2019a). Over a median follow-up of 6 years, every additional 10% in the proportion (in weight) of ultra-processed foods in the diet increased the risk of developing type 2 diabetes by 15% (Srour et al. 2019a). The results remained statistically significant even after adjustment for several markers of dietary quality, other metabolic comorbidities, and weight change.
This study’s finding of a positive association between the relative share of ultra-processed foods in the diet and hypertension is in line with those from a prospective cohort study of over 14,000 adult university graduates from Spain (Mendonça et al. 2016b). Participants in the highest tertile of ultra-processed food consumption at baseline had a 21% higher risk of developing hypertension than those in the lowest tertile over a median 9-year follow-up after adjusting for a number of potential confounders, including total energy intake and family history of hypertension. High intakes of specific ultra-processed foods and drinks (e.g., processed meats and sugar-sweetened beverages) have also been directly linked to higher risk of hypertension (Lajous et al. 2014; Xi et al. 2015).
Our study found a positive but non-significant association between a greater relative share of ultra-processed food in the diet and heart disease after adjusting for a range of confounders. Because of the cross-sectional nature of our study, it is possible that adults diagnosed with heart disease or other cardiometabolic outcomes may have adopted healthier diets as a means of controlling their condition, which would have obscured or attenuated any association. A recent prospective cohort study from France showed that a 10% increase in usual intake of ultra-processed foods (as % of total food and drink weight consumed) was associated with 12% increased risk of cardiovascular disease and 13% increased risk for coronary heart disease (Srour et al. 2019b). Another recent study based on national-level dietary recall data of US adults found a graded inverse association between the proportion of energy from ultra-processed foods consumed in a typical day and an overall measure of cardiovascular health (Zhang et al. 2020).
This study assessed whether the association between ultra-processed food intake and health varies by sex, age and education. For obesity prevalence, we did not observe heterogeneous effects by age or sex, consistent with a previous Canadian study but contrary to analyses from the USA and Brazil (Juul et al. 2018; Louzada et al. 2015; Nardocci et al. 2018). However, the odds of obesity were highest among adults with a university diploma and no association was observed among those with high school or less. While reasons for this finding are unclear, a partial explanation may be higher levels of physical activity reported by adults with lower levels of education in our sample (data not shown), which may relate to higher levels of occupational physical activity or higher proportion of physically active younger adults who have yet to complete their post-secondary education. For hypertension prevalence, the effect of higher levels of ultra-processed food consumption was more pronounced among adults aged 19–50 than among those aged 51 or older. These results are difficult to explain and merit confirmation in other populations and settings.
This study’s findings should be interpreted in light of a number of caveats. First, because of the cross-sectional nature of this study, our findings cannot be used to draw causal inferences and are subject to reverse causality: that is, the health status of the participants could have influenced their consumption of ultra-processed foods. The likely effect of this would be a dilution of the true association between ultra-processed foods intake and chronic disease. Second, this study used data from a single dietary recall to estimate mean intake at the population level, which may not represent usual intake (due to day-to-day variation in a person’s diet, a type of random measurement error). Random error can bias the results toward the null, attenuating the association between ultra-processed food consumption and cardiometabolic outcomes. However, because ultra-processed foods are ubiquitously consumed in the Canadian diet, the impact of day-to-day variation is expected to be minor (Kirkpatrick et al. 2019). Third, diabetes, hypertension and heart disease were self-reported by survey respondents and could not be verified against clinical records; medication use was also not assessed in this survey. This study could not distinguish between type 1 and type 2 diabetes; however, 90% of Canadian adults with diabetes have type 2 diabetes (Public Health Agency of Canada 2017a). Fourth, misclassification of foods and drinks according to the NOVA system cannot be ruled out. However, this misclassification would be non-differential between cases and non-cases, with the potential to bias results towards the null. Fifth, all self-reported food intake data are subject to misreporting. To address this, models were adjusted for energy reporting group. Additionally, if systematic misreporting were present (e.g., higher rates of energy under-reporting among persons with obesity or under-reporting of certain ultra-processed foods) (Health Canada 2017), then this would result in an underestimation of observed associations. Finally, although these analyses were adjusted for a slate of potential confounders, as with any observational study, the results may be subject to some degree of residual confounding, which can bias results in any direction.
Strengths of this study include the use of a large, nationally representative sample of Canadian adults, which makes results highly generalizable. Dietary intake assessment was based on 24-h food recalls collected using the Automated Multiple Pass Method adapted for Canada, which represents the most robust self-reported dietary data available. Additionally, the availability of socio-demographic and lifestyle information on the survey allowed for adjustment for a range of important covariates, as well as subgroup analyses.
Conclusion
This study provides the first Canadian evidence that diets based on ultra-processed foods are associated with higher prevalence of multiple cardiometabolic outcomes, namely, obesity, diabetes and hypertension. This evidence is consistent with a growing body of research, including from prospective and controlled studies, which documents that diets high in ultra-processed foods are associated with poorer overall diet quality, weight gain and increased risk of a range of cardiometabolic disorders (Hall et al. 2019; Monteiro et al. 2019). While further evidence from longitudinal and experimental studies would help to establish causality and elucidate the relative influence of various aspects of ultra-processed foods (e.g., nutrient content, additives, energy density) on health (Lawrence and Baker 2019), the accumulating evidence calls for urgent action to limit consumption of ultra-processed foods, consistent with the precautionary principle. The 2019 Canada’s Food Guide recommendations to “cook more often” and to choose fresh or minimally processed food on a daily basis over “highly processed foods” (Health Canada 2019) are a step in the right direction. A coordinated and comprehensive set of strategies and policies is needed to discourage consumption of ultra-processed foods in Canada and to make unprocessed or minimally processed foods more affordable, available and appealing. These can include advertising restrictions and taxation of ultra-processed foods, the reintroduction of cooking classes in school curricula, and support for industry actions to produce less processed foods.
References
Branca, F., Lartey, A., Oenema, S., Aguayo, V., Stordalen, G. A., Richardson, R., Arvelo, M., & Afshin, A. (2019). Transforming the food system to fight non-communicable diseases. BMJ, 364, l296. https://doi.org/10.1136/bmj.l296.
Diabetes Canada. (2019). Diabetes in Canada. Prevalence and costs. https://www.diabetes.ca/getmedia/a13c0439-fae8-488d-a90b-7a28f1899386/2019-Backgrounder-Canada.pdf.aspx
Garriguet, D. (2008). Impact of identifying plausible respondents on the under-reporting of energy intake in the Canadian Community Health Survey. Health Reports, 19(4), 47–55.
Gorber, S. C., Shields, M., Tremblay, M. S., & McDowell, I. (2008). The feasibility of establishing correction factors to adjust self-reported estimates of obesity. Health Reports, 19(3), 71–82.
Hall, K. D., Ayuketah, A., Bernstein, S., Brychta, R., Cai, H., Cassimatis, T., Chen, K. Y., Chung, S. T., Costa, E., Courville, A., Darcey, V., Fletcher, L. A., Forde, C. G., Gharib, A. M., Guo, J., Howard, R., Joseph, P. V., McGehee, S., Ouwerkerk, R., … Zhou, M. (2019). Ultra-processed diets cause excess calorie intake and weight gain: a one-month inpatient randomized controlled trial of ad libitum food intake. NutriXiv. https://doi.org/10.31232/osf.io/w3zh2.
Health Canada. (2017). Reference guide to understanding and using the data: 2015 Canadian Community Health Survey-Nutrition. http://www.deslibris.ca/ID/10093153
Health Canada. (2019). Canada’s food guide. https://food-guide.canada.ca/
Institute for Health Metrics and Evaluation. (2018). Canada profile. http://www.healthdata.org/canada
Juul, F., Steele, E. M., Parekh, N., Monteiro, C. A., & Chang, V. W. (2018). Ultra-processed food consumption and excess weight among US adults. The British Journal of Nutrition, 120(1), 90–100. https://doi.org/10.1017/S0007114518001046.
Kirkpatrick, S. I., Baranowski, T., Subar, A. F., Tooze, J. A., & Frongillo, E. A. (2019). Best practices for conducting and interpreting studies to validate self-report dietary assessment methods. Journal of the Academy of Nutrition and Dietetics, 119(11), 1801–1816. https://doi.org/10.1016/j.jand.2019.06.010.
Lajous, M., Bijon, A., Fagherazzi, G., Rossignol, E., Boutron-Ruault, M.-C., & Clavel-Chapelon, F. (2014). Processed and unprocessed red meat consumption and hypertension in women. The American Journal of Clinical Nutrition, 100(3), 948–952. https://doi.org/10.3945/ajcn.113.080598.
Lawrence, M. A., & Baker, P. I. (2019). Ultra-processed food and adverse health outcomes. BMJ, 365. https://doi.org/10.1136/bmj.l2289.
Louzada, M. L. d. C., Baraldi, L. G., Steele, E. M., Martins, A. P. B., Canella, D. S., Moubarac, J.-C., Levy, R. B., Cannon, G., Afshin, A., Imamura, F., Mozaffarian, D., & Monteiro, C. A. (2015). Consumption of ultra-processed foods and obesity in Brazilian adolescents and adults. Preventive Medicine, 81, 9–15. https://doi.org/10.1016/j.ypmed.2015.07.018.
Mendonça, R. de D., Pimenta, A. M., Gea, A., de la Fuente-Arrillaga, C., Martinez-Gonzalez, M. A., Lopes, A. C. S., & Bes-Rastrollo, M. (2016a). Ultraprocessed food consumption and risk of overweight and obesity: the University of Navarra Follow-Up (SUN) cohort study. The American Journal of Clinical Nutrition. https://doi.org/10.3945/ajcn.116.135004
Mendonça, R., de D., Lopes, A. C. S., Pimenta, A. M., Gea, A., Martinez-Gonzalez, M. A., & Bes-Rastrollo, M. (2016b). Ultra-processed food consumption and the incidence of hypertension in a Mediterranean cohort: the Seguimiento Universidad de Navarra Project. American Journal of Hypertension. https://doi.org/10.1093/ajh/hpw137.
Monteiro, C. A., Cannon, G., Moubarac, J.-C., Levy, R. B., da Louzada, M. L., C., & Jaime, P. C. (2017). The UN Decade of Nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutrition, 1–13. https://doi.org/10.1017/S1368980017000234.
Monteiro, C. A., Cannon, G., Lawrence, M., Louzada, M. L. da C, & Machado, P. P. (2019). Ultra-processed foods, diet quality, and health using the NOVA classification system. FAO.
Moubarac, J.-C., Batal, M., Martins, A. P. B., Claro, R., Levy, R. B., Cannon, G., & Monteiro, C. A. (2014). Processed and ultra-processed food products: consumption trends in Canada from 1938 to 2011. Canadian Journal of Dietetic Practice and Research 75(1), 15–21. https://doi.org/10.3148/75.1.2014.15.
Moubarac, J.-C., Batal, M., da Louzada, M. L., C., Steele, E. M., & Monteiro, C. A. (2017). Consumption of ultra-processed foods predicts diet quality in Canada. Appetite, 108, 512–520. https://doi.org/10.1016/j.appet.2016.11.006.
Nardocci, M., Leclerc, B.-S., da Louzada, M. L., C., Monteiro, C. A., Batal, M., & Moubarac, J.-C. (2019). Consumption of ultra-processed foods and obesity in Canada. Canadian Journal of Public Health 110(1), 4–14.
PAHO. (2015). Ultra-processed food and drink products in Latin America: trends, impact on obesity, policy implications. Pan American Health Organization. http://www.paho.org/hq/index.php?option=com_content&view=article&id=11153%3Aultra-processed-food-and-drink-products&catid=4999%3Adocuments&Itemid=0&lang=en
Public Health Agency of Canada. (2017a). Diabetes in Canada: highlights from the Canadian Chronic Disease Surveillance System. Public Health Agency of Canada. http://publications.gc.ca/collections/collection_2018/aspc-phac/HP35-94-2017-eng.pdf
Public Health Agency of Canada. (2017b). Canadian chronic disease indicators, Quick Stats, 2017 Edition. Canadian Chronic Disease Indicators, Quick Stats, 2017 Edition., 37(8), 248–251.
Srour, B., Fezeu, L. K., Kesse-Guyot, E., Allès, B., Chazelas, E., Deschasaux, M., Hercberg, S., Monteiro, C. A., Julia, C., & Touvier, M. (2019a). Ultra-processed food intake and risk of type 2 diabetes in a French cohort of middle-aged adults. European Journal of Public Health, 29(Supplement_4). https://doi.org/10.1093/eurpub/ckz185.388.
Srour, B., Fezeu, L. K., Kesse-Guyot, E., Allès, B., Méjean, C., Andrianasolo, R. M., Chazelas, E., Deschasaux, M., Hercberg, S., Galan, P., Monteiro, C. A., Julia, C., & Touvier, M. (2019b). Ultra-processed food intake and risk of cardiovascular disease: prospective cohort study (NutriNet-Santé). BMJ, 365. https://doi.org/10.1136/bmj.l1451.
Statistics Canada. (2017). 2015 Canadian Community Health Survey (CCHS) – nutrition. User: Guide.
Swinburn, B. A., Kraak, V. I., Allender, S., Atkins, V. J., Baker, P. I., Bogard, J. R., Brinsden, H., Calvillo, A., Schutter, O. D., Devarajan, R., Ezzati, M., Friel, S., Goenka, S., Hammond, R. A., Hastings, G., Hawkes, C., Herrero, M., Hovmand, P. S., Howden, M., … Dietz, W. H. (2019). The global syndemic of obesity, undernutrition, and climate change: The Lancet Commission report. Lancet, 0(0). https://doi.org/10.1016/S0140-6736(18)32822-8.
Thompson, F. E., Kirkpatrick, S. I., Krebs-Smith, S. M., Reedy, J., Schap, T. E., Subar, A. F., & Wilson, M. M. (2015). The National Cancer Institute’s Dietary Assessment Primer: a resource for diet research. Journal of the Academy of Nutrition and Dietetics, 115(12), 1986–1995. https://doi.org/10.1016/j.jand.2015.08.016.
Vandevijvere, S., Jaacks, L. M., Monteiro, C. A., Moubarac, J.-C., Girling-Butcher, M., Lee, A. C., Pan, A., Bentham, J., & Swinburn, B. (2019). Global trends in ultraprocessed food and drink product sales and their association with adult body mass index trajectories. Obesity Reviews : An Official Journal of the International Association for the Study of Obesity, 20(Suppl 2), 10–19. https://doi.org/10.1111/obr.12860.
Xi, B., Huang, Y., Reilly, K. H., Li, S., Zheng, R., Barrio-Lopez, M. T., Martinez-Gonzalez, M. A., & Zhou, D. (2015). Sugar-sweetened beverages and risk of hypertension and CVD: a dose-response meta-analysis. The British Journal of Nutrition, 113(5), 709–717. https://doi.org/10.1017/S0007114514004383.
Zhang, Z., Jackson, S. L., Martinez, E., Gillespie, C., & Yang, Q. (2020). Association between ultraprocessed food intake and cardiovascular health in US adults: A cross-sectional analysis of the NHANES 2011–2016. The American Journal of Clinical Nutrition. https://doi.org/10.1093/ajcn/nqaa276
Funding
This study was funded by the Heart and Stroke Foundation of Canada.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and analysis were performed by Milena Nardocci, Jane Y. Polsky and Jean-Claude Moubarac. The first draft of the manuscript was written by Milena Nardocci and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 28 kb)
Rights and permissions
About this article
Cite this article
Nardocci, M., Polsky, J.Y. & Moubarac, JC. Consumption of ultra-processed foods is associated with obesity, diabetes and hypertension in Canadian adults. Can J Public Health 112, 421–429 (2021). https://doi.org/10.17269/s41997-020-00429-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.17269/s41997-020-00429-9