Abstract
Objectives
Pre-exposure prophylaxis (PrEP) is a highly effective, HIV prevention strategy increasingly being accessed by gay, bisexual, and other men who have sex with men (GBMSM). GBMSM face structural and individual-level barriers accessing PrEP, including awareness and cost. This paper assesses socio-demographic factors associated with awareness, interest, and willingness to pay for PrEP in a sample of Canadian GBMSM.
Methods
Data were derived from the 2015 Sex Now survey, a cross-sectional, online survey of GBMSM. Respondents were recruited through social media, sex-seeking “apps,” and by word of mouth. We used univariable and multivariable logistic regression models to estimate associations between socio-demographic factors and three primary outcomes.
Results
Our sample consisted of 7176 HIV-negative Canadian GBMSM. Of respondents, 54.7% were aware of PrEP, 47.4% were interested in PrEP, and 27.9% of PrEP-interested respondents reported they would pay for PrEP out-of-pocket. Awareness and interest varied between provinces, while GBMSM outside urban areas were less likely to be PrEP aware. Bisexual-identified men, and men over 50, were less likely to be aware and interested in PrEP in multivariable models. Only annual income and educational attainment were associated with willingness to pay for PrEP.
Conclusion
This study identifies important disparities in awareness, interest, and willingness to pay for PrEP. Future interventions and educational efforts should target non-gay-identified and older GBMSM, as well as GBMSM outside urban areas. PrEP implementation may risk further perpetuating existing health inequities based on socio-economic status if PrEP continues to be accessed primarily through private insurance or paid for out-of-pocket.
Résumé
Objectif
La prophylaxie préexposition (PrEP) est. une stratégie de prévention du VIH très efficace, de plus en plus utilisée par les hommes gais et bisexuels et les hommes ayant des relations sexuelles avec d’autres hommes (GBHARSAH). Par contre, les GBHARSAH sont confrontés à des obstacles structurels et individuels face à l’accès à la PrEP, y compris la connaissance de la PrEP et les coûts. Cet article évalue les facteurs sociodémographiques associés à la connaissance, l’intérêt et la volonté de payer pour la PrEP dans un échantillon de GBHARSAH canadiens.
Méthode
Les données proviennent de l’enquête Sexe au présent 2015, un sondage en ligne de GBHARSAH. Les répondants ont été recrutés par le biais des médias sociaux, des applications de rencontre et du bouche-à-oreille. Nous avons utilisé des modèles de régression logistique univariée et multivariée pour mesurer les associations entre les facteurs sociodémographiques et les trois principales variables de résultats.
Résultats
Notre échantillon comprenait 7176 GBHARSAH canadiens séronégatifs. En tout, 54,7% des répondants étaient au courant de la PrEP, 47,4% des répondants étaient intéressés par la PrEP, et 27,9% des répondants intéressés par la PrEP ont indiqué qu’ils seraient prêts à payer pour la PrEP. La connaissance et l’intérêt envers la PrEP variaient d’une province à l’autre, tandis que les GBHARSAH en dehors des zones urbaines étaient moins susceptibles de connaitre la PrEP. Les hommes bisexuels et les hommes de plus de 50 ans étaient moins susceptibles de connaître et d’être intéressés par la PrEP dans les modèles multivariés. Seul le revenu annuel et le niveau de scolarité étaient associés à la volonté de payer pour la PrEP.
Conclusion
Cette étude a identifié des disparités importantes dans la connaissance, l’intérêt et la volonté de payer pour la PrEP. Les interventions et les efforts d’éducation devraient cibler les GBHARSAH qui ne s’identifient pas comme gai, les GBHARSAH plus âgés, ainsi que les GBHARSAH en dehors des zones urbaines. De plus, la mise en œuvre de la PrEP risque de perpétuer davantage les inégalités existantes en matière de santé en fonction du statut socioéconomique si la PrEP continue d’être accessible principalement par le biais d’une assurance privée ou si les GBHARSAH doivent payer pour celle-ci.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pre-exposure prophylaxis (PrEP) is a highly effective, evidence-based, biomedical HIV prevention strategy that involves taking daily oral antiretroviral (ARV) medication (tenofovir disoproxil fumarate–emtricitabine; TDF-FTC) on an ongoing basis, prior to and after potential exposure to HIV (Lachowsky et al. 2016). Use of TDF-FTC for PrEP was approved by the United States (US) Food and Drug Administration (FDA) in July 2012 and by Health Canada in February 2016. Since its approval, PrEP has increasingly been incorporated into comprehensive HIV prevention strategies in the US and Canada, with a primary focus on gay, bisexual, and other men who have sex with men (GBMSM) (Stahlman et al. 2017; Underhill et al. 2016), as this demographic continues to account for the majority of new HIV infections in North America (Public Health Agency of Canada 2014). Despite the potential for PrEP to be an effective HIV prevention tool for GBMSM, there remain fundamental barriers to its uptake in the Canadian context (King et al. 2014).
GBMSM face both structural and individual-level barriers effectively accessing PrEP (Knight et al. 2016). Documented individual-level barriers include health and risk literacy (Knight et al. 2016; Young et al. 2014); concerns about drug toxicity, side effects, and effectiveness (King et al. 2014; Golub et al. 2013); and need for adherence to medication once started on PrEP (Mayer et al. 2015; Oldenburg et al. 2016). Lack of awareness of PrEP also constitutes a significant individual-level barrier to access, and has been shown to differ significantly among GBMSM (Lachowsky et al. 2016; Rucinski et al. 2013). Structural-level barriers include physicians' and nurse practitioners’ awareness and willingness to prescribe, or provide necessary follow-up care, for PrEP (Smith et al. 2016; Connif and Evensen 2016); stigmatization (Knight et al. 2016); and cost (King et al. 2014). Indeed, the cost of non-generic formulations of TDF-FTC for PrEP can exceed CAD$1000 per month, which ultimately limits its uptake for those without third party insurance, in the absence of provincial funding mechanisms (King et al. 2014). Individual willingness to pay may be considered an individual-level attribute that reflects both personal inclination to spend money on medication like PrEP, as well as structural barriers related to cost. Together, these barriers may contribute to inequities in the uptake of PrEP.
Eligible GBMSM in Canada currently access PrEP through a variety of means, including private insurance, government health programs, or out-of-pocket. Currently, only the provinces of British Columbia, Ontario, and Quebec, and the First Nations and Inuit Health Branch—a federally funded program responsible for health services and prescription drugs for Indigenous and Inuit people across Canada—publicly fund PrEP for eligible members. Elsewhere, PrEP is principally accessed through private or employer insurance, although there have been media reports that some private insurance carriers have removed PrEP from their formularies (Bell 2016; Himpe 2017). Generic formulations of PrEP were approved by Health Canada in 2017, although costs could remain as high as CAD$400 per month (CATIE 2017). To circumvent these cost-related barriers, some Canadians purchase generic PrEP from international pharmacies online, and import their prescription through the US, known as “buyers’ clubs” (Hibbard 2017). Given this complex and geographically varied coverage of PrEP, many Canadians continue to face cost-related barriers.
The purpose of this exploratory analysis is to assess socio-demographic factors associated with awareness of, interest in, and willingness to pay for PrEP, in a sample of Canadian GBMSM. Our goal is to identify subpopulations in the Canadian context which may face disproportionately greater barriers in accessing PrEP, such as cost, or could benefit from targeted PrEP awareness campaigns. Ultimately, these findings can help design interventions to maximize the success of PrEP implementation in Canada, and reduce inequities in its uptake. We hypothesize that both individual characteristics and willingness to pay—a proxy for structural-level barriers related to cost—will impact respondents’ ability to access PrEP, particularly among respondents with fewer social and economic resources that are often required to access health innovation (Link and Phelan 1995).
Methods
Data for this study were derived from Sex Now 2015, a national periodic, community-based, cross-sectional survey of GBMSM in Canada. The Sex Now Survey is stewarded by the Community-Based Research Centre for Gay Men’s Health, a non-profit charitable organization dedicated to community-based and participatory research, based in Vancouver, British Columbia. The survey was conducted between November 2014 and April 2015, offered anonymously in English and French. Respondents were recruited online through social media, sex-seeking web-based mobile phone “apps” and websites, an email invitation sent to past survey respondents, and by word of mouth. The 2015 Sex Now survey was run in collaboration with a group of youth peer researchers, called the Investigaytors, who contributed to all phases of the study, including survey development, analysis, and communicating the results (including the current report).
Ethics
The research ethics committee of the Community-Based Research Centre for Gay Men’s Health reviewed and approved this study.
Measures
Awareness of PrEP
Respondents were provided with the following definition of PrEP: “Pre Exposure Prophylaxis is a daily antiretroviral medication now available for HIV negative men that can prevent sexual transmission of HIV (not yet approved in Canada [at time of data collection]).” Respondents were asked: “Were you previously aware [of PrEP] before taking this survey?”, and could respond with “no” or “yes.” Those who answered “yes” were considered aware of PrEP.
Interest in PrEP
To gauge interest in PrEP, respondents were provided with a supplementary definition of PrEP: “PrEP is a new drug-based approach to HIV prevention that uses an antiretroviral medication, Truvada—normally applied in treatment—to help prevent new HIV infections from establishing.” Respondents were asked: “How interested would you be in taking a daily medication for HIV prevention?” Possible responses included: “Yes… I’m interested”; “I’m already taking PrEP”; “I’ve taken PrEP but not longer on it”; “I’m HIV positive”; or “No… I’m not interested.” Only respondents who chose “Yes… I’m interested” were considered interested in PrEP. All other respondents were considered not interested in PrEP. Consistent with previous studies assessing awareness and interest in PrEP, HIV-positive participants were excluded from this analysis (Lachowsky et al. 2016; Leonardi et al. 2011; Snowden et al. 2017).
Willingness to pay for PrEP
Respondents who indicated they were interested in PrEP were subsequently asked: “What would be the maximum you would be willing to pay to access PrEP?”, hereafter referred to as “willingness to pay.” Possible responses included: “Only if covered by my health insurance,” hereafter referred to as “not willing to pay,” or “If less than (enter amount below) per month.” Respondents who chose the latter could indicate an amount between $100 and $1200, in increasing $100 increments. Respondents who selected any dollar amount per month were considered “willing to pay.” In univariable and multivariable models, willingness to pay was dichotomized as “willing to pay” and “not willing to pay.” Respondents who did not have health insurance may have selected “less than $100” to indicate they would be unwilling to pay for PrEP; to accommodate this potential limitation of the survey measure, a sensitivity analysis was performed, defining willingness to pay as any amount more than $100.
Respondent socio-demographics
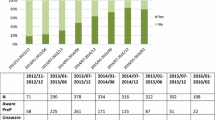
Respondents self-reported demographic characteristics, including their sexual orientation, ethnicity, annual personal income before tax, age, level of education, and geography (Table 1). Geography measures included environment (i.e., urban, suburban, or rural) and province of residence. Additional exclusion criteria included: participants who self-identified as women (and no other gender identity); respondents who reported they lived outside of Canada; as well as participants who did not complete the survey.
Statistical analyses
Only HIV-negative and HIV-untested respondents were included in this study. Analyses were conducted using IBM SPSS™ Statistics Version 21. First, we used binary logistic regression to estimate crude univariable associations between demographic factors and each of the three outcomes (i.e., awareness, interest, and willingness to pay). Subsequently, three separate multivariable logistic regression models were used to estimate adjusted associations between socio-demographic factors and each of the three outcomes. All multivariable models were adjusted for the respondents’ self-reported socio-demographics. Odds ratios (OR) were considered statistically significant if the 95% confidence interval (CI) did not include 1.
Results
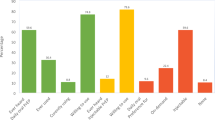
Our sample consisted of GBMSM who were HIV-negative (n = 5919) or had an unknown HIV status (n = 1257), for a total of 7176 respondents living in Canada. The demographic characteristics of respondents are detailed in Table 1. The median age was 42 (interquartile range 29–53 years). Overall, 54.7% (n = 3923) of respondents were aware of PrEP and 47.4% (n = 3399) of respondents reported they were interested in using PrEP. Of respondents who indicated they were interested in using PrEP, 72.1% (n = 2452) said they would only use PrEP if it was covered by their health insurance and the remainder (27.9%) were willing to pay out-of-pocket. The amount respondents were willing to pay for PrEP out-of-pocket per month is summarized in Fig. 1.
Correlates of awareness
Correlations between demographic characteristics and PrEP awareness, interest, and willingness to pay for PrEP are summarized in Table 2. In both univariable and multivariable models, PrEP awareness was positively associated with higher educational attainment (compared to completing some high school), while awareness was negatively associated with self-identifying as bisexual or other (compared to self-identifying as gay), being ≥ 30 years old (compared to ≤ 30), and living in non-urban areas (compared to urban areas). Awareness was not significantly associated with annual personal income in either the univariable or multivariable models.
Correlates of interest
In both univariable and multivariable models, interest in using PrEP was positively associated with respondents who self-reported non-white and non-Aboriginal ethnicity (compared to white). Conversely, interest was negatively associated with self-identifying as bisexual and “other” (compared to self-identifying as gay), being ≥ 50 years old (compared to ≤ 30), and holding a graduate degree (compared to some high school). In the univariable model, participants living in small cities/towns or in rural/remote environments were more interested in PrEP compared to those living in urban areas, although this association did not remain significant in the multivariable model when adjusted for other socio-demographic characteristics. Interest in PrEP was not significantly associated with annual personal income.
Correlates of willingness to pay
Only annual personal income and educational attainment were significantly associated with willingness to pay for PrEP out-of-pocket in either univariable or multivariable models. Compared to those earning < $20,000, respondents with an annual income ≥ $40,000 were more willing to pay for PrEP. Similarly, those with an undergraduate or graduate degree were more willing to pay for PrEP compared to respondents who completed high school.
Discussion
This study details awareness, interest, and willingness to pay for PrEP among a large sample of GBMSM across Canada. The national scope of the Sex Now survey allows for direct comparison between provinces, which is significant given that most PrEP research in the Canadian context has been conducted in large urban centres (Lachowsky et al. 2016; Young et al. 2014; Lebouché et al. 2016; Ko et al. 2016). Indeed, we found significant differences in awareness and interest in PrEP between provinces, even after adjusting for socio-demographic and behavioural characteristics. As funding models and interventions for PrEP are being considered across Canada, this research identifies populations that may benefit from additional PrEP education efforts or may face other individual-level barriers accessing PrEP. Ultimately, the results support an implementation strategy that offers financial or medication assistance to reduce demonstrated financial barriers that limit the uptake of this effective health innovation. Notwithstanding the importance of our findings related to high awareness and interest of future PrEP use, one of the novel contributions of our study is measuring GBMSM’s willingness to pay for PrEP out of pocket, which is particularly important given the impending Canadian decisions about funding models for PrEP. We first interpret these findings in the interest of helping policymakers to attend to these social differences in willingness to pay.
Our study found that willingness to pay for PrEP was significantly associated with respondents’ socio-economic status (SES), which we measured using educational attainment and annual income. While willingness to pay for PrEP is less documented in the literature, these data support findings reported elsewhere, which identify the high cost of PrEP as a barrier to uptake (King et al. 2014; Ko et al. 2016). Increased willingness to pay for PrEP among respondents with higher SES, as well as increased awareness of PrEP among respondents with higher educational attainment, is consistent with fundamental cause theory—first articulated by Link and Phelan (1995). Fundamental cause theory maintains that many associations between SES and negative health outcomes are explained by access to resources, which can be used to minimize or avoid the consequences of disease once (or before) it occurs (Link and Phelan 1995).
When considering new health innovations, such as PrEP, it holds that people with greater resources are more favourably positioned to know about, or have the means to access, new health technologies (Link and Phelan 1995; Rubin et al. 2010; Holloway et al. 2017; Allgood et al. 2016). The fact that educational attainment was positively associated with awareness and willingness to pay for PrEP out-of-pocket, but not with interest in PrEP, is consistent with fundamental causes theory: respondents with higher SES are more likely to know about, and have the means to access PrEP, despite being equally as interested in this health innovation as those with lower SES.
Despite data collection occurring before Health Canada approved the use of TDF-FTC for PrEP in 2016, awareness of PrEP in our sample was 55%. This finding is relatively high compared to previous estimates of PrEP awareness in Canada reported elsewhere between 2011 and 2013 (Lachowsky et al. 2016; Leonardi et al. 2011; Lebouché et al. 2016). Once respondents were informed of PrEP in the survey, 47% expressed interest in using PrEP. This finding likely reflects some proportion of GBMSM who do not perceive themselves to be “at-risk” for HIV, and therefore do not consider themselves as a prospective consumer of PrEP (Knight et al. 2016; Young et al. 2014; Parsons et al. 2017); this highlights the need for targeted education campaigns among GBMSM to improve knowledge regarding the benefits of PrEP. Moreover, such campaigns should specifically target populations this research identifies as being already less aware of PrEP, such as bisexual-identified and older men.
Awareness and interest in PrEP varied between provinces, with respondents in British Columbia reporting the highest level of awareness of PrEP (59.5%), and individuals living in the prairie provinces (i.e., Alberta, Saskatchewan, and Manitoba) reporting the highest level of interest in PrEP. High levels of interest in PrEP within Saskatchewan may be promising for future PrEP rollout in this province, particularly given that Saskatchewan has the highest rates of HIV in Canada (Public Health Agency of Canada 2014). While this study highlights significant differences between provinces broadly, future research should ask related questions “in context” to further identify province-specific barriers to PrEP access.
Perhaps unsurprisingly, awareness of PrEP was significantly higher in urban areas (60.7%), compared to among GBMSM living in suburban (50.3%), small city/town (44.1%), and rural and remote (48.0%) areas. This is consistent with geographic disparities in HIV literacy in the Canadian context more broadly, which suggests rurality is negatively associated with knowledge of HIV/AIDS, as well as the likelihood that people have talked about HIV/AIDS with others (Veinot and Harris 2011). These findings suggest that future PrEP interventions and educational efforts should extend beyond urban areas, as non-urban areas currently have significantly lower levels of awareness of this HIV prevention strategy.
Limitations
There are some important limitations that need to be considered when interpreting the current study results. First, the data were drawn from a cross-sectional Internet survey that used non-probability sampling strategies for recruitment; therefore, despite the large sample size, it is difficult to say to what extent this sample represents gay and bisexual men in Canada or elsewhere. Second, the online nature of the survey may have excluded some respondents, while oversampling those with strong ties to the GBMSM community and those who are educated and affluent, leading to an over-reporting of PrEP interest. Third, the data were collected before the approval of PrEP by Health Canada and as such may not represent the current state of awareness and interest. Continued monitoring of PrEP interest and willingness to pay is warranted. Fourth, we used the contingent valuation method to assess willingness to pay. Contingent valuation asks survey respondents how much they would be willing to pay for a particular good, and is widely used to measure the value of goods not traded in the marketplace (such as PrEP at the time of data collection) (Bradford et al. 2004). However, the contingent valuation method has several limitations and biases identified elsewhere, such as “starting point bias” and other response effects which may influence how respondents answer the question, particularly in cases when respondents have little direct experience with the product in question (Bradford et al. 2004; Klose 1999). Future research should consider other approaches to capture willingness to pay for PrEP to minimize response biases, such as the double-bounded dichotomous choice method. Finally, we did not consider how risk for HIV (e.g., number of sex partners) may relate to awareness, interest, or willingness to use PrEP, which has been shown to be associated with these outcomes (Lachowsky et al. 2016; Rucinski et al. 2013) and remains an important future research direction. For example, with regard to implementation, while providing PrEP to all eligible GBMSM would have the greatest overall impact on reducing new HIV infections and mortality, a dynamic modeling study in a Canadian context suggests this would not be cost-effective at the health systems level due to the high cost of PrEP. Instead, focusing PrEP uptake among the highest risk GBMSM was the most efficient approach to implementation (MacFadden et al. 2016).
Conclusions
These findings have important implications for future policy and interventions related to PrEP. In particular, this study has identified important disparities in awareness, interest, and willingness to pay for PrEP, which should be taken into consideration as PrEP becomes more widely available in Canada. While current PrEP efforts in Canada have largely targeted gay-identified MSM, future interventions and education efforts should extend to eligible non-gay-identified and older GBMSM, who may also benefit from PrEP. Finally, if PrEP continues to be accessed primarily through private insurance or out-of-pocket, or without publicly funded universal or SES-targeted access to PrEP, we risk perpetuating existing health inequities within GBMSM, as SES is already a known indicator for HIV infection and related mortality.
References
Allgood, K. L., Hunt, B., & Rucker, M. G. (2016). Black:white disparities in HIV mortality in the United States: 1990-2009. Journal of Racial and Ethnic Health Disparities, 3(1), 168–175.
Bell, N. (2016). Why a BC insurance company is backtracking on PrEP. Daily Xtra. May 5, 2016. Available at: https://www.dailyxtra.com/why-a-bc-insurance-company-is-backtracking-on-prep-70891. (Accessed 1 Oct 2017).
Bradford, W. D., Kleit, A. N., Krousel-Wood, M. A., & Re, R. M. (2004). Willingness to pay for telemedicine assessed by the double-bounded dichotomous choice method. Journal of Telemedicine and Telecare, 10(6), 325–330.
CATIE (2017). Generic tenofovir + FTC coming to Canada. CATIE. July 27, 2017. Available at: http://www.catie.ca/en/catienews/2017-07-27/generic-tenofovir-ftc-coming-canada. (Accessed 25 Oct 2017).
Connif, J., & Evensen, A. (2016). Preexposure prophylaxis (PrEP) for HIV prevention: the primary care perspective. Journal of American Board of Family Medicine, 29(1), 143–151.
Golub, S. A., Gamarel, K. E., Renina, H. J., Surace, A., & Lelutiu-Weinberger, C. L. (2013). From efficacy to effectiveness: facilitators and barriers to PrEP acceptability and motivations for adherence among MSM and transgender women in New York City. AIDS Patient Care and STDs, 27(4), 248–254.
Hibbard S. (2017) B.C. residents at risk of contracting HIV turn to online buyer’s club to afford pricey lifesaving drug. CBC. June 9, 2017. Available at: http://www.cbc.ca/news/canada/british-columbia/b-c-residents-at-risk-of-contracting-hiv-turn-to-online-buyer-s-club-to-afford-pricey-lifesaving-drug-1.4150345. (Accessed 25 Oct 2017).
Himpe J. Insurance coverage inconsistent for HIV prevention drug Truvada in Alberta. Global News. August 1, 2017. Available at: https://globalnews.ca/news/3604477/insurance-coverage-inconsistent-for-hiv-prevention-drug-truvada-in-alberta/. (Accessed 1 Oct 2017).
Holloway, I. W., Dougherty, R., Gildner, J., Beougher, S. C., Pulsipher, C., Montoya, J. A., et al. (2017). PrEP uptake, adherence, and discontinuation among California YMSM using geosocial networking applications. Journal of Acquired Immune Deficiency Syndromes, 74(1), 15–20.
King, H. L., Keller, S. B., Giancola, M. A., Rodriguez, D. A., Chau, J. J., Young, J. A., et al. (2014). Pre-exposure prophylaxis accessibility research and evaluation (PrEPARE Study). AIDS and Behavior, 18(9), 1722–1725.
Klose, T. (1999). The contingent valuation method in health care. Health Policy, 47, 97–123.
Knight, R., Small, W., Carson, A., & Shoveller, J. (2016). Complex and conflicting social norms: Implications for implementation of future HIV pre-exposure prophylaxis (PrEP) interventions in Vancouver, Canada. PLoS One, 11(1), e0146513.
Ko, N. Y., Chen, B. J., Li, C. W., Ku, W. W., & Hsu, S. T. (2016). Willingness to self-pay for pre-exposure prophylaxis in men who have sex with men: a national online survey in Taiwan. AIDS Education and Prevention, 28(2), 128–137.
Lachowsky, N. J., Lin, S. Y., Hull, M. W., Cui, Z., Sereda, P., Jollimore, J., et al. (2016). Pre-exposure prophylaxis awareness among gay and other men who have sex with men in Vancouver, British Columbia, Canada. AIDS and Behavior, 20(7), 1408–1422.
Lebouché, B., Engler, K., Machouf, N., Lessard, D., & Thomas, R. (2016). Predictors of interest in taking pre-exposure prophylaxis among men who have sex with men who used a rapid-HIV-testing site in Montreal (Actuel sur Rue). HIV Medicine, 17(2), 152–158.
Leonardi, M., Lee, E., & Tan, D. H. S. (2011). Awareness of, usage of and willingness to use HIV pre-exposure prophylaxis among men in downtown Toronto, Canada. International Journal of STD & AIDS, 22(12), 738–741.
Link, B. G., Phelan J. (1995). Social conditions as fundamental causes of disease. Journal of Health and Social Behavior. Spec No:80–94.
MacFadden, D. R., Tan, D. H., & Mishra, S. (2016). Optimizing HIV pre-exposure prophylaxis implementation among men who have sex with men in a large urban centre: a dynamic modelling study. Journal of the International AIDS Society, 19, 20791.
Mayer, K. H., Hosek, S., Cohen, S., Liu, A., Pickett, J., Warren, M., et al. (2015). Antiretroviral pre-exposure prophylaxis implementation in the United States: a work in progress. Journal of the International AIDS Society, 18(4 Suppl 3), 19980.
Oldenburg, C. E., Mitty, J. A., Biello, K. B., Closson, E. F., Safren, S. A., Mayer, K. H., et al. (2016). Differences in attitudes about HIV pre-exposure prophylaxis use among stimulant versus alcohol using men who have sex with men. AIDS and Behavior, 20(7), 1451–1460.
Parsons, J. T., Rendina, H. J., Lassiter, J. M., Whitfield, T. H., Starks, T. J., & Grov, C. (2017). Uptake of HIV pre-exposure prophylaxis (PrEP) in a national cohort of gay and bisexual men in the United States. Journal of Acquired Immune Deficiency Syndromes, 74(3), 285–292.
Public Health Agency of Canada (2014). HIV and AIDS in Canada: surveillance report to December 31, 2014. Ottawa: Minister of Public Works and Government Services Canada. 2014. Available at: http://healthycanadians.gc.ca/publications/diseases-conditions-maladies-affections/hiv-aids-surveillance-2014-vih-sida/alt/hiv-aids-surveillance-2014-vih-sida-eng.pdf. (N).
Rubin, M. S., Colen, C. G., & Link, B. G. (2010). Examinations of inequalities in HIV/AIDS mortality in the United States from a fundamental cause perspective. American Journal of Public Health, 100(6), 1053–1059.
Rucinski, K. B., Mensah, N. P., Sepkowitz, K. A., Cutler, B. H., Sweeney, M. M., & Myers, J. E. (2013). Knowledge and use of pre-exposure prophylaxis among an online sample of young men who have sex with men in New York City. AIDS and Behavior, 17(6), 2180–2184.
Smith, D. K., Mendoza, M. C. B., Stryker, J. E., & Rose, C. E. (2016). PrEP awareness and attitudes in a national survey of primary care clinicians in the United States, 2009-2015. PLoS One, 11(6), e0156592.
Snowden, J. M., Chen, Y.-H., McFarland, W., & Raymond, H. F. (2017). Prevalence and characteristics of users of pre-exposure prophylaxis among men who have sex with men, San Francisco, 2014 in a cross-sectional survey: implications for disparities. Sexually Transmitted Infections, 93(1), 52–55.
Stahlman, S., Lyons, C., Sullivan, P. S., Mayer, K. H., Hosein, S., Beyrer, C., et al. (2017). HIV incidence among gay men and other men who have sex with men in 2020: where is the epidemic heading? Sexual Health, 14(1), 5–17.
Underhill, K., Morrow, K. M., Colleran, C., Calabrese, S. K., Operario, D., Salovey, P., et al. (2016). Explaining the efficacy of pre-exposure prophylaxis (PrEP) for HIV prevention: a qualitative study of message framing and message preferences among US men who have sex with men. AIDS and Behavior, 20(7), 1514–1526.
Veinot, T. C., & Harris, R. (2011). Talking about, knowing about HIV/AIDS in Canada: a rural-urban comparison. The Journal of Rural Health, 27(3), 310–318.
Young, I., Flowers, P., & McDaid, L. M. (2014). Barriers to uptake and use of pre-exposure prophylaxis (PrEP) among communities most affected by HIV in the UK: findings from a qualitative study in Scotland. BMJ Open, 4(11), e005717.
Acknowledgements
The authors wish to thank all the respondents who participated in the 2015 Sex Now survey; Rick Marchand and Terry Trussler for their mentorship; and the Investigaytors other staff and volunteers of the Community-Based Research Centre for Gay Men’s Health who helped with survey design and recruitment.
Funding
The 2015 Sex Now survey was funded by the Vancouver Foundation. The opinions, results, and conclusions are those of the authors and no endorsement by the Ontario HIV Treatment Network or its funder is intended or should be inferred.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Morgan, J., Ferlatte, O., Salway, T. et al. Awareness of, interest in, and willingness to pay for HIV pre-exposure prophylaxis among Canadian gay, bisexual, and other men who have sex with men. Can J Public Health 109, 791–799 (2018). https://doi.org/10.17269/s41997-018-0090-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.17269/s41997-018-0090-1