Abstract
Objective
Medium-chain fatty acids (MCFAs) can rapidly cross the blood-brain barrier and provide an alternative energy source for the brain. This study aims to determine 1) whether plasma caprylic acid (C8:0) is associated with risk of incident mild cognitive impairment (MCI) among baseline cognitively normal (CN) participants, and incident Alzheimer’s Disease (AD) among baseline MCI participants; and 2) whether these associations differ by sex, comorbidity of cardiometabolic diseases, apolipoprotein E (APOE) ε4 alleles, and ADAS-Cog 13.
Methods
Within the Alzheimer’s Disease Neuroimaging Initiative (ADNI) cohort, plasma C8:0 was measured at baseline in 618 AD-free participants aged 55 to 91. Logistic regression models were used to estimate odds ratios (ORs) and 95% CIs with incident MCI and AD as dependent variables, separately.
Results
The inverse association between circulating C8:0 and risk of incident MCI was of borderline significance. The inverse association between circulating levels of C8:0 and risk of incident MCI was significant among CN participants with ≥1 cardiometabolic diseases [OR (95% CI): 0.75 (0.58–0.98) (P=0.03)], those with one copy of APOE ε4 alleles [OR (95% CI): 0.43 (0.21–0.89) (P=0.02)], female [OR (95% CI): 0.60 (0.38–0.94) (P=0.02)], and ADAS-Cog 13 above the median [OR (95%CI): 0.69 (0.50–0.97)(P=0.03)] after adjusting for all covariates.
Conclusion
The inverse associations were present only among subgroups of CN participants, including female individuals, those with one or more cardiometabolic diseases, or one APOE ε4 allele, or higher ADAS-Cog 13 scores. If confirmed, this finding will facilitate precision prevention of MCI, in turn, AD among CN older adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past two decades, mortality rates due to Alzheimer’s disease (AD) increased by 110% in the U.S., and 13.8 millions of Americans are expected to be affected by 2050 (1). To date, no FDA-approved drugs, including aducanumab have confirmed effects to stop or slow the damage to neurons that cause the progression of AD (2). A delay of five years in the expression of AD would reduce the incidence rate by 50% (3) and prevalence by 41% (4). Thus, the need to develop preventive strategies for AD cannot be overstated. A well-established characteristic of AD is brain glucose hypometabolism, which can appear decades before the manifestation of AD symptoms (5, 6). While the improvement in brain energy metabolism through a classic ketogenic diet with ultra-low-carbohydrate intake is associated with better cognitive outcomes in patients with AD or mild cognitive impairment (MCI) (7), the classic ketogenic diet is too strict to maintain long-term (8) and can lead to side effects (9–11). However, previous studies indicate that it produces ketone bodies, which in turn, rescue brain energy (12–16) and improve cognition (7, 17, 18).
Medium-chain fatty acids (MCFAs) are saturated fatty acids of 6–12 carbons in chain length. The main source of MCFAs are mammalian milk and tropical plant oils, such as coconut and palm kernel oils (19). In a precision-based randomized controlled trial, we recently found that in addition to dietary intake, MCFAs (i.e., C7:0 and C8:0) can also be produced by gut microbiota in humans through optimizing calcium: magnesium ratio by magnesium supplementation (20). In contrast to long-chain fatty acids, MCFAs can rapidly cross the blood-brain barrier (8), directly enter the mitochondrial matrix, have intramitochondrial conversion to acyl-CoA thioesters and be directly metabolized by the brain (21). Unlike other MCFAs (22), C12:0, i.e., lauric acid is structurally closer to saturated long-chain fatty acids and may increase blood levels of low-density lipoprotein (LDL) cholesterol (23). The ‘medium chain triglyceride (MCT) ketogenic diet’, designed as an alternative dietary approach comprising 60% caprylic acid (C8:0) and 40% capric acid (C10:0), has a more flexible carbohydrate restriction to treat drug-resistant epilepsy (8). Recent evidence has shown that an MCT ketogenic diet improved cognition in patients with AD or MCI (7, 8, 24). Three randomized, double-blind, placebo-controlled trials (25–27) and a retrospective case study (28) conducted in patients with mild cognitive impairment (MCI), or mild-to-moderate AD found that supplementation of MCT containing C8:0 regardless of C10:0 without any dietary restriction, significantly improved cognition. Although promising, these previous studies were short-term and were conducted among individuals with AD or MCI. It remains unclear whether C8:0 can prospectively prevent or predict the development of MCI and the progression from MCI to AD.
In addition to providing an alternative energy source, C8:0 is the precursor for the biosynthesis of alpha (α)-lipoic acid, which is essential in energy metabolism (29) and may delay AD development (30). Previous studies found that, while C10:0 prefers glycolysis, C8:0 undergoes β-oxidation to readily produce ketones in brain cells (8). Herein, we hypothesize that low circulating levels of C8:0 are associated with an increased risk for MCI (development from cognitively normal to MCI) or AD (progression from MCI to AD). We test our hypothesis in the Alzheimer’s Disease Neuroimaging Initiative (ADNI) cohort, a cohort with up to 13.4 years of follow-up among AD-free older adults. Since cardiometabolic diseases are a major risk factor for MCI and AD (31–33), and the MCT ketogenic diet improves insulin resistance in patients with cardiometabolic diseases (8, 34), we examined whether the associations between levels of C8:0 and risk of incident MCI and AD were stronger among high risk populations, i.e., those with cardiometabolic diseases and APOE ε4 alleles.
Methods
Study Cohort
Data used in the preparation of this article were obtained from the ADNI database (adni.loni.usc.edu). The ADNI was launched as a public-private partnership, led by Principal Investigator Michael W. Weiner, MD. The primary goal of ADNI has been to test whether serial magnetic resonance imaging (MRI), positron emission tomography (PET), other biological markers, and clinical and neuropsychological assessment can be combined to measure the progression of MCI and early AD. The initial phase (ADNI-1) of ADNI was launched in 2003 and subsequent phases (ADNI-GO, ADNI-2, and ADNI-3) were conducted for follow-up of existing participants and additional new enrollments. The detailed design of ADNI has been described elsewhere (35, 36). Volunteer participants between ages 55 and 90 are recruited at 63 sites across the USA and Canada. For this analysis, 829 eligible participants had data on plasma MCFAs and were enrolled in ADNI-1, ADNI-GO, ADNI-2, or ADNI-3 between September 30th 2005 and March 4th 2019. We excluded 20 duplicate records, 1 participant with a missing diagnosis, and 190 participants with AD at baseline, leaving 618 participants for analysis. Among these, 226 were cognitively normal (CN) and 392 were MCI at baseline. Consent forms were approved by each participating site’s Institutional Review Board (IRB) and all participants provided written informed consent at the time of enrollment.
Assay of Metabolomics
The metabolomics database for plasma biospecimens was obtained from the Alzheimer Disease Metabolomics Consortium (ADMC) funded by the National Institute on Aging (37). Details of sample preparation, data generation, quality control (QC), data filtering and normalization have been described elsewhere (38). In brief, the NIH-West Coast Metabolomics Center used a gas chromatography time of flight mass spectrometry (GCTOFMS) to measure the lipid metabolite profile of blood specimens from individuals from ADNI at baseline (39–41). Metabolomics lab staff were blinded to diagnostic data. After unblinding and data release, metabolite profiles went through QC checks and data preprocessing including batch-effect adjustment, missing value imputation, and log-transformation (37).
Outcome ascertainment
The ADNI diagnostic criteria for determining CN, MCI and AD were previously reported (42). In brief, ADNI investigators used conventional Petersen/Winblad criteria to categorize participants into CN, MCI or AD (42). Endpoints were measured using categorical response variables: any incident MCI among CN participants at baseline, or any incident AD among MCI participants at baseline. In the current study, we only included AD-related dementia as the outcome. Those participants with dementias from other causes were excluded from eligible participants and those who developed non-AD dementias during follow-up were treated as non-cases in the logistic regression models.
Measurement of Covariates
Covariates were determined based on a priori review of AD-related factors from previous publications. Demographic characteristics were obtained from the ADNI data repository (43). During baseline interviews, self-identified demographic characteristics including age (date of birth), sex (male/female), race (American Indian or Alaskan Native/ Asian/Native Hawaiian or Other Pacific Islander/Black or African American/ White/More than one race), ethnicity (Hispanic or Latino/Not Hispanic or Latino), and years of education (years) were collected in the case report form. A self-reported physician-diagnosed history of medical conditions including type 2 diabetes, hypertension, stroke, cardiovascular disease, and endocrine-metabolic diseases were also collected in the case report form (yes/ no). If yes, additional questions captured information about whether the condition was current and the age at diagnosis as well as details of medication use. APOE ε4 genotyping was performed at the time of participant enrollment. The two SNPs (rs429358, rs7412) that define the epsilon 2, 3, and 4 alleles were genotyped and the copy numbers of APOE ε4 alleles for each individual were calculated based on genotyping data (44).
Statistical analysis
Included in the analysis are 392 participants with MCI at baseline of whom 210 (53.6%) developed incident AD. Also included are 226 CN participants at baseline, of whom 42 (18.6%) of participants converted from CN to MCI only, 17 (7.5%) of participants further converted to incident AD during the follow-up interval, and 3 (1.3%) of participants converted directly from CN to incident AD without an observed MCI phase (Figure 1). Logistic regression models and multinomial logistic regression models were used to estimate odds ratios (ORs) and 95% CIs with incident MCI and AD as dependent variables. Log-transformed circulating levels of C8:0 served as independent variables. Associations between log-transformed circulating levels of C8:0 and risk of incident MCI among CN participants, and risk of incident AD among MCI participants were examined in 3 models, respectively. Model 1 shows crude ORs (95% CIs) without adjustment. In Model 2, we adjust for age, sex, race, ethnicity, years of education, and APOE ε4 alleles. In multivariable-adjusted model 3, we additionally adjust for type 2 diabetes, hypertension, stroke, cardiovascular disease, and metabolic diseases. Since cardiometabolic diseases and APOE ε4 alleles are two major risk factors for MCI and AD (31–33), subgroup analyses were conducted to examine the associations stratified by sex, comorbidity of cardiometabolic diseases, APOE ε4 alleles, and the 13-item Alzheimer’s Disease Assessment Scale - Cognitive Subscale (ADAS-Cog 13, range: 0–85, higher scores indicate greater dysfunction), respectively. The significance of multiplicative interactions was evaluated by adding a corresponding interaction terms in the models. We also repeated the analyses using Cox regression models. For exploratory analyses, multinomial logistic regression models were used to predict the risk of incident MCI only and incident AD among baseline CN participants. Sensitivity analysis was conducted by excluding amyloid-negative MCI patients predicted by cerebrospinal fluid (CSF) biomarkers at baseline. Elecsys p-tau/Aβ42 ratio has been shown in previous studies to have >94% overall, positive, and negative agreement with amyloid positron emission tomography (PET) classification (45); thus, we used the CSF p-tau/Aβ42 ratio to classify amyloid positive and negative MCI participants at baseline. Restricted cubic splines were used to examine possible nonlinear relationships between log-transformed circulating levels of MCFAs and risk of incident MCI and AD, respectively (46). AIC was used for knots selection and three knots for the spline curve achieved the best performance. Multivariable-adjusted analyses with 3 knots were conducted within the values between the 5th and 95th percentile to minimize the impact of potential outliers. Three knots were located at the 10th, 50th, and 90th percentiles of log-transformed circulating levels of MCFAs, respectively. All analyses were conducted using Statistical Analysis Software, version 9.4 (SAS Institute Inc., Cary, North Carolina) and restricted cubic splines were plotted using R 4.2.0 (https://cran.r-project.org/). All hypothesis testing was 2-sided with P<0.05 indicating a statistically significant finding.
Results
Baseline characteristics of ADNI participants were compared (CN vs. MCI) (Table 1). Baseline race, ethnicity, years of education, plasma levels of C8:0, and comorbidity of cardiometabolic diseases did not differ significantly between CN and MCI participants, whereas participants with MCI at baseline were likely to be younger, male, APOE ε4 carriers, amyloid-positive, and have higher ADAS-Cog 13 scores.
Associations between circulating levels of C8:0 and risk of incident MCI among CN participants are presented in Table 2. The association between log-transformed circulating levels of C8:0 and risk of incident MCI was statistically significant in the crude model (P=0.04) with an OR (95% CI) of 0.80 (0.64–0.99). The association became of borderline significance after adjusting for all covariates in model 3 (P=0.08) with an OR (95% CI) of 0.81 (0.64-1.03). The OR (95%CI) associated with a one standard deviation change in log-transformed levels of circulating C8:0 was 0.85 (0.71–1.02) in model 3. In secondary analyses, no associations were observed between circulating levels of C10:0 and C12:0 and risk of incident MCI among CN participants (Supplemental Tables S2–S3).
In subgroup analyses stratified by comorbidity of cardiometabolic diseases, the inverse association between levels of C8:0 and risk of incident MCI was statistically significant among participants with one or more cardiometabolic diseases after adjusting for all covariates with an OR (95% CI) of 0.75 (0.58–0.98) (P=0.03) (Table 2). However, the association was not present among those without comorbidity of cardiometabolic diseases. In subgroup analyses stratified by APOE ε4 alleles, the inverse association between levels of C8:0 and risk of incident MCI was statistically significant only among participants with one copy of APOE ε4 alleles after adjusting for all covariates with an OR (95% CI) of 0.43 (0.21–0.89) (P=0.02). The association attenuated when we collapsed those with two copies of APOE ε4 alleles to those with one copy, with an OR (95%CI) of 0.56 (0.31–1.02) (P=0.06). The sample size was too small to run the analyses among those with two copies of APOE ε4 alleles alone. In subgroup analyses stratified by sex, the inverse association between levels of C8:0 and risk of incident MCI was statistically significant only among female participants after adjusting for all covariates with an OR (95% CI) of 0.60 (0.38–0.94) (P=0.0248) (P for interaction=0.1458). We conducted additional analyses among participants with normal cognition at baseline stratified by cognition (ADAD-Cog13) below or above the median, separately. Although the P for interaction was not significant, C8:0 was associated with reduced risk of incident MCI among participants with normal cognition and ADAS-Cog 13 above the median at baseline with OR (95%CI) of 0.69 (0.50–0.97) in the multivariable-adjusted model (Table 2).
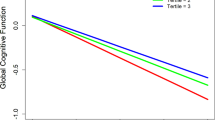
Multivariable-adjusted restricted cubic spline analyses indicated no evidence of nonlinear associations between circulating levels of C8:0 and risk of incident MCI among CN participants (P for nonlinearity=0.17); as circulating levels of C8:0 increased, there was a clear dose-response decreasing trend for risk of incident MCI, particularly at higher circulating levels of C8:0 (Figure 2A); and the dose-response trend became slightly steeper among participants with one or more cardiometabolic diseases (Figure 2B) while the trend not only became much steeper but also started to decline at lower levels of C8:0 among those with one copy of APOE ε4 alleles (Figure 2C). On the other hand, there was no dose-response trend for the association between circulating levels of C8:0 and risk incident AD among baseline MCI participants (P for nonlinearity=0.11) (Figure 2D).
Multivariable-adjusted Odds Ratios and 95% Confidence Intervals of Incident MCI or AD Associated with Circulating Levels of C8:0
Restricted cubic spline analyses used 3 knots and the 5% highest and lowest log serum C8:0 were trimmed to minimize the impact of potential outliers. All models were adjusted for age, sex, race, ethnicity, education years, APOE ε4 alleles, type 2 diabetes, hypertension, stroke, cardiovascular disease, and metabolic diseases. *Model was adjusted for age, sex, race, ethnicity, education years, and APOE ε4 alleles.
In exploratory analyses among baseline CN participants using a multinomial logistic regression model, we found that the inverse association between levels of C8:0 and risk of incident MCI only was statistically significant in the crude model (P=0.04) with an OR (95% CI) of 0.78 (0.61–0.99) and was of borderline significance after adjusting for all covariates with an OR (95% CI) of 0.78 (0.60–1.01)(P=0.06) (Supplemental Table S1). The associations between levels of C8:0 and risk of incident AD among baseline CN participants were not statistically significant in all 3 models.
Associations between circulating levels of C8:0 and risk of incident AD among baseline MCI participants and stratified analyses are presented in Table 3 and Supplemental Table S4, respectively. There were null associations between log-transformed circulating levels of C8:0 and risk of incident AD among MCI participants in main models as well as stratified analyses. After excluding amyloid-negative MCI patients classified by CSF p-tau/Aβ42 ratio, the sensitivity analysis did not show evidence of a significant association between circulating C8:0 level and AD incidence among baseline MCI patients. No associations were observed between circulating levels of C10:0 and C12:0 and risk of incident AD among MCI participants (Supplemental Tables S5–S6). We also repeated the analyses using Cox regression models and found similar results (Supplemental Tables S7-S8).
Discussion
This study examined the relationship between circulating MCFAs levels and risk of incident MCI or AD in the ADNI cohort. We found that increasing circulating level of C8:0 was significantly and prospectively associated with a reduced risk of incident MCI among cognitively normal participants in a dose-response manner, particularly among female individuals, those with one or more cardiometabolic diseases, or one APOE ε4 allele, or higher ADAS-Cog 13 scores at baseline. However, no associations were observed between circulating C8:0 and risk of incident AD among those with MCI at baseline overall and regardless of strata.
To the best of our knowledge, the present study is the first to longitudinally examine the association of C8:0 and risk of developing MCI or AD. Our findings are supported by previous short-term clinical trials conducted in patients with MCI or AD. The modified MCT ketogenic diet, which mainly consists of MCFAs, has been shown to be beneficial in patients with neurologic and metabolic disorders, including drug-resistant epilepsy (47, 48), obesity and type-2 diabetes (49, 50), and AD (51, 52). Although more flexible, the MCT ketogenic diet still necessitates carbohydrate restriction (8). However, in a 6-month randomized placebo-controlled trial, a 30 g/day ketogenic MCT drink (60% C8:0 and 40% C10:0) resulted in significantly improved cognitive function in MCI patients (25). A human study of case records from eight patients with mild-to-moderate AD who were treated with tricaprylin (20 gram/day) for ≥6 months showed delayed cognitive impairment and progression of AD compared to historical conventional pharmacotherapy (28). A randomized, double-blind, placebo controlled, multicenter trial of oral administration of AC-1202, an MCT composed almost entirely of C8:0, showed positive effects in improving cognitive function among patients with mild to moderate AD (26). Furthermore, C8:0 has also been suggested to be beneficial in ameliorating neurodegenerative disorders other than AD due to its role in promoting brain hypometabolism. For example, in vivo studies demonstrated that C8:0 triglyceride significantly promoted the mitochondrial oxygen consumption rate and alleviated amyotrophic lateral sclerosis (ALS)-type motor impairment through restoration of energy metabolism in transgenic ALS animal models (53). Although interventional studies have consistently reported the beneficial effects of C8:0 among patients with MCI, AD and other neurodegenerative disorders, no studies to date have prospectively examined the role of C8:0 in the etiology of developing MCI or AD among AD-free older adults.
Previous studies relatively consistently reported the beneficial effects of C8:0 supplementation among clinically diagnosed MCI or AD patients. In these randomized trials, large doses of interventional C8:0 supplementation were used to improve cognition. The improvement in cognition could be short-term and did not change the disease etiology course. In contrast, in the current study we used the ADNI cohort, an observational study which included free-living older adults. Dietary intakes of MCFAs in typical western diets are much lower than treatment doses used in previous randomized trials. Thus, one possible explanation for the disparities in results between the current study on AD risk and previous interventional studies may be due to the differences in doses of MCFAs.
Our findings of an inverse association between circulating levels of C8:0 and risk of incident MCI among female participants, those with cardiometabolic risk factors or one APOE ε4 allele, or higher ADAS-Cog 13 scores at baseline, are biologically plausible. The brain primarily utilizes glucose for energy production under normal conditions. AD patients have been commonly characterized with impaired glucose uptake and cerebral hypometabolism in the brain monitored by 18F-FDG PET, which is correlated with clinical cognitive decline and pathological progression of AD (54). Among CN individuals, high C8:0 levels may lead to mild-to-moderate ketosis, which provides brain cells with a more efficient energy source than glucose, resulting in improvement in cognition as well as neuroprotective effects. C8:0, the most ketogenic MCFA, can be rapidly broken down to produce ketone bodies (55). Although the mechanism by which ketones could improve cognitive function is as yet elusive, it has been shown that mild to moderate ketosis may stimulate mitochondrial biogenesis, and improve oxidative phosphorylation and ATP generation in the brain (12–16, 56). Some studies, including a recent review, argue that MCFAs may exert neuroprotective effects through mechanisms independent of ketone bodies (8). The proposed therapeutic mechanism of ketones implicated in human studies cannot be entirely replicated in animal models and several studies observed a poor correlation between plasma ketone levels and clinical phenotype, raising the question of the role of other components involved (57–59). As one of the MCFAs that can cross the brain blood-barrier and permeate the mitochondrial membrane independently of the carnitine transport system, C8:0 may directly recue brain energy hypometabolism through promoting mitochondrial biogenesis (21). On the other hand, CN individuals with low levels of C8:0 may be a biomarker of a low capacity of alternative energy supplies or exhausting alternative energy supplies during cerebral hypometabolism. Finally, unlike other MCFAs, C8:0 serves as the precursor for the biosynthesis of α-lipoic acid in mitochondrial (29), one essential antioxidant in energy metabolism (30).
Older adults with insulin resistance show the same pattern of brain glucose hypometabolism as in AD (60), with glucose hypometabolism being most significant in frontal, parietotemporal and cingulate regions, areas affected in AD (60). Furthermore, brain hypometabolism has been longitudinally linked to insulin resistance (6). There is significant evidence demonstrating that individuals with insulin resistance, type 2 diabetes and metabolic syndrome are at increased risk for AD and cognitive decline (60–65). Thus, circulating levels of C8:0 may provide a promising risk stratification biomarker among CN older adults, especially those with cardiometabolic diseases and those carrying one APOE ε4 allele. Increasing levels of C8:0 may be an effective intervention for the prevention of MCI or AD among older adults with lower levels of C8:0 and/ or cardiometabolic and genetic risk factors. The main finding of this study is the absence of an association with conversion to AD among those with MCI at baseline and presence of an association with conversion to MCI among CN participants. The etiologic significance of the finding is that it predicts the true onset of the disease versus the progression of the disease, marked by MCI. Further studies are warranted to understand these and other potential mechanisms.
This study has a number of strengths. First, ADNI is a longitudinal multicenter cohort, which was designed to incorporate clinical, imaging, genetic, and biochemical biomarkers for the early detection and tracking of AD progression. Based on this unique resource, we examined the prospective relationship between circulating levels of C8:0 and risk of incident MCI and AD over a long-term follow-up interval, up to 13.4 years. Second, AD patients at baseline were excluded prior to study entry and multiple clinic visits per person were performed to confirm and track the diagnoses during the follow-up which minimized the possibility of outcome misclassification. Third, because the risk of MCI in baseline CN participants and risk of AD in baseline MCI participants were analyzed separately, the imbalance of baseline characteristics such as age and APOE ε4 alleles may not impact the results. Nevertheless, we adjusted all available covariates in the models including age, sex, race, ethnicity, education years, APOE ε4 alleles, and cardiometabolic diseases. Finally, results from the exploratory analysis were consistent with the main analysis, suggesting that the significant inverse association was present only with risk of incident MCI, but not risk of incident AD among baseline CN participants.
There are also some limitations for the current study. First, the sample size is limited for those with data on circulating levels of MCFAs. Although we separately examined the associations between circulating levels of C8:0 and risks of incident MCI among CN participants and incident AD among MCI participants, the nonsignificant associations may be attributable to insufficient statistical power. Nevertheless, we found that the inverse associations with C8:0 were present only for the development of MCI, but not AD. This finding is consistent with the fact that other protective factors, such as physical activity (66) and intakes of omega 3 fatty acids (67, 68) are linked to benefits in the prodromal period of AD but not in the conversion from MCI to AD. Likewise, in subgroup analyses, we found that the inverse association between levels of C8:0 and risk of incident MCI was only present in CN female participants, those with one or more cardiometabolic diseases or one APOE ε4 allele. Therefore, cardiometabolic disease may be instrumental in further depleting reserve and edging the patient toward the clinical threshold of cognitive dysfunction. The non-significant association in participants with zero or two APOE ε4 alleles could be due to lack of sufficient power in these subgroups. In addition, unlike our finding, two previous studies found that C8:0 supplementation improved cognitive function in APOE ε4-negative AD patients (26, 27). One possible explanation is that the presence of an APOE ε4 allele overwhelms the protective effect from supplementation of C8:0 among AD patients. A previous study conducted in the ADNI cohort utilized logistic regression models for the risk of conversion from MCI to AD (37). Following this previous report (37), we used logistic regression models to compare converted patients to non-converted controls in the current study. The reason that we used logistic regression models, which were less powerful than Cox regression models in cohort studies, was because there were several limitations to identify the exact diagnosis or censoring dates for a number of participants. Using more conservative logistic regression models rather than Cox regression models (69), it is possible that some significant associations may become non-significant. Nevertheless, the results from Cox regression models were similar to the main results from logistic regression models. We only had baseline data, and circulating levels of C8:0 levels likely varied over time during the 13-year follow up period. This non-differential misclassification of exposure usually biases the results toward the null value, indicating that true associations are stronger than what we have observed. Future longitudinal studies with repeated measures of circulating C8:0 levels are needed to examine whether the inverse associations would be stronger. Finally, the covariates used in the current study were derived from physician-diagnosed medical history that were collected by self-reported survey questionnaires, thus, it may lead to misclassification that usually biases the association towards the null.
Conclusion
In summary, higher circulating levels of C8:0 were associated with a reduced risk of incident MCI among cognitively normal female participants, and those with one or more cardiometabolic diseases, or one APOE ε4 allele, or higher ADAS-Cog 13 scores at baseline during the 13-year follow up. No associations with incident AD were found among participants with MCI at baseline. Future studies, including randomized trials, are needed to confirm these findings. If confirmed, this finding will facilitate precision prevention of MCI or AD among CN older adults, i.e., circulating levels of C8:0 together with sex, cardiometabolic disease status, APOE ε4 alleles and ADAS-Cog 13 can be used to identify a subgroup of CN older adults at higher risk of developing MCI or AD, in whom dietary or supplemental use of C8:0 that results in elevated circulating C8:0 levels, and in turn, preventing or delaying the onset of MCI or AD.
References
Alzheimer’s Association. 2018 Alzheimer’s disease facts and figures. Alzheimer’s & Dementia, 2018, 14(3): 367–429.
2021 Alzheimer’s disease facts and figures. Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association. 2021;17(3): 327–406. https://doi.org/10.1002/alz.12328.
Brookmeyer R, Gray S, Kawas C. Projections of Alzheimer’s disease in the United States and the public health impact of delaying disease onset. American Journal of Public Health. 1998;88(9): 1337–1342. https://doi.org/10.2105/ajph.88.9.1337.
Zissimopoulos J, Crimmins E, St.Clair P. The Value of Delaying Alzheimer’s Disease Onset: Forum for Health Economics and Policy. 2015;18(1): 25–39. https://doi.org/10.1515/fhep-2014-0013.
Cisternas P, Inestrosa NC. Brain glucose metabolism: Role of Wnt signaling in the metabolic impairment in Alzheimer’s disease. Neuroscience and Biobehavioral Reviews. 2017;80: 316–328. https://doi.org/10.1016/j.neubiorev.2017.06.004.
An Y, Varma VR, Varma S, Casanova R, Dammer E, Pletnikova O, et al. Evidence for brain glucose dysregulation in Alzheimer’s disease. Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association. 2018;14(3): 318–329. https://doi.org/10.1016/j.jalz.2017.09.011.
Grammatikopoulou MG, Goulis DG, Gkiouras K, Theodoridis X, Gkouskou KK, Evangeliou A, et al. To Keto or Not to Keto? A Systematic Review of Randomized Controlled Trials Assessing the Effects of Ketogenic Therapy on Alzheimer Disease. Advances in Nutrition (Bethesda, Md.). 2020;11(6): 1583–1602. https://doi.org/10.1093/advances/nmaa073.
Augustin K, Khabbush A, Williams S, Eaton S, Orford M, Cross JH, et al. Mechanisms of action for the medium-chain triglyceride ketogenic diet in neurological and metabolic disorders. The Lancet. Neurology. 2018;17(1): 84–93. https://doi.org/10.1016/S1474-4422(17)30408-8.
Durrer C, Lewis N, Wan Z, Ainslie PN, Jenkins NT, Little JP. Short-Term Low-Carbohydrate High-Fat Diet in Healthy Young Males Renders the Endothelium Susceptible to Hyperglycemia-Induced Damage, An Exploratory Analysis. Nutrients. 2019;11(3): E489. https://doi.org/10.3390/nu11030489.
Harvey CJDC, Schofield GM, Williden M. The use of nutritional supplements to induce ketosis and reduce symptoms associated with keto-induction: a narrative review. PeerJ. 2018;6: e4488. https://doi.org/10.7717/peerj.4488.
Włodarek D. Role of Ketogenic Diets in Neurodegenerative Diseases (Alzheimer’s Disease and Parkinson’s Disease). Nutrients. 2019;11(1): E169. https://doi.org/10.3390/nu11010169.
Cunnane SC, Courchesne-Loyer A, Vandenberghe C, St-Pierre V, Fortier M, Hennebelle M, et al. Can Ketones Help Rescue Brain Fuel Supply in Later Life? Implications for Cognitive Health during Aging and the Treatment of Alzheimer’s Disease. Frontiers in molecular neuroscience. 2016;9: 53–53. https://doi.org/10.3389/fnmol.2016.00053.
Roy M, Beauvieux MC, Naulin J, Hamrani DE, Gallis JL, Cunnane SC, et al. Rapid adaptation of rat brain and liver metabolism to a ketogenic diet: an integrated study using 1H-and 13C-NMR spectroscopy. Journal of Cerebral Blood Flow & Metabolism. 2015;35(7): 1154–1162.
CahillJr GF. Fuel metabolism in starvation. Annu. Rev. Nutr. 2006;26: 1–22.
Veech RL, Chance B, Kashiwaya Y, Lardy HA, CahillJr GF. Ketone bodies, potential therapeutic uses. IUBMB life. 2001;51(4): 241–247.
Devivo DC, Leckie MP, Ferrendelli JS, McDougalJr DB. Chronic ketosis and cerebral metabolism. Annals of Neurology: Official Journal of the American Neurological Association and the Child Neurology Society. 1978;3(4): 331–337.
Phillips MC, Deprez LM, Mortimer GM, Murtagh DK, McCoy S, Mylchreest R, et al. Randomized crossover trial of a modified ketogenic diet in Alzheimer’s disease. Alzheimer’s research & therapy. 2021;13(1): 1–12.
Taylor MK, Sullivan DK, Mahnken JD, Burns JM, Swerdlow RH. Feasibility and efficacy data from a ketogenic diet intervention in Alzheimer’s disease. Alzheimer’s & Dementia: Translational Research & Clinical Interventions. 2018;4: 28–36.
Roopashree PG, Shetty SS, Kumari NS. Effect of medium chain fatty acid in human health and disease. Journal of Functional Foods. 2021;87: 104724.
Fan L, Zhu X, Sun S, Yu C, Huang X, Ness R, Dugan LL, Shu L, Seidner DL, Murff HJ, Fodor AA, Azcarate-Peril MA, Shrubsole MJ, Dai Q. Ca: Mg Ratio, Medium-chain Fatty Acids, and the Gut Microbiome. Clin Nutr, 2022, in press.
Schönfeld P, Wojtczak L. Short- and medium-chain fatty acids in energy metabolism: the cellular perspective. Journal of Lipid Research. 2016;57(6): 943–954. https://doi.org/10.1194/jlr.R067629.
Panth N, Abbott KA, Dias CB, Wynne K, Garg ML. Differential effects of medium- and long-chain saturated fatty acids on blood lipid profile: a systematic review and meta-analysis. The American Journal of Clinical Nutrition. 2018;108(4): 675–687. https://doi.org/10.1093/ajcn/nqy167.
Sacks FM. Coconut Oil and Heart Health: Fact or Fiction? Circulation. 2020;141(10): 815–817. https://doi.org/10.1161/CIRCULATIONAHA.119.044687.
Avgerinos KI, Egan JM, Mattson MP, Kapogiannis D. Medium Chain Triglycerides induce mild ketosis and may improve cognition in Alzheimer’s disease. A systematic review and meta-analysis of human studies. Ageing Research Reviews. 2020;58: 101001. https://doi.org/10.1016/j.arr.2019.101001.
Fortier M, Castellano CA, Croteau E, Langlois F, Bocti C, St-Pierre V, et al. A ketogenic drink improves brain energy and some measures of cognition in mild cognitive impairment. Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association. 2019;15(5): 625–634. https://doi.org/10.1016/j.jalz.2018.12.017.
Henderson ST, Vogel JL, Barr LJ, Garvin F, Jones JJ, Costantini LC. Study of the ketogenic agent AC-1202 in mild to moderate Alzheimer’s disease: a randomized, double-blind, placebo-controlled, multicenter trial. Nutrition & Metabolism. 2009;6: 31. https://doi.org/10.1186/1743-7075-6-31.
Xu Q, Zhang Y, Zhang X, Liu L, Zhou B, Mo R, et al. Medium-chain triglycerides improved cognition and lipid metabolomics in mild to moderate Alzheimer’s disease patients with APOE4-/-: A double-blind, randomized, placebo-controlled crossover trial. Clinical Nutrition (Edinburgh, Scotland). 2020;39(7): 2092–2105. https://doi.org/10.1016/j.clnu.2019.10.017.
Maynard SD, Gelblum J. Retrospective case studies of the efficacy of caprylic triglyceride in mild-to-moderate Alzheimer’s disease. Neuropsychiatric Disease and Treatment. 2013;9: 1629–1635. https://doi.org/10.2147/NDT.S49895.
Mayr JA, Feichtinger RG, Tort F, Ribes A, Sperl W. Lipoic acid biosynthesis defects. Journal of Inherited Metabolic Disease. 2014;37(4): 553–563. https://doi.org/10.1007/s10545-014-9705-8.
Kaur D, Behl T, Sehgal A, Singh S, Sharma N, Chigurupati S, et al. Decrypting the potential role of α-lipoic acid in Alzheimer’s disease. Life Sciences. 2021;284: 119899. https://doi.org/10.1016/j.lfs.2021.119899.
Sims-Robinson C, Kim B, Rosko A, Feldman EL. How does diabetes accelerate Alzheimer disease pathology? Nature Reviews. Neurology. 2010;6(10): 551–559. https://doi.org/10.1038/nrneurol.2010.130.
Craft S. The Role of Metabolic Disorders in Alzheimer Disease and Vascular Dementia: Two Roads Converged. Archives of Neurology. 2009;66(3): 300–305. https://doi.org/10.1001/archneurol.2009.27.
Razay G, Vreugdenhil A, Wilcock G. The Metabolic Syndrome and Alzheimer Disease. Archives of Neurology. 2007;64(1): 93–96. https://doi.org/10.1001/archneur.64.1.93.
Eckel RH, Hanson AS, Chen AY, Berman JN, Yost TJ, Brass EP. Dietary substitution of medium-chain triglycerides improves insulin-mediated glucose metabolism in NIDDM subjects. Diabetes. 1992;41(5): 641–647.
Weiner MW, Veitch DP, Aisen PS, Beckett LA, Cairns NJ, Green RC, et al. Recent publications from the Alzheimer’s Disease Neuroimaging Initiative: Reviewing progress toward improved AD clinical trials. Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association. 2017;13(4): e1–e85. https://doi.org/10.1016/j.jalz.2016.11.007.
Saykin AJ, Shen L, Yao X, Kim S, Nho K, Risacher SL, et al. Genetic studies of quantitative MCI and AD phenotypes in ADNI: Progress, opportunities, and plans. Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association. 2015;11(7): 792–814. https://doi.org/10.1016/j.jalz.2015.05.009.
MahmoudianDehkordi S, Arnold M, Nho K, Ahmad S, Jia W, Xie G, et al. Altered bile acid profile associates with cognitive impairment in Alzheimer’s disease—an emerging role for gut microbiome. Alzheimer’s & Dementia. 2019;15(1): 76–92.
Barupal DK, Fan S, Wancewicz B, Cajka T, Sa M, Showalter MR, et al. Generation and quality control of lipidomics data for the alzheimer’s disease neuroimaging initiative cohort. Scientific Data. 2018;5: 180263. https://doi.org/10.1038/sdata.2018.263.
Tsugawa H, Cajka T, Kind T, Ma Y, Higgins B, Ikeda K, et al. MS-DIAL: data-independent MS/MS deconvolution for comprehensive metabolome analysis. Nature Methods. 2015;12(6): 523–526. https://doi.org/10.1038/nmeth.3393.
McCoin CS, Piccolo BD, Knotts TA, Matern D, Vockley J, Gillingham MB, et al. Unique plasma metabolomic signatures of individuals with inherited disorders of long-chain fatty acid oxidation. Journal of Inherited Metabolic Disease. 2016;39(3): 399–408. https://doi.org/10.1007/s10545-016-9915-3.
Cajka T, Davis R, Austin KJ, Newman JW, German JB, Fiehn O, et al. Using a lipidomics approach for nutritional phenotyping in response to a test meal containing gamma-linolenic acid. Metabolomics. 2016;12(8): 1–16.
Bondi MW, Edmonds EC, Jak AJ, Clark LR, Delano-Wood L, McDonald CR, et al. Neuropsychological criteria for mild cognitive impairment improves diagnostic precision, biomarker associations, and progression rates. Journal of Alzheimer’s disease: JAD. 2014;42(1): 275–289. https://doi.org/10.3233/JAD-140276.
Nho K, Kueider-Paisley A, Arnold M, MahmoudianDehkordi S, Risacher SL, Louie G, et al. Serum metabolites associated with brain amyloid beta deposition, cognition and dementia progression. Brain communications. 2021;3(3): fcab139.
Saykin AJ, Shen L, Foroud TM, Potkin SG, Swaminathan S, Kim S, et al. Alzheimer’s Disease Neuroimaging Initiative biomarkers as quantitative phenotypes: Genetics core aims, progress, and plans. Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association. 2010;6(3): 265–273. https://doi.org/10.1016/j.jalz.2010.03.013.
Campbell MR, Ashrafzadeh-Kian S, Petersen RC, Mielke MM, Syrjanen JA, van Harten AC, et al. P-tau/Aβ42 and Aβ42/40 ratios in CSF are equally predictive of amyloid PET status. Alzheimer’s & Dementia (Amsterdam, Netherlands). 2021;13(1): e12190. https://doi.org/10.1002/dad2.12190.
Durrleman S, Simon R. Flexible regression models with cubic splines. Statistics in Medicine. 1989;8(5): 551–561. https://doi.org/10.1002/sim.4780080504.
Ye F, Li XJ, Jiang WL, Sun HB, Liu J. Efficacy of and patient compliance with a ketogenic diet in adults with intractable epilepsy: a meta-analysis. Journal of Clinical Neurology (Seoul, Korea). 2015;11(1): 26–31. https://doi.org/10.3988/jcn.2015.11.1.26.
Martin K, Jackson CF, Levy RG, Cooper PN. Ketogenic diet and other dietary treatments for epilepsy. The Cochrane Database of Systematic Reviews. 2016;2: CD001903. https://doi.org/10.1002/14651858.CD001903.pub3.
Geng S, Zhu W, Xie C, Li X, Wu J, Liang Z, et al. Medium-chain triglyceride ameliorates insulin resistance and inflammation in high fat diet-induced obese mice. European Journal of Nutrition. 2016;55(3): 931–940. https://doi.org/10.1007/s00394-015-0907-0.
Mumme K, Stonehouse W. Effects of medium-chain triglycerides on weight loss and body composition: a meta-analysis of randomized controlled trials. Journal of the Academy of Nutrition and Dietetics. 2015;115(2): 249–263. https://doi.org/10.1016/j.jand.2014.10.022.
Chatterjee P, Fernando M, Fernando B, Dias CB, Shah T, Silva R, et al. Potential of coconut oil and medium chain triglycerides in the prevention and treatment of Alzheimer’s disease. Mechanisms of Ageing and Development. 2020;186: 111209. https://doi.org/10.1016/j.mad.2020.111209.
Taylor MK, Swerdlow RH, Sullivan DK. Dietary Neuroketotherapeutics for Alzheimer’s Disease: An Evidence Update and the Potential Role for Diet Quality. Nutrients. 2019;11(8). https://doi.org/10.3390/nu11081910.
Zhao W, Varghese M, Vempati P, Dzhun A, Cheng A, Wang J, et al. Caprylic triglyceride as a novel therapeutic approach to effectively improve the performance and attenuate the symptoms due to the motor neuron loss in ALS disease. PloS One. 2012;7(11): e49191. https://doi.org/10.1371/journal.pone.0049191.
Small GW, Ercoli LM, Silverman DH, Huang SC, Komo S, Bookheimer SY, et al. Cerebral metabolic and cognitive decline in persons at genetic risk for Alzheimer’s disease. Proceedings of the National Academy of Sciences of the United States of America. 2000;97(11): 6037–6042. https://doi.org/10.1073/pnas.090106797.
Cunnane SC, Courchesne-Loyer A, St-Pierre V, Vandenberghe C, Pierotti T, Fortier M, et al. Can ketones compensate for deteriorating brain glucose uptake during aging? Implications for the risk and treatment of Alzheimer’s disease. Annals of the New York Academy of Sciences. 2016;1367(1): 12–20. https://doi.org/10.1111/nyas.12999.
Bough KJ, Wetherington J, Hassel B, Pare JF, Gawryluk JW, Greene JG, et al. Mitochondrial biogenesis in the anticonvulsant mechanism of the ketogenic diet. Annals of Neurology: Official Journal of the American Neurological Association and the Child Neurology Society. 2006;60(2): 223–235.
Chang P, Augustin K, Boddum K, Williams S, Sun M, Terschak JA, et al. Seizure control by decanoic acid through direct AMPA receptor inhibition. Brain: A Journal of Neurology. 2016;139(Pt 2): 431–443. https://doi.org/10.1093/brain/awv325.
Thavendiranathan P, Mendonca A, Dell C, Likhodii SS, Musa K, Iracleous C, et al. The MCT ketogenic diet: effects on animal seizure models. Experimental Neurology. 2000;161(2): 696–703. https://doi.org/10.1006/exnr.1999.7298.
Likhodii SS, Musa K, Mendonca A, Dell C, Burnham WM, Cunnane SC. Dietary fat, ketosis, and seizure resistance in rats on the ketogenic diet. Epilepsia. 2000;41(11): 1400–1410. https://doi.org/10.1111/j.1528-1157.2000.tb00115.x.
Neth BJ, Craft S. Insulin Resistance and Alzheimer’s Disease: Bioenergetic Linkages. Frontiers in Aging Neuroscience. 2017;9: 345. https://doi.org/10.3389/fnagi.2017.00345.
Finch CE, Cohen DM. Aging, metabolism, and Alzheimer disease: review and hypotheses. Experimental Neurology. 1997;143(1): 82–102. https://doi.org/10.1006/exnr.1996.6339.
Assuncao N, Sudo FK, Drummond C, de Felice FG, Mattos P. Metabolic Syndrome and cognitive decline in the elderly: A systematic review. PloS One. 2018;13(3): e0194990. https://doi.org/10.1371/journal.pone.0194990.
Rawlings AM, Sharrett AR, Mosley TH, Ballew SH, Deal JA, Selvin E. Glucose Peaks and the Risk of Dementia and 20-Year Cognitive Decline. Diabetes Care. 2017;40(7): 879–886. https://doi.org/10.2337/dc16-2203.
Stanley M, Macauley SL, Holtzman DM. Changes in insulin and insulin signaling in Alzheimer’s disease: cause or consequence? The Journal of Experimental Medicine. 2016;213(8): 1375–1385. https://doi.org/10.1084/jem.20160493.
Kang S, Lee YH, Lee JE. Metabolism-Centric Overview of the Pathogenesis of Alzheimer’s Disease. Yonsei Medical Journal. 2017;58(3): 479–488. https://doi.org/10.3349/ymj.2017.58.3.479.
Brini S, Sohrabi HR, Peiffer JJ, Karrasch M, Hämäläinen H, Martins RN, et al. Physical Activity in Preventing Alzheimer’s Disease and Cognitive Decline: A Narrative Review. Sports Medicine. 2018;48(1): 29–44. https://doi.org/10.1007/s40279-017-0787-y.
Thomas J, Thomas CJ, Radcliffe J, Itsiopoulos C. Omega-3 Fatty Acids in Early Prevention of Inflammatory Neurodegenerative Disease: A Focus on Alzheimer’s Disease. Calviello G (ed.) BioMed Research International. 2015;2015: 172801. https://doi.org/10.1155/2015/172801.
Jicha GA, Markesbery WR. Omega-3 fatty acids: potential role in the management of early Alzheimer’s disease. Clinical interventions in aging. 2010;5: 45–61. https://doi.org/10.2147/cia.s5231.
Staley JR, Jones E, Kaptoge S, Butterworth AS, Sweeting MJ, Wood AM, et al. A comparison of Cox and logistic regression for use in genome-wide association studies of cohort and case-cohort design. European journal of human genetics: EJHG. 2017;25(7): 854–862. https://doi.org/10.1038/ejhg.2017.78.
Acknowledgment
Data collection and sharing for this project was funded by the Alzheimer’s Disease Neuroimaging Initiative (ADNI) (National Institutes of Health Grant U01 AG024904) and DOD ADNI (Department of Defense award number W81XWH-12-2-0012).
Funding
QD and MJS are supported by R01 DK110166 from National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). LLD was supported by grant AG058856 from the VA Tennessee Valley Geriatric Research, Education, and Clinical Center (GRECC). LF was supported by the Vanderbilt Ingram Cancer Center Endowment Fund.
Author information
Authors and Affiliations
Contributions
LF and QD contributed to the hypothesis development. LF and QD contributed to study design. LF and QD conducted the research. LF performed statistical analysis. All authors drafted the manuscript. All authors contributed to the data interpretation and manuscript revision and approved the final version of this manuscript.
Corresponding author
Ethics declarations
We used the existing data collected from the ADNI. In ADNI, “Written informed consent for the study must be obtained from all subjects and/or authorized representatives and study partners before protocol-specific procedures are carried out.
Additional information
Conflict of Interest and Disclosure Statement
All authors have no conflicts of interest.
For the Alzheimer’s Disease Neuroimaging Initiative
Data used in preparation of this article were obtained from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database (adni.loni.usc.edu). As such, the investigators within the ADNI contributed to the design and implementation of ADNI and/or provided data but did not participate in analysis or writing of this report. A complete listing of ADNI investigators can be found at: http://adni.loni.usc.edu/wp-content/uploads/how_to_apply/ADNI_Acknowledgement_List.pdf
Rights and permissions
About this article
Cite this article
Fan, L., Zhu, X., Borenstein, A.R. et al. Association of Circulating Caprylic Acid with Risk of Mild Cognitive Impairment and Alzheimer’s Disease in the Alzheimer’s Disease Neuroimaging Initiative (ADNI) Cohort. J Prev Alzheimers Dis 10, 513–522 (2023). https://doi.org/10.14283/jpad.2023.37
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.14283/jpad.2023.37