Abstract
Background
Although frailty status greatly impacts health care in countries with rapidly aging populations, little is known about the frailty status in Chinese older adults.
Objectives
Given the increased health care needs associated with frailty, we sought to develop an easily applied self-report screening tool based on four of the syndromic frailty components and sought to validate it in a population of older adults in China.
Design
Prospective epidemiological cohort study.
Setting
Community-dwelling residents living in Beijing, China.
Participants
1724 community-dwelling adults aged ≥60 years in 2004 with an 8-year follow up.
Measurements
We developed a simple self-report frailty screening tool—the Frailty Screening Questionnaire (FSQ)—based on the modified Fried frailty components. The predictive ability for outcome was assessed by age and sex adjusted Cox proportional hazards model.
Results
According to FSQ criteria, 7.1% of the participants were frail. Frailty was associated with poor physical function, fractures, falls, and mortality. Both frailty and pre-frailty were associated with a higher mortality rate: frailty—hazards ratio (HR), 3.94, 95% confidence interval (CI), 3.16–4.92, P<0.001; pre-frailty—HR, 1.89; 95% CI, 1.57–2.27, P <0.001; adjusted models for this variable did not affect the estimates of the association. Among the four frailty components, slowness was the strongest predictor of mortality. The combination of the four components provided the best risk prediction.
Conclusions
FSQ is a self-report frailty measurement tool that can be rapidly performed to identify older adults with higher risk of adverse health outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One of the most commonly recognized risk states for adverse outcomes in older adults is frailty. Quality frailty measurement should be able to identify frailty and those frail older adults that might respond to treatment, predict adverse outcomes, and ideally be able to identify those with a common biological underpinning (1). Frailty is most often defined as a geriatric syndrome, resulting from a cumulative decrease in multiple physiological systems and consequent reduction in physical reserve and defense ability (2, 3). It is often accompanied by increased vulnerability to adverse outcomes including falls, disability, and mortality (2). The most common definition of frailty was proposed by Fried, who considered the clinical phenotype of frailty as a well-defined syndrome with biological underpinnings (3). The Fried frailty detection identifies frailty by evaluating symptoms and signs associated with biological aging, including shrinking, exhaustion, weakness, slowness, and low levels of activity (3). Other main frailty concepts are often measured by cumulative comorbidities or “deficits” (4). The deficit model assesses accumulated declines in multiple domains with regard to diseases, and physical, psychological, and social functions, and comprehensively captures comorbidity and disability.
Although the original Fried’s physical frailty phenotype scale remains the most validated and utilized method, selfreport information on Fried components also showed good predictive ability (5, 6). Hence, a self-report frailty detection tool may provide an alternative method for rapidly screening large populations of frail adults. Although dozens of other measurement tools for frailty have been reported, frailty detection methods are recommended to be matched to a particular need or environment to be most effective (7).
When attempting to identify frailty detection methods applicable to Chinese older adults, it is evident that available screening tools present two major limitations. First, most are time-consuming and are difficult to apply in busy medical practices with large populations. Second, no tool to date has been developed specific for Chinese elders. Given the large number of older outpatients in Chinese health care settings, the use of a standardized subjective evaluation of frailty would likely be readily accepted and adopted by busy clinicians. To address the current lack of an easy-to-use, valid, reliable screening measure of physical frailty consistent with original conceptual and biological model, we developed and validated a simple frailty pre-screening tool for outpatient settings—the Phenotypic Frailty Screening Questionnaire (FSQ).
Methods
Participants
Data were from the Beijing Longitudinal Study of Aging, a longitudinal study funded by the United Nations Population Fund (UNPFA CPR/90/P23) in 1992 (8). A cross-sectional survey comprising 1865 adults aged ≥60 years was conducted based on sample data from the fourth census of Beijing in 2004. Well-established statistical sampling techniques, which included clustering, stratification, and random selection were applied. Details of the sampling scheme were described elsewhere (9, 10). 1724 participants completed the frailty assessment. Data were collected on the following aspects: socioeconomic and demographic characteristics, physical health (self-report history of chronic disease and clinical syndromes), physical function, life behavior and social function, neuropsychological health, and medical condition. The definitions of cognitive impairment and depression appear in our previous publication (11). The mortality data for all subjects were collected every year until the end of December 2012. Mortality ascertainment was 100% complete. Instances of death were confirmed by family members or neighborhood or village committees. This study was approved by the ethics review board of Xuanwu Hospital, Capital Medical University and all the participants provided informed consent.
FSQ assessment
The FSQ scale was developed to represent four of five components of the Fried criteria: slowness, weakness, inactivity, and exhaustion (Table S1). Slowness received a score of 1 if participants had difficulty walking 250 meters. Weakness received a score of 1 if participants had difficulty in lifting or carrying something weighing 5 kilograms. Exhaustion received a score of 1 for participants who responded yes to either “Everything I did was an effort” or “I could not get going” in the past week. Inactivity was measured by asking participants how many hours they had spent on weekly exercise; subjects who responded <3 hours/week scored 1 point. The FSQ total score is 0–4. A score of 0 was considered robust; 1–2 was considered pre-frail; and a score of ≥3 indicated frailty.
Physical function
We assessed physical function by means of the balance test, chair-stand test, activities of daily living (ADL), and instrumental activities of daily living (IADL) as well as in terms of fractures and falls.
Statistical methods
Statistical analyses were performed by SPSS 11.5 (SPSS, Inc., Chicago, IL, USA). Chi-square tests were conducted for discrete variables, and analysis of variance and Student t tests were used to compare means of the groups for continuous variables with Tukey post hoc tests. We evaluated survival using Kaplan-Meier curves stratified for different sex and agegroups. A Cox proportional hazards model was used to evaluate the effect of covariates (age, sex, and frailty) on mortality after testing for the proportionality assumption. We considered P <0.05 statistically significant.
Results
Using the FSQ in the Beijing Longitudinal Study of Aging population, 194 participants were identified as frail and the prevalence was 11.3% (weighted, 7.1%). The prevalence of pre-frailty was 32.5% (weighted, 29.5%). Frailty was associated with female gender, rural residency, older age, and lower socioeconomic status. Higher prevalence of frailty was observed among participants who were not married, those with a history of heavy physical labor occupation, and those with poor health or life satisfaction (Table 1). For both men and women, the prevalence of frailty increased with age and was higher among rural residents (Table S2). Frailty was more common in subjects with chronic diseases (Table S3).
The prevalence of frailty components according to the FSQ included slowness, 15.3%; weakness, 19.0%; inactivity, 23.0%; and exhaustion, 21.9%. The prevalence of 0, one, two, three, and four components was 56.3%, 22.9%, 9.6%, 7.9%, and 3.4%, respectively. The prevalence of the four components was higher among women than among men (Table S4).
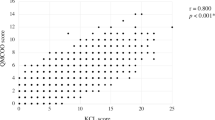
Compared with robust subjects, frail and pre-frail status was associated with poor balance and chair-stand performance, ADL dependency, IADL dependency, fracture and falls, even after adjustment for sex (but not fractures in male) (Table 2). Among both men and women, being frail or pre-frail was associated with 8-year mortality. The four components showed a higher mortality rate in the overall, female, and male samples (Table S5). Frailty and each of the four components were associated with mortality in every age-group (except inactivity in 60–69 years group and exhaustion in ≥ 80 years group) (Table S6). Figures S1, S2 and S3 present Kaplan-Meier curves for the proportional survival of participants with different frail statuses in the different age- and sex groups. The unadjusted associations were significant for the predictive association of frailty and pre-frailty with mortality; after adjusting for age and sex, the 8-year mortality hazard ratio was 2.131– 3.444 and 1.318–1.972, respectively, for frailty and prefrailty. Each component could predict mortality—even after adjusting for age and sex. Slowness was the strongest predictor and exhaustion the weakest predictor. Combined, the four components offered best risk prediction for mortality than the single component (Table 3; Figure S4).
Discussion
The FSQ is an easy to use self-report tool developed in a Chinese population. It was loosely derived from the phenotypic frailty detection method. This was developed in part because of the need for quick pre-screening tool for frailty in busy Chinese outpatient practices where up to 10 patients an hour may be seen. This study found the weighted prevalence of frailty based on the FSQ to be 7.1%. This is similar to the prevalence of frailty as measured using the Fried phenotype criteria in China (7.0%) (12). Most data on the prevalence of frailty in the Chinese population have been based on frailty index conceptual model. We previously reported the prevalence of frailty based on frailty index to be 8.8% in the China Comprehensive Geriatric Assessment Study and 9.1% in the Beijing Longitudinal Study of Aging II (13, 14). In this study, the prevalence of frailty based on the FSQ was found to be higher in women and increased with advancing age, consistence with previous studies (3, 13, 15–17). One metaanalysis confirmed the pattern of sex differences in frailty and mortality to be a “male-female health-survival paradox” (18).
We found that slowness was the highest predictor among the four components. This result constitutes a response to the question as to which component of the phenotype model is more informative with regard to frailty assessment. Another investigation found gait speed to be the best indicator of frailty and that the combination of gait speed and physical activity was the most informative among the Fried components (19). Several studies have determined gait speed to be the preeminent frailty screening tool (20–22). Gait speed is a simple, acceptable measurement that can be easily performed in a routine clinic. The present investigation provides evidence that among the four components, self-report slowness is also the most important indicator for mortality in older subjects.
We compared the new tool with other instruments reported in the literature in terms of the following five aspects: population; frailty components; ease of application; primary use; and validity (Table S7). Among the eleven self-report instruments in the comparison, the FSQ was one of only two tools which were based on physical frailty and showed validity in outcome prediction in a large population.
The present study’s strengths include the large sample and completeness of the long-term follow-up. The Beijing Longitudinal Study of Aging is based on a large populationbased cohort using clustering, stratification, and randomselection sampling techniques; thus, it can be taken to be representative of older Chinese people (8). Moreover, in the 8-year follow-up, mortality ascertainment was 100% complete. The present study also addressed the question as to which component of the phenotype model was more important. As shown in Table S7, the FSQ is quick to use by non-specific staff, and it is available from routinely comprehensive geriatric assessment data. Last and the most important, this study shows that the FSQ is feasible for a Chinese population. To the best of our knowledge, the FSQ tool is the only assessment tool based on the frailty phenotype designed for screening frailty in a Chinese population.
Our study also has several limitations. One of the main limitations is the lack of objective measurements. Hence, we were unable to evaluate the five-item Fried Phenotype in comparative analyses. Future studies on validation of FSQ with measured Fried phenotype should be conducted. Second, we did not take into account potential changes in frailty status between visits. A scoring system is needed to capture the dynamic nature of frailty so that it can be used as an outcome and intervention measurement (23). Third, we demonstrated that the four self-report Fried frailty components do not play the same role in predicting mortality, and the total level of frailty is not equivalent to the sum of those components. Future studies should weigh those components, characterize the trajectories of frailty, and examine cross-cultural validation.
Conclusions
FSQ is a useful quick and feasible self-report frailty tool that has been demonstrated to predict mortality in Chinese old adults. To our knowledge, this study is the first to report the prevalence of frailty and long-term prognosis using a self-report version of the Fried phenotype in a large longitudinal Chinese population. The FSQ was gathered using information provide by participants; it is associated with physical function, chronic disease, fracture, falls, and mortality, and it shows a good agreement with prior studies in China using Fried phenotype. The results of this study may ease frailty screening in older Chinese population by offering a very simple way to identify frailty and related risk of mortality in older adults. This in turn may facilitate targeted comprehensive geriatric assessment for the frail subset of patients as has previously been recommended in the United Kingdom (24). In addition, it may facilitate the development of novel interventions to better manage frailty and slow declines in health status.
Supplementary materials: Available at the https://springerlink.bibliotecabuap.elogim.com/journal/42415.
Funding: This work was supported by United Nations Population Fund (CPR/90/P23) and Milstein Medical Asian American Partnership Foundation Project Award in Geriatrics.
Acknowledgement: We acknowledge all the people who participated in the cohort study.
Prsented as poster in Society for Epidemiologic Research 51 Annual Meeting (SER2018), Baltimore, Maryland, USA, June 19–22, 2018.
Conflict of Interest: None.
References
Dent E, Kowal P, Hoogendijk EEO. Frailty measurement in research and clinical practice: A review. Eur J Intern Med 2016;31:3–10.
Morley JE, Vellas B, Abellan van Kan G, et al. Frailty consensus: A call to action. J Am Med Dir Assoc 2013;14:392–7.
Fried LP, Tangen CM, Walston J, et al. Frailty in Older Adults: Evidence for a Phenotype. Journals Gerontol Ser A Biol Sci Med Sci 2001;56:M146–57.
Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci 2007;62:722–7.
Zaslavsky O, Zelber-Sagi S, Gray SL, et al. Comparison of Frailty Phenotypes for Prediction of Mortality, Incident Falls, and Hip Fracture in Older Women. J Am Geriatr Soc 2016;64:1858–62.
Paulson D, Lichtenberg PA. The Paulson–Lichtenberg Frailty Index: evidence for a self-report measure of frailty. Aging Ment Health 2017;19:892–901.
Buta BJ, Walston JD, Godino JG, et al. Frailty assessment instruments: Systematic characterization of the uses and contexts of highly-cited instruments. Ageing Res Rev 2016;26:53–61.
Zimmer Z, Kaneda T, Tang Z, Fang X. Explaining Late Life Urban vs. Rural Health Discrepancies in Beijing. Soc Forces 2010;88:1885–908.
Ma L, Zhang L, Tang Z, et al. Use of the frailty index in evaluating the prognosis of older people in Beijing: A cohort study with an 8-year follow-up. Arch Gerontol Geriatr 2016;64:172–7.
Ma L, Zhao X, Tang Z, et al. Epidemiological characteristics of hypertension in the elderly in Beijing, China. PLoS One 2015;10:1–8.
Ma L, Tang Z, Sun F, et al. Risk factors for depression among elderly subjects with hypertension living at home in China. Int J Clin Exp Med 2015;8:2923–8.
Wu C, Smit E, Xue Q-L, Odden MC. Prevalence and Correlates of Frailty among Community-Dwelling Chinese Older Adults: The China Health and Retirement Longitudinal Study. J Gerontol A Biol Sci Med Sci 2017;73:102–108.
Ma L, Tang Z, Zhang L, Sun F, Chan P. Prevalence of frailty and associated factors in the community-dwelling population of China. J Am Geriatr Soc 2018;66:559–564.
Zheng Z, Guan S, Ding H, et al. Prevalence and Incidence of Frailty in Community-Dwelling Older People: Beijing Longitudinal Study of Aging II. J Am Geriatr Soc 2016;64:1281–6. doi:10.1111/jgs.14135.
Shi J, Yang Z, Song X, et al. Sex differences in the limit to deficit accumulation in late middle-aged and older Chinese People: Results from the Beijing longitudinal study of aging. J Gerontol A Biol Sci Med Sci 2014;69:702–9. doi:10.1093/gerona/glt143.
Rockwood K, Howlett SE, MacKnight C, et al. Prevalence, attributes, and outcomes of fitness and frailty in community-dwelling older adults: report from the Canadian study of health and aging. J Gerontol A Biol Sci Med Sci 2004;59:1310–7. doi:10.1093/gerona/59.12.1310.
Bandeen-Roche K, Seplaki CL, Huang J, et al. Frailty in Older Adults: A Nationally Representative Profile in the United States. Journals Gerontol Ser A Biol Sci Med Sci 2015;70:1427–34.
Gordon EH, Peel NM, Samanta M, Theou O, Howlett SE, Hubbard RE. Sex differences in frailty: A systematic review and meta-analysis. Exp Gerontol 2017;89:30–40.
Hoogendijk EO, Abellan van Kan G, Guyonnet S, Vellas B, Cesari M. Components of the Frailty Phenotype in Relation to the Frailty Index: Results From the Toulouse Frailty Platform. J Am Med Dir Assoc 2015;16:855–9.
Woo J. Walking Speed: A Summary Indicator of Frailty? J Am Med Dir Assoc 2015;16:635–7.
Studenski S, Perera S, Patel K. Gait speed and survival in older adults. JAMA 2011;305:50–8.
Woo J, Leung J, Zhang T. Successful Aging and Frailty: Opposite Sides of the Same Coin? J Am Med Dir Assoc 2016;17:797–801.
Mitnitski AB, Mogilner AJ, Rockwood K. Accumulation of Deficits as a Proxy Measure of Aging. Sci World J 2001;1:323–36.
Turner G, Clegg A. Best practice guidelines for the management of frailty: a British Geriatrics Society, Age UK and Royal College of General Practitioners report. Age Ageing 2014;43:744–7.
Author information
Authors and Affiliations
Corresponding authors
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Ma, L., Tang, Z., Chan, P. et al. Novel Frailty Screening Questionnaire (FSQ) Predicts 8-Year Mortality in Older Adults in China. J Frailty Aging 8, 33–38 (2019). https://doi.org/10.14283/jfa.2018.38
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.14283/jfa.2018.38