Abstract
Background
Neoadjuvant immunotherapy using immune checkpoint inhibitors (ICIs) has revolutionized the treatment of early stage non-small cell lung cancer (NSCLC). However, little is known about which patients are likely to benefit most from neoadjuvant immunotherapy. In this study, we performed a multiplatform analysis on samples from resectable NSCLC treated with neoadjuvant immunotherapy to explore molecular characteristics related to immune responses.
Patients and Methods
A total of 17 patients with resectable stage IB–IIIA NSCLC treated with neoadjuvant immunotherapy were included. A multiplex cytokine assay, bulk TCR sequencing in peripheral blood, and multiplexed immunohistochemistry were performed.
Results
Low levels of stromal cell-derived factor (SDF)-1alpha at baseline were associated with unfavorable disease-free survival (DFS). Patients with major pathologic response (MPR) showed a decrease in HGF after one cycle of neoadjuvant immunotherapy. An increase in IDO and IP-10 was observed in patients who developed immune-related adverse events (irAEs) after neoadjuvant immunotherapy. There were no correlations between irAEs and MPR or DFS. The MPR group presented a significant decrease in white blood cells and neutrophil count after neoadjuvant immunotherapy. The high peripheral baseline TCR convergence was correlated with MPR and favorable DFS in lung squamous cell carcinoma (LUSC) receiving neoadjuvant immunotherapy. Neoadjuvant immunotherapy led to a significant increase in CD4+, CD8+, and CD8+CD39+ T-cell infiltration in tumor areas.
Conclusions
This study suggests the potential roles of cytokines and TCR convergence for predicting ICIs response in resectable NSCLC and LUSC. CD8+CD39+T cells and CD4+ T cells could be involved in the action of neoadjuvant immunotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Immune checkpoint inhibitors (ICIs) directed against programmed death-1 (PD-1) and cytotoxic T lymphocyte antigen-4 (CTLA-4) proteins have greatly expanded therapeutic options in oncology.1 Single-agent PD-1/PD-L1 blockade or combination therapy becomes a standard first-line regimen for advanced non-small cell lung cancer (NSCLC) without driver gene mutations.2,3 In recent years, emerging data from various ongoing trials suggest that neoadjuvant immunotherapy combining chemotherapy has significant efficacy and improve the survival of patients with resectable NSCLC. For the NADIM II study, the pathological complete response (pCR) rate with nivolumab plus chemotherapy versus chemotherapy was 36.8% versus 6.9%, and the major pathologic response (MPR) rate was 52.6% versus 13.8%.4 CheckMate 816 showed 24% versus 2.2% of pCR and 31.6 months versus 20.8 months of median event-free survival (EFS) for patients treated with nivolumab plus chemotherapy and those with chemotherapy alone.5 The patients who benefit most from neoadjuvant immunotherapy could be those with pCR or MPR. However, the molecular features of pCR or MPR still need to be discovered.
Programmed death-ligand 1 (PD-L1) protein expression detected by immunohistochemistry (IHC) has been the predictive biomarker for response to ICIs pursued in most immuno-oncology clinical trials, but PD-L1 expression remains an imperfect biomarker, as it is a continuous variable, inducible in certain conditions and with a certain degree of temporal and spatial heterogeneity.6 It is still unclear whether the response to immunotherapy is related to PD-L1 expression, especially in neoadjuvant immunotherapy combining chemotherapy settings. Some patients with PD-L1 negative expression still achieved MPR in response to neoadjuvant immunotherapy combining chemotherapy.5,7
Chronic stimulation of T cells with tumor neoantigen may elicit convergent T-cell responses. The frequency of convergent T-cell receptors (TCRs) within a repertoire may indicate the immunogenicity of a tumor, thus its possible sensitivity to checkpoint blockade therapy.8 Cytokines are small soluble proteins secreted by immune cells or tumor cells, regulating the proliferation, differentiation, and activity of immune cells. It has been reported that the level of baseline and changes of cytokines correlated with ICIs response in various patients with tumors.9 However, changes in cytokines are not evident in neoadjuvant immunotherapy settings in NSCLC.
Resected tumor tissues after neoadjuvant immunotherapy provide materials for investigating the potential mechanisms of response and resistance. Blood TCR and cytokines status could reflect peripheral immune responses. To know biomarkers of response to neoadjuvant immunotherapy and biology of PD-1/PD-L1 action, multiplatform analysis including multiplexed immunohistochemistry (mIHC), multiplex cytokine assay, and TCRβ repertoire sequencing was performed on 17 patients with resectable stage IB–IIIA NSCLC who were treated with neoadjuvant immunotherapy.
Patients and Methods
Study Design and Patient Samples
In this study, we analyzed 17 patients with resectable stage IB–IIIA NSCLC who received two or three cycles of neoadjuvant immunotherapy followed by surgery at Tianjin Medical University Cancer Institute and Hospital between August 2018 and July 2019. The primary inclusion criteria for patients were as follows: (1) patients with resectable stage IB–IIIA NSCLC diagnosed histologically and by positron emission tomography/computed tomography (PET‐CT); (2) patients with Eastern Cooperative Oncology Group status score between 0 and 1; (3) patients with radiologically measurable target lesions and normal organ functions; and (4) patients receiving neoadjuvant immunotherapy (anti-PD-1 plus platinum-doublet chemotherapy or anti-PD-1 plus anti-CTLA-4) followed by surgery. The primary exclusion criteria were: (1) patients with EGFR, ALK, and other driver gene mutations; (2) patients previously receiving other neoadjuvant therapies; (3) patients combined with other malignant tumors; and (4) patients with active autoimmune or infectious diseases, and previous exposure to immunosuppressive drugs. Some patients were from our previous study.10 Of the 17 patients, 13 cases were treated with two or three cycles of anti-PD-1 plus platinum-doublet chemotherapy before surgical resection, and 4 cases were treated with two or three cycles of anti-PD-1 plus anti-CTLA-4 before surgical resection. The pathological response was assessed for the percentage of residual viable tumors identified on routine hematoxylin and eosin staining in resected primary tumors. Tumors were classified into MPR and non-MPR tumors. Tumors with no more than 10% viable tumor cells were considered to achieve an MPR, and those with more than 10%, non-MPR. The median follow-up time was 37 months. Formalin-fixed paraffin-embedded (FFPE) tissues were analyzed from baseline tumor biopsies and resected tumor tissues. mIHC was performed on these FFPE tissue slides. Peripheral blood samples were collected for cytokine analyses and TCRβ repertoire sequencing at three timepoints: baseline (BL), the start of treatment cycle two relative to baseline (C2), and within 2 weeks prior to surgery (S0). The peripheral blood count parameters data during routine clinical tests were collected at the same three timepoints (Fig. S1).
We analyzed another 33 patients with resectable NSCLC with stage IB–IIIA receiving 2–4 cycles of anti-PD-1 plus chemotherapy treatment followed by surgery at Tianjin Medical University Cancer Institute and Hospital between January 2019 and September 2020 to validate some results (Table S1). Baseline plasma samples were collected. The peripheral blood count parameters data were recorded at baseline and before surgery.
Sample Processing
Peripheral blood was collected in BD Vacutainer K2 EDTA tube (10ml) and centrifuged at 1600×g for 10 min to separate plasma and peripheral blood mononuclear cells (PBMCs). Supernatant plasma was transferred to a 2 mL centrifuge tube and stored at – 80 °C. PBMCs were isolated by Ficoll-Paque density gradient centrifugation.
Multiplex Cytokine Assay
Plasma cytokines were measured through the 45-ProcartaPlex human cytokine/ chemokine/growth factor panel and the 14-ProcartaPlex human immuno-oncology checkpoint panel (Afymetrix Inc., USA). Concentration values were obtained by Luminex 200 and converted to log2 format. Cytokines with more than 70% of samples below the limit of detect would be excluded. A detailed list of 59 cytokines was presented in Table S2.
Human CXCL12/SDF-1 ELISA kit (Multisciences Biotech, China) and Human SCF ELISA kit (Multisciences Biotech, China) were used to test plasma SDF-1alpha and SCF levels according to the kit manual.
TCRβ Repertoire Sequencing
The Allprep DNA/RNA mini kit extraction kit (QIAgen Inc., German) was used to extract PBMC DNA/RNA in accordance with the instructions. Oncomine™ TCR Beta SR panel kit (ThermoFisher, USA) was used for multiplex PCR amplification and library preparation. Ion library TaqMan quantitative ion kit (ThermoFisher, USA) was used for quantification, and LabChip (PerkinElmer, USA) was used for fragment distribution detection. The samples were then sequenced by the Thermo S5 platforms. Reads greater than 500,000 would be included in further analysis.
Calculation of TCR Repertoire Diversity Indexes
TCR convergence stands for the frequency of clonotypes identical in amino acid but different in nucleotide. Convergent TCRs can preferentially arise owing to T-cell responses to chronic antigen stimulation during tumor antigen-induced chronic inflammation. TCR convergence was calculated as described previously.8
Shannon was adapted to measure the clonal diversity of T-cell repertoire and calculated as: \(- \sum\nolimits_{i = 1}^R {{p_i}{{\log }_2}({p_i})}\), where pi indicates the frequency of the ith clone and R indicates the total number of clones. Samples having many clones of similar frequencies will have a high Shannon diversity.
Evenness was also known as the normalized Shannon diversity for measurement of the similarity of clone sizes and is calculated as: \(\frac{{ - \sum\nolimits_{i = 1}^R {{p_i}{{\log }_2}({p_i})} }}{{{{\log }_2}(R)}}\), where pi indicates the frequency of the ith clone and R indicates the total number of clones. Evenness values range from 0 to 1. Samples where all clones are of equal frequency have an evenness of 1, while samples having clones of unequal sizes have evenness < 1.
The clonality of the TCR repertoire was calculated as 1-Pielou index, which was calculated using the formula: \(1 + \sum\nolimits_{i = 1}^n {({p_i}*\ln ({p_i}))/\ln (n)}\), where pi indicates the frequency of the ith clone and R indicates the total number of clones. This metric is normalized to the number of unique clones and ranges from 0 to 1. The calculation of the TCR diversity index is to filter out clones with a frequency of less than 0.001%.
Multiplexed Immunohistochemistry
Two panels were designed in this study. Panel 1 comprised PD-L1, CD68, CD163, CD57, and panCK, and panel 2 included CD45RO, CD4, CD8, CD39, and FOXP3. A series of processing and staining, including epitope retrieval, endogenous peroxidase and protein blocking, antigen labeling, and tyramide signal amplification (TSA) visualization, was performed on the FFPE tissue slides according to the kit instruction (Opal 7-Color IHC Kit, PerkinElmer). Slides were scanned using the PerkinElmer Vectra V.3.0.5. Multispectral images were unmixed using spectral libraries built from images of single-stained tissue samples for each reagent using inForm Advanced Image Analysis software (inForm V.2.3.0, PerkinElmer).
Statistical Analysis
The association between categorical groups (MPR versus non-MPR) was determined using Fisher’s exact test. The Wilcoxon rank-sum test examined the continuous variable between two group comparisons. Disease-free survival (DFS) was defined as the time from the date that surgery started to the date of disease progression, with 95% confidence intervals calculated using the Kaplan–Meier method. Between-group comparisons in survival analysis were performed using the log-rank test. Statistical analysis was carried out using R 4.0.2 (R Foundation for Statistical Computing, Vienna, Austria). All tests were two-sided, and p < 0.05 was considered significant.
Results
Cytokine Analyses and Response to Neoadjuvant Immunotherapy in NSCLC
Our cohort consisted of 17 patients with resectable NSCLC who received two or three cycles of neoadjuvant immunotherapy (13 cases of anti-PD-1 plus chemotherapy and 4 cases of anti-PD-1 plus anti-CTLA-4) followed by surgery. MPR occurred in 9 of 17 patients. The clinicopathological characteristics of patients were summarized in Table 1. Patients’ baseline characteristics such as age, smoking history, histology, and clinical stage had no association with MPR (p > 0.05). There was a significant correlation between standardized uptake values (SUVmax) reduction and pathologic response (p = 0.0003) (Fig. S2).
Considering the important roles of cytokines in immunotherapy, immune-related cytokines (n = 59) were examined using plasma from patients before and during neoadjuvant immunotherapy. We first analyzed the association of baseline cytokine levels with DFS. Survival analysis showed that high levels of CD152 (also called CTLA4), low levels of SDF-1alpha (also called CXCL12), and SCF (stem cell factor, KIT ligand) at baseline were associated with unfavorable DFS (p = 0.014, 0.014, and 0.026) (Fig. 1A). Low levels of SDF-1alpha and SCF at baseline were still associated with unfavorable DFS in the anti-PD-1 plus chemotherapy subgroup (p = 0.011 and 0.011) (Fig. S3A). Dynamic change analysis revealed that the levels of HGF were significantly decreased in the MPR group after one cycle of treatment but not in the non-MPR group (Fig. 1B). A similar result was found in the anti-PD-1 plus chemotherapy subgroup (Fig. S3B).
Relationship of cytokine levels with DFS and MPR; A Kaplan–Meier curves were drawn according to baseline CD152 (p = 0.014, high versus low), SDF-1alpha (p = 0.014, high versus low), and SCF (p = 0.026, high versus low) levels, the median value was used as the threshold; B comparison of dynamic change of HGF in the MPR and non-MPR groups; BL baseline time, C2 the start of the second treatment cycle (after one cycle of neoadjuvant immunotherapy), S0 2 weeks before surgery (after 3 or 2 cycles of neoadjuvant immunotherapy)
We used larger sample numbers from another 33 patients with resectable NSCLC receiving anti-PD-1 plus chemotherapy treatment to validate the correlation between SDF-1alpha and SCF at baseline and DFS (Table S1). Baseline SDF-1alpha and SCF were detected by ELISA assays. Consistently, patients with low levels of SDF-1alpha had shorter DFS (Fig. S3C). In the multivariate analysis, SDF-1alpha remained an independent predictor for DFS (Table S3).
Cytokine Analyses and Immune-Related Adverse Events (irAEs)
In our cohort, 6 of 17 patients developed grade 1–3 irAEs following neoadjuvant immunotherapy. The most common irAEs included hypothyroidism, autoimmune thyroiditis, aminotransferase elevations, rash, and erythema; four of six patients developed more than one irAEs. The majority of irAEs occurred after two cycles of neoadjuvant immunotherapy. There were no correlations between irAEs and MPR or DFS (Fig. 2A, B). Growing evidence indicates that cytokines may be related to the occurrence of irAEs during cancer immunotherapies.11 We analyzed the association of the 59 cytokines with irAEs. Patients who developed irAEs had a trend of lower baseline MIP-1alpha levels (p = 0.055) compared with those who did not (Fig. 2C). Analysis of dynamic change of the cytokines showed a significant increase for IDO and IP-10 both after one cycle and three (or two) cycles of neoadjuvant immunotherapy in patients with irAEs but not in patients without irAEs (Fig. 2D).
Relationship between cytokines and irAE; A comparison of irAE between the MPR and non-MPR groups (p = 0.335), B Kaplan–Meier curves (p = 0.19, irAE_0 versus irAE_1), C there was a trend toward lower levels of baseline MIP-1alpha in patients who developed irAEs (p = 0.055), D cytokine levels of IDO and IP-10 in irAE_0 and irAE_1 before and during neoadjuvant immunotherapy; irAE_0 patients without irAE, irAE_1 patients with irAE
Peripheral Blood Count Parameters and Response to Neoadjuvant Immunotherapy in NSCLC
We further analyzed the association between the peripheral blood count parameters and MPR. Baseline peripheral blood count parameters did not show significant differences between the MPR and non-MPR groups. However, the platelet-to-lymphocyte ratio significantly increased after one cycle of neoadjuvant immunotherapy (p = 0.039) in the non-MPR group but not in the MPR group (Fig. 3A). Absolute monocyte count significantly increased after one cycle of neoadjuvant immunotherapy (p = 0.014) and continuously elevated after three (or two) cycles of treatment (p = 0.0078) in the non-MPR group (Fig. 3B). The patients achieving MPR after neoadjuvant immunotherapy had relatively stable monocyte count over time. A significant decrease was observed for white blood cells and neutrophil count after three (or two) cycles of treatment (p = 0.024, 0.02) and for eosinophil count after one cycle of treatment (p = 0.018) in the MPR group (Fig. 3C–E). Mean platelet volume and platelet distribution width significantly declined after one cycle of treatment in both the non-MPR group (p = 0.023, 0.022) and the MPR group (p = 0.0039, 0.014) (Fig. 3F, G).
Association of the peripheral blood count parameters with response to neoadjuvant immunotherapy; A platelet-to-lymphocyte ratio (PLR) in the MPR and non-MPR groups, absolute count of monocytes (MONO) (B), white blood cells (WBC) (C), neutrophils (NEUT) (D), and eosinophils (EO) (E) in the MPR and non-MPR groups before and during neoadjuvant immunotherapy, F, G both the MPR and non-MPR groups showed a decrease in mean platelet volume (MPV) and platelet distribution width (PDW) after neoadjuvant immunotherapy
The anti-PD-1 plus chemotherapy subgroup analysis showed that white blood cells count, neutrophil count, eosinophil count, mean platelet volume, and platelet distribution width significantly decreased after treatment in the MPR group but not in the non-MPR group, while absolute monocyte count showed a trend of progressive increase after anti-PD-1 plus chemotherapy treatment in the non-MPR group (Fig. S4A–G).
The peripheral blood count parameters from the 33 patients with NSCLC were also analyzed to validate their correlation with MPR. The MPR group consistently presented a significant decrease in white blood cells and neutrophil count after anti-PD-1 plus chemotherapy treatment (Fig. S5A–G). However, multivariate logistic analysis revealed no associations between white blood cells and neutrophil count and MPR.
There were no differences in baseline peripheral blood count parameters between the irAE and non-irAE groups (Fig. S6A). The patients with irAE showed a decrease in lymphocyte count after one cycle of treatment (p = 0.031) (Fig. S6B).
TCR Repertoire Diversity Index and Response to Neoadjuvant Immunotherapy in NSCLC
To investigate the effects of neoadjuvant immunotherapy on overall T-cell responses during cancer treatment, we performed TCR sequencing on PBMCs from 17 patients before and during neoadjuvant immunotherapy. Samples from 13 patients generated high-quality sequencing data for analysis. We first explored whether there were differences in the TCR repertoire diversity index between the MPR (n = 7) and non-MPR groups (n = 6). The peripheral baseline Shannon, evenness, clonality, and convergence showed no significant differences between the two groups (p > 0.05, Fig. S7A). However, the peripheral baseline TCR convergence was significantly lower in the non-MPR group (n = 3) than in the MPR group (n = 5) in lung squamous cell carcinoma (LUSC) (p = 0.036, Fig. 4A). The peripheral Shannon, evenness, and clonality did not change significantly after one cycle and 3 (or 2) cycles of neoadjuvant immunotherapy (p > 0.05, Fig. S7B). TCR convergence decreased after one cycle of treatment in the MPR group (p = 0.016, Fig. S7B).
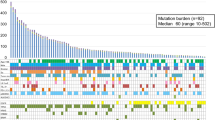
Correlation of TCR repertoire diversity indexes with MPR and DFS in patients with LUSC; A comparison of baseline Shannon, evenness, clonality, and TCR convergence in the MPR and non-MPR groups of patients with LUSC, B Kaplan–Meier curves of DFS comparing low TCR convergence (< 50%) versus high TCR convergence (≥ 50%) of patients with LUSC with neoadjuvant immunotherapy
We next analyzed the association between peripheral baseline TCR convergence and the prognosis of patients with LUSC receiving neoadjuvant immunotherapy. LUSC patients with “high” convergence had longer DFS than those with “low” convergence (not reached versus 8 months; log-rank p = 0.0067; Fig. 4B).
PD-L1 Expression and Immune Cell Infiltrates in Response to Neoadjuvant Immunotherapy in NSCLC
We performed mIHC on cancer tissues to investigate the influence of neoadjuvant immunotherapy on PD-L1 expression and intratumoral lymphocytes. Two panels were used; 9 baseline tissue samples were successfully tested by panel one and 11 baseline tissue samples by panel two. PD-L1 expression was assessed on tumor and stroma areas. The density of baseline PD-L1 expression in both tumor and stroma areas was not different between the MPR (n = 5) and non-MPR (n = 4) groups (Fig. S8A). Baseline levels of intratumoral lymphocytes were not correlated with MPR in the studied samples (Fig. S8A).
Panel one assessment was carried out on six cases with paired baseline and resection specimens, and panel two assessment on seven cases with matched specimens before and after neoadjuvant immunotherapy. A total of two, three, and one patients showed an increase, decrease, and no change in PD-L1 expression in tumor areas after treatment, respectively (p > 0.05, Figs. S5B–D). The levels of CD68+CD163+PD-L1- M2 macrophages in tumor areas showed a declination trend after neoadjuvant immunotherapy (p = 0.063), though not significantly possibly due to the small sample size (Fig. S8B–D). Neoadjuvant immunotherapy led to a significant increase of CD4+, CD4+FOXP3−, CD8+, CD8+CD45RO−, CD8+CD39+, and CD8+CD39− T-cell populations in tumor areas (p = 0.047, 0.016, 0.016, 0.031, 0.047, 0.016, respectively, Fig. 5A–C) and CD8+, CD8+CD45RO−, and CD8+CD39− T-cell populations in stromal areas (p = 0.031, 0.016, 0.016, respectively, Fig. 5A–C).
Immune cell infiltrates in response to neoadjuvant immunotherapy by mIHC; A images showed immunohistochemical staining of CD4 (orange), CD8 (green), CD39 (pink), CD45RO (red), and FOXP3 (cyan) in the paired FFPE tumor tissues before (BL) and after (S0) neoadjuvant immunotherapy, nuclei were counterstained with DAPI, magnification, ×200, B heatmap of the differences in immune cell density before (BL) and after (S0) neoadjuvant immunotherapy in tumor and stroma areas, C quantitative mIHC results of immune cell density; tumor tumor area, stromal stromal area
Discussion
Neoadjuvant immunotherapy has shown excellent efficacy on resectable NSCLC. However, the molecular characteristics associated with response to neoadjuvant immunotherapy need to be better understood. In this study, we found a decrease in HGF, white blood cells, and neutrophil count in patients with MPR after treatment of neoadjuvant immunotherapy. Baseline levels of SDF-1alpha were associated with DFS. The increase of checkpoint proteins such as IDO and IP-10 was related to irAEs. The peripheral baseline TCR convergence was associated with MPR and DFS in resectable LUSC. Neoadjuvant immunotherapy significantly increased the CD4+, CD8+, and CD8+CD39+ T cells.
Cytokines exhibited both antitumor activity by stimulating the cytotoxic activity of immune cells and protumor activity by promoting tumor immune escape. Many studies have investigated cytokines as biomarkers for predicting response to ICI therapy. Shi et al. reported that IL-1β, IFN-γ, and IL-6 were associated with efficacy and survival in advanced NSCLC receiving chemoimmunotherapy.12 However, few studies have investigated the association between peripheral cytokines and the efficiency of neoadjuvant ICIs in resectable NSCLC. We found plasma levels of SDF-1alpha at baseline had a significant association with DFS in our cohort. High SDF-1alpha expression in tumor tissues was associated with poor survival in most cancer types, and CXCL12/CXCR4 antagonists or in combination with ICIs showed antitumor activity.13,14,15 However, some studies have reported that CXCL12 is involved in the formation of tertiary lymphoid structures, which is associated with a favorable response to immunotherapy in many solid cancers.16,17,18 Blood SDF-1alpha as a prognostic factor has not been thoroughly evaluated. It still needs to validate the value of the blood levels of SDF-1alpha as a biomarker to predict the efficacy of ICIs.
We observed a correlation between the decrease in HGF concentration and neoadjuvant immunotherapy response. Supporting our findings, a high level of HGF decreased perforin secretion and was associated with a poor response to anti-PD-1 antibody treatment in advanced melanoma and NSCLC.19,20 Therefore, the role of HGF in antitumor immunotherapy response deserves further study.
Some studies have revealed the potential of peripheral immune factors, such as routinely available blood count parameters, for predicting response to immunotherapy. Despina reported that higher baseline absolute monocyte count and platelet-to-lymphocyte ratio were associated with shorter OS in patients with cancer treated with ICIs.21 Lower absolute neutrophil count after ICI treatment showed a correlation to responders in metastatic NSCLC.22 Consistent with the studies, a significant decrease was observed in white blood cells and neutrophil count in the MPR group. Our study also suggests the potential of blood count parameters as predictors for immunotherapy.
Some patients benefit from neoadjuvant immunotherapy, but some suffer from irAEs, which is difficult to predict. Currently, most studies about biomarkers exploration are based on patients with advanced NSCLC receiving immunotherapy. Several studies reported high post-treatment levels of RANTES, CXCL9, and CXCL10 in irAE patients with advanced NSCLC receiving ICI treatment.23 We found that increased IDO and IP-10 (CXCL10) levels could be related to irAEs in resectable NSCLC after neoadjuvant immunotherapy treatment. However, no correlation was observed between the baseline levels of cytokines and irAEs, suggesting that it might be more valuable to monitor the dynamic changes of cytokines than the baseline levels to identify the possible irAEs in patients. Consistent with the results revealed by Jun Oyanagi et al. in advanced NSCLC, there are neither associations nor overlapping cytokines between neoadjuvant immunotherapy efficacy and irAE onset in resectable NSCLC.
The T-cell receptor (TCR) repertoire represents the spectrum of TCR antigen specificities that the body can recognize. ICI therapy depends on T-cell antigen recognition; therefore, the TCR repertoire is an attractive biomarker to evaluate responses to checkpoint blockade.24,25 We evaluated the correlation between Shannon, evenness, and clonality, the diversity metrics commonly used in TCR repertoire, and MPR in patients with LUSC, respectively. No correlations were found. Interestingly, higher peripheral baseline TCR convergence was associated with MPR and longer DFS in patients with LUSC. Our finding was similar to the reports that increased TCR convergence was associated with durable clinical benefit in patients with NSCLC receiving ICI therapy.8,26 TCR convergence has the advantage that it may detect T-cell responses to tumor neoantigens beyond those arising from non-synonymous mutations and compare favorably with the historical performance of TMB in the periphery as a biomarker. Therefore, our results would have important implications for the establishment of predictive biomarkers through liquid biopsy approaches. Larger cohorts are warranted to evaluate these features as predictive markers for response to neoadjuvant immunotherapy and disease-free survival.
PD-L1 expression has been shown to correlate with response in advanced NSCLC treated with ICI monotherapy. However, the predictive role of PD-L1 expression remains controversial in resectable NSCLC in the setting of neoadjuvant immunotherapy. In our study, we did not find significant associations between baseline PD-L1 expression or changes in PD-L1 level from baseline to post-therapy and MPR. In support of our findings, a trial of neoadjuvant atezolizumab and chemotherapy in resectable NSCLC reported no significant association between PD-L1 expression and MPR.27 NEOSTAR trial revealed that PD-L1-negative patients also responded to neoadjuvant nivolumab and nivolumab + ipilimumab.28 Studies with large sample sizes are needed to clarify the value of PD-L1 expression for predicting a treatment benefit in the setting of neoadjuvant immunotherapy.
We observed increases in T-cell infiltration in tumors, including CD4+ and CD8+ T cells on the basis of paired pre- and post-treatment tissues, irrespective of MPR, suggesting that neoadjuvant ICIs treatments boost anti-cancer immune responses. CD39 was reported as a marker of tumor-specific and exhausted T cells. Several studies found that CD39+CD8+ T cells could predict response to ICIs in advanced NSCLC.29 Kathryn et al. reported that ICI treatment elevated the exhausted CD39+CD8+ TILs in advanced basal cell carcinoma (BCC) and squamous cell carcinoma (SCC).30 Similarly, we also observed the increase of intratumoral CD39+CD8+ T cells after neoadjuvant ICIs treatment in early stage NSCLC. CD4+ T cells tend to enhance the antitumor activity of CD8+ cytotoxic T lymphocytes. Our results indicated that the infiltration of CD4+ T cells was indeed increased after neoadjuvant ICI treatment, implying the involvement of CD4+ T cells during the action of neoadjuvant ICI treatment, but the underlying mechanisms require further study.
The current study’s limitations include but are not limited to the following: (1) the number of patients was small, and the postoperative follow-up did not reach 5 years, possibly compromising the power of statistical analyses; (2) the sample size of patients with lung adenocarcinoma (LUAD) is too small to explore the value of TCR convergence in the prediction of efficacy and prognosis of neoadjuvant immunotherapy in patients with LUAD; (3) as the difficulty of gaining enough samples, especially tissue samples, samples used for each multiplatform analysis were not fully matched, making the integration of these analyses difficult.
In conclusion, we comprehensively investigated the molecular characteristics associated with response to neoadjuvant immunotherapy using multiplatform analysis in resectable NSCLC. Our findings provide candidate biomarkers for predicting neoadjuvant immunotherapy efficacy and irAEs in resectable NSCLC. Moreover, our findings suggest that CD8+CD39+T cells and CD4+ T cells were involved in the action of neoadjuvant immunotherapy.
Data Availability
The datasets supporting the findings of this article are available from the corresponding author on reasonable request.
References
Havel JJ, Chowell D, Chan TA. The evolving landscape of biomarkers for checkpoint inhibitor immunotherapy. Nat Rev Cancer. 2019;19:133–50.
Carbone DP, Reck M, Paz-Ares L, et al. First-line nivolumab in stage IV or recurrent non-small-cell lung cancer. N Engl J Med. 2017;376:2415–26.
Gandhi L, Rodriguez-Abreu D, Gadgeel S, et al. Pembrolizumab plus chemotherapy in metastatic non-small-cell lung cancer. N Engl J Med. 2018;378:2078–92.
Provencio-Pulla M, Nadal E, Larriba JLG, et al. Nivolumab plus chemotherapy versus chemotherapy as neoadjuvant treatment for resectable stage IIIA NSCLC: primary endpoint results of pathological complete response (pCR) from phase II NADIM II trial. J Clin Oncol. 2022;40:2924.
Forde PM, Spicer J, Lu S, et al. Neoadjuvant nivolumab plus chemotherapy in resectable lung cancer. N Engl J Med. 2022;386:1973–85.
Doroshow DB, Bhalla S, Beasley MB, et al. PD-L1 as a biomarker of response to immune-checkpoint inhibitors. Nat Rev Clin Oncol. 2021;18:345–62.
Sepesi B, Swisher SG. Role of neoadjuvant chemoimmunotherapy for resectable NSCLC. Nat Rev Clin Oncol. 2022;19:497–8.
Looney TJ, Topacio-Hall D, Lowman G, et al. TCR convergence in individuals treated with immune checkpoint inhibition for cancer. Front Immunol. 2019;10:2985.
Wang M, Zhai XY, Li J, et al. The role of cytokines in predicting the response and adverse events related to immune checkpoint inhibitors. Front Immunol. 2021;12:670391.
Yue DS, Liu WR, Chen C, et al. Circulating tumor DNA predicts neoadjuvant immunotherapy efficacy and recurrence-free survival in surgical non-small cell lung cancer patients. Transl Lung Cancer R. 2022;11:263–76.
Kang JH, Bluestone JA, Young A. Predicting and preventing immune checkpoint inhibitor toxicity: targeting cytokines. Trends Immunol. 2021;42:293–311.
Shi Y, Liu X, Du J, et al. Circulating cytokines associated with clinical outcomes in advanced non-small cell lung cancer patients who received chemoimmunotherapy. Thorac Cancer. 2022;13:219–27.
Zhou WQ, Guo SC, Liu ML, et al. Targeting CXCL12/CXCR4 axis in tumor immunotherapy. Curr Med Chem. 2019;26:3026–41.
Song JS, Chang CC, Wu CH, et al. A highly selective and potent CXCR4 antagonist for hepatocellular carcinoma treatment. P Natl Acad Sci USA. 2021;118:e2015433118.
Mezzapelle R, Leo M, Caprioglio F, et al. CXCR4/CXCL12 Activities in the tumor microenvironment and implications for tumor immunotherapy. Cancers. 2022;14:2314.
Siliņa K, Soltermann A, Attar FM, et al. Germinal centers determine the prognostic relevance of tertiary lymphoid structures and are impaired by corticosteroids in lung squamous cell carcinoma. Cancer Res. 2018;78:1308–20.
Cabrita R, Lauss M, Sanna A, et al. Tertiary lymphoid structures improve immunotherapy and survival in melanoma. Nature. 2020;577:561–5.
Gong W, Zhang S, Tian X, et al. Tertiary lymphoid structures as a potential prognostic biomarker for combined hepatocellular-cholangiocarcinoma. Hepatol Int 2024. Epub ahead of print.
Kubo Y, Fukushima S, Inamori Y, et al. Serum concentrations of HGF are correlated with response to anti-PD-1 antibody therapy in patients with metastatic melanoma. J Dermatol Sci. 2019;93:33–40.
Costantini A, Takam Kamga P, Julie C, et al. Plasma biomarkers screening by multiplex ELISA assay in patients with advanced non-small cell lung cancer treated with immune checkpoint inhibitors. Cancers (Basel). 2020;13:97.
Michailidou D, Khaki AR, Morelli MP, et al. Association of blood biomarkers and autoimmunity with immune related adverse events in patients with cancer treated with immune checkpoint inhibitors. Sci Rep. 2021;11:9029.
Parikh K, Kumar A, Ahmed J, et al. Peripheral monocytes and neutrophils predict response to immune checkpoint inhibitors in patients with metastatic non-small cell lung cancer. Cancer Immunol Immunother. 2018;67:1365–70.
von Itzstein MS, Khan S, Gerber DE. Investigational biomarkers for checkpoint inhibitor immune-related adverse event prediction and diagnosis. Clin Chem. 2020;66:779–93.
Li Y, Jiao SC, Wu LL, et al. T cell receptor beta-chain repertoire analysis to reveal potential predictive biomarker for the use of immune checkpoint blockade in patients with advanced solid tumors. J Clin Oncol. 2019;37:suppl.e14152.
Zhang JJ, Ji ZC, Caushi JX, et al. Compartmental analysis of T-cell clonal dynamics as a function of pathologic response to neoadjuvant PD-1 blockade in resectable non-small cell lung cancer. Clin Cancer Res. 2020;26:1327–37.
Jermann P, Leonards K, Looney T, et al. TCR-beta repertoire convergence and evenness are associated with response to immune checkpoint inhibitors. Ann Oncol. 2019;30(Suppl 5):V851.
Shu CA, Gainor JF, Awad MM, et al. Neoadjuvant atezolizumab and chemotherapy in patients with resectable non-small-cell lung cancer: an open-label, multicentre, single-arm, phase 2 trial. Lancet Oncol. 2020;21:786–95.
Cascone T, William WN Jr, Weissferdt A, et al. Neoadjuvant nivolumab or nivolumab plus ipilimumab in operable non-small cell lung cancer: the phase 2 randomized NEOSTAR trial. Nat Med. 2021;27:504–14.
Yeong J, Suteja L, Simoni Y, et al. Intratumoral CD39(+)CD8(+) T cells predict response to programmed cell death protein-1 or programmed death ligand-1 blockade in patients with NSCLC. J Thorac Oncol. 2021;16:1349–58.
Yost KE, Satpathy AT, Wells DK, et al. Clonal replacement of tumor-specific T cells following PD-1 blockade. Nat Med. 2019;25:1251–9.
Acknowledgment
We thank all the participants contributing to this research. This work was supported by the National Natural Science Foundation of China (Grant Nos. 82273428, 82173038, 82273119).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics approval
This study was approved by the ethics committee of Tianjin Medical University Cancer Institute and Hospital (No.bc2019006). Written informed consent was obtained from all patients.
Disclosure
No potential conflict of interest was reported by the author(s). This study was approved by the ethics committee of Tianjin Medical University Cancer Institute and Hospital (No. bc2019006). Written informed consent was obtained from all patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, W., Chen, C., Li, C. et al. Comprehensive Analysis of Immune Responses to Neoadjuvant Immunotherapy in Resectable Non-small Cell Lung Cancer. Ann Surg Oncol (2024). https://doi.org/10.1245/s10434-024-16053-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1245/s10434-024-16053-7