Abstract
Background
The purpose of this study was to test for survival differences according to adjuvant chemotherapy (AC) status in radical nephroureterectomy (RNU) patients with pT2–T4 and/or N1–2 upper tract urothelial carcinoma (UTUC).
Patients and Methods
Within the Surveillance, Epidemiology, and End Results database (SEER, 2007–2020), patients with UTUC treated with AC versus RNU alone were identified. Kaplan–Meier plots and multivariable Cox regression models addressed cancer-specific mortality (CSM).
Results
Of 1995 patients with UTUC, 804 (40%) underwent AC versus 1191 (60%) RNU alone. AC rates increased from 36.1 to 57.0% over time in the overall cohort [estimated annual percentage changes (EAPC) ± 4.5%, p < 0.001]. The increase was from 28.8 to 50.0% in TanyN0 patients (EAPC ± 7.8%, p < 0.001) versus 50.0–70.9% in TanyN1–2 patients (EAPC ± 2.3%, p = 0.002). Within 698 patients harboring TanyN1–2 stage, median CSM was 31 months after AC versus 16 months in RNU alone (Δ = 15 months, p < 0.0001) and AC independently predicted lower CSM [hazard ratio (HR) 0.64; p < 0.001]. Similarly, within subgroup analyses according to stage, relative to RNU alone, AC independently predicted lower CSM in T2N1–2 (HR 0.49; p = 0.04), in T3N1–2 (HR 0.72; p = 0.015), and in T4N1–2 (HR 0.49, p < 0.001) patients. Conversely, in all TanyN0 as well as in all stage-specific subgroup analyses addressing N0 patients, AC did not affect CSM rates (all p > 0.05).
Conclusions
In RNU patients, AC use is associated with significantly lower CSM in lymph-node-positive (N1–2) patients but not in lymph-node-negative patients (N0). The distinction between N1–2 and N0 regarding the effect of AC on CSM applied across all T stages from T2 to T4, inclusively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Adjuvant chemotherapy (AC) after radical nephroureterectomy (RNU) is guideline-recommended in patients with pT2–T4 and/or N1–2 upper tract urothelial carcinoma (UTUC).1,2 Although AC after RNU demonstrated improved survival in prospective randomized trials as well as in select single-institution studies,3,4,5,6 only two small population-based studies validated its survival benefits at large.7,8 Of two prospective randomized trials that addressed this endpoint, none stratified according to N1–2 versus N0 status or according to the T stage.3,4,9 Similarly, of three population-based studies addressing AC effect on cancer-specific mortality (CSM), none stratified according to T stage or lymph node status.7,8,10 Additionally, of three population-based studies, only one relied on CSM as an endpoint.10 The remaining two did not address CSM and relied on overall mortality (OM) as a substitute.7,8 Unfortunately, such methodology may not be valid when analyses focus on groups in whom large proportions of patients remain alive or succumb to other cause mortality. In consequence, it is unknown whether AC survival benefits recorded in two prospective randomized trial applied to all T and N UTUC stages or whether its effect predominantly applies to a specific stage profile, such as N0 versus N1–2 stage. We addressed this knowledge gap and studied the relationship between AC and CSM within a large-scale contemporary UTUC population in which presence or absence of AC use is universally defined. We hypothesized that AC use is associated with lower CSM in RNU patients. To test this hypothesis, we relied on the Surveillance, Epidemiology, and End Results (SEER) database 2007–2020.
Patients and Methods
Study Population
Within the SEER database from 2007 to 2020, all patients ≥ 18 years old with histologically confirmed urothelial carcinoma of renal pelvis or ureter [International Classification of Disease (ICD-10) site code C65 and C66] and treated with RNU and lymph node dissection (surgery site codes 40 and 50) were identified. According to the 2016 World Health Organization (WHO) classification of urothelial tumors, we only included nonmetastatic patients with UTUC.11,12 Patients who underwent other surgical procedures, such as endoscopic treatment, partial nephrectomy, or segmental ureterectomy, were excluded. Patients with unknown vital status, unknown T stage, or T less than T2 and/or unknown N stage and low-grade disease were excluded. Autopsy- or death-certificate-only cases were also not included. These selection criteria resulted in 1995 assessable patients.
Definition of Variables for Analyses
Included patients were stratified according to treatment type (RNU AC vs. RNU alone). The stratification was first applied to TanyN0 versus TanyN1–2 stage groupings. Subsequently, within N0 patients’ subgroups, analyses addressed individual stages (T2 vs. T3 vs. T4). The same stratification was then applied in N1–2 patients. In all analyses, the endpoint of interest consisted of cancer-specific mortality (CSM). Covariates consisted of age at diagnosis (years, continuously coded), sex (male vs. female), tumor location (kidney and renal pelvis vs. ureter), T stage (T2, T3, and T4), N stage (N0 and N1–2) and number of lymph node removed (continuously coded) according to previous methodology.
Statistical Analyses
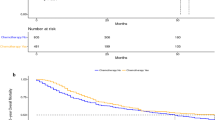
To assess CSM differences between patients with UTUC who received AC versus RNU alone, four analytical steps were completed. First, baseline characteristics were tabulated (Table 1). Descriptive statistics included medians and interquartile ranges (IQR) for continuously coded variables and frequencies and proportions for categorical variables. Wilcoxon rank sum test examined the statistical significance of medians’ differences for categorical variables. Pearson’s chi-squared test assessed the statistical significance in proportions’ differences for categorical variables. Second, estimated annual percentage changes (EAPC) described the rates of AC use over time between 2007 and 2020 in the overall population and in stage-specific patient subgroups (TanyN0 vs. TanyN1–2, Fig. 1). Third, Kaplan–Meier plots graphically depicted CSM according to treatment modality (RNU AC vs. RNU alone). Multivariable Cox regression models (CRM) addressing CSM were then fitted. This methodology first addressed TanyN0 patients (Fig. 2, Table 2). It was then re-applied to TanyN1–2 patients (Fig. 2, Table 2). Subsequently, six specific subgroup analyses focused on T2N0, T2N1–2, T3N0, T3N1, T4N0, and T4N1–2 (Figs. 3, 4, Table 2). All tests were two-sided, with a significance level p < 0.05. R software environment for statistical computing and graphics (R version 4.2.2, R Foundation for Statical Computing, Vienna Austria) was used for all analyses (3).
Results
Descriptive Characteristics of the Study Population
Overall, we identified 1995 high-grade patients with UTUC treated with RNU between 2007 and 2020 (Table 1). Of those, 804 (40%) patients received AC and 1191 (60%) received RNU alone. Relative to RNU alone patients, RNU AC patients were younger (69 vs. 73 years, IQR 62–75 vs. 66–79 years; p < 0.001). RNU AC patients harbored higher proportion of T3 (67% vs. 60%) and T4 stage (17% vs. 12%) stages, as well as higher proportion of N1–2 (47% vs. 27%, both p < 0.001) stage relative to their RNU alone counterparts. Conversely, neither statistically significant nor clinically meaningful differences were observed for sex and tumor location (both p > 0.05).
Rate of Adjuvant Systemic Therapy Over Time in RNU Patients
Among 1995 patients with UTUC, the rates of AC significantly increased over time from 36.1 to 57.0% (EAPC + 4.5%, 95% CI + 2.8 to + 6.1%, p < 0.001). In 1297 TanyN1–2 stage patients, the rates of AC use significantly increased over time from 28.8 to 50.0% (EAPC + 2.3%, 95% CI + 1.0 to + 3.5%, p = 0.002). In 698 TanyN0 stage patients, the rates of AC use significantly increased over time from 50.0 to 70.9% (EAPC + 7.8%, 95% CI + 5.1 to + 10.9%, p < 0.001).
Survival Analyses According to the Absence (TanyN0) Versus Presence (TanyN1–2) of Lymph Node Metastases in Upper Tract Urothelial Carcinoma
Survival Analyses in Lymph-Node-Positive (N1–2) Patients According to Stage
In the cohort of 698 TanyN1–2 stage patients, median cancer-specific mortality-free survival (CSM-FS) was 31 months in 381 AC patients versus 16 months in 317 RNU alone patients (Δ = 15 months, p < 0.0001). At 5 years follow-up, CSM-FS rates were 34% in RNU AC patients versus 25% in RNU alone patients (Δ = 9%, p < 0.0001). In multivariable CRM that adjusted for age, sex, and number of lymph nodes, within lymph-node-metastases-positive (TanyN1–2) patients, AC independently predicted lower CSM in T2 [hazard ratio (HR) 0.49, 95% confidence interval (CI) 0.24–0.96; p = 0.04], T3 (HR 0.72, 95% CI 0.55–0.93; p = 0.01), and T4 (HR 0.49, 95% CI 0.34–0.71; p < 0.001) stages.
Survival Analyses in Lymph-Node-Negative (N0) Patients According to Stage
In the cohort of 1297 TanyN0 stage patients, median CSM-FS of 127 months was only recorded in 874 RNU alone patients but not in 423 RNU AC patients. At 5 years follow-up, CSM-FS rates were 64% in RNU AC patients versus 61% RNU alone patients (Δ = 3%, p = 0.1). In multivariable CRM that adjusted for age, sex, and number of lymph node, within lymph node metastases negative (TanyN0) patients, AC status did not predict CSM differences in T2 (HR 0.97, 95% CI 0.57–1.66), T3 (HR 0.83, 95% CI 0.63–1.08) or T4 (HR 0.87, 95% CI 0.47–1.61) stages (all p ≥ 0.1).
Discussion
Although AC exhibited a survival benefit in two prospective randomized trials,3,4 its effect has not been tested according to the presence or absence of lymph node metastases or according to specific T stage. We addressed this knowledge gap within this large population-based cohort of patients with UTUC treated with RNU with or without AC. We made several noteworthy observations.
First, UTUC is a rare entity.1,12,13 In the Peri-Operative chemotherapy versus sUrveillance in upper Tract urothelial cancer (POUT) prospective randomized trial that relied on 51 centers and enrolled patients over 6 years, only 261 AC patients were included.3 Similarly, Cohen et al. reported a population-based study addressing 405 AC patients identified over a period of 10 years within SEER Medicare.10 The present study provides a large number of observations (n = 804) and relied on the more contemporary sample (2007–2020). Moreover, it relies on CSM as an endpoint, which is essential to avoid bias introduced by other-cause mortality when overall survival is used. Last but not the least, unlike the current analysis, it also relies on a stratification according to T and N stages.
Second, although AC use is guideline recommended, only 40% of RNU patients received such treatment within the current study. This rate represents the most contemporary estimation of AC use at large. Moreover, the rate recorded in the current study is twofold higher than the previous most contemporary estimates reported by Seisen et al.8 (23.4%). No other multi-institutional or population-based studies provide AC use estimates that could be compared with the current study or with that of Seisen et al. Within the current study, we also recorded important and statistically significant increases in AC uses over time (EAPC + 4.5%, p < 0.001; between 2007 and 2020). This increase was higher in N0 patients (EAPC +7.8%, p < 0.001) than in their N1–2 counterparts (EAPC + 2.3%, p = 0.002). Importantly, the increases recorded in the current study substantially exceeded those reported by Seisen et al., where the AC rate in the initial study year was 20% versus 22% in the final year, with a peak in 2010 study year. Taken together, these observations indicate greater use of AC in contemporary patients and a steeper increase in the adherence to AC recommendations than historically reported.8
Third, we tested for CSM differences between AC RNU versus RNU alone in TanyN0 versus TanyN1–2 patients. The overall results demonstrated a CSM benefit when AC was used after RNU versus RNU alone, in patients with lymph node metastases (TanyN1–2) as evidenced by HR of 0.6 (p < 0.001). Virtually the same results were recorded in subgroup analyses of T2 (HR 0.4), T3 (HR 0.7), and T4 (HR 0.4) stage patients with lymph node metastases (N1–2; all p ≤ 0.04). Conversely, AC status did not affect CSM in lymph-node-metastases-negative patients (N0) as well as in specific T stage subgroup analyses performed within patients with N0 UTUC (all p ≥ 0.1). These observations indicate that AC should be strongly considered in lymph-node-positive patients regardless of T stage. Absence of survival benefit recorded in patients without lymph node metastases cannot be directly interpreted as contraindication to AC in such patients. Unfortunately, the retrospective nature of the current study prevents this type of interpretation. Ideally prospective randomized trials, which included a pre-planned stratification according to presence or absence of lymph node metastases, should validate whether an equally important survival benefit applies to lymph-node-metastases-negative patients as was recorded in their lymph-node-metastases-positive counterparts.
Our study is not devoid of limitations. First and foremost, it is retrospective in nature. However, this limitation is shared with all other studies on the basis of the SEER database,14,15 National Inpatients Sample (NIS),16 or on other similar large-scale data repositories, such as National Cancer Database (NCDB).8 This design type only allows to test the association between AC and survival but does not allow to infer causality. The same limitation applies to Seisen et al.8 on the basis of the same retrospective design consideration as in the present study. Second, specific information regarding chemotherapy composition, duration, timing between surgery, and chemotherapy administration, as well as other related considerations, could not be included.17,18 Moreover, the SEER database does not provide any secondary cancer control endpoints, such as recurrence-free survival and metastasis-free survival.19 Third, specific contraindications to AC could not be used as adjustment for selection criteria, since variables such as performance status, organ function, and hematological values are not reported in the SEER database. Fourth, heterogeneity regarding tumor stage may be present because pathology was not centrally reviewed. Finally, we relied on SEER database, which only includes patients from the USA treated within SEER participating institutions. For this reason, our findings may be not generalizable to different populations, such as European or Asian patients. Additionally, our findings may not be comparable to those of patients treated at centers of excellence within the USA.
Conclusions
In RNU patients, AC use is associated with significantly lower CSM in lymph-node-positive (N1–2) patients but not in lymph-node-negative-patients (N0). The distinction between N1–2 and N0 regarding the effect of AC on CSM applied across all T stages from T2 to T4, inclusively.
Data availability
All analyses and their reporting followed the Surveillance, Epidemiology, and End Results (SEER) reporting guidelines. The dataset supporting the conclusions of this article is available in the SEER Incidence Data, 1975–2020 repository, https://seer.cancer.gov/data/. The specific datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
EAU Guidelines on Upper Urinary Tract Urothelial Cell Carcinoma - INTRODUCTION - Uroweb. Uroweb - European Association of Urology. https://uroweb.org/guidelines/upper-urinary-tract-urothelial-cell-carcinoma. Accessed 3 July 2022.
Flaig TW, Spiess PE, Abern M, et al. NCCN Guidelines® insights: bladder cancer, version 2.2022. J Natl Compr Cancer Netw. 2022;20(8):866–78. https://doi.org/10.6004/jnccn.2022.0041.
Birtle A, Johnson M, Chester J, et al. Adjuvant chemotherapy in upper tract urothelial carcinoma (the POUT trial): a phase 3, open-label, randomised controlled trial. Lancet. 2020;395(10232):1268–77. https://doi.org/10.1016/S0140-6736(20)30415-3.
Luo Y, Feng B, Wei D, et al. Adjuvant chemotherapy after radical nephroureterectomy improves the survival outcome of high-risk upper tract urothelial carcinoma patients with cardiovascular comorbidity. Sci Rep. 2020;10:17674. https://doi.org/10.1038/s41598-020-74940-x.
Kwak C, Lee SE, Jeong IG, Ku JH. Adjuvant systemic chemotherapy in the treatment of patients with invasive transitional cell carcinoma of the upper urinary tract. Urology. 2006;68(1):53–7. https://doi.org/10.1016/j.urology.2006.01.053.
Suzuki S, Shinohara N, Harabayashi T, Sato S, Abe T, Koyanagi T. Impact of adjuvant systemic chemotherapy on postoperative survival in patients with high-risk urothelial cancer. Int J Urol. 2004;11(7):456–60. https://doi.org/10.1111/j.1442-2042.2004.00841.x.
Nazzani S, Mazzone E, Preisser F, et al. Rates of lymph node invasion and their impact on cancer specific mortality in upper urinary tract urothelial carcinoma. Eur J Surg Oncol. 2019;45(7):1238–45. https://doi.org/10.1016/j.ejso.2018.12.004.
Seisen T, Krasnow RE, Bellmunt J, et al. Effectiveness of adjuvant chemotherapy after radical nephroureterectomy for locally advanced and/or positive regional lymph node upper tract urothelial carcinoma. J Clin Oncol. 2017;35(8):852–60. https://doi.org/10.1200/JCO.2016.69.4141.
Birtle AJ, Jones R, Chester J, et al. Improved disease-free survival with adjuvant chemotherapy after nephroureterectomy for upper tract urothelial cancer: final results of the POUT trial. J Clin Oncol. 2024. https://doi.org/10.1200/JCO.23.01659.
Cohen A, Kuchta K, Park S. Neoadjuvant and adjuvant chemotherapy use in upper tract urothelial carcinoma. Urol Oncol. 2017;35(6):322–7. https://doi.org/10.1016/j.urolonc.2016.11.018.
Humphrey PA, Moch H, Cubilla AL, Ulbright TM, Reuter VE. The 2016 WHO Classification of tumours of the urinary system and male genital organs-part b: prostate and bladder tumours. Eur Urol. 2016;70(1):106–19. https://doi.org/10.1016/j.eururo.2016.02.028.
Collà Ruvolo C, Nocera L, Stolzenbach LF, et al. Incidence and survival rates of contemporary patients with invasive upper tract urothelial carcinoma. Eur Urol Oncol. 2021;4(5):792–801. https://doi.org/10.1016/j.euo.2020.11.005.
Collà Ruvolo C, Nocera L, Stolzenbach LF, et al. Tumor size predicts muscle-invasive and non-organ-confined disease in upper tract urothelial carcinoma at radical nephroureterectomy. Eur Urol Focus. 2022;8(2):498–505. https://doi.org/10.1016/j.euf.2021.03.003.
Morra S, Scheipner L, Baudo A, et al. Unmarried status effect on stage at presentation and treatment patterns in non-metastatic upper tract urothelial carcinoma patients. Clin Genitourin Cancer. 2024. https://doi.org/10.1016/j.clgc.2024.102105.
de Angelis M, Baudo A, Siech C, et al. Trimodal therapy effect on survival in urothelial vs non-urothelial bladder cancer. BJU Int. 2024. https://doi.org/10.1111/bju.16333.
Siech C, Baudo A, de Angelis M, et al. Perioperative complications and in-hospital mortality in partial and radical nephrectomy patients with heart-valve replacement. Ann Surg Oncol. 2024. https://doi.org/10.1245/s10434-024-15228-6.
Califano G, Xylinas E. Re: phase II trial of neoadjuvant systemic chemotherapy followed by extirpative surgery in patients with high grade upper tract urothelial carcinoma. Eur Urol. 2020;78(1):113–4. https://doi.org/10.1016/j.eururo.2020.04.008.
Califano G, Ouzaid I, Verze P, Hermieu JF, Mirone V, Xylinas E. Immune checkpoint inhibition in upper tract urothelial carcinoma. World J Urol. 2021;39(5):1357–67. https://doi.org/10.1007/s00345-020-03502-7.
Dobé TR, Califano G, von Rundstedt FC, et al. Postoperative chemotherapy bladder instillation after radical nephroureterectomy: results of a European survey from the Young Academic Urologist Urothelial Cancer Group. Eur Urol Open Sci. 2020;22:45–50. https://doi.org/10.1016/j.euros.2020.10.003.
Funding
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Contributions
Conceptualization, F.D.B., P.I.K., L.M.I.J, and C.S.; methodology, F.D.B. and Z.T.; validation, L.M.I.J., C.C.R., and M.D.A.; formal analysis, Z.T. and F.D.B.; investigation, P.I.K, J.A.G, and F.D.B.; resources, P.A., S.M. and M.C.; data curation, F.D.B. and N.R.P; writing—original draft preparation, F.D.B., F.S., P.I.K., S.S. and N.L.; writing—review and editing, O.D.C. and A.B.; visualization, F.K.H.C., G.C. and S.M.; supervision, S.S., N.L. and A.B.; project administration, P.I.K. and F.S. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Di Bello, F., Jannello, L.M.I., Siech, C. et al. Adjuvant Systemic Therapy Improved Survival After Radical Nephroureterectomy for Upper Tract Urothelial Carcinoma. Ann Surg Oncol 31, 7229–7236 (2024). https://doi.org/10.1245/s10434-024-15814-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-024-15814-8