Abstract
Background
There is no widely employed staging system for mucosal melanoma (MuM) that incorporates all anatomic sites. We hypothesized that MuM patients arising from different anatomical sites could be staged using a common approach.
Methods
A prospective database contained 1814 MuM patients with a median follow-up of 5.14 years was employed. Overall survival (OS) was calculated from the time of pathological diagnosis to the date of death from any cause. Multivariate analyses of prognostic variables and OS were performed using the Cox proportional hazard model.
Results
For localized MuM, the most significant median OS differences were primary tumors invading submucosa (i.e., T1) versus deeper (i.e., T2/T3/T4): 4.3 versus 3.4, 3.1, and 2.9 years, respectively (p < 0.001). For patients only with regional node metastasis at presentation, the most significant were: 1 versus ≥ 2 regional nodes (N1 vs. N2, 2.5 vs. 2.1 years, p < 0.001). For patients with distant metastasis at presentation, the median OS was 1.5, 1.2, 0.8, and 0.6 years respectively for skin/subcutaneous tissue/distant lymph nodes (M1a), lung metastasis (M1b), all other visceral sites except brain (M1c), and brain (M1d) (p < 0.001). Based on these results, the staging system for MuM is proposed: (1) Stage I: T1N0M0 (median OS, 4.3 years); (2) Stage II: T2-4N0M0 (3.1 years); (3) Stage IIIA: T1-4N1M0 (2.5 years), Stage IIIB: T1-4N2M0 (2.1 years); (4) Stage IV: TanyNanyM1 (0.9 years) (p < 0.001).
Conclusions
A single, unified, staging system for mucosal melanoma inclusive of all anatomical primary tumor sites can harmonize staging of MuM and the design of clinical trials.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
A standardized staging system for mucosal melanoma (MuM) across anatomic sites has not been established. The American Joint Committee on Cancer (AJCC) 8th Edition Cancer Staging Manual only included a staging system for MuM of the head and neck region.1 Most current prognostic criteria used for classification and staging of cutaneous melanoma (CM), such as primary tumor thickness and ulceration or the use of the sentinel node biopsy for staging, have not been shown to apply to mucosal melanoma.1,2,3,4 However, MuM patients usually have poor prognosis, and a staging system is in need urgently. Previously, we examined the natural history and patterns of metastasis of 706 MuM from different anatomic sites.5 With few exceptions, the presenting stages, incidence of nodal and distant metastases, the site of predilection of distant metastases, or overall survival were similar despite different primary anatomic sites. The prognostic characteristics of MuM can be staged as a single histological group, regardless of the anatomic site of the primary tumor.6 Therefore, in this study, we combined these cohorts of mucosal melanoma from multiple anatomical sites to identify factors that could potentially be used in a unified staging system for MuM.
Methods
Database
A prospective database containing clinical and pathological information for 1814 patients with mucosal melanoma treated between December 2005 and May 2020 at the following institutions that served as the basis for prior studies5 was updated for this study: Peking University Cancer Hospital & Institute (1703 patients, 94.0%), Yunnan Cancer Hospital (55 patients, 3.0%), SUN YAT-SEN University Cancer Center (30 patients, 1.6%), and the First Hospital of Jilin University (26 patients, 1.4%) (Table 1). MuM primary anatomic sites were: nasal cavity and paranasal sinuses, oral cavity, upper gastrointestinal tract (esophageal and gastric), lower gastrointestinal tract (colon and anorectal), gynecological sites, urological sites. Patients with vulvar melanoma and anal cutaneous melanoma (i.e., with skin and its appendages in pathology) were excluded. Patients presenting with melanoma in one or more lymph nodes without a known primary tumor also were excluded from this study.
The extent of resection of the primary conformed to The NCCN Guidelines for Melanoma to guarantee the negative margin, which was similar across all surgeons for all patients. Specifically, most of the tumor in the head and neck was completely resected with negative margin, and some of them received local radiotherapy after operation. Part of the patients with gynecological or anorectum tumor underwent extended resection, and the margin was generally 1–2 cm. The others received local resection with negative margin. Usually, lymph node surgery was performed if the patients showed positive node in CT or MRI imaging without distant metastasis. Generally speaking, the number of lymph nodes in the dissection for most of head and neck tumors is at least 15, and the number of those in the dissection for most of gynecological or anorectum tumors is at least 10 according to The NCCN Guidelines for Melanoma. There was no difference in the number of nodes removed that could affect the results of the prognosis. All primary tumor pathology specimens were centrally reviewed at Peking University Cancer Hospital & Institute for presence or absence of tumor ulceration, tumor thickness (measuring depth of the primary MuM in mm), and depth (not level) of invasion). Depth of invasion was defined as follows: T1, tumor invading the mucosa or submucosa; T2, tumor invading the muscularis propria; T3, tumor invading the adventitia; T4, tumor invading adjacent structures.4,5 All patients had imaging examination to detect regional or distant metastases. Patients categorized as “clinically node negative” were based on radiographic findings, primarily by CT or MRI or PET/CT scans. Regional node staging by lymphatic mapping and sentinel node biopsy was not performed. The number of metastatic regional lymph nodes from each defined anatomic region was recorded based on lymph node dissection of clinically node-positive basin(s). Microsatellites, satellites, and in-transit metastases occurred rarely and so were not included in the analysis. All patients received baseline imaging examination for initial stage diagnosis, then every 3 months in the period of adjuvant treatment, and every 1 or 2 months for the evaluation of advanced melanoma. Almost all patients were included in the analysis. The patients who could not collect the data of the T stage were included in the Tx group. Similarly, those who could not know the N stage were included in the Nx group. These patients were enrolled in the overall population, and the factors of Tx and Nx were taken into account in the univariate and multivariate analysis.
Statistical Analyses
In our study, almost all of the patients died of progression of the melanoma. This is a retrospective study, so the data could not be collected exactly for the reason of death in every patient. We used overall survival (OS) instead of melanoma-specific survival (MSS) to describe the real situation in this study. OS was calculated from the onset of pathological diagnosis to the date of death from any cause. Survival rates were estimated by using the Kaplan-Meier method, and statistical significance was evaluated by the log-rank test. Multivariate analyses of prognostic variables and OS were performed using the Cox proportional hazard model.7 Variables with a p value < 0.10 in univariate analyses were included in multivariate analysis. Both univariate and multiple covariate analyses of OS were used to identify significant combinations of prognostic factors within the proposed stages of localized, regional nodal metastatic, or distant metastatic MuM.
Results
The data cutoff was March 20, 2021. The median follow-up was 5.14 years (95% CI 4.81–5.46). The distribution of all 1814 MuM patients based on clinical and pathological characteristics is shown in Table 1. The median age at diagnosis was 59 years, and 62.7% were female. The anatomic sites of the primary MuM were: nasal cavity and paranasal sinuses, 28.6%; oral cavity, 13.3%; upper gastrointestinal tract (esophageal and gastric), 6.7%; lower gastrointestinal tract (colon and anorectal), 25.4%; gynecological sites (excluding vulva), 22.3%; urological sites, 3.8%.
Overall, 343 MuM pts (18.9%) presented with T1 lesions (depth of invasion, mucosa or submucosa), 402 (22.2%) with T2 lesions (muscularis propria), 385 (21.2%) with T3 lesions (adventitia), 306 (16.9%) with T4 lesions (adjacent structures) and 378 (20.8%) with an unknown depth (Table 1). Tumor thickness was > 4.0 mm in 531 pts (29.3%), and tumor ulceration was present in 1035 pts (57.1%).
Among MuM patients only presenting with nodal metastases, 113 patients presented with one metastatic lymph node (32.1%), 125 had two to three metastatic lymph nodes (35.5%), and 103 had four or more metastatic lymph nodes (29.3%) (Table 1). Some patients had lymph node metastasis but without surgery. They were included in the group of stage III with Nx. However, they were not included in the group of exact N stage, such as N1, N2, and N3 group, because these patients the exact number of lymph nodes could not be determined. Among the 603 (33.2%) patients who presented with distant metastases, 87 presented with skin, subcutaneous tissue, or distant lymph nodes (14.4%), 125 had lung metastases (20.7%), 348 had metastases at other visceral metastatic sites except brain (57.7%), and 43 presented with brain metastases (with or without other sites) (7.1%; Table 1). Of the 603 patients who presented with distant metastases, 260 (43.1%) had an elevated serum LDH.
In China, resected MuM patients mainly received high-dose interferon or adjuvant temozolomide-based chemotherapy, and advanced MuM usually received chemotherapy (including dacarbazine/temozolomide, carboplatin/cisplatin, or paclitaxel) combined with anti-VEGF therapy (endostar or bevacizumab) before 2016. After 2016, almost all patients received PD-1 immunotherapy or PD-1/PDL1-based combination therapy. All patients were balanced, and the treatment did not affect the survival of patients in different years. Meanwhile, the data were not biased among MuM patients in terms of adjuvant treatment, so the relevant treatment might not affect the survival results and the staging system.
Localized Mucosal Melanoma
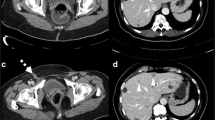
Among 660 patients who presented with localized MuM (i.e., no regional or distant metastasis at presentation), the distribution based on depth of primary tumor invasion was 28.2% for T1 tumors, 23.8% for T2 tumors, 26.2% for T3 tumors, and 21.8% for T4 tumors (Table 2). There were significant differences in median OS and 5-year survival according to depth of primary tumor invasion: T1 (4.3 years; 41.8% 5-year survival), T2 (3.4 years; 22.4% 5-year survival), T3 (3.1 years; 8.0% 5-year survival), and T4 (2.9 years; 8.6% 5-year survival) (p < 0.001; Table 2; Fig. 2a). Using the tumor thickness T-category definitions described for CM in the AJCC 8th edition staging system (i.e., ≤ 1.0 mm, 1.1–2.0 mm, 2.1–4.0 mm, and > 4.0 mm), there were no significant OS or 5-year survival differences by univariate analysis (p = 0.361) (Table 2; Fig. S1a).
Another important prognostic and staging criterion for CM is primary tumor ulceration. Overall, 57.1% of primary MuM tumors were ulcerated. However, there were no significant differences in median OS or 5-year survival comparing ulcerated versus nonulcerated MuM versus unknown (3.2 vs. 3.6 vs. 3.0 years, p = 0.057) (Table 2; Fig S1b).
The most significant primary tumor factor identified in both univariate and multivariate analysis were NRAS mutation status (p < 0.001) and the depth of invasion (p < 0.001; Table; Fig. 2a). Other factors that did not significantly correlate with OS included patient gender and age, anatomic site of primary melanoma (head and neck vs. gastrointestinal tract vs. gynecological and urological, 3.3 years vs. 3.4 years vs. 3.2 years, p = 0.926) (Table 2; Fig. 1a), and c-kit/Braf mutational status, when analyzed for the entire cohort.
Mucosal Melanoma with Regional Metastases
Various stratifications of number of nodal metastases were analyzed with respect to OS, including those categories used for CM (AJCC 8th edition melanoma staging system) (1 vs. 2–3 vs. 4 or more metastatic nodes) (Fig. S1c). We examined combinations of 1 metastatic node versus > 1 metastatic node; 1–2 metastatic nodes versus > 2; or 1–3 metastatic nodes versus > 3; and 1 versus 2 versus >2. The most significant survival differences were: 1 versus 2 or more regional metastatic nodes. The median OS was 2.5 years versus 2.1 years, and the 3-year survival was 32.6% versus 14.2% (p < 0.001; Fig. 2b). This combination was statistically significant in a multiple covariate analysis OS (p < 0.001; Table 3). Primary tumor depth of invasion also was statistically significantly associated with OS by both univariate and multiple covariate analysis.
Mucosal Melanoma with Distant Metastases
In MuM patients who presented with distant metastatic disease, the median OS and 2-year survival for distant metastases was 1.5 years and 35.1% for the skin, subcutaneous tissue, or distant lymph nodes; 1.2 years and 18.5% for lung metastases; 0.8 years and 10.1% for all other visceral metastatic sites except brain; and 0.6 years and 7.0% for brain metastases (with or without metastases at other sites) (p < 0.001; Fig. 2c). Patients with distant metastasis who had an elevated serum lactate dehydrogenase at the time of staging had a lower median OS and 2-year survival compared with those with a normal serum LDH (0.7 vs. 1.2 years, 10.7% vs. 18.8%; p < 0.001; Fig. 2d).
In multivariate analysis, site of distant metastases and serum LDH level was the most significant prognostic factor (p < 0.001; Table 4). ECOG status, depth of invasion, CKIT, and BRAF mutation status were independent predictors of overall survival in the multivariate analysis. Thus, we propose that MuM M category distant metastases can be stratified by anatomic site of the distant metastasis in similar fashion as for the CM staging criteria in the AJCC 8th edition.
Analysis of Potential Stage Groupings
We next analyzed combinations of prognostic factors that would best fit potential stage groupings. We used the same categories defined for CM in the AJCC 8th, and those combinations of independent prognostic factors resulting from our own analysis of MuM.
Stage I and II stage groups—Using the CM AJCC 8th edition as a template, we first examined whether localized MuM could be categorized using tumor thickness and ulceration; however, there were no significant survival differences (Figs. S1a and S1b). When we used combinations of T1, T2, T3, and T4 for localized mucosal melanoma, the most significant survival differences occurred when Stage I was defined as T1 only, and Stage II as any T2/T3/T4 primary tumor (Fig. 2a and e). Combinations were analyzed using the depth of primary tumor invasion criteria to select the best partitioning of survival curves. The most significant OS differences were observed when patients with T1 tumors were compared with tumors at deeper tissue penetrations as a group (i.e., T2–T4) (Fig. 2a and e). Therefore, we propose that mucosal melanoma localized to the primary mucosal site should be categorized as Stage I MuM for T1 tumors and Stage II MuM defined as any T2, T3, or T4 tumors.
Stage III stage groups—Because the most significant survival differences were observed when comparing MuM with one nodal metastasis versus two or more nodal metastases (Fig. 2b), we propose that MuM with regional node metastases should be categorized as one metastatic node (i.e., N1) for Stage IIIA disease and two or more regional metastatic nodes (i.e., N2 category) for Stage IIIB disease.
Stage IV stage groups—Consistent with AJCC staging for CM, we defined substages for stage IV MuM (Table 5).
Survival Rates and Incidence of Proposed Stage Groupings
The median OS was 4.3 years for Stage I, 3.1 years for Stage II, 2.2 years for Stage III, and 0.9 years for Stage IV (p < 0.001; Fig. 2e). The 3-year survival rates were 70.2% for Stage I, 51.6% for Stage II, 25.5% for Stage III, and 5.9% for presenting Stage IV (p < 0.001; Fig. 2e). Survival rates according to T and N categories in localized and regional MuM are shown in Table S1. And the median OS was 2.12 years (95% CI 2.00–2.25 years) and 2.08 years (95% CI 1.87–2.30 years) in the patients before and after 2016. The survival was similar between the patients before and after 2016 according to the survival curves. Using these definitions, the incidence for stage at diagnosis for our entire cohort of 1814 patients was: Stage I, 14.4%; Stage II, 32.5%; Stage III, 19.6%; and Stage IV, 33.5%. Proposed TNM staging and stage groupings for mucosal melanoma are defined in Table 5.
Discussion
To our knowledge, this is the first study proposing an evidence-based staging system for mucosal melanoma for all anatomical sites. Based on a multifactorial analysis of a large database, we recommend the TNM staging and stage grouping definitions for mucosal melanoma as listed in Table 5. The proposed staging system follows the general approach for staging of cutaneous melanoma but uses definitions based on the data analysis specific for MuM. We defined Stage I and II localized MuM based on the depth of tumor invasion, because tumor thickness and ulceration were not prognostic in this analysis. For Stage III MuM, we recommend only two categories: Stage IIIA, one metastatic node (N1); Stage IIIB, 2 or more nodal metastases (N2). For Stage IV MuM, consistent with The AJCC CM staging system, we did not propose stage IV stage groups.
A key principle of deriving MuM staging is our finding in this and previous publications that there were no survival differences of melanoma patients according to the anatomic site of the primary mucosal melanoma.5,6 Similar conclusions were made in a retrospective study of 444 German mucosal melanoma patients, where a multivariate Cox regression did not find primary tumor site as an independent prognostic factor.8 Taken together, these data support that mucosal melanomas can be staged using a common staging system, regardless of the anatomic site of the primary.1,9
For localized MuM, unlike the staging factors used for cutaneous melanoma,1,9 there are no standardized thresholds of tumor staging for mucosal melanomas using tumor thickness or level of tissue invasion. In our study, 46.4% of patients presented with locally advanced lesions (i.e., depth of invasion at least T3 or tumor thickness > 4 mm), 33.8% (223/660) of patients presented with tumor thickness > 4 mm, and 48.0% (317/660) of primary MuM penetrated to the submucosal layer or deeper (T3 or T4). Such patients have a high risk of harboring subclinical distant metastases. Nonetheless, depth of invasion was independently associated with OS, while the measured tumor thickness (in mm) was not.5,6 The prognostic value of depth of invasion has been previously explored in MuM involving oropharyngeal sites.10,11 In multiple other MuM studies, tumor thickness was associated with little or no prognostic significance.8,12,13
Several studies have reported that tumor thickness is a prognostic factor for vulvar melanoma, but the natural history, metastatic behavior, and survival rates of vulvar melanoma have generally been shown to be more consistent with those of cutaneous melanoma, not mucosal melanomas.8,13,14,15,16 Similarly, a large study of anorectal melanoma demonstrated that tumor thickness was a significant prognostic factor as a continuous variable (73% had a tumor thickness > 4.0 mm) and that tumor ulceration, present in 88% of patients, was not a significant variable.15 This study included lesions arising in the rectum (32%), anorectal junction (28%), and anal canal (40%). These sites reflect potentially heterogenous sites of origin, i.e., from either rectal mucosa (derived from endoderm) or anus (which is derived from ectoderm). We did not include melanomas derived from the ectoderm, including the anal verge, anus, or female vulva, because the natural history of such melanomas appear to behave more like those of cutaneous melanoma.
The presence of primary tumor ulceration is a significant adverse determinant of survival for patients with cutaneous melanoma.17,18 In contrast, 57.1% of primary tumors in our series of MuM were ulcerated, but this characteristic was not an independent prognostic factor for OS.6 The high frequency of tumor ulceration in these patients may have diminished the ability to discern survival differences and precluded this as a T-category factor.
The number of regional lymph node metastases was independently associated with OS.6 This is consistent with results for cutaneous melanoma.19 In several studies, the presence of nodal metastases was an independent risk factor for disease progression,8,11,12,13 including patients with lymph node metastases from vaginal and anal melanomas whose OS was significantly lower.20,21,22 Among our stage III patients, the number of metastatic nodes was detected surgically, and this factor predicted the patient’s subsequent clinical course, similar to the results of Stage III patients with cutaneous melanoma.18
Patients who present with distant metastatic mucosal melanoma at the time of initial diagnosis have a poor prognosis and OS.12,23 Among patients with Stage IV MuM in this study, the site of distant metastases was a significant prognostic factor. We defined categories M1a through M1d according to sites of distant metastases based on OS and consistent with a similar categorization in CM. Also, MuM patients with an elevated serum lactate dehydrogenase (LDH) level at the time of staging had a worse prognosis, which is similar to the findings for cutaneous melanoma, where elevated serum LDH was an independent prognostic factor that also is used as an M-category criterion.1,9 We recommend that an elevated serum LDH at the time of staging be designated in parenthesis, consistent with the staging rules used for cutaneous melanoma (8th edition).1
There are some limitations in this study. A possible limitation of this study is that the patients are all of Chinese ethnicity. Meanwhile, there is no evidence that mutational events or pathological characteristics of patients in this study are any different from the results published involving other ethnic populations.24 Another limitation of this study is that the database of patients from 2005 to 2020 spans a long time. The purpose is to expand the number of cases. Although there are some differences in the treatment of patients in different years, the overall patients are balanced and the treatment does not affect the survival of patients in different years.
The structure of head and neck MuM is special indeed, although currently the Mucosal Melanoma of the Head and Neck-American Joint Committee on Cancer (AJCC) staging system criteria is specifically applicable to it, this study provides another stage system for head and neck MuM. We also will compare the advantages and disadvantages of the two stage systems in the future, hoping to provide more choices for clinical practice. A standardized approach to staging this uncommon cancer, if validated and ultimately employed, may greatly facilitate reporting of treatment outcomes for patients with MuM and in the design, stratification, and analysis of clinical trials for such patients. Future studies are warranted to explore the potential prognostic impact of additional clinicopathological elements, as well as molecular and immune factors, to enhance risk modeling and ultimately improve clinical decision-making.25
References
Amin MB, Edge SB, Greene FL, et al. AJCC cancer staging manual. 8th edn. New York: Springer; 2017.
Gershenwald JE, Scolyer RA, Hess KR, et al. Melanoma staging: evidence-based changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin. 2017;67:472–92.
Keung EZ, Balch CM, Thompson JF, et al. Melanoma prognosis and staging. 6th edn. Cham: Springer; 2020.
Wong SL, Faries MB, Kennedy EB, et al. Sentinel lymph node biopsy and management of regional nodes in melanoma: American Society of Clinical Oncology and Society of Surgical Oncology Clinical Practice Guideline. J Clin Oncol. 2018;36(4):399–413.
Lian B, Cui CL, Zhou L, et al. The natural history and patterns of metastasis from mucosal melanoma: an analysis of 706 prospectively followed patients. Ann Oncol. 2017;28:868–73.
Cui C, Bin L, Li Z, et al. Multifactorial analysis of prognostic factors and survival rates among 706 mucosal melanoma patients. Ann Surg Oncol. 2018;25(8):2184–92.
Cox DR. Regression model and life tables. J R Stat Soc B. 1972;34:187.
Heppt MV, Roesch A, Weide B, et al. Prognostic factors and treatment outcomes in 444 patients with mucosal melanoma. Eur J Cancer. 2017;7(81):36–44.
Balch CM, Gershenwald JE, Soong SJ, et al. Final version of 2009 AJCC melanoma staging and classification. J Clin Oncol. 2009;27(36):6199–206.
Wu Y, Wang L, Ma X, et al. The existence of early stage oral mucosal melanoma: a 10-year retrospective analysis of 170 patients in a single institute. Oral Oncol. 2018;87:70–6.
Chang AE, Karnell LH, Menck HR. The National Cancer Data Base report on cutaneous and noncutaneous melanoma: a summary of 84,836 cases from the past decade. The American College of Surgeons Commission on Cancer and the American Cancer Society. Cancer. 1998;83(8):1664–78.
Altieri L, Eguchi M, Peng DH. Predictors of mucosal melanoma survival in a population-based setting. J Am Acad Dermatol. 2019;81(1):136–42.
Mehra T, Grozinger G, Mann S, et al. Primary localization and tumor thickness as prognostic factors of survival in patients with mucosal melanoma. PLoS One. 2014;9(11):e112535.
Moxley KM, Fader AN, Rose PG, et al. Malignant melanoma of the vulva: an extension of cutaneous melanoma? Gynecol Oncol. 2011;122(3):612–7.
Nagarajan P, Piao J, Ning J, et al. Prognostic model for patient survival in primary anorectal mucosal melanoma: stage at presentation determines relevance of histopathologic features. Mod Pathol. 2020;33(3):496–513.
Seifried S, Haydu LE, Quinn MJ, et al. Melanoma of the vulva and vagina: principles of staging and their relevance to management based on a clinicopathologic analysis of 85 cases. Ann Surg Oncol. 2015;22(6):1959–66.
Eriksson H, Frohm-Nilsson M, Jaras J, et al. Prognostic factors in localized invasive primary cutaneous malignant melanoma: results of a large population-based study. Br J Dermatol. 2015;172:175–86.
Lyth J, Hansson J, Ingvar C, et al. Prognostic subclassifications of T1 cutaneous melanomas based on ulceration, tumour thickness and Clark’s level of invasion: results of a population-based study from the Swedish Melanoma Register. Br J Dermatol. 2013;168:779–86.
Balch CM, Gershenwald JE, Soong SJ, et al. Multivariate analysis of prognostic factors among 2,313 patients with stage III melanoma: comparison of nodal micro metastases versus macro metastases. J Clin Oncol. 2010;28(14):2452–9.
Frumovitz M, Etchepareborda M, Sun CC, et al. Primary malignant melanoma of the vagina. Obstet Gynecol. 2010;116:1358–65.
Sugiyama VE, Chan JK, Shin JY, et al. Vulvar melanoma: a multi-variable analysis of 644 patients. Obstet Gynecol. 2007;110:296–301.
Iddings DM, Fleisig AJ, Chen SL, et al. Practice patterns and outcomes for anorectal melanoma in the USA, reviewing three decades of treatment: is more extensive surgical resection beneficial in all patients? Ann Surg Oncol. 2010;17:40–4.
Keller DS, Thomay AA, Gaughan J, et al. Outcomes in patients with mucosal melanomas. J Surg Oncol. 2013;108(8):516–20.
Sarac E, Amaral T, Keim U, et al. Prognostic factors in 161 patients with mucosal melanoma: a study of German Central Malignant Melanoma Registry. J Eur Acad Dermatol Venereol. 2020. https://doi.org/10.1111/jdv.16306.
Gershenwald JE, Scolyer RA. Melanoma staging: American Joint Committee on Cancer (AJCC) 8th edition and Beyond. Ann Surg Oncol. 2018;25(8):2105–10.
Acknowledgments
The authors thank the patients and families for making this study possible. JEG gratefully acknowledges support by the Dr. John M. Skibber Endowed Professorship and the Michael and Patricia Booker Melanoma Research Endowment.
Funding
This work was supported by grants from National Natural Science Foundation of China (No. 81972562), Beijing Municipal Administration of Hospitals Incubating Program (Code: PX2017042, PX2021046), Beijing Municipal Administration of Hospitals’ Youth Programme (Code: QML20181101).
Author information
Authors and Affiliations
Contributions
Conception and design: JG, CMB, CLC, BL, JEG. Provision of study materials or patients: CLC, BL, XSZ, DW, KL. Collection and assembly of data: JG, CLC, BL, XSZ, DW, KL, LS, YY, HT, LZ, ZHC, XNS, YK. Data analysis and interpretation: JG, CMB, CLC, BL, JEG. Manuscript writing: All authors. Final approval of manuscript: All authors. Accountable for all aspects of the work: All authors.
Corresponding author
Ethics declarations
Disclosure
Dr. Jun Guo is the member of the advisory board/consultant of MSD, Roche, Pfizer, Bayer, Novartis, Simcere, Shanghai Junshi Bioscience, and Oriengene. Jeffrey E. Gershenwald has served as a consultant and/ or on advisory boards for Merck, Novartis, Bristol-Myers Squibb, Regeneron, Syndax, outside of the current work. Xue Bai declares a merit award supported by BMS. All remaining authors have declared no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cui, C., Lian, B., Zhang, X. et al. An Evidence-Based Staging System for Mucosal Melanoma: A Proposal. Ann Surg Oncol 29, 5221–5234 (2022). https://doi.org/10.1245/s10434-022-11670-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-11670-6