Abstract
Background
Cytoreductive surgery (CRS) and administration of hyperthermic intraperitoneal chemotherapy (HIPEC) have shown their efficacy in multiple malignancies and also could offer a prognostic benefit for patients with advanced ovarian cancer.
Methods
A prospective, single-center, parallel-group, randomized phase 3 clinical trial analyzed patients with a diagnosis of carcinomatosis from ovarian cancer treated with neoadjuvant systemic chemotherapy (NACT). In this trial, 71 patients were randomized to receive CRS alone (36 patients) or CRS with HIPEC (35 patients) using cisplatin (75 mg/m2 for 60 min at 42 °C). The primary end point was disease-free survival (DFS). Overall survival (OS), morbidity, and quality of life (QoL) were the secondary end points.
Results
During a median follow-up period of 32 months, the median DFS was 12 months in the control group (CRS) and 18 months in the experimental group (CRS and HIPEC). The findings showed HIPEC to be an independent protective factor against the development of recurrence (hazard ratio [HR], 0.12, 95 % confidence interval [CI], 0.02–0.89; p = 0.038). The median OS was 45 months in the control group and 52 months in the experimental group. The respective morbidity rates for any grade (1 to 5) were respectively 58.3 % and 45.7 % (p > 0.05), with a mortality rates of 2.8 % and 2.9 % (p > 0.05). In the dimensions evaluated, CRS with or without HIPEC had no impact on QoL.
Conclusions
For patients who had advanced ovarian cancer treated with NACT, CRS and HIPEC was associated with better DFS and OS, but without a difference in postoperative morbidity, mortality, or in the QoL evaluation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Ovarian cancer is the most lethal gynecologic malignancy. Up to 75 % of patients have gynecologic malignancy diagnosed when it has spread within the peritoneal cavity.1 Some clinical trials have evaluated the administration of postoperative intraperitoneal chemotherapy after primary cytoreductive surgery (CRS), reporting better prognostic results2,3,4 but low rates of therapeutic compliance due to complications related to the catheter and systemic toxicity.5 Treatment with intraoperative hyperthermic intraperitoneal chemotherapy (HIPEC) proved to be useful for patients with peritoneal carcinomatosis from different neoplasms,6,7,8,9 and its use for patients with ovarian cancer has been gaining attention.
The phase 3 clinical trial published by a Dutch group10 reported a prognostic improvement in disease-free survival (DFS) and overall survival (OS) for patients who had epithelial ovarian cancer (EOC) treated with CRS and HIPEC using cisplatin (100 mg/m2 for 90 min at 42 °C) versus a control group without HIPEC after systemic neoadjuvant chemotherapy (NACT). The results in terms of morbidity, mortality, and quality of life (QoL) were similar between the two groups. Despite this, the use of HIPEC after CRS in ovarian cancer continues to be discussed,11 although this treatment has generated interest in the scientific community.
In this report, we describe the results of our single-center, randomized, prospective phase 3 clinical trial of interval CRS with or without HIPEC for patients with peritoneal carcinomatosis from ovarian, fallopian tube, or peritoneal cancer. The hypothesis of this study was that the administration of HIPEC for patients with peritoneal carcinomatosis from ovarian cancer allows for reductions and delays in the appearance of recurrences, thus increasing DFS and OS without causing an increase in postoperative morbidity, mortality, or subsequent QoL.
The main objective of this study was to investigate whether the administration of HIPEC with cisplatin after complete CRS improves DFS versus treatment with CRS alone. The secondary objective was to evaluate differences in OS, morbimortality, and QoL results.
Methods
Trial Design
A prospective, randomized phase 3 clinical trial (CARCINOHIPEC, NCT-02328716) was designed. This study was conducted at the General and Digestive Surgery Service of the Virgen de la Arrixaca University Hospital (Murcia, Spain) within the Fundación para la “Formación e Investigación Sanitarias” of the Region of Murcia (FFIS) and the “Instituto Murciano de Investigación Biosanitaria” (IMIB). The clinical trial was analyzed and accepted by the Ethics Committee of our hospital, and all patients signed written informed consent.
Randomization and Masking
At the time of inclusion in the study, the patients were randomized to undergo CRS alone (control arm) or CRS followed by the administration of HIPEC (experimental arm) using a simple blinded randomization system carried out by an independent committee.
Patients
The study aimed to evaluate patients with a diagnosis of primary EOC, tubal carcinoma, or primary peritoneal carcinoma (International Federation of Gynecology and Obstetrics [FIGO] stage 3B/C) who had been treated with three cycles of systemic NACT. The inclusion criteria specified patients younger than 75 years with adequate performance status (American Society of Anesthesiology [ASA] 1–3, Eastern Cooperative Oncology Group [ECOG] 0–1) and adequate systemic function who consented to participate in the study. The exclusion criteria ruled out extra-abdominal extension of the disease, unresectable peritoneal disease, intestinal obstruction, high anesthetic risk (ASA 4), pregnancy, or history of other malignant neoplasms.
Treatment
All the patients were treated with a minimum of three cycles of systemic NACT with carboplatin (AUC 5) and paclitaxel (175 mg/m2). Then, 4 weeks after the last cycle of chemotherapy, surgical intervention was planned, starting with a complete revision of the peritoneal cavity, to establish the possibility of resection. The peritoneal disease was quantified by calculating the Peritoneal Carcinomatosis Index (PCI), and the grade of cytoreduction achieved was classified according to the completeness of cytoreduction (CC) score as CC-0 (no visible macroscopic disease) or CC-1 (tumor residue <2.5 mm).
At the end of the surgery, HIPEC was administered by the open technique (Coliseum) to the patients of the experimental arm according to the following scheme: cisplatin 75 mg/m2 diluted for perfusion in 3 L of dialysis fluid (Dialisan, Shanghai Plop Medical Technology Co., Ltd. China), with circulation maintained in a constant flow of 0.5 to 0.7 L/min longer than 60 min. Two intra-abdominal thermometers positioned in the pelvis and diaphragmatic area were used to monitor the temperature during perfusion, with maintenance of a constant temperature between 42 and 43 ºC. During the intervention, the temperature was strictly controlled through an esophageal thermometer, with the objective of keeping the patient normothermic (37 ºC), using physical measures and serotherapy.
The same effort was made for all the patients to achieve complete cytoreduction regardless of the treatment arm. All the patients were treated by the same surgical team. After recovery and hospital discharge, up to six cycles of systemic adjuvant chemotherapy were completed per patient with the same carboplatin and paclitaxel scheme.
Follow-up Evaluation
All adverse events during the first 30 days after surgery were collected and classified according to the criteria established by the National Cancer Institute (NCI-CTCAE version 3.0).12 Quality-of-life parameters were evaluated by the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire-Core 30 (EORTC QLQ-C30) using the module for ovarian cancer (OV-28) and the EuroQoL Quality of Life Scale (EQ-5D). The questionnaires were completed with the help of medical staff at the time the patients were included in the trial, then again 3 months and 12 months after surgery. Follow-up assessment with a thoraco-abdominal computed tomography (CT) scan and a tumor marker (Ca125) was performed every 3 months for the first 18 months, then every 6 months until 5 years of follow-up evaluation.
End Points
The primary end point was DFS, defined as the time from surgery to disease recurrence or death, whichever occurred first. Criteria based on the serologic determination of Ca125 and radiologic findings were used to diagnose recurrent disease. The definitive diagnosis and the date established for recurrence were determined based on the results of imaging tests (CT/positron emission tomography [PET]) or the date of histologic confirmation. The secondary end points were OS, morbidity, mortality, and health-related QoL.
Statistical Analysis
The study was designed to recruit patients during a period of 48 months. Considering the study population, the expected frequency of the phenomenon was 0.025. Assuming an error of 0.01 for a 95 % confidence interval (CI), the sample size would imply the recruitment of 63 patients into each treatment arm of the study (n = 126) to achieve differences of 20 %.
The survival analysis was performed according to Kaplan-Meier curves, and comparison of the survival curves was performed with the log-rank test. To determine the association of the factors studied, a multivariate analysis of logistic regression was performed, obtaining an odds ratio with a 95 % CI.
All the results with an α value lower than 0.05 were considered significant. To study the evolution of the patients’ QoL according to the treatment arm, two-factor analysis of variance (ANOVA) tests were performed with repeated measurements of one of the factors through the general linear model (GLM) procedure and Cochran's non-parametric tests.
Role of the Funding Source
The funding was allocated for the monitoring and insurance needed to conduct the clinical trial. The sponsor had no role in the design of the study; in the collection, analysis, and interpretation of the data, in the writing of the report, or in the decision to submit the document for publication.
Results
Patient Characteristics
The recruitment period began in March 2012 and was canceled in November 2018. The database was closed for analysis on 1 February 2020, with a minimum follow-up period of 15 months after the last patient was treated. Of the 92 patients evaluated, 71 were included in the study (Fig. 1). As detailed in Table 1, no significant differences were found in the clinical, demographic, or intraoperative variables between the two treatment groups, except for the operating time, which included the HIPEC treatment phase in the experimental arm.
DFS and OS
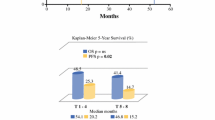
During a median follow-up period of 32 months, 49 (69 %) of the 71 patients had a disease recurrence event, and 34 patients (47.9 %) had a death event by the time the database was closed. The median DFS was 12 months in the control group (without HIPEC) and 18 months in the experimental group (with HIPEC) (Fig. 2a), with a DFS probability at 5 years of 23 % in the control group and 31 % in the experimental group.
The multivariate analysis showed that HIPEC was significantly associated with a lower risk of recurrence during the follow-up period (hazard ratio [HR], 0.12, 95 % CI, 0.02–0.89; p = 0.038; Table 2). The presence of disease in the supramesocolic compartment also was significantly associated with an increased risk of recurrence (HR, 3.48; 95 % CI, 1.14–10.64; p = 0.029). For the patients with tumor disease at that location, HIPEC administration was associated with increased DFS in the univariate analysis (9.4 months in the control group and 24.1 months in experimental group; p = 0,031; Fig. S3). The median OS was 45 months in the control group and 52 months in the experimental group (Fig. 2b). The probability of OS at 5 years was 25 % in the control group and 45 % in the experimental group.
Morbidity, Mortality, and Quality of Life
An adverse event of any grade (1 to 5) developed for 37 patients (52.1 %). Some complication (grade 3, 4, or 5) developed for 10 patients (27.8 %) in the control group and 10 patients in the experimental group (28.6 %). The difference between the two groups was not significant. Table 3 details the type of complications in both groups. The only difference was with surgical wound seroma, which occurred more frequently in the control group. Two patients died, one patient in the control group as a result of septic shock and one patient in the HIPEC group due to the development of Takotsubo cardiomyopathy (total mortality of 2.8 %).13 No anastomotic dehiscence was detected, and only one patient in the control group required the performance of a derivative stoma.
The average stay in the recovery unit was 1.4 days. The overall hospital stay was 9.6 days, with tolerance starting in an average of 1.8 days and similar results in both groups. In the multivariate analysis, HIPEC showed no relationship with the development of postoperative complications. The only factor independently related to an adverse event of any grade (1–5) was the presence of diabetes mellitus, with the occurrence of severe adverse events (grades 3 to 5 diabetes mellitus and splenectomy; Tables S2 and S3). The evaluation of all the dimensions related to the QoL showed no significant differences in relation to whether the patient was treated with or without HIPEC after CRS (Tables S4 to S13).
Discussion
Ovarian cancer is the most common cause of peritoneal carcinomatosis in women. Despite optimal surgery, intra-abdominal recurrence is frequent, prompting study of the direct intraperitoneal route in the administration of chemotherapy.
Several trials have demonstrated an increase in both OS and DFS after normothermic intraperitoneal administration of chemotherapy through an intraperitoneal catheter during the late postoperative period.2,3,4 The high systemic toxicity and morbidity with a poor QoL associated with the treatment4 has not allowed the generalization of this intraperitoneal chemotherapy scheme despite the favorable prognostic results obtained.
In the management of ovarian cancer with peritoneal dissemination, HIPEC is gaining attention. With HIPEC, a single cycle of intraperitoneal chemotherapy administered during surgery is associated with hyperthermia. The recent publication of the results from the clinical trial conducted by Van Driel et al.10 showed an improvement in both OS (+11.8 months) and DFS (+3.8 months) in favor of the patients treated with CRS and HIPEC versus the control group without HIPEC.14 In our study, treatment with HIPEC after CRS for patients who have advanced ovarian cancer treated with NACT also improved DFS (+6 months) and OS (+7 months), with no difference in postoperative morbidity, mortality, or QoL.
Some systematic reviews and meta-analyses also have reported a reduction in the risk of recurrence after the use of HIPEC for patients with EOC.15,16,17 Recently, a Chinese retrospective study using a propensity score on 584 patients with newly diagnosed ovarian cancer but no previous neoadjuvant treatment showed an improvement in OS results (+15 months in the median OS and +10.8 % in the OS at 3 years) favoring HIPEC treatment with cisplatin at a dose of 50 mg/m.2,18 However, criticism of HIPEC treatment for ovarian cancer remains frequent and intense.19,20
The current clinical trial was designed for an initial sample of 126 patients. After a period of 6 years and 8 months, 79 patients were selected, and 71 of these patients finally participated in the study. Due to a lack of funding to increase the participation of other centers in the recruitment, and especially due to the refusal of the patients to participate after hearing the results obtained in the Van Driel et al.10 trial, it was decided to suspend the recruitment of new patients after consulting the ethical committee.
This study had some limitations. First, it was not possible to reach the sample size initially proposed. However, HIPEC was an independent factor related to a lower risk of relapse (8 times lower than for the patients in the control group), which was the main objective of the study. If HIPEC treatment is effective for the minimal residual component of the disease, which is responsible for the recurrence, it seems that the time to recurrence (DFS) is the factor that will be most influenced after its administration. The sample size and the fact that relapse implies a great variety of clinical scenarios (sensitivity to platinum, possibility of treatment with multiple chemotherapy lines, characteristics and location of the relapse, and patient variables) justify the conclusion that the statistical significance of OS, a clinically valuable outcome, has not been reached.21 Furthermore, treatment with HIPEC was not related to differences in morbidity, mortality, or QoL in relation to the control group.
Second, randomization was performed before the surgical procedure and at the end of the CRS. In our center, HIPEC treatment involves the participation of multiple professionals (e.g., medical oncologists, pharmacists, perfusionists and specialized nursing staff, occupational health personnel) and specific equipment (e.g., perfusion pump, specific operating room, extended time), which makes it difficult to mobilize a number of resources systematically for the care of half the patients.
Currently, the ideal HIPEC protocol with intraperitoneal cisplatin continues to be discussed. Traditionally, the main adverse effect described has been the nephrotoxicity of cisplatin, whose rate ranges from 28 % to 36 % after systemic administration at a dose of 50 mg/m.22 Although some data suggest that at an 80-mg/m2 dose of intraperitoneal cisplatin can increase systemic toxicity and renal dysfunction,23 Van Driel et al.10 reported a rate of renal failure similar to ours (2 % after CRS and 4 % after CRS with HIPEC) with a dose of 100 mg/m2 during 90 min and the use of sodium thiosulphate for nephroprotection.
In our series, the rate of acute renal failure with a dose of 75 mg/m2 during 60 min was similar to that of the control group without the use of sodium thiosulphate (5.5 % after CRS and 2.9 % after CRS and HIPEC; p > 0.05). The optimal perfusion time also remains to be determined. As Gardner24 explained, after a certain time of peritoneal exposure of cisplatin, a plateau for the cytotoxic effect is reached. As a result, longer infusions may not offer any additional advantage, with an increased risk of systemic toxicity.
In our study, the administration of HIPEC was not related in the uni- or multivariate analysis to adverse events of any grade or to high-grade adverse events. The only complication that showed an unequal distribution between the two groups was surgical wound seroma. The effect of HIPEC on wound healing has been previously studied, and a deficit in healing with platinum-based chemotherapy and consequent decrease in tensile wound strength has been described.25 However, this phenomenon does not explain the reduction of seromas in the experimental group, so we think that this result may be due to chance. None of the 24 patients who underwent some type of digestive anastomosis experienced dehiscence during the postoperative period. However, the number of infectious complications was significantly higher among the patients with an anastomosis than among those without an anastomosis (20.8 % vs 4.3 %; p = 0.04). The derivative stoma was accurate for only one patient (temporary protective ileostomy).
Similar to other groups, we consider that the morbidity associated with intestinal resection is acceptable and therefore should be safely considered if necessary for complete elimination of the disease.26 Among the patients in our study who underwent a splenectomy, we observed an increase in infectious complications (26.7 % vs 5.4 % of patients without splenectomy; p = 0.032) such as intra-abdominal abscesses and surgical wound infections. Quality of life did not differ between the two treatment groups and remained stable during monitoring.
Based on the previously published evidence and in view of the results from the current study, we consider that HIPEC offers a prognostic advantage for patients with ovarian peritoneal carcinomatosis after NACT treatment without affecting the postoperative morbidity, mortality, or QoL associated with the procedure. Treatment with HIPEC after optimal CRS should be seriously considered for these patients.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66:7–30.
Alberts DS, Liu PY, Hannigan EV, et al. Intraperitoneal cisplatin plus intravenous cyclophosphamide versus intravenous cisplatin plus intravenous cyclophosphamide for stage III ovarian cancer. N Engl J Med. 1996;335:1950–5.
Markman M, Bundy BN, Alberts DS, et al. Phase III trial of standard-dose intravenous cisplatin plus paclitaxel versus moderately high-dose carboplatin followed by intravenous paclitaxel and intraperitoneal cisplatin in small-volume stage III ovarian carcinoma: an intergroup study of the Gynecologic Oncology Group, Southwestern Oncology Group, and Eastern Cooperative Oncology Group. J Clin Oncol. 2001;19:1001–7.
Armstrong DK, Bundy B, Wenzel L, et al. Intraperitoneal cisplatin and paclitaxel in ovarian cancer. N Engl J Med. 2006;354:34–43.
Walker JL. Intraperitoneal chemotherapy for ovarian cancer: 2009 goals. Gynecol Oncol. 2009;112:439–40.
Elias D, Benizri E, Di Pietrantonio D, Menegon P, Malka D, Raynard B. Comparison of two kinds of intraperitoneal chemotherapy following complete cytoreductive surgery of colorectal peritoneal carcinomatosis. Ann Surg Oncol. 2006;14:509–14.
Elias D, Gilly F, Quenet F, et al. Pseudomyxoma peritonei: a French multicentric study of 301 patients treated with cytoreductive surgery and intraperitoneal chemotherapy. Eur J Surg Oncol. 2010;36:456–62.
Stamou K, Tsamis D, Pallas N, et al. Treating peritoneal mesothelioma with cytoreductive surgery and hyperthermic intraperitoneal chemotherapy: a case series and review of the literature. Int J Hyperthermia. 2015;31:850–6.
Verwaal VJ, van Ruth S, de Bree E, et al. Randomized trial of cytoreduction and hyperthermic intraperitoneal chemotherapy versus systemic chemotherapy and palliative surgery in patients with peritoneal carcinomatosis of colorectal cancer. J Clin Oncol. 2003;21:3737–43.
van Driel WJ, Koole SN, Sonke GS, et al. Hyperthermic intraperitoneal chemotherapy in ovarian cancer. N Engl J Med. 2018;378:230–40.
Spriggs DR, Zivanovic O. Ovarian cancer treatment: are we getting warmer? N Engl J Med. 2018;378:293–4.
National Institutes of Health National Cancer Institute. Common Terminology Criteria for Adverse Events (CTCAE) version 3.0. Published 9 August 2006 (v3.03: 31 March 2003). Retrieved xxxx at https://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcaev3.pdf.
González-Gil A, Gómez-Ruiz ÁJ, Gil-Martínez J, et al. Tako-tsubo syndrome after intraperitoneal hyperthermic chemotherapy (HIPEC) with cisplatin: an unusual complication of cytoreductive surgery plus HIPEC. Clin Exp Metastasis. 2020;37:445–6.
Koole SN, Kieffer JM, Sikorska K, Schagen van Leeuwen JH, Schreuder HWR, Hermans RH, et al. Health-related quality of life after interval cytoreductive surgery with or without hyperthermic intraperitoneal chemotherapy (HIPEC) in patients with stage III ovarian cancer. Eur J Surg Oncol. 2019;S0748-7983:30444–5.
Wang Y, Ren F, Chen P, Liu S, Song Z, Ma X. Effects of CytoReductive surgery plus hyperthermic IntraPEritoneal chemotherapy (HIPEC) versus CytoReductive surgery for ovarian cancer patients: a systematic review and meta-analysis. Eur J Surg Oncol. 2019;45:301–9.
Wu Q, Wu Q, Xu J, et al. Efficacy of hyperthermic intraperitoneal chemotherapy in patients with epithelial ovarian cancer: a meta-analysis. Int J Hyperthermia. 2019;36:562–72.
Huo YR, Richards A, Liauw W, Morris DL. Hyperthermic intraperitoneal chemotherapy (HIPEC) and cytoreductive surgery (CRS) in ovarian cancer: a systematic review and meta-analysis. Eur J Surg Oncol. 2015;41:1578–89.
Lei Z, Wang Y, Wang J, et al. Evaluation of cytoreductive surgery with or without hyperthermic intraperitoneal chemotherapy for stage III epithelial ovarian cancer. JAMA Netw Open. 2020;3:e2013940.
Vergote I, Harter P, Chiva L. Is there a role for intraperitoneal chemotherapy, including HIPEC, in the management of ovarian cancer? J Clin Oncol. 2019;37:2420–3.
Colombo N, Sessa C, du Bois A, et al. ESMO-ESGO consensus conference on ovarian cancer: pathology and molecular biology, early and advanced stages, borderline ovarian tumours and recurrent disease. Ann Oncol. 2019;30:672–705.
Markman M. Progression-free survival versus overall survival as the primary end point in anticancer drug trials: increasingly relevant impact of therapy following progression. Curr Oncol Rep. 2009;11:1–2.
Kintzel PE. Anticancer drug-induced kidney disorders. Drug Saf. 2001;24:19–38.
Gouy S, Ferron G, Glehen O, et al. Results of a multicenter phase I dose-finding trial of hyperthermic intraperitoneal cisplatin after and complete cytoreductive surgery and followed by maintenance bevacizumab in initially unresectable ovarian cancer. Gynecol Oncol. 2016;142:237–42.
Gardner SN. A mechanistic, predictive model of dose-response curves for cell cycle phase-specific and non-specific drugs. Cancer Res. 2000;60:1417–25.
Hopkins MP, Shellhaas C, Clark T, Stakleff KS, Jenison EL. The effect of immediate intraperitoneal carboplatinum on wound healing. Gynecol Oncol. 1993;51:210–3.
Fournier M, Huchon C, Ngo C, et al. Morbidity of rectosigmoid resection in cytoreductive surgery for ovarian cancer: risk factor analysis. Eur J Surg Oncol. 2018;44:750–3.
Acknowledgment
This study was funded by the Dirección General de Farmacia y Productos Sanitarios (Ministerio Español de Sanidad, Política Social e Igualdad)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Antonio, C.C.P., Alida, G.G., Elena, G.G. et al. Cytoreductive Surgery With or Without HIPEC After Neoadjuvant Chemotherapy in Ovarian Cancer: A Phase 3 Clinical Trial. Ann Surg Oncol 29, 2617–2625 (2022). https://doi.org/10.1245/s10434-021-11087-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-11087-7