Abstract
Background
Talimogene laherparepvec (T-VEC) is an oncolytic virus approved for the treatment of unresectable, recurrent melanoma. The role of T-VEC after progression on systemic immunotherapy (IO) remains undefined. The goal of this study was to characterize the efficacy of T-VEC after failure of IO in patients with unresectable metastatic melanoma.
Methods
An international, multi-institutional review of AJCC version 8 stage IIIB-IV melanoma patients treated with T-VEC after failure of IO was performed at six centers from October 2015-December 2020. Primary outcome was in-field response; secondary outcomes included analyses of in-field and overall progression-free survival (PFS) and in-field and overall disease-free survival (DFS) after a complete response. Subset analysis of T-VEC initiation sequentially after or concurrently with IO was performed.
Results
Of 112 patients, median age at T-VEC initiation was 69 years (range 21–93); 65 (58%) were male. Before T-VEC, 57% patients received one IO regimen, 42% received two or more, with most patients (n = 74, 66%) receiving T-VEC sequential to IO. Most were stage 3C (n = 51, 46%) at T-VEC initiation, 29 (26%) received injections to nodal disease. Over median follow-up of 14 months, in-field response at final T-VEC injection was 37% complete (CR), 14% partial (PR). T-VEC initiation sequentially or concurrently did not significantly affect in-field response (p = 0.26). Median in-field PFS was 15 months (95% confidence interval 4.6-NE). Median overall DFS after CR was 32 months (95% confidence interval 17-NE).
Conclusions
T-VEC after failure of IO is effective in unresectable, metastatic stage IIIB-IV melanoma. T-VEC initiation sequentially or concurrently did not significantly affect in-field response.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Unresectable, in-transit melanoma metastases present a clinical challenge, because there is currently no established “gold standard” of treatment. Treatment options include systemic therapies and regional therapies, such as limb infusions or intralesional therapies, although it is not known which treatment is most effective.1 Talimogene laherparepvec (T-VEC) is an oncolytic virus approved for the treatment of advanced, unresectable subcutaneous, cutaneous, or nodal recurrent melanoma. FDA approval was based on the phase III OPTiM trial, which randomized patients to intralesional T-VEC or GM-CSF monotherapy until disease progression, lack of response at 12 months or no remaining injectable lesions.2 Of note, 53% of patients in this trial received prior systemic treatment. T-VEC therapy elicited superior overall response rate (ORR; 26% vs. 6%, complete response [CR] 11%) with no significant difference in median overall survival (OS; 23.3 vs. 18.9 months). Clinical studies of T-VEC monotherapy have reported ORR of 56.5–88.5% and CR of 20–61.5%, although patients in clinical settings usually have received prior treatment and often receive T-VEC as second- or later-line therapy.3,4,5,6
The advantages of T-VEC therapy are twofold. First, there is a local oncolytic effect as the virus selectively kills tumor cells at the injection site.7 It also induces an immune response through release of viral antigens, which enhances dendritic cell uptake and presentation to prime the immune system.8 This effect has been demonstrated by identification of melanoma-associated antigen recognized by T cells (MART-1)-specific CD8+ T cells in injected lesions.7,9 These mechanisms are synergistic with systemic checkpoint inhibitor immunotherapies (anti-PD-1/PD-L1 and anti-CTLA-4), which are first-line systemic agents for the treatment of advanced melanoma.10 Unfortunately, at least 40% of patients obtain no benefit from immunotherapy (IO).11 These patients are more likely to lack CD8+ T cell infiltration into the tumor.12 By combining IO with T-VEC, these patients may be rendered susceptible to IO.
The goal of this study was to characterize the clinical effect of T-VEC among patients who have disease progression while undergoing treatment with systemic IO and secondarily evaluate whether differences were apparent in the timing of T-VEC administration regarding use concurrently with or sequential to systemic IO.
Materials and Methods
Patient Selection
An international, multi-institutional retrospective study of patients treated with T-VEC was performed from October 1, 2015 to December 31, 2020. There were six participating centers: five from the United States and one from the Netherlands. All centers obtained institutional review board and/or ethics committee approval and performed independent data abstraction from medical records systems, which were provided to the coordinating center for analysis. Inclusion criteria were patients aged 18 years or older treated with intralesional T-VEC injection following disease progression on treatment with one or more lines of IO. Single-agent anti-PD-1, anti-CTLA-4 antibody, or combination therapy were allowed. Patients who received additional systemic therapies, including cytotoxic chemotherapy or experimental clinical trial drugs, and regional therapies, such as isolated limb infusion with melphalan hydroxide, were not excluded; however, we did exclude patients who received BRAF-targeted therapies without an immunomodulatory agent. Patient demographic, disease characteristics, and clinical outcomes were collected, including age at first T-VEC injection, sex, disease stage at the initiation of T-VEC, and in-field response to T-VEC therapy.
T-VEC Protocol
All patients were treated with the standard injection protocol in the outpatient setting.13,14 The first (seroconversion) cycle was a maximum of 4 mL of T-VEC injected into all visible lesions or the largest lesions at a concentration of 1 × 106 plaque-forming units (PFU)/mL. The second cycle was administered 3 weeks later at a concentration of 1 × 108 PFU/mL and continued every 2 weeks until there were no remaining injectable lesions or there was disease progression. One cycle of therapy was defined as a single treatment session in which all injectable lesions were treated. Completion of therapy was determined by the treating physician at each participating institution. A punch biopsy was performed in patients with residual pigmentation thought to have complete clinical response to confirm response.
Study Objectives and Subset Analysis
The primary outcome was in-field response to T-VEC injection. Bystander effect at distant sites was not evaluated in this study. All patients were staged at the initial T-VEC injection according to the American Joint Committee on Cancer (AJCC) 8th edition staging manual. Burden of disease (BOD) was assessed before initiation of T-VEC injections using the definition outlined by Muilenburg and Zager as follows: low BOD limited to less than ten lesions with none greater than 2 cm in maximum diameter, whereas high BOD includes more than ten distinct lesions or any single lesion greater than 2 cm in maximum diameter.15 The revised World Health Organization Handbook criteria were used to measure response to therapy, and if patients underwent surgical resection of disease after T-VEC injection, response was recorded immediately before resection.16
Secondary outcomes were exploratory analyses of in-field progression-free survival (PFS), in-field disease-free survival (DFS), overall PFS, and overall DFS. Subset analysis of the timing of T-VEC initiation relative to IO treatment was performed to assess effect on outcomes. Patients were divided into two groups regarding timing of T-VEC: (1) patients who initiated T-VEC therapy after discontinuation of IO (sequential); and (2) patients that initiated T-VEC therapy while undergoing IO (concurrent). Decision to stop IO was made at the discretion of the treating physician at each participating center. No patients were treated concurrently with T-VEC and IO as part of a separate clinical trial.
Statistical Methods
The primary outcome of in-field response was evaluated using univariable and multivariable cumulative logistic regression models built using backwards selection at an alpha level of 0.2. An exploratory analysis of the secondary outcomes (in-field PFS, in-field DFS, overall PFS, overall DFS) was performed by using Kaplan-Meier method, univariable and multivariable Cox proportional hazards models, and log-rank test. ANOVA for numerical covariates and Chi-square test for categorical covariates were used to evaluate in-field response to T-VEC (CR vs. partial response [PR] vs. no response) and timing of T-VEC initiation (sequential vs. concurrent). Outcome differences between timing of T-VEC, location of T-VEC, burden of disease, and clinical response were compared using log-rank tests. In-field PFS was calculated as the interval from the first T-VEC injection to in-field disease progression, and in-field DFS was calculated as the interval from documented complete in-field response to disease recurrence. Overall PFS was calculated as the interval from the first T-VEC injection to disease progression at any disease site, and overall DFS was calculated as the interval from documented complete response at all disease sites to disease recurrence at any site. Median follow-up time was calculated from date of first T-VEC injection to date of last known follow-up or death. P < 0.05 was considered statistically significant. All statistical analyses were performed using SAS® software version 9.4 (Copyright © 2013, SAS Institute Inc., Cary, NC).
Results
Patient and Treatment Demographics
A total of 112 patients treated with T-VEC as second- or later-line therapy after progression on IO were identified. The median age of patients at initiation of T-VEC was 69 years (range 21–93), and 58% (n = 65) of patients were male. The majority (n = 66, 59%) were BRAF wild-type. Sixty-four (57%) patients received one line of IO before T-VEC, whereas 37% (n = 41) received two, and 6% (n = 7) received three or four or more lines of therapy before T-VEC (Table 1). Anti-PD-1 therapy was the most common initial IO agent (n = 72, 64%), followed by anti-CTLA-4 (n = 26, 23%), and combination anti-PD-1/anti-CTLA-4 (n = 12, 11%). The median duration of first-line IO was 3.5 months (range 1–24.5). Best response to the first IO regimen included 11% CR (n = 13), 25% PR (n = 28), 33% stable disease (SD; n = 38), and 29% progressive disease (PD, n = 33; Table 1).
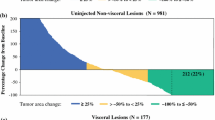
The median time from initial melanoma diagnosis to T-VEC initiation was 33 months (range 3–287). T-VEC injections were administered to concurrent nodal disease in 26% (n = 29). All patients were stage IIIB-IV at initiation of T-VEC; most were stage IIIC (n = 46, 47%). Stage IV patients at T-VEC initiation had metastatic disease at distant skin and soft tissue (n = 9, 26%), lung (n = 10. 29%), viscera (n = 8, 23%), or brain (n = 8, 23%), with median total diameter 9.7 cm2 of disease. BOD was found to be high in most patients (n = 68, 61%), with median largest lesion diameter of 2 cm (range 0.1–32) and median total number of lesions of 4 (range 1–130). All lesions were injected in 67% (n = 74) of patients. The lower extremity was the most frequently treated anatomic region (n = 61, 55%), followed by the torso (n = 21, 19%), head and neck (n = 19, 17%), and upper extremity (n = 11, 10%) regions. Patients received a median of 6 cycles of T-VEC (range 1–34) over a median 2.6 months (range 1–21) duration of T-VEC therapy. Seventy-four patients (66%) were treated sequentially, and 38 patients (34%) were treated concurrently with T-VEC and IO (Table 1). After final T-VEC injection, 8 patients (7%) with PR underwent surgical resection to no evidence of disease and 64 patients (57%) received additional therapy, most often rechallenge of systemic IO (n = 25/64, 39%), targeted systemic therapies (n = 8/64, 13%), or a sequential combination of systemic IO, targeted therapy, clinical trial, or other regional therapy. such as radiation or intralesional therapy (n = 16, 25%).
In-Field Response to T-VEC Injection
Over a median follow-up of 14 months (range 0.7–61) after T-VEC initiation, patients were found to have a median of eight clinic visits and median five imaging studies (majority use full-body PET/CT, n = 67, 60%) over the course of T-VEC treatment. The in-field ORR (CR + PR) was 51%; with CR in 41 patients (37%) and PR in 16 patients (14%). The disease-control rate (ORR + SD; DCR) was 59% (SD: n = 9, 8%). Responders also received more T-VEC treatment cycles (6.5 vs. 5 cycles, p < 0.001) over a longer duration of treatment (3.2 vs. 2 months, p < 0.001) than nonresponders. No significant difference for in-field response was found between patient age or gender, number of IO regimens administered before T-VEC, the use of T-VEC sequential to versus concurrent with IO, or injection location (Table 2).
Univariable logistic regression demonstrated a lower likelihood of in-field CR versus PR and no response to T-VEC in patients with high BOD (odds ratio [OR] 0.41, 95% confidence interval [CI] 0.2–0.85, p = 0.016) and for each unit increase in largest lesion diameter (OR 0.69, 95% CI 0.56–0.86, p < 0.001). A significantly greater likelihood of response occurred in patients with stage IIIB disease (OR 8.8, 95% CI 2.8–27.1, p < 0.001) and stage IIIC-D disease (OR 4.8, 95% CI 1.9–12.3, p < 0.001) compared with stage IV disease, longer duration of treatment (OR 1.01, 95% CI 1.0–1.01, p = 0.012), and higher total number of T-VEC cycles (OR 1.2, 95% CI 1.1–1.3, p < 0.001). On multivariable logistic regression, increasing largest lesion diameter was associated with significantly worse response (OR 0.7, p = 0.012); however, a higher total number of T-VEC cycles was associated with significantly better response (OR 1.3, p < 0.001; Table 3).
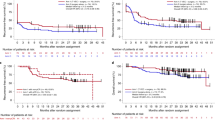
Progression-Free and Disease-Free Survival
The median in-field PFS was 14.5 months (95% CI 4.6-NE) and median overall PFS was 9.9 months (95% CI 5.0–14.9). Univariable proportional hazard modeling demonstrated that patients with greater largest lesion diameter had increasingly higher risk of both in-field (hazard ratio [HR] 1.14, 95% CI 1.1–1.2, p < 0.001) and overall (HR 1.14, 95% CI 1.1–1.2, p < 0.001) progression, and patients treated with a greater number of T-VEC treatment cycles were associated with lower risk of both in-field (HR 0.87, 95% CI 0.8–1.0, p = 0.002) and overall (HR 0.87, 95% CI 0.8–0.9, p < 0.001) progression. Patients with high BOD had significantly higher risk of both in-field (HR 1.8, 95% CI 1.0–3.2, p = 0.044; Fig. 1) and overall (HR 1.8, 95% CI 1.1–3.0, p = 0.025) progression compared with those with low BOD, and those who experienced PR were at significantly lower risk of in-field (HR 0.2, 95% CI 0.1–0.5, p < 0.001) and overall (HR 0.3, 95% CI 0.1–0.6, p < 0.001) progression compared with those with no response. A CR also significantly lowered the risk of both in-field (HR 0.0, 95% CI 0.0–0.1, p < 0.001) and overall (HR 0.1, 95% CI 0.02–0.12, p < 0.001) progression compared with those with no response (Fig. 1). While no significant difference in disease progression was found between patients with stage IIIB and stage IIIC/D disease, those with stage IV disease had significantly higher risk of both in-field (HR 3.5, 95% CI 1.5–8.0, p = 0.003) and overall (HR 4.6, 95% CI 2.1–9.8, p < 0.001) progression compared with stage IIIB disease (Table 4). On multivariable proportional hazard modeling, increasing number of T-VEC cycles (HR 0.85, 95% CI 0.76–0.96, p = 0.008) and greater largest lesion diameter (HR 1.12, 95% CI 1.04–1.2, p = 0.003) were found to significantly affect risk of in-field progression. No other variables, including sequential versus concurrent administration and location of T-VEC injections, were associated with significant differences in overall or in-field PFS.
Kaplan-Meier method analysis for overall progression-free and disease-free survival stratified by burden of disease and in-field response. A Overall progression-free survival stratified by burden of disease. B Overall progression-free survival stratified by in-field response. C Overall disease-free survival stratified by burden of disease. D Overall disease-free survival stratified by in-field response
Eight (20%) patients who demonstrated CR developed in-field recurrence at median 6 months from final T-VEC injection. Median in-field DFS and overall DFS were not reached due to a relatively low rate of disease progression after initiation of CR. When stratified by response, those with CR demonstrated a median DFS of 32 months (17-not estimable [NE]), and by BOD, those with low BOD had a median DFS of 36 months (32-NE) (Fig. 1). On univariable analysis, those who experienced CR had significantly longer in-field (HR 27.7, 95% CI 1.2–620, p = 0.002) and overall (HR 8.8, 95% CI 1.4–54.8, p = 0.005) DFS compared with those with no response, while patients demonstrating PR had no significant difference on analysis of in-field (p = 0.2) and overall (p = 0.38) DFS compared with no response. There were no significant differences found among all variables on multivariable analysis for in-field or overall DFS.
Timing of T-VEC Therapy
Comparison of sequential versus concurrent T-VEC and IO did not identify any significant differences in patient clinicopathologic characteristics or in-field response rates (Table 5). Among patients treated sequentially, the ORR was 52% (CR: 30 patients, 41%; PR: 8 patients, 11%) and those treated concurrently experienced an ORR of 50% (CR: 11 patients, 29.0%; PR: 8 patients, 21%, p = 0.25). Log-rank tests comparing in-field PFS, in-field DFS, overall PFS, and overall DFS also did not demonstrate statistically significant differences in outcomes, confirmed on univariable and multivariable proportional hazards models.
T-VEC Adverse Events
Among all treated patients, 64% (n = 72) had no reported adverse events (AE). Constitutional and flu-like symptoms (e.g., fever, chills, malaise, fatigue, myalgia, vomiting, nausea; n = 30, 27%) and injection site symptoms (e.g., dermal irritation, ulceration, infection; n = 8, 7%) were the most commonly reported AEs. Of the 40 patients who experienced AEs, 72.5% (n = 29) were grade 1, 25% (n = 10) were grade 2, 0% (n = 0) were grade 3, and 2.5% (n = 1) were grade 4. Four patients discontinued T-VEC due to AEs, all related to injection site infection. One of these four patients had preexisting drug rash with eosinophilia and systemic symptoms (DRESS) syndrome exacerbated by T-VEC injection and a second had injection site infection progress to cellulitis and sepsis classified as grade 4 as the patient required hospitalization (Table 6).
Discussion
This study demonstrated that intralesional T-VEC for unresectable, metastatic melanoma is an effective and safe treatment option for patients with disease progression on IO. While an in-field ORR of 51% was observed over a median follow-up time of 14 months, it is important to note that patients with stage IV disease derived lesser overall response from T-VEC injection after IO failure and those with lower BOD derived better overall response. Furthermore, this study demonstrated that response did not differ significantly whether T-VEC therapy was initiated sequentially after discontinuation of IO or added on concurrently. ORR remained similar between these two defined treatment groups (sequential 52% vs. concurrent 50%). Secondary outcome analysis demonstrated in-field PFS of 14.5 months and overall PFS of 9.9 months, demonstrating local control with T-VEC therapy after IO failure. Median in-field and overall DFS were not reached due to low event rate, but when stratified by response and BOD, patients with CR and low BOD demonstrated overall DFS of 32 months and 36 months, respectively.
The AE profile did not differ significantly compared with previously published studies of T-VEC monotherapy despite the timing proximity to IO treatment.5 The most commonly reported serious AEs were flu-like symptoms (e.g., fever, chills, fatigue) and diarrhea, which are known T-VEC-related AEs.12,17,18 Immune-related AEs from IO were not significantly increased in the phase II trial of T-VEC in combination with ipilimumab (19% in the combination arm vs. 18% in the ipilimumab arm).18 These results provide additional clinical evidence that combination therapy is effective for patients that have limited treatment options aside from clinical trials.
Review of the literature revealed several studies of combination T-VEC and IO for metastatic, unresectable melanoma, which report improved response rates. Two phase Ib trials exploring combination therapy have been performed. The first, by Puzanov et al., evaluated combination T-VEC and ipilimumab in 19 previously untreated stage IIIB-IVM1c melanoma patients and reported an ORR of 50% (22% CR).17 The second study, part of the phase Ib/III MASTERKEY-265 trial (NCT02263508), reported an ORR of 62% (33% CR) at median 19 months follow-up.12 Updated interim results at 37 months follow-up reported an ORR of 67%, with CR increasing to 43%.19 Median PFS has not been reached and no changes in treatment safety were reported. The only randomized trial of combination T-VEC and IO was a phase II study,18 where stage IIIB-IVM1c melanoma patients were randomized to combination T-VEC and ipilimumab versus ipilimumab alone and demonstrated improved ORR with combination therapy (39% vs. 18%). Of note, patients were not excluded if they received prior treatment. Lastly, a retrospective case series of ten stage IIIB-IV patients (4 received prior treatment) treated with combination T-VEC and anti-PD-1 therapy reported a 90% ORR and 60% CR with median follow-up of 7 months.20
While these studies address the clinical outcomes of combination T-VEC and IO, the role of T-VEC as a salvage therapy after disease progression on systemic IO has only been described in case series. In a small cohort of two patients, each patient was treated with T-VEC after failure of numerous lines of systemic therapy. One patient had a PR and the second had a CR after 23 weeks of therapy.21 While this study had too few patients for statistical measures of outcome, biopsy of metastatic lesions demonstrated infiltration of both CD4+ and CD8+ T cells, leading the authors to conclude that T-VEC therapy may induce tumor immunogenicity. Another cohort of two patients reported similar durable responses.22
Among the studies that performed biomarker analyses, significant increases in CD8+ T cells were observed after treatment which corresponded to patient response.12,17 Sun et al. observed increased levels of PD-1-expressing circulating T cells among the complete responders compared with partial responders.20 In the context of the phase Ib results from the MASTERKEY-265 trial, these studies of T-cell populations both in the tumor microenvironment and peripheral circulation support the notion that better responses may be reflected by the degree of immune priming.12,17 While we eagerly await the publications of these phase III results from the MASTERKEY-265 (NCT02263508) trial, there are two ongoing phase II studies evaluating T-VEC and pembrolizumab (NCT02965716 and MASTERKEY-115 [NCT04068181]) for melanoma. The primary objective of both studies is to evaluate the objective response rate of combination T-VEC and pembrolizumab after progression on prior anti-PD-1/PD-L1 therapy. The results from these studies are eagerly awaited to see if results from prospective trials confirm our observations.
This study is subject to the inherent limitations of retrospective studies, including selection bias, incomplete medical records and nonuniform reporting of treatment responses given the number of institutions involved. Nonetheless, this study builds on prior research supporting the synergistic effect of intratumoral T-VEC and IO. We demonstrated that T-VEC is effective not only in combination with IO, but also after failure of these agents either added in conjunction to or after discontinuation of systemic treatment. This is the largest series of patients to date in an international cohort that supports the efficacy of this treatment in the clinical setting. Prospective trials are warranted to further assess the role of T-VEC after IO failure and to better define whether the immune-priming from T-VEC is truly synergistic with IO. Identification of a patient subset who will benefit the most from intralesional therapy after IO failure may provide a better understanding of the treatment of advanced in-transit melanoma.
Conclusions
T-VEC is a safe and effective treatment option after failure of systemic immunotherapy for unresectable, metastatic stage IIIB-IV melanoma as second- or later-line therapy with the greatest benefit observed in patients with regional disease and low burden of disease. T-VEC initiation sequentially to or concurrently with systemic immunotherapy did not significantly affect in-field response. In-field complete response improved overall survival outcomes.
References
Thompson JF, Mozzillo N, Ross MI, et al. Local melanoma recurrence, satellitosis, and in-transit metastasis: incidence, outcomes, and selection of treatment options. In: CM Balch, MB Atkins, C Garbe, et al., editors. Cutaneous melanoma. Cham: Springer; 2020. p. 867–94.
Andtbacka RH, Kaufman HL, Collichio F, et al. Talimogene laherparepvec improves durable response rate in patients with advanced melanoma. J Clin Oncol. 2015;33(25):2780–8.
Perez MC, Miura JT, Naqvi SMH, et al. Talimogene laherparepvec (TVEC) for the treatment of advanced melanoma: a single-institution experience. Ann Surg Oncol. 2018;25(13):3960–5.
Perez MC, Zager JS, Amatruda T, et al. Observational study of talimogene laherparepvec use for melanoma in clinical practice in the United States (COSMUS-1). Melanoma Manag. 2019;6(2):MMT19.
Louie RJ, Perez MC, Jajja MR, et al. Real-world outcomes of talimogene laherparepvec therapy: a multi-institutional experience. J Am Coll Surg. 2019;228(4):644–9.
Franke V, Berger DMS, Klop WMC, et al. High response rates for T-VEC in early metastatic melanoma (stage IIIB/C-IVM1a). Int J Cancer. 2019;145(4):974–8.
Conry RM, Westbrook B, McKee S, Norwood TG. Talimogene laherparepvec: first in class oncolytic virotherapy. Hum Vaccin Immunother. 2018;14(4):839–46.
Liu BL, Robinson M, Han ZQ, et al. ICP34.5 deleted herpes simplex virus with enhanced oncolytic, immune stimulating, and anti-tumour properties. Gene Ther. 2003;10(4):292–303.
Kaufman HL, Bines SD. OPTIM trial: a Phase III trial of an oncolytic herpes virus encoding GM-CSF for unresectable stage III or IV melanoma. Future Oncol. 2010;6(6):941–9.
National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology, Cutaneous Melanoma version 3.2019. 2019.
Mooradian MJ, Sullivan RJ. What to do when anti-PD-1 therapy fails in patients with melanoma. Oncology (Williston Park). 2019;33(4):141–8.
Ribas A, Dummer R, Puzanov I, et al. Oncolytic virotherapy promotes intratumoral T cell infiltration and improves anti-PD-1 immunotherapy. Cell. 2017;170(6):1109-1119.e1110.
Collichio F, Burke L, Proctor A, et al. Implementing a program of talimogene laherparepvec. Ann Surg Oncol. 2018;25(7):1828–35.
Harrington KJ, Michielin O, Malvehy J, et al. A practical guide to the handling and administration of talimogene laherparepvec in Europe. Onco Targets Ther. 2017;10:3867–80.
Muilenburg DJ, Beasley GM, Thompson ZJ, Lee J-H, Tyler DS, Zager JS. Burden of disease predicts response to isolated limb infusion with melphalan and actinomycin D in melanoma. Ann Surg Oncol. 2014;22(2):482–8.
World Health Organization. WHO handbook for reporting results of cancer treatment. Geneva: World Health Organization; 1979.
Puzanov I, Milhem MM, Minor D, et al. Talimogene laherparepvec in combination with ipilimumab in previously untreated, unresectable stage IIIB-IV melanoma. J Clin Oncol. 2016;34(22):2619–26.
Chesney J, Puzanov I, Collichio F, et al. Randomized, open-label phase II study evaluating the efficacy and safety of talimogene laherparepvec in combination with ipilimumab versus ipilimumab alone in patients with advanced, unresectable melanoma. J Clin Oncol. 2018;36(17):1658–67.
Long GV, Dummer R, Andtbacka RH, et al. Follow-up analysis of MASTERKEY-265 phase 1b (ph1b) study of talimogene laherparepvec (T-VEC) in combination (combo) with pembrolizumab (pembro) in patients (pts) with unresectable stage IIIB–IVM1c melanoma (MEL). In: Society for Melanoma Research Fifteenth International Congress; October 24–27, 2018, 2018; Manchester, England.
Sun L, Funchain P, Song JM, et al. Talimogene Laherparepvec combined with anti-PD-1 based immunotherapy for unresectable stage III-IV melanoma: a case series. J Immunother Cancer. 2018;6(1):36.
Chesney J, Imbert-Fernandez Y, Telang S, et al. Potential clinical and immunotherapeutic utility of talimogene laherparepvec for patients with melanoma after disease progression on immune checkpoint inhibitors and BRAF inhibitors. Melanoma Res. 2018;28(3):250–5.
Seremet T, Planken S, Schwarze JK, et al. Successful treatment with intralesional talimogene laherparepvec in two patients with immune checkpoint inhibitor-refractory, advanced-stage melanoma. Melanoma Res. 2019;29(1):85–8.
Acknowledgments
Supported by the Biostatistics and Bioinformatics Shared Resources at Moffitt Cancer Center, Tampa, FL (P30-CA076292).
Funding
This paper was not funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
J.S. has received research funding from Amgen. A.v.A. receives advisory board and consultancy honoraria from Amgen, Bristol-Myers Squibb, Novartis, MSD-Merck, Merck-Pfizer, Sanofi and 4SC, all paid to the institution. He has received research grants from Amgen, Bristol-Myers Squibb, and Novartis, all paid to the institution. F.C.’s institution receives research funding from Amgen, Merck and Novartis, a portion of which supports her salary. J.S.Z. has advisory board relationships with Merck speaker’s bureau for Pfizer and Sun Pharma. He also receives research funding from Amgen, Delcath Systems, Philogen, Provectus and Novartis. He also is a member of the speaker’s bureau for Amgen and SunPharma. A.S.—Consulting fees and sponsored travel from Iovance Biotherapeutics Inc. Consulting fees from Guidepoint and Defined Health Inc. Honorarium and sponsored travel from Physicians' Educational Resource, LLC. Patent royalties from methods to improve adoptive cell therapy using tumor-infiltrating lymphocytes. None of the financial disclosures are related to this present work. The remaining authors have no relevant conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Carr, M.J., Sun, J., DePalo, D. et al. Talimogene Laherparepvec (T-VEC) for the Treatment of Advanced Locoregional Melanoma After Failure of Immunotherapy: An International Multi-Institutional Experience. Ann Surg Oncol 29, 791–801 (2022). https://doi.org/10.1245/s10434-021-10910-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-10910-5