Abstract
Objective
This study aimed to construct a nomogram to quantitatively predict pneumonectomy complication risks for non-small cell lung cancer (NSCLC) patients.
Methods
Data from 1052 NSCLC patients who underwent pneumonectomy were retrospectively retrieved from the databases of three thoracic centers. Multivariable logistic regression was used to investigate postoperative morbidity predictors. Clinical parameters and operative features were analyzed using univariable and multivariable logistic regression analyses, and a nomogram to predict the risk of postoperative complications was constructed using bootstrap resampling. A receiver operating characteristic (ROC) curve was used to estimate the discrimination power for the nomogram.
Results
A total of 212 patients (20.2%) had major complications. After regression analysis, forced expiratory volume in 1 s, Charlson Comorbidity Index score, male sex, and right-sided pneumonectomy were identified and entered into the nomogram. The nomogram showed a robust discrimination, with an area under the ROC curve of 0.753 (95% confidence interval 0.604–0.818). The calibration curves for the probability of postoperative complications showed optimal agreement between the nomogram and the actual probability.
Conclusions
Based on preoperative data, we developed a nomogram for predicting complication risks after pneumonectomy. This model may be helpful for thoracic surgeons in selecting appropriate patients for adopting prophylactic measures after surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Pneumonectomy is most frequently performed for the management of bronchogenic central-type carcinoma and is associated with a higher risk of mortality, morbidity, and economical cost than other types of pulmonary resection.1,2 Although postoperative complications were decreased by precise preoperative selection, improvement in operative techniques, and postoperative careful nursing, complications after pneumonectomy are still not rare and are occasionally unpredictable.3 The optimal prediction of postoperative complication risks after pneumonectomy is a growing clinical concern.
Nomograms have been accepted as a reliable tool to create a simple intuitive graph of a statistical predictive model that quantifies the risk of a clinical event.4 In this study, we aimed to identify the combination of routinely collected preoperative variables that resulted in a highly accurate prediction of postoperative complications in pneumonectomy patients. A nomogram predicting the probability of the risk of postoperative complications was then constructed to support the clinicians in their treatment recommendations.
Methods
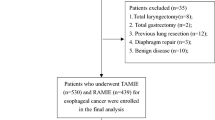
From December 2009 to December 2019, 1052 consecutive patients who underwent pneumonectomy at three lung cancer centers in China (Shanghai Pulmonary Hospital, Beijing Chest Hospital, and Peking University People’s Hospital) were retrospectively analyzed (Fig. 1). Preoperative patient characteristics, including demographics, comorbidities, and laboratory and pulmonary function test data, were extracted from the electronic medical records at the time of the initial visit. All 90-day postoperative complications were prospectively recorded and graded according to the Clavien–Dindo classification of surgical complications (Appendix 1).5 In this study, minor complications were defined as grades I and II in the Clavien–Dindo classification system, while major complications were defined as grade III or higher. This study was exempted from ethics approval by the Ethical Committee and the Institutional Review Board of all three hospitals.
Data Analysis and Statistical Methods
All statistical analyses were conducted using IBM SPSS 20.0 (IBM Corporation, Armonk, NY, USA) and R version 3.2.4 (The R Foundation for Statistical Computing, Vienna, Austria). The severity of postoperative complications was measured and was classified into two groups—the none/minor group and the major group. The linearity assumption in continuous variables was examined using restricted cubic splines, and the correlation between a major complication and clinical parameters was evaluated by univariable logistic regression. Logistic regression models were refined using backward selection with the minimal Akaike information criterion (AIC) value to obtain a good model fit but to avoid overfitting. Variables with a p-value <0.1 were entered into the backward regression multivariable analysis to identify the risks for complication factors.
A nomogram is based on a multiple logistic regression model. The score of each influencing factor on the main complications is calculated and the total score is then added. According to the function transformation relationship between the total score and the probability of outcome events, the predictive value of complications is calculated. Finally, by reading out the scores of each factor and summing them up, the corresponding complication risk can be easily found on the nomogram.
The performance of the nomogram was assessed by discrimination and calibration. The discriminative ability of the model was determined by the area under the receiver operating characteristic (ROC) curve (AUC), which ranged from 0.5 (no discrimination) to 1 (perfect discrimination).6,7 Calibration of the prediction model was performed by a visual calibration plot comparing the predicted and actual probabilities of postoperative complications. In addition, the nomogram was subjected to 1000 bootstrap resamples for internal validation to assess the predictive accuracy. All statistical tests were two tailed, with the alpha threshold of significance set at 0.05.
Results
The demographic and clinical features of patients are shown in Table 1. Overall, 93% of patients were male and the median age was 58.8 years (range 23–79). Postoperative pathology indicated that 709 cases had squamous cell carcinoma, 246 cases had adenocarcinoma, and 97 cases had other primary lung cancer. A total of 212 patients (20.2%) had major complications. The specific complications and classifications are shown in Fig. 2. The overall perioperative mortality rate was 1.8% (19/1052).
Selected Factors for the Model
After univariable analysis, variables such as sex, age, forced expiratory volume in 1 s (FEV1), FEV1%, smoking history, albumin, arterial PO2, chronic obstructive pulmonary disease (COPD), Charlson Comorbidity Index (CCI) score,8,9 neoadjuvant treatment, operation method, and surgical laterality were entered into the multivariable logistic regression analysis. Multivariable analyses showed that major complications were significantly correlated with male sex (p = 0.001), FEV1 ≤2 L (p < 0.023), CCI >3 (p = 0.007), and right-sided pneumonectomy (p = 0.003) (Table 2).
Predictive Nomogram for the Probability of Postoperative Complications
On the basis of the final regression analysis, a nomogram that incorporated the four significant risk factors for predicting postoperative complication risks was constructed (Fig. 3). The total score was calculated using the parameters of sex (male/female), FEV1 (L), CCI score, and surgical laterality (right/left). The total score could be easily calculated by adding the points from each factor. By projecting the total score to the lower total point scale, we were able to preoperatively estimate the probability of postoperative complication risks.
Performance of the Nomogram
Based on the ROC curve analysis, the nomogram showed a robust discrimination, with an AUC of 0.753 (95% confidence interval 0.604–0.818) (Fig. 4). A calibration curve of the nomogram is presented in Fig. 5, which shows that the postoperative major complication risk probabilities predicted by the nomogram were in good agreement with the actual probabilities.
Discussion
Based on the currently largest pneumonectomy database, we created a simple intuitive graph of a statistical predictive model that indicated the risk of postoperative complications. This may help clinicians in making management recommendations before surgery when patients are scheduled for pneumonectomy. In the model, FEV1, CCI score, sex, and right-sided pneumonectomy were identified as predictive factors of postoperative complications. Our nomogram displayed optimal discrimination and excellent calibration in predicting the specific possibility of postoperative complications.
A large-scale cohort study showed that the mortality rate of pneumonectomy was 7.8% and the total perioperative complication rate was 39.2%;10 however, the mortality and major complication rates in our study were 1.8% and 20.2%, respectively. Several risk-prediction models have been developed to assess the probability of complications after pneumonectomy10,11,12 and some of the factors in these models are similar to those reported in our study.
Right-sided surgery was a risk factor for the incidence of bronchopleural fistula in both our study and other literature because the left bronchial stump is better protected by the mediastinal tissue.11,13 The right lung accounts for about 55% of the ventilation function of both lungs. Right pneumonectomy leads to a more obviously imbalanced ratio of ventilation and blood flow (V/Q) than left pneumonectomy;10,14 therefore, acute respiratory distress syndrome (ARDS), heart failure, and other complications can easily develop after right pneumonectomy. In addition, the mediastinum and left lung shift obviously to the right due to a larger right chest cavity, which can compress the trachea and lead to right pneumonectomy syndrome.15,16,17 The results of this study are consistent with the above literature. Right-sided pneumonectomy was included in the nomogram as an important factor.
The age-adjusted CCI index quantifies complications based on the number and severity of diseases, which can be used to predict the death risk of diseases. Higher scores are associated with increased 3-year mortality risk in lung cancer patients.18,19,20 Blanc et al. found that the CCI index was an independent risk factor for ARDS and tracheal intubation after pneumonectomy,14 while Daffre et al. pointed out that the CCI index was closely related to perioperative death.17 In the current study, patients with a CCI index >3 had more postoperative complications, which is consistent with the above results. It is very important to evaluate the basic state of patients prior to operation.
Pulmonary function examination is important for pneumonectomy. It is generally believed that patients with FEV1 >2 L can tolerate pneumonectomy. Studies have shown that ARDS after pneumonectomy is associated with poor pulmonary function or COPD;21,22 in our study, 34 patients had postoperative ARDS. The average preoperative FEV1 was significantly lower than patients with minor complications, which is consistent with the results of previous study. A small-scale sample study found that FEV1% of the predicted value was associated with pneumonectomy survival;23 however, the prediction of FEV1 for postoperative complications is controversial. In a study that analyzed 146 patients subjected to pneumonectomy, univariable analysis showed a significant association of FEV1 with pulmonary complications, but multivariable analysis revealed that FEV1 was not an independent factor.24
In our study, male patients were more likely to develop complications than female patients; however, the number of male patients was much higher than that of female patients, which may have led to selection bias. Subgroup analysis showed that average age, smoking history, and the CCI score of female patients were lower than those of male patients, which suggests that the basic state of female patients was better than that of male patients. Cao et al. identified that male sex was a risk factor for patients who underwent robotic anatomic pulmonary resections;25 however, there are few previous reports regarding sex in relation to the complications of pneumonectomy.
However, contrary to previous reports, factors such as advanced age and American Society of Anesthesiologists score >2, were found to be non-significant predictors in our study. Elderly patients were not inclined to experience more complications compared with younger age groups. This phenomenon may be explained by a relatively lower CCI score and low proportion of elderly patients in the whole group.
The limitations of our study should be addressed. First, although our nomogram was built from a multicenter data resource, selection bias and record collection variation were inevitable factors in our model. Second, external validation by additional databases, especially from other countries, is required. Third, our nomogram only provides a whole possibility of complication risks and information on the specific type of postoperative complications was not available.
Conclusion
We developed an internally validated nomogram for predicting the risk of postoperative complications for patients who underwent pneumonectomy. The nomogram has excellent calibration and might help clinicians to make individual predictions of complications by reviewing preoperative factors prior to surgery, and make precise recommendations regarding treatment and perioperative management for patients who have received pneumonectomy.
REFERENCES
Pei G, Zhou S, Han Y, Liu Z, Xu S. Risk factors for postoperative complications after lung resection for non-small cell lung cancer in elderly patients at a single institution in China. J Thorac Dis. 2014;6(9):1230–8. https://doi.org/10.3978/j.issn.2072-1439.2014.07.23.
Handy JR Jr, Denniston K, Grunkemeier GL, Wu YX. What is the inpatient cost of hospital complications or death after lobectomy or pneumonectomy? Ann Thorac Surg. 2011;91(1):234–8. https://doi.org/10.1016/j.athoracsur.2010.08.043.
Wang G, Liu L, Zhang J, Li S. The analysis of prognosis factor in patients with non-small cell lung cancer receiving pneumonectomy. J Thorac Dis. 2020;12(4):1366–73. https://doi.org/10.21037/jtd.2020.02.33.
Iasonos A, Schrag D, Raj GV, Panageas KS. How to build and interpret a nomogram for cancer prognosis. J Clin Oncol. 2008;26(8):1364–70. https://doi.org/10.1200/JCO.2007.12.9791.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13. https://doi.org/10.1097/01.sla.0000133083.54934.ae.
Jin C, Cao J, Cai Y, et al. A nomogram for predicting the risk of invasive pulmonary adenocarcinoma for patients with solitary peripheral subsolid nodules. J Thorac Cardiovasc Surg. 2017;153(2):462-469 e1. https://doi.org/10.1016/j.jtcvs.2016.10.019.
Wang S, Yang L, Ci B, et al. Development and validation of a nomogram prognostic model for SCLC patients. J Thorac Oncol. 2018;13(9):1338–48. https://doi.org/10.1016/j.jtho.2018.05.037.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. https://doi.org/10.1016/0021-9681(87)90171-8.
Birim O, Maat AP, Kappetein AP, van Meerbeeck JP, Damhuis RA, Bogers AJ. Validation of the Charlson comorbidity index in patients with operated primary non-small cell lung cancer. Eur J Cardiothorac Surg. 2003;23(1):30–4. https://doi.org/10.1016/s1010-7940(02)00721-2.
Thomas PA, Berbis J, Baste JM, et al. Pneumonectomy for lung cancer: contemporary national early morbidity and mortality outcomes. J Thorac Cardiovasc Surg. 2015;149(1):73–82. https://doi.org/10.1016/j.jtcvs.2014.09.063.
Pforr A, Pages PB, Baste JM, et al. A Predictive Score for Bronchopleural Fistula Established Using the French Database Epithor. Ann Thorac Surg. 2016;101(1):287–93. https://doi.org/10.1016/j.athoracsur.2015.06.026.
Dong J, Mao Y, Li J, He J. Stair-Climbing Test Predicts Postoperative Cardiopulmonary Complications and Hospital Stay in Patients with Non-Small Cell Lung Cancer. Med Sci Monit. 2017;23:1436–41. https://doi.org/10.12659/msm.900631.
Mazzella A, Pardolesi A, Maisonneuve P, et al. Bronchopleural fistula after pneumonectomy: risk factors and management, focusing on open-window Thoracostomy. Semin Thorac Cardiovasc Surg Spring. 2018;30(1):104–13. https://doi.org/10.1053/j.semtcvs.2017.10.003.
Blanc K, Dechartres A, Zaimi R, et al. Patients experiencing early acute respiratory failure have high postoperative mortality after pneumonectomy. J Thorac Cardiovasc Surg. Dec 2018;156(6):2368–76. https://doi.org/10.1016/j.jtcvs.2018.08.113.
Soll C, Hahnloser D, Frauenfelder T, Russi EW, Weder W, Kestenholz PB. The postpneumonectomy syndrome: clinical presentation and treatment. Eur J Cardiothorac Surg. 2009;35(2):319–24. https://doi.org/10.1016/j.ejcts.2008.07.070.
da Silva PS, de Oliveira R, Tamura N, Neto HM. Right pneumonectomy syndrome: a late life-threatening complication of pneumonectomy. Pediatr Emerg Care. 2010;26(7):499–502. https://doi.org/10.1097/PEC.0b013e3181e5bfb3.
Daffre E, Prieto M, Huang H, et al. Normalized pulmonary artery diameter predicts occurrence of postpneumonectomy respiratory failure, ARDS, and mortality. Cancers (Basel). 2020;12(6):1515. https://doi.org/10.3390/cancers12061515.
Birim O, Kappetein AP, Bogers AJ. Charlson comorbidity index as a predictor of long-term outcome after surgery for nonsmall cell lung cancer. Eur J Cardiothorac Surg. 2005;28(5):759–62. https://doi.org/10.1016/j.ejcts.2005.06.046.
Otake S, Ohtsuka T, Asakura K, Kamiyama I, Kohno M. Impact of comorbidity index on morbidity and survival in non-small cell lung cancer. Asian Cardiovasc Thorac Ann. 2016;24(1):30–3. https://doi.org/10.1177/0218492315617834.
Yang CC, Fong Y, Lin LC, et al. The age-adjusted Charlson comorbidity index is a better predictor of survival in operated lung cancer patients than the Charlson and Elixhauser comorbidity indices. Eur J Cardiothorac Surg. 2018;53(1):235–40. https://doi.org/10.1093/ejcts/ezx215.
Mitsudomi T, Mizoue T, Yoshimatsu T, et al. Postoperative complications after pneumonectomy for treatment of lung cancer: multivariate analysis. J Surg Oncol. 1996;61(3):218–22. https://doi.org/10.1002/(SICI)1096-9098(199603)61:3%3c218::AID-JSO11%3e3.0.CO;2-3.
Rodriguez M, Gomez Hernandez MT, Novoa NM, Aranda JL, Jimenez MF, Varela G. Morbidity and mortality in octogenarians with lung cancer undergoing pneumonectomy. Arch Bronconeumol. 2015;51(5):219–22. https://doi.org/10.1016/j.arbres.2014.07.008.
Leo F, Scanagatta P, Baglio P, et al. The risk of pneumonectomy over the age of 70 A case-control study. Eur J Cardiothorac Surg. 2007;31(5):780–2. https://doi.org/10.1016/j.ejcts.2007.01.036.
Parquin F, Marchal M, Mehiri S, Herve P, Lescot B. Post-pneumonectomy pulmonary edema: analysis and risk factors. Eur J Cardiothorac Surg. 1996;10(11):929–32. https://doi.org/10.1016/s1010-7940(96)80392-7 (discussion 933).
Cao C, Louie BE, Melfi F, et al. Outcomes of major complications after robotic anatomic pulmonary resection. J Thorac Cardiovasc Surg. 2020;159(2):681–6. https://doi.org/10.1016/j.jtcvs.2019.08.057.
Acknowledgments
This study was supported by the Beijing Municipal Administration of Hospitals Incubating Program (Code: PX2021060) and the National Nature Science Foundation of China (No. 81670089). The authors thank LetPub (www.letpub.com) for their linguistic assistance during the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosure
Wang Chong, Wang Shaodong, He Wenxin, and Li Zhixin declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix 1
Rights and permissions
About this article
Cite this article
Wang, C., Wang, S., Li, Z. et al. A Multiple-Center Nomogram to Predict Pneumonectomy Complication Risk for Non-Small Cell Lung Cancer Patients. Ann Surg Oncol 29, 561–569 (2022). https://doi.org/10.1245/s10434-021-10504-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-10504-1