Abstract
Background
Some subgroups of breast cancer patients receiving neoadjuvant chemotherapy (NACT) show high rates of pathologic complete response (pCR) in the breast, proposing the possibility of omitting surgery. Prediction of pCR is dependent on accurate imaging methods. This study investigated whether magnetic resonance imaging (MRI) is better than ultrasound (US) in predicting pCR in breast cancer patients receiving NACT.
Methods
This institutional, retrospective study enrolled breast cancer patients receiving NACT who were examined by either MRI or combined US and mammography before surgery from 2016 to 2019. Imaging findings were compared with pathologic response evaluation of the tumor. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy for prediction of pCR were calculated and compared between MRI and US.
Results
Among 307 patients, 151 were examined by MRI and 156 by US. In the MRI group, 37 patients (24.5 %) had a pCR compared with 51 patients (32.7 %) in the US group. Radiologic complete response (rCR) was found in 35 patients (23.2 %) in the MRI group and 26 patients (16.7 %) in the US group. In the MRI and US groups, estimates were calculated respectively for sensitivity (87.7 % vs 91.4 %), specificity (56.8 % vs 33.3 %), PPV (86.2 % vs 73.8 %), NPV (60.0 % vs 65.4 %), and accuracy (80.1 % vs 72.4 %).
Conclusions
In predicting pCR, MRI was more specific than US, but not sufficiently specific enough to be a valid predictor of pCR for omission of surgery. As an imaging method, MRI should be preferred when future studies investigating prediction of pCR in NACT patients are planned.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Neoadjuvant chemotherapy (NACT) is increasingly used to treat larger tumors in patients with invasive breast cancer to minimize the surgical procedure and reduce its adverse effects. This has led to more breast-conserving surgery (BCS), resulting in better cosmesis and fewer axillary lymph node dissections without compromising survival.1,2,3,4
In the last decade, studies have reported complete eradication of tumor, with a pathologic complete response (pCR) in 20 % to 60 % of patients receiving NACT.1,5–7
The response of breast cancer patients to NACT varies between cancer subtypes,7–10 and studies report high rates of complete response, up to 70 % in triple-negative (estrogen receptor-negative (ER−)/human epidermal growth factor receptor 2-negative (HER2−) and HER2+ breast cancers (ER−/HER2+)7, indicating the extensive improvement in the effect of NACT. Surgery performed after NACT to ensure that no cancer remains still is advised for women with complete response on imaging,11,12 but currently is questioned due to the high rates of pCR.13,14
Diagnostic mammography (MG) combined with ultrasound (US) and magnetic resonance imaging (MRI) are the imaging methods used to measure tumor response during and after NACT. The extent of residual tumor on imaging is used by the surgeon when planning the surgical treatment.8,15,16 Overestimation of residual tumor size by imaging results in unnecessary large operations, whereas underestimation could result in multiple operations to obtain free margins. Accordingly, high accuracy of the imaging methods is crucial when surgery is planned. The possibility of omitting surgery also is highly dependent on the accuracy of the imaging method.
In 2013, a meta-analysis by Marinovich et al.17 stated that MRI and US are similar in predicting residual tumor burden compared with pathology, although further comparisons between MRI and other tests still are warranted. Later, in 2016, a study by Vriens et al.18 found US to be at least as good in predicting residual tumor size as MRI. However smaller studies have shown MRI to be a more valid predictor of pCR than US,16,19–21 leaving no definite answer as to which imaging method should be used. In Denmark, the Danish Breast Cancer Group (DBCG) suggests the use of MRI, and we hypothesized that MRI is better in predicting pCR than US.
This study aimed to investigate whether MRI is better than US in predicting pCR in breast cancer patients receiving NACT from two breast cancer centers. Furthermore, we compared the imaging prediction of pCR in receptor subgroups.
Methods
Study Population
For this institutional retrospective study, women with breast cancer receiving NACT and examined by either combined MG and US or MRI before surgery between 1 January 2016 and 31 December 2019 at Herlev Hospital or Rigshospitalet were identified using the DBCG database, the Patobank database, and the IMPAX radiology system. Information on the eligibility of identified patients was searched using original patient files.
The study enrolled women with invasive breast cancer diagnosed by core needle biopsy and planned for six series of NACT. Patients planned for eight series of NACT and patients who did not start the sixth series of NACT were excluded from the study. If surgery was performed more than 65 days after the last imaging, the patient was excluded. Patients with insufficient imaging also were excluded (Fig. 1). Ethical approval was waived by the Danish Patient Safety Authority due to the retrospective nature of the study because all the procedures performed were part of the routine care.
Inclusion of breast cancer patients planned for neoadjuvant chemotherapy (NACT) at Herlev Hospital and Rigshospitalet between 1 January 2016 and 31 December 2019. Lucidchart.com was used for the creation of this figure. DBCG, Danish Breast Cancer Group; MRI, magnetic resonance imaging; NACT, neoadjuvant chemotherapy; 6s, 6th series
The patients were allocated to treatment at either Herlev Hospital or Rigshospitalet based on their municipality. Both breast centers are highly specialized with similar diagnostic procedures.
Chemotherapeutic Protocols
The neoadjuvant treatment comprised three series of cyclophosphamid and epirubicin every third week followed by three series of taxane-based chemotherapy. The HER2+ cancers received a trastuzumab/pertuzumab-based regimen together with taxanes.
Imaging Methods
Before initiation of the neoadjuvant treatment, the initial tumor size was measured by handheld US in connection with the primary diagnostic MG, and an MR-compatible metallic coil was placed, guided by US, inside the tumor of each patient for identification of the primary tumor bed at the time of surgery. This was performed the same way in both the US and MRI groups. The initial US measurement of most patients for Herlev Hospital was performed in specific private clinics with a financial regional agreement according to the fastest logistics of the Danish Health System, and the patients were afterward referred to the breast center.
At Rigshospitalet, the initial US measurement was performed at the breast center in connection with the primary diagnostic MG. In addition, the patients in the MRI group had an MRI scan before initiation of the neoadjuvant treatment. Tumor size was evaluated after two series of NACT and before surgery using a handheld US in the US group and using an MRI in the MRI group. These scans were performed and evaluated at the breast centers by trained breast radiologists.
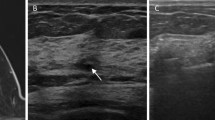
Ultrasound
The coil used in the US group was the UltraClip II Titanium Tissue Marker coil from Bard Biopsy Systems. All US procedures were performed by a trained breast radiologist with high expertise using Esaote Mylab 70XVG with a LA523 13-4MHz linear probe. The patients with no residual measurable tumor on US or MG were considered to have a radiologic complete response (rCR). The remaining patients were considered to have a non-radiologic complete response (non-rCR). Persisting suspicious and malignant calcifications were not included in the response evaluation, but recorded to aid the decision for the optimal method of surgery.
MRI
All MRI scans were performed at Rigshospitalet using either a GE 1.5 T Discovery or GE 1.5 T Optima with an eight-channel 1.5 T HD Breast Array, a Liberty 9000 8 Breast coil, and a 1.5 T HD flat gem table breast array before NACT using dynamic contrast-enhanced MRI. The coil used in the MRI group was the Ultraclip II BioDur 108 Tissue Marker coil from Bard Biopsy Systems. The following scan protocol was applied in all MR examinations: one axial T2W fast spin echo (FSE), one axial diffusion-weighted imaging (DWI), and one T1W sequence before infusion of Multihance 0.2 ml/kg at an infusion rate 1.5 ml/s.
After admission of contrast, five T1W sequences (multiphase), one T1W sagittal, and one TW (with phase AP) including subtraction recordings were performed. For agreement, the MRIs were reviewed by a senior radiologist with 7 years of experience in breast radiology, and the rCRs were doublechecked by another senior radiologist with more than 25 years of experience in breast radiology. Both radiologists were blinded to the pathologic data.
An rCR on MRI was defined as no enhancement according to tumor bed. A near rCR was defined as a minimal border of enhancement around the coil artifact and counted as a non-rCR. Any enhancement in the primary tumor bed was considered a non-rCR.
Histopathologic Analyses
Pathologic examination and immunohistochemistry (IHC) were performed according to the national guidelines of DBCG.22 Tumor molecular characteristics on biopsy were evaluated by HER2, ER, and ki-67%. An HER2 expression status of 3+ was defined as positive, with 1+ and 0 defined as negative. Tumors with a response of 2+ were further evaluated by fluorescence in situ hybridizing (FISH), and gene amplification was counted as positive. No gene amplification was counted as negative. The ER expression status was defined as positive if 1 % or more of the cells stained and negative if less than 1 % stained.
From the IHC, the tumors were divided into four subgroups; ER−/HER2−, ER−/HER2+, ER+/HER2−, and ER+/HER2+. The Ki-67 % index was evaluated manually for samples retrieved from Rigshospitalet and by automated procedure for samples retrieved from Herlev Hospital. A pCR was defined as no invasive tumor cells or ductal carcinoma in situ (DCIS) remaining. A non-pCR was defined as invasive tumor cells or DCIS remaining according to the Residual Cancer Burden classification.23,24 For the patients with multifocal cancers, only information regarding the largest tumor was collected for this study. The response in lymph nodes was not included in this study.
Statistical Analyses
Baseline characteristics were compared between the US and MRI groups using the chi-square test for the categorical variables and Student's t test for comparison of means for continuous variables. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy were calculated for each group and further calculated in receptor subgroups. True-positive (TP) was defined as non-pCR and non-radiologic complete response (rCR), and true-negative (TN) was defined as pCR and rCR. False-positive (FP) was defined as pCR and non-rCR, and false-negative (FN) was defined as non-pCR and rCR. Sensitivity was calculated by TP/(TP+FN), specificity by TN/(TN+FP), PPV by TP/(TP+FP), NPV by TN/(TN+FN), and accuracy by (TP+TN)/(TP+TN+FP+FN). Comparison to determine a difference between proportions was performed between the groups evaluated by US and MRI using a z test. A p value lower than 0.05 was considered significant. Analyses were performed using R version 3.5.2.
Approval
The study was approved by the head of management at Rigshospitalet, the head of the Department of Breast Surgery at Herlev and Gentofte Hospital, the head of the Department of Radiology, and The Danish Patient Safety Authority.
Results
Patient and Tumor Characteristics
The study identified 1888 breast cancer patients through searches of the DBCG database, the Patobank database, and the IMPAX radiology system Of these 1888 patients, 305 (307 breasts) fulfilled the inclusion criteria and were included in the study (Fig. 1).
Data on ethnicity were not available from the patient files. The study included 156 patients in the US group and 151 patients in the MRI group. Two patients had bilateral breast cancer, and these tumors were evaluated individually. One patient in the US group had insufficient receptor status and was not included in the subgroup analyses.
The patient and tumor characteristics of the two imaging groups are shown in Tables 1 and 2. No significant differences in patient or tumor characteristics were found between the US and MRI groups except for a small but significant difference in age and body mass index (BMI). The mean age was 52.4 years in the US group and 49.5 years in the MRI group (p = 0.028). The mean BMI was 26.3 kg/m2 in the US group and 24.9 kg/m2 in the MRI group (p = 0.020). The number of days between the last imaging and surgery or between the final chemotherapy session and the surgery did not differ significantly. The rates of reoperations in the two groups were comparable, with 12 (11.1 %) in the US group and 10 (9.9 %) in the MRI group (p = 0.776). Approximately one third of the patients in both groups were treated by mastectomy without a significant difference between the groups. In the US group, 56.4 % (n = 88) of the tumors were overestimated in size, and 26.9 % (n = 42) of the tumors were underestimated in size. In the MRI group, 51 % (n =77) of the tumors were overestimated in size, and 21.9 % (n = 33) of the tumors were underestimated in size. The numeric deviation in tumor size on imaging compared with pathology was 9.1 mm in the US group and 8.6 mm in the MRI group, and the difference was not statistically significant (p = 0.609).
Response Evaluation
In the US group, 51 (32.7 %) of the patients achieved a pCR compared with 37 (24.5 %) of the patients in the MRI group (p = 0.113) (Table 3). Of the four subgroups, the ER−/HER2+ subgroup in the US group had the highest rates of pCR (65.2 %), and the ER−/HER2− subgroup had the second highest rate (55.9 %) (Table 4). The MRI group had lower rates of pCR, with the highest rates being those of ER−/HER2+ (31.8 %) and ER+/HER2+ (29.8). The ER+/HER2− subgroup had the lowest pCR rate in both groups. In the MRI group 23.2 % of patients had a rCR compared with 16.7 % in the US group (p = 0.153).
Comparison of pCR Prediction
Agreement between the pathologic and radiologic responses in the US and MRI groups is shown in Table 5. Sensitivity, specificity, PPV, NPV, and accuracy for the US and the MRI groups are shown in Table 6. The US group had a lower specificity than the MRI group (p = 0.049), whereas sensitivity was high in both groups, with no significant difference. The PPV was significantly higher in the MRI group (p = 0.025), and accuracy also was higher, but the difference between the groups was not significant.
No significant difference in NPV was found between the groups. Estimates for the subgroups are shown in supplementary. The patients in the ER−/HER2− subgroup had the highest NPV in both the US group and the MRI group, but the results should be interpreted with caution due to the low number of patients in each subgroup, and accordingly, further statistical analysis was not performed.
Discussion
We found that MRI had a higher specificity and PPV than US in predicting pCR after NACT in breast cancer patients. The MRI group had a higher rate of rCR, which was more in agreement with pCR, causing the higher specificity and PPV. Sensitivity was high in both the MRI and US groups, supporting the view that both imaging methods are good at determining residual cancer.18 Although a difference in specificity between the two imaging methods was observed, this did not affect the rates of re-surgeries or mastectomy, which were comparable between the two groups. This indicates that both imaging methods are equally accurate for clinicians to use in planning post-NACT surgery. In addition, the choice of surgical procedure is not solely dependent on the response to chemotherapy, but is also dependent on other factors such as patient preference, persisting microcalcifications, and multifocality. The NPV was comparable between the two groups, although far from ideal (US, 65.4 %; MRI, 60.0 %) when the prospective aim was an attempted omission of surgery.
Like others, we found that the ER−/HER2+ subgroup showed the highest rate of pCR10 in both the MRI and US groups. The pCR rates of the US group were comparable with what has previously been found.7,10,25,26 In the subgroups of the MRI group, the rates of pCR differed from what would be expected with ER+/HER2+, rates almost as high as with ER−/HER2+ and with the ER−/HER2− rate as the second lowest. This variation could be explained by the relatively small number of patients in the subgroups.
In the literature, the definitions of pCR vary between pCR without DCIS (ypT0, pathologic evaluation after NACT showing no microscopic cancer cells or in situ components)8,27,28 and pCR with DCIS (ypT0/is, pathologic evaluation after NACT showing no cancer cells but allowing in situ components).29,30,31 This is important for clinicians to consider when comparing the pCR rates of NACT among studies. What is defined as positive and negative results also differs among studies. Some studies count pCR as a positive result,8,31,32 and others define the presence of tumor as a positive result.27,29,30,33 This must be kept in mind when sensitivity, specificity, PPV, and NPV are compared between studies. In this study, we regarded pCR without DCIS (ypT0) as a negative result.
This study of more than 300 patients is one of the larger studies on the topic. The prediction of pCR with MRI (NPV) found in our study was comparable with the finding of a smaller study by Bouzon et al.34 that included 91 patients,34 but we found a lower specificity of only 56 % compared with 79 % found by Bouzon et al.34 They used ypT0/is as their definition of pCR and did not include comparison with US.
A recent large study of 1219 patients by Zhang et al.,32 also using ypT0/is, compared US with MRI and found that MRI had a higher specificity than US (MRI, 44.4 % vs US, 36.2 %), as confirmed in our study. However, the difference was not significant. Vriens et al.18 stated in a study based on 182 patients that US is at least as good in predicting tumor size after NACT as MRI. However, the prediction of an absent residual tumor (NPV) was 33 % for US and 26 % for MRI, in contrast to our results showing NPV to be higher with both imaging methods (65.4 % with US and 60.0 % with MRI).
A limitation in this study was its design, with two groups examined via different imaging methods instead of a paired design with all patients examined via both MRI as US. The latter method would have lowered the risk of selection bias.
However, the differences in patient and tumor characteristics between the groups were small and mainly nonsignificant. A significant difference in age and BMI in the two groups was found, but this difference still was small and not considered to affect the evaluation of the imaging. Furthermore, the patients were allocated to treatment based on their municipality and not on their voluntary choice of hospital because both breast centers are highly specialized with similar diagnostic procedures.
Also, the user-dependent aspect of handheld US should be considered, although in the current study only breast-trained radiologists with high expertise performed US. The void artifact caused by the coil in the MRI measuring about 10 mm also was a notable consideration because this could have caused higher rates of false-negatives in the MRI group. A strength of the study was the definition of pCR (ypT0) that did not accept the remains of DCIS in the breast according to the clinical precautions of surgical practice.
The number of days between the last imaging and surgery was due to logistical structures of the clinical practice in the centers and could have caused further shrinkage and eradication of tumors, although no difference was observed between the US and MRI groups, and this interval was therefore considered to affect the groups equally. The number of days between the last imaging and surgery also would cause the imaging methods to overestimate tumor size more often, as seen in our study.
For patients with pCR, surgery in the breast is redundant. In attempts to avoid surgery for complete responders, neither MRI nor US were able to predict pCR in a way that surgery could be safely omitted. From this study, it was not possible to determine subgroups with higher predictability from the imaging methods. For omission of surgery in selected breast cancer patients after NACT, an important step is to compare the prediction of pCR in subgroups, especially the ER−/HER2− and ER−/HER2+ subgroups because they are known to have the highest rates of pCR and a better correlation between MRI and pathology.9 We found the estimates of the subgroups to be inconsistent with relatively large confidence intervals, which is why further comparison of the subgroups was not performed. Larger studies are needed for possible comparison and identification of subgroups with both a good response and good prediction of pCR.
In future studies, the accuracy of MRI could be further enhanced by minimizing the coil artifact via careful selection of coils. Also, biopsy techniques in addition to imaging have been suggested by several studies as a way to attempt an increase in the predictability of pCR.13,14,35,36,37 A recent study by Lee et al.38 stated that MRI findings indicating complete eradication of tumor combined with US-guided preoperative biopsies could help raise the prediction of pCR (NPV) to 87.1 %, which is higher than both the US and MRI findings in this study. The results from our study, based on a large study population, support the use of MRI in such studies.
Conclusion
In summary, to date, patients receiving NACT cannot avoid surgery, but MRI should be the imaging method used for optimizing and further improving the diagnostic accuracy of pCR prediction. Compared with US, MRI was significantly more specific in predicting pCR, although still not high enough to be a valid predictor of pCR for omission of surgery. The NPV was comparable between US and MRI. In future studies, MRI should be chosen as the preferred imaging method for a more accurate prediction of pCR. No subgroup in the current study showed a significantly higher specificity or NPV considering the relatively small number of patients in the groups. Larger subgroups are required for further studies.
References
Fisher B, Bryant J, Wolmark N, et al. Effect of preoperative chemotherapy on the outcome of women with operable breast cancer. J Clin Oncol. 1998;16:2672–85. https://doi.org/10.1200/jco.1998.16.8.2672.
Scholl SM, Fourquet A, Asselain B, et al. Neoadjuvant versus adjuvant chemotherapy in premenopausal patients with tumours considered too large for breast-conserving surgery: preliminary results of a randomised trial: S6. Eur J Cancer. 1994;30:645–52. https://doi.org/10.1016/0959-8049(94)90537-1.
Wolmark N, Wang J, Mamounas E, Bryant J, Fisher B. Preoperative chemotherapy in patients with operable breast cancer: nine-year results from National Surgical Adjuvant Breast and Bowel Project B-18. J Natl Cancer Inst Monogr. 2001;2001(30):96–102. https://doi.org/10.1093/oxfordjournals.jncimonographs.a003469.
Rastogi P, Anderson SJ, Bear HD, et al. Preoperative chemotherapy: updates of National Surgical Adjuvant Breast and Bowel Project Protocols B-18 and B-27. J Clin Oncol. 2008;26:778–85. https://doi.org/10.1200/jco.2007.15.0235.
Chen M, Zhan WW, Han BS, et al. Accuracy of physical examination, ultrasonography, and magnetic resonance imaging in predicting response to neo-adjuvant chemotherapy for breast cancer. Chin Med J. 2012;125:1862–6.
Hayashi N, Tsunoda H, Namura M, et al. Magnetic resonance imaging combined with second-look ultrasonography in predicting pathologic complete response after neoadjuvant chemotherapy in primary breast cancer patients. Clin Breast Cancer. 2019;19:71–7. https://doi.org/10.1016/j.clbc.2018.08.004.
Bouzon A, Iglesias A, Acea B, Mosquera C, Santiago P, Mosquera J. Evaluation of MRI accuracy after primary systemic therapy in breast cancer patients considering tumor biology: optimizing the surgical planning. Radiol Oncol. 2019;53:171–7. https://doi.org/10.2478/raon-2019-0023.
Fukuda T, Horii R, Gomi N, et al. Accuracy of magnetic resonance imaging for predicting pathological complete response of breast cancer after neoadjuvant chemotherapy: association with breast cancer subtype. Springerplus. 2016;5:152. https://doi.org/10.1186/s40064-016-1800-x.
Namura M, Tsunoda H, Yagata H, et al. Discrepancies between pathological tumor responses and estimations of complete response by magnetic resonance imaging after neoadjuvant chemotherapy differ by breast cancer subtype. Clin Breast Cancer. 2018;18:128–34. https://doi.org/10.1016/j.clbc.2017.07.001.
Houssami N, MacAskill P, Von Minckwitz G, Marinovich ML, Mamounas E. Meta-analysis of the association of breast cancer subtype and pathologic complete response to neoadjuvant chemotherapy. Eur J Cancer. 2012. https://doi.org/10.1016/j.ejca.2012.05.023.
van la Parra RF, Kuerer HM. Selective elimination of breast cancer surgery in exceptional responders: historical perspective and current trials. Breast Cancer Res. 2016;18:28. https://doi.org/10.1186/s13058-016-0684-6.
Curigliano G, Burstein HJ, Winer EP, et al. De-escalating and escalating treatments for early-stage breast cancer: the St. Gallen International Expert Consensus Conference on the Primary Therapy of Early Breast Cancer 2017. Ann Oncol. 2017. https://doi.org/10.1093/annonc/mdx308.
van der Noordaa MEM, van Duijnhoven FH, Loo CE, et al. Identifying pathologic complete response of the breast after neoadjuvant systemic therapy with ultrasound guided biopsy to eventually omit surgery: study design and feasibility of the MICRA trial (Minimally Invasive Complete Response Assessment). Breast. 2018;40:76–81. https://doi.org/10.1016/j.breast.2018.04.015.
Kuerer HM, Rauch GM, Krishnamurthy S, et al. A clinical feasibility trial for identification of exceptional responders in whom breast cancer surgery can be eliminated following neoadjuvant systemic therapy. Ann Surg. 2018;267:946–51. https://doi.org/10.1097/sla.0000000000002313.
Schaefgen B, Mati M, Sinn HP, et al. Can routine imaging after neoadjuvant chemotherapy in breast cancer predict pathologic complete response? Ann Surg Oncol. 2016;23:789–95. https://doi.org/10.1245/s10434-015-4918-0.
Shin HJ, Kim HH, Ahn JH, et al. Comparison of mammography, sonography, MRI, and clinical examination in patients with locally advanced or inflammatory breast cancer who underwent neoadjuvant chemotherapy. Br J Radiol. 2011;84:612–20. https://doi.org/10.1259/bjr/74430952.
Marinovich ML, Macaskill P, Irwig L, et al. Meta-analysis of agreement between MRI and pathologic breast tumour size after neoadjuvant chemotherapy. Br J Cancer. 2013;109:1528–36. https://doi.org/10.1038/bjc.2013.473.
Vriens BE, de Vries B, Lobbes MB, et al. Ultrasound is at least as good as magnetic resonance imaging in predicting tumour size post-neoadjuvant chemotherapy in breast cancer. Eur J Cancer. 2016;52:67–76. https://doi.org/10.1016/j.ejca.2015.10.010.
Taydas O, Durhan G, Akpinar MG, Demirkazik FB. Comparison of MRI and US in tumor size evaluation of breast cancer patients receiving neoadjuvant chemotherapy. Eur J Breast Heal. 2019;15:119–24. https://doi.org/10.5152/ejbh.2019.4547.
Park J, Chae EY, Cha JH, et al. Comparison of mammography, digital breast tomosynthesis, automated breast ultrasound, magnetic resonance imaging in evaluation of residual tumor after neoadjuvant chemotherapy. Eur J Radiol. 2018;108:261–8. https://doi.org/10.1016/j.ejrad.2018.09.032.
Londero V, Bazzocchi M, Del Frate C, et al. Locally advanced breast cancer: comparison of mammography, sonography, and MR imaging in evaluation of residual disease in women receiving neoadjuvant chemotherapy. Eur Radiol. 2004;14:1371–9. https://doi.org/10.1007/s00330-004-2246-z.
Danish Breast Cancer Cooperative Group. Pathology Guidelines. DBCG. Published 2013. Retrieved 17 July 2020 at https://www.dmcg.dk/siteassets/forside/kliniske-retningslinjer/godkendte-kr/dbcg/dbcg_patologiprocedure_rkkp_admgodk300420x.pdf.
Müller HD, Posch F, Suppan C, et al. Validation of residual cancer burden as prognostic factor for breast cancer patients after neoadjuvant therapy. Ann Surg Oncol. 2019. https://doi.org/10.1245/s10434-019-07741-w.
Campbell JI, Yau C, Krass P, et al. Comparison of residual cancer burden, American Joint Committee on Cancer staging and pathologic complete response in breast cancer after neoadjuvant chemotherapy: results from the I-SPY 1 trial (CALGB 150007/150012; ACRIN 6657). Breast Cancer Res Treat. 2017. https://doi.org/10.1007/s10549-017-4303-8.
Buzdar AU, Ibrahim NK, Francis D, et al. Significantly higher pathologic complete remission rate after neoadjuvant therapy with trastuzumab, paclitaxel, and epirubicin chemotherapy: results of a randomized trial in human epidermal growth factor receptor 2-positive operable breast cancer. J Clin Oncol. 2005. https://doi.org/10.1200/JCO.2005.07.032.
Gianni L, Eiermann W, Semiglazov V, et al. Neoadjuvant chemotherapy with trastuzumab followed by adjuvant trastuzumab versus neoadjuvant chemotherapy alone in patients with HER2-positive locally advanced breast cancer (the NOAH trial): a randomised controlled superiority trial with a parallel HER. Lancet. 2010. https://doi.org/10.1016/S0140-6736(09)61964-4.
van Ramshorst MS, Loo CE, Groen EJ, et al. MRI predicts pathologic complete response in HER2-positive breast cancer after neoadjuvant chemotherapy. Breast Cancer Res Treat. 2017. https://doi.org/10.1007/s10549-017-4254-0.
Gampenrieder SP, Peer A, Weismann C, et al. Radiologic complete response (rCR) in contrast-enhanced magnetic resonance imaging (CE-MRI) after neoadjuvant chemotherapy for early breast cancer predicts recurrence-free survival but not pathologic complete response (pCR). Breast Cancer Res. 2019. https://doi.org/10.1186/s13058-018-1091-y.
Baumgartner A, Tausch C, Hosch S, et al. Ultrasound-based prediction of pathologic response to neoadjuvant chemotherapy in breast cancer patients. Breast. 2018. https://doi.org/10.1016/j.breast.2018.02.028.
De Los Santos JF, Cantor A, Amos KD, et al. Magnetic resonance imaging as a predictor of pathologic response in patients treated with neoadjuvant systemic treatment for operable breast cancer: translational Breast Cancer Research Consortium trial 017. Cancer. 2013. https://doi.org/10.1002/cncr.27995.
Weber JJ, Jochelson MS, Eaton A, et al. MRI and prediction of pathologic complete response in the breast and axilla after neoadjuvant chemotherapy for breast cancer. J Am Coll Surg. 2017. https://doi.org/10.1016/j.jamcollsurg.2017.08.027.
Zhang K, Li J, Zhu Q, Chang C. Prediction of pathologic complete response by ultrasonography and magnetic resonance imaging after neoadjuvant chemotherapy in patients with breast cancer. Cancer Manage Res. 2020;12:2603–12. https://doi.org/10.2147/CMAR.S247279.
Croshaw R, Shapiro-Wright H, Svensson E, Erb K, Julian T. Accuracy of clinical examination, digital mammogram, ultrasound, and MRI in determining postneoadjuvant pathologic tumor response in operable breast cancer patients. Ann Surg Oncol. 2011;18:3160–3. https://doi.org/10.1245/s10434-011-1919-5.
Bouzon A, Acea B, Soler R, et al. Diagnostic accuracy of MRI to evaluate tumour response and residual tumour size after neoadjuvant chemotherapy in breast cancer patients. Radiol Oncol. 2016;50:73–9. https://doi.org/10.1515/raon-2016-0007.
Heil J, Schaefgen B, Sinn P, et al. Can a pathological complete response of breast cancer after neoadjuvant chemotherapy be diagnosed by minimal invasive biopsy? Eur J Cancer. 2016. https://doi.org/10.1016/j.ejca.2016.09.034.
Basik M, Costantino JP, De Los Santos JF, et al. NRG Oncology BR005: phase II trial assessing accuracy of tumor bed biopsies (Bx) in predicting pathologic response in patients (Pts) with clinical/radiological complete response (CR) after neoadjuvant chemotherapy (NCT) in order to explore the feasibility. J Clin Oncol. 2018. https://doi.org/10.1200/jco.2018.36.15_suppl.tps604.
Heil J, Sinn P, Richter H, et al. RESPONDER: diagnosis of pathological complete response by vacuum-assisted biopsy after neoadjuvant chemotherapy in breast Cancer: a multicenter, confirmative, one-armed, intra-individually controlled, open, diagnostic trial. BMC Cancer. 2018. https://doi.org/10.1186/s12885-018-4760-4.
Lee H-B, Han W, Kim S-Y, et al. Prediction of pathologic complete response using image-guided biopsy after neoadjuvant chemotherapy in breast cancer patients selected based on MRI findings: a prospective feasibility trial. Breast Cancer Res Treat. 2020;182:97–105. https://doi.org/10.1007/s10549-020-05678-3.
Acknowledgments
Funding for the study was granted by the research fund of Herlev and Gentofte University Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
There are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Palshof, F.K., Lanng, C., Kroman, N. et al. Prediction of Pathologic Complete Response in Breast Cancer Patients Comparing Magnetic Resonance Imaging with Ultrasound in Neoadjuvant Setting. Ann Surg Oncol 28, 7421–7429 (2021). https://doi.org/10.1245/s10434-021-10117-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-10117-8