Abstract
Background
Anatomic resection with lymph node dissection or sampling is the standard treatment for early non-small cell lung cancer (NSCLC), and wedge resection is an option for compromised patients. This study aimed to determine whether wedge resection can provide comparable prognoses for elderly patients with NSCLC.
Methods
The study analyzed the clinicopathologic findings and surgical outcomes during a median follow-up period of 39.6 months for 156 patients with solid dominant (consolidation-to-tumor ratio > 0.5) small (whole tumor size ≤ 2 cm) NSCLC among 892 patients 80 years of age or older with medically operable lung cancer between April 2015 and December 2016.
Results
The 3-year overall survival (OS) rates after wedge resection and after segmentectomy plus lobectomy did not differ significantly (86.5 %; 95 % confidence interval [CI], 74.6–93.0 % vs 83.7 % 95 % CI, 74.0–90.0 %; P = 0.92). Multivariable Cox regression analysis of OS with propensity scores showed that the surgical procedure was not an independent prognostic predictor (hazard ratio [HR], 0.84; 95 % CI, 0.39–1.8; P = 0.64). The 3-year OS rates were slightly better after wedge resection for 97 patients who could tolerate lobectomy than after segmentectomy plus lobectomy (89.4 %; 95 % CI, 73.8–95.9 % vs 75.8 %; 95 % CI, 62.0–85.2 %; P = 0.14). The cumulative incidence of other causes for death was marginally higher after segmentectomy plus lobectomy than after wedge resection (P = 0.079).
Conclusions
Wedge resection might be equivalent to lobectomy or segmentectomy for selected patients 80 years of age or older with early-stage NSCLC who can tolerate lobectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The ongoing, prospective, randomized Japanese Clinical Oncology Group 0802/West Japan Oncology Group 4607L (JCOG0802/WJOG4607L) trial1 mainly compares prognoses and postoperative pulmonary functions between patients treated with anatomic segmentectomy and those treated with lobectomy for early-stage non-small cell lung cancer (NSCLC) when the whole tumor size, including ground glass opacity (GGO), is 2 cm or smaller and the consolidation-to-tumor (C/T) ratio is higher than 0.5 (i.e., a solid dominant tumor) on high-resolution computed tomography (CT) images. The Cancer and Leukemia Group B (CALGB) 140503 trial2 is similar, but sublobar resection in that study comprises segmentectomy and wedge resection. Although the standard surgical procedure for lung cancer is lobectomy with lymph node dissection or sampling.3,4 this could be changed from lobectomy to segmentectomy for early-stage NSCLC if the results of these randomized trials are positive. Anatomic resection including segmentectomy and lobectomy is considered a possible standard treatment for such populations based on previous clinical findings of patients who were mostly younger than 80 years.5 However, the prevalence of octogenarians with NSCLC is increasing.
Patients 80 years of age or older are assumed to be at higher risk for anatomic resection than those younger than 80 years.6,7 Thus, whether anatomic or wedge resection would be optimal for such populations has remained unclear. Although similar prognoses, fewer postoperative complications, and fewer other causes of death after wedge resection than after anatomic resection have been reported,8 lobectomy tolerance has remained unknown. Thus, the group treated by wedge resection in that study included compromised patients who could not tolerate lobectomy, and the anatomic resection group included patients with centrally located tumors that could not be eliminated by wedge resection.
The Japanese Association for Chest Surgery (JACS) conducted a nationwide, multicenter, large-scale, prospective, observational cohort study of postoperative risk and prognosis scores for elderly patients, especially those 80 years of age or older, with medically operable lung cancer (JACS1303), which was published in 2016.9 The data include preoperative Charlson Comorbidity Indices (CCIs), tumor location, and preoperative pulmonary function so wedge and anatomic resection could be compared among octogenarians who could tolerate lobectomy in the database.
The current study aimed to determine the prognostic ability and short-term outcomes, including operative findings and postoperative complications, of the extent of lung resection for peripherally located tumors in patients 80 years old or older with tumors 2 cm or smaller who had a C/T ratio higher than 0.5 in the JACS1303 database and could tolerate lobectomy.
Methods
Patient Eligibility
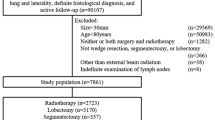
Between April 2015 and December 2016, 1019 patients 80 years of age or older with medically operable lung cancer at 82 institutions were enrolled in the JACS1303 cohort (UMIN000016756). A comprehensive surgical risk score was devised to predict postoperative complications for 895 of these patients.10 Briefly, additional inclusion criteria comprised no previous chemotherapy or radiation therapy for lung cancer, sufficient organ function, measurable preoperative comprehensive geriatric assessment, and written informed consent.
Among the 895 patients who underwent surgical resection for primary lung cancer and had sufficient clinical records for comprehensive surgical risk score analyses of predictive postoperative complications, we analyzed 156 who had whole tumors 2 cm in size or smaller, including GGO components, and a C/T ratio higher than 0.5 (solid dominant). The C/T ratio was defined as the maximum consolidated diameter divided by the maximum tumor diameter. The 156 patients were followed up for a median of 39.6 months (range, 11.8–54.3 months).
We defined fitness for lobectomy according to the JCOG0802/WJOG4607L1 criteria of tumor location and pulmonary functions as peripherally located tumors centered in the outer third of the lung field with a predicted postoperative forced expiratory volume in 1 s (FEV1) greater than 800 mL and a preoperative Charlson Comorbidity Index (CCI) of 2 or lower.
Data Collection
The institutional review boards of all the participating institutions approved the data collection and analyses. After obtaining written informed consent from the patients, recruiting clinicians completed case report forms describing the clinicopathologic factors of age, sex, smoking status, tumor size and location, histologic subtypes according to the World Health Organization classification,11 and stage according to the seventh edition of the tumor-node-metastasis (TNM) classification of lung and pleural tumors.12 The condition of the patients was determined from performance status, pulmonary function including percentage of vital capacity (%VC), FEV1, and FEV1%. Comorbidity indices were calculated using the CCI.13 Postoperative data also were collected.
The follow-up evaluation of the patients after pulmonary resection depended on the schedule of the participating institutions. In general, the patients were followed up at 3- to 6-month intervals for 3 years, at 6- to 12-month intervals for the next 2 years, and then annually as required. The follow-up evaluations included a physical examination and routine laboratory tests including tumor markers, chest x-rays, and chest and abdominal CT. Fluorodeoxyglucose-positron emission tomography (FDG-PET) and brain imaging were requested as required based on clinical symptoms.
Statistical Analyses
Continuous and categorical variables were analyzed using nonparametric Mann-Whitney U tests, Kruskal-Wallis tests, and chi-square or Fisher’s exact tests. Overall survival (OS) and progression-free survival (PFS) rates were calculated from Kaplan-Meier curves, and two groups were compared using univariable log-rank analyses. Prognostic factors were determined by uni- and multivariable analyses of OS using Cox regression. Background variables with potential differences between wedge resection and segmentectomy plus lobectomy were adjusted using propensity score stratification.
Propensity scores were calculated using a logistic regression model based on preoperative characteristics that included age, gender, smoking status (pack-years), and tumor size on high-resolution CT (HRCT). Stratified propensity scores were included as covariates in multivariable Cox regression analyses of OS. The cumulative incidences of all-cause lung cancer and other causes of death were estimated considering competing risk according to surgical procedures, and P values were calculated using Gray tests.
All data were statistically analyzed using EZR, version 1.37 (Saitama Medical Centre, Jichi Medical University, Shimotsuke, Tochigi, Japan), which is a graphic user interface for R version 3.4.4 (The R Foundation for Statistical Computing, Vienna, Austria).14 Values with a P value of 0.05 or lower were deemed statistically significant.
Results
Clinicopathologic Findings and Prognosis for Octogenarians with Clinical Stage 1A Tumors 2 cm or Smaller and a C/T Ratio Greater Than 0.5
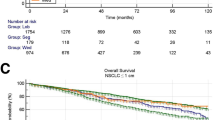
The prevalence of males, smoking status, performance status, tumor types, comorbidity indices, and preoperative pulmonary functions were similar between the patients after wedge and anatomic resection (Table 1). After patients who underwent wedge resection had shorter surgical durations, less blood loss during procedures, shorter hospital stays, and lower frequencies of postoperative complications than the patients who had anatomic resection (Table 1). The 3-year OS and PFS rates were similar for the patients after wedge and anatomic resections (P = 0.92 [Fig. 1], P = 0.76 [Fig. S1A]). Multivariable Cox regression analysis for OS using propensity scores showed that the choice of surgical procedures was not a prognostic factor (Table 2).
The 3-year survival rates for patients 80 years old or older with clinical stage 1A tumors 2 cm or smaller and C/T ratios greater than 0.5 according to surgical procedures. The 3-year OS rates for patients after wedge and anatomic resections (segmentectomy and lobectomy) (86.5 %; 95 % CI, 74.6–93.0 % vs 83.7 %; 95 % CI, 74.0–90.0 %; P = 0.92, log-rank tests) are shown. CI, confidence interval; C/T, consolidation to tumor; OS, overall survival
Clinicopathologic findings and prognoses also were assessed among wedge resection, segmentectomy, and lobectomy (Tables S1 and S2; Figs. S2 and S1C). The patients who underwent wedge resection, had shorter surgical durations and hospital stays, less blood loss during procedures, and lower frequencies of postoperative complications than those who underwent the other procedures (Table S2), but OS and PFS did not differ significantly among the three groups (Figs. S2 and S1C).
Clinicopathologic Findings, Prognoses, and Cumulative Incidences of Death Among Octogenarians with Clinical Stage 1A Tumors 2 cm or Smaller and a C/T Ratio Greater Than 0.5 who were Suitable for Lobectomy
We assumed that among the 156 patients, lobectomy would be tolerated by 43 patients after wedge resection and by 54 patients after and anatomic resection (including 14 segmentectomies and 40 lobectomies). That is, they met the lobectomy-fitness criteria. Table 3 shows similar clinicopathologic findings between the total cohort and the patients who met the lobectomy fitness criteria.
Although the difference did not reach significance, the OS and PFS were slightly better for octogenarians with small (≤ 2 cm) and solid predominant (C/T ratio > 0.5) clinical stage 1A tumors after wedge resection than after anatomic resection (Fig. 2 and Fig. S1B). Moreover, the cumulative incidences of other causes of death were marginally lower after wedge resection than after anatomic resection (P = 0.079; Fig. 3).
The 3-year survival rates for patients 80 years old or older with clinical stage 1A tumors 2 cm or smaller and C/T ratios greater than 0.5 who could tolerate lobectomy according to surgical procedures. The 3-year OS rates of patients after wedge resection and anatomic resections (segmentectomy and lobectomy) (89.4 %; 95 % CI, 73.8–95.9 % vs 75.8 %; 95 % CI, 62.0–85.2 %; P = 0.14, log-rank tests) are shown. CI, confidence interval; C/T, consolidation to tumor; OS, overall survival
The clinicopathologic findings, prognoses, and cumulative incidences of death also were compared after wedge resection, segmentectomy, and lobectomy (Tables S3 and S4; Figs. S1D, S3, and S4). In terms of locoregional failure, among 43 patients, 2 (4.7 %) had lung stump recurrence and 1 (2.3 %) had intrathoracic lymph node recurrence after wedge resection, whereas 1 (2.5 %) of 40 patients had intrathoracic lymph node recurrence after lobectomy. The rates of local and distant recurrence were comparable among the patients after the three types of surgery (Tables S5 and S6).
Discussion
The current findings showed that the OS after wedge resection and anatomic resection comprising segmentectomy and lobectomy was similar among octogenarians with early-stage, NSCLC tumors 2 cm or smaller including GGO components and a C/T ratio greater than 0.5. In fact, wedge resection was associated with less toxicity, shorter procedures, less operative blood loss, and fewer postoperative complications than anatomic resection. Furthermore, the prevalence of other causes of death was lower after wedge resection than after anatomic resection. These findings are important for deciding treatment strategies for octogenarians with NSCLC.
The current study analyzed octogenarians with NSCLC tumors 2 cm or smaller and a C/T ratio greater than 0.5. Although the standard surgical procedure for this population currently is lobectomy, segmentectomy also will become a standard surgical procedure if the postoperative pulmonary function and prognoses are positive in the JCOG0802/WJOG4607L1 and CALGB1405032 trials. Therefore, we compared the outcomes between wedge resection and segmentectomy plus lobectomy (standard anatomic resection). The results showed similar prognoses for both the total cohort and octogenarians who were deemed fit to undergo lobectomy after the three types of procedures.
In terms of OS, prognosis is affected by oncologic aspects and general status including cardiopulmonary function. Based on the association between wedge resection and fewer other causes of death than with segmentectomy and lobectomy (Fig. 3 and Fig. S4), wedge resection was less toxic in general over the long term. In addition, wedge resection also was less toxic than anatomic resection from the viewpoint of short-term surgical outcomes including surgical duration, procedural blood loss, and length of postoperative hospital stay. Similar to previous findings,3,15 fewer postoperative complications occurred after wedge resection than after anatomic resection. Notably, severe postoperative complications did not arise, and postoperative mortality was not increased among the octogenarians after wedge resection.
On the other hand, the cumulative incidence of cancer death was similar between wedge resection and anatomic resection although oncologic control of NSCLC generally is better after anatomic resection. One reason for this was that the tumors were slightly smaller in the wedge resection group. Another reason was less oncologic aggressiveness because NSCLC with a whole tumor size of 2 cm or smaller and a C/T ratio greater than 0.5 might have been less malignant,16 which would have resulted in few differences in oncologic control among the procedures. Even if a smaller tumor is balanced, the prognosis might be at least similar among surgical procedures because in this study, OS was slightly better after wedge resection than after anatomic resection.
Because the median follow-up duration was shorter than 5 years, we also assessed the PFS among the patients who underwent the three types of surgical procedures. The finding that PFS also was slightly better after wedge resection than after anatomic resection, segmentectomy, and lobectomy in the lobectomy-fit population supported the OS data.
The OS was not better in the lobectomy-fit population than in the unselected cohort after anatomic resection, although it was slightly better after wedge resection. One explanation might be that some compromised patients who could not tolerate lobectomy underwent wedge resection, whereas fewer compromised patients underwent anatomic resection. Although borderline patients also might have undergone anatomic resection, all the patients in that group also were judged as able to tolerate lobectomy.
Lymph nodes were not sampled for most of the patients treated by wedge resection. This study targeted early-stage NSCLC based on preoperative findings. Hence, in terms of preoperative clinical staging, our study population would not have changed even if the lymph nodes in the wedge resection group had been sampled for pathologic staging. However, the global oncologic gold standard for all NSCLC resections is lymph node dissection or sampling for tolerant patients. Although intolerance due to factors such as advanced age is one justification for omitting lymph node sampling in some specific clinical situations, it should be attempted with extreme caution. For instance, one way to interpret the data is to consider that the threefold higher incidence of local recurrence after wedge resection group versus lobectomy plus segmentectomy might be due to the omission of lymph node-sampling. In addition, although the prognosis was comparable between wedge resection and lobectomy plus segmentectomy during approximately 3 years of follow-up evaluation, the influence of omitting of lymph node-sampling on prognosis might become apparent only after 5 years of follow-up evaluation. Thus, lymph nodes should be sampled during wedge resection for tolerant patients.
A previous study found that OS is not inferior after wedge resection compared with anatomic resection,8 but the preoperative findings that were applied to determine surgical procedures, such as tumor location and comorbidity, were not included in the report. Thus, we had less selection bias than that study. We determined lobectomy tolerance based on peripheral tumor location, pulmonary function defined as more than 800 mL of predicted postoperative FEV1, and a preoperative Charlson Comorbidity Index of 2 or lower. The lobectomy fitness criterion of the tumor location was assumed from a prospective randomized study that compared wedge resection and anatomic resection. Therefore, lobectomy-fitness data will support the design of clinical trials to determine optimal surgical procedures for elderly patients with early-stage NSCLC. On the other hand, the focus of the current study was a specific population such as that in the JCOG0802/WJOG4607L prospective clinical trial.1
This study had several limitations. One limitation was selection bias. Although the data were collected prospectively, the surgeons at each institution determined the surgical strategy, considering the oncologic status of each patient including intraoperative nodal involvement and overall condition. We reduced selection bias by analyzing data regarding a likely tolerance of lobectomy. With this analysis, the prognosis might be comparable or better for elderly patients who could tolerate lobectomy after wedge resection compared with the prognosis of patients after anatomic resection, even considering the limitation of selection bias.
The median follow-up duration was approximately 40 months, not 60 months. Although 40 months might be insufficient for determining long-term survival, octogenarians are unlikely to remain alive longer than patients 79 years of age or younger, and we added the PFS data to help compensate for this. At this writing, we plan to provide 5-year OS data after another 20 months. Thus, the current study provided important survival information.
The database does not include information about the surgical margin or the numbers of lymph nodes and lymph node stations. The database also includes no information about postoperative quality of life. If the quality of life is considerably worse after than before surgical resection, then any procedures would not be optimal for patients, even if their cancer is completely controlled by surgical resection. Anatomic resection, lobectomy, and segmentectomy include more awareness of reducing the postoperative quality of life than wedge resection. We considered that the number of patients regarded as sufficiently fit to tolerate lobectomy was small (~ 100) because this study targeted a specific population to address the vital clinical issue of which surgical procedure is optimal for octogenarians with early-stage NSCLC considering oncologic aspects and overall status. The database includes information from more than 80 institutions, which causes difficulties collecting more targeted patients. Nonetheless, the prognostic role of wedge resection should be validated in a prospective randomized comparison between wedge resection and standard lobectomy or segmentectomy.
In conclusion, wedge resection might be equivalent to anatomic resection, including lobectomy or segmentectomy, for selected octogenarians with early-stage NSCLC. A prospective study of a larger patient cohort is required to validate the current findings.
References
Nakamura K, Saji H, Nakajima R, Okada M, Asamura H, Shibata T, et al. A phase III randomized trial of lobectomy versus limited resection for small-sized peripheral non-small cell lung cancer (JCOG0802/WJOG4607L). Jpn J Clin Oncol. 2010;40:271–4.
Kohman LJ, Gu L, Altorki N, Scalzetti E, Veit LJ, Wallen JM, et al. Biopsy first: lessons learned from Cancer and Leukemia Group B (CALGB) 140503. J Thorac Cardiovasc Surg. 2017;153:1592–7.
Ginsberg RJ, Rubinstein LV. Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung Cancer Study Group. Ann Thorac Surg. 1995;60:615–22 (discussion 22–3).
Darling GE, Allen MS, Decker PA, Ballman K, Malthaner RA, Inculet RI, et al. Randomized trial of mediastinal lymph node sampling versus complete lymphadenectomy during pulmonary resection in the patient with N0 or N1 (less than hilar) non-small cell carcinoma: results of the American College of Surgery Oncology Group Z0030 Trial. J Thorac Cardiovasc Surg. 2011;141:662–70.
Okada M, Yoshikawa K, Hatta T, Tsubota N. Is segmentectomy with lymph node assessment an alternative to lobectomy for non-small cell lung cancer of 2 cm or smaller? Ann Thorac Surg. 2001;71:956–60 (discussion 61).
Okami J, Shintani Y, Okumura M, Ito H, Ohtsuka T, Toyooka S, et al. Demographics, safety and quality, and prognostic information in both the seventh and eighth editions of the TNM Classification in 18,973 surgical cases of the Japanese Joint Committee of Lung Cancer Registry Database in 2010. J Thorac Oncol. 2019;14:212–22.
Okami J, Higashiyama M, Asamura H, Goya T, Koshiishi Y, Sohara Y, et al. Pulmonary resection in patients aged 80 years or over with clinical stage I non-small cell lung cancer: prognostic factors for overall survival and risk factors for postoperative complications. J Thorac Oncol. 2009;4:1247–53.
Mimae T, Miyata Y, Tsutani Y, Imai K, Ito H, Nakayama H, et al. Wedge resection as an alternative treatment for octogenarian and older patients with early-stage non-small cell lung cancer. Jpn J Clin Oncol. 2020;50:1051–7.
Saji H, Ueno T, Nakamura H. Prospective observational cohort study of postoperative risk and prognosis scoring for elderly patients with medically operable lung cancer (JACS1303). Gen Thorac Cardiovasc Surg. 2016;64:634–5.
Saji H, Ueno T, Nakamura H, Okumura N, Tsuchida M, Sonobe M, et al. A proposal for a comprehensive risk scoring system for predicting postoperative complications in octogenarian patients with medically operable lung cancer: JACS1303. Eur J Cardiothorac Surg. 2018;53:835–41.
Travis WDBE, Burke AP, Marx A, Nicholson AG. WHO Classification of tumours of the lung, pleura, thymus and heart. 4th edn. Lyon, France: International Agency for Research on Cancer; 2015.
TNM Classification of Malignant Tumours. 7th ed. Wiley-Blackwell, Oxford, UK, 2009.
Charlson ME, Sax FL, MacKenzie CR, Fields SD, Braham RL, Douglas RG Jr. Resuscitation: how do we decide? A prospective study of physicians’ preferences and the clinical course of hospitalized patients. JAMA. 1986;255:1316–22.
Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transp. 2013;48:452–8.
Linden PA, D’Amico TA, Perry Y, Saha-Chaudhuri P, Sheng S, Kim S, et al. Quantifying the safety benefits of wedge resection: a Society of Thoracic Surgery database propensity-matched analysis. Ann Thorac Surg. 2014;98:1705–11 (discussion 11–2).
Mimae T, Tsutani Y, Miyata Y, Imai K, Ito H, Nakayama H, et al. Solid tumor size of 2 cm divides outcomes of patients with mixed ground-glass-opacity lung tumors. Ann Thorac Surg. 2020;109:1530–6.
Acknowledgments
This study was supported by a Grant-in-Aid from the Committee for Scientific Affairs, The Japanese Association for Chest Surgery, Kyoto, Japan and by grants from the Japan Society for the Promotion of Science (JSPS) KAKENHI (20K09177). The language in this report was proof-checked by a native English speaker with more than 25 years of experience in professionally editing medical manuscripts.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Keiju Aokage gave lecture presentations for Mochida Pharmaceutical Co., Ltd, Astrazeneca, Covidien Japan, Taiho Parma, Bristol Myers Squibb, and Eli Lilly; gave seminar presentations for MSD; and did writing for Taiho Parma and Care-net.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.




Rights and permissions
About this article
Cite this article
Mimae, T., Saji, H., Nakamura, H. et al. Survival of Octogenarians with Early-Stage Non-small Cell Lung Cancer is Comparable Between Wedge Resection and Lobectomy/Segmentectomy: JACS1303. Ann Surg Oncol 28, 7219–7227 (2021). https://doi.org/10.1245/s10434-021-09835-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-09835-w